Abstract
Objective
To analyze sleep quality and associated socio-demographic and lifestyle factors in participants from a city originally colonised by Germans in southern Brazil.
Methods
A cross-sectional population-based study of 2333 individuals aged 20 to 79 years. Data was collected by interview using a structured questionnaire. Sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI) questionnaire. The prevalence of poor sleep quality (PSQI score five or more) was estimated and the associations with study variables were measured by crude and adjusted prevalence ratios using Poisson regression.
Results
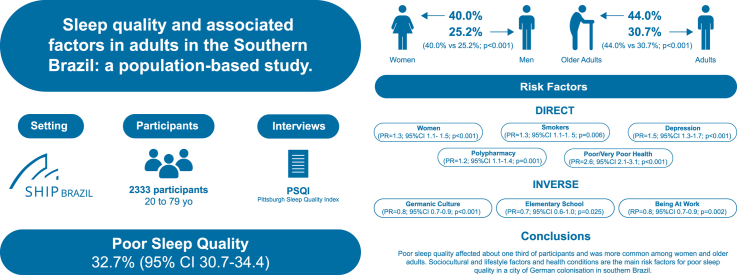
participants were mostly women (50.9 %), with an average age of 43.3 years. The median total PSQI score was 4 (IQ = 3-7). The frequency of poor sleep quality was 32.7 % (95 % CI 30.7-34.4), higher in older adults (44.0 % vs 30.7 %; p<0.001) and women (40.0 % vs 25.2 %; p<0.001). Multivariate analysis showed that women (PR = 1.3; 95%CI 1.1- 1.5; p<0.001), former smokers (PR = 1.2; 95%CI 1.0-1.4; p = 0.014), current smokers (PR = 1.3; 95%CI 1.1-1.5; p = 0.006), depression (PR = 1.5; 95%CI 1.3-1.7; p<0.001), taking 5 or more medications (PR = 1.2; 95%CI 1.1-1.4; p = 0.001), self-perceived fair health (PR = 2.1; 95%CI 1.8-2.4; p<0.001) or poor/very poor health (PR = 2.6; 95%CI 2.1-3.1; p<0.001) were risk factors for poor sleep quality. Germanic culture (PR = 0.8; 95%CI 0.7-0.9; p<0.001), high school (PR = 0.8; 95%CI 0.6–1.0; p = 0.046) or elementary school (PR = 0.7; 95%CI 0.6-1.0; p = 0.025) or being at work (RP = 0.8; 95%CI 0.7-0.9; p = 0.002) were inversely associated with poor sleep quality.
Conclusions
Women, older adults and some clinical, social, cultural and behavioural conditions are associated with poor sleep quality.
Keywords: Sleep quality, Sleep duration, Older adults, Polypharmacy, Smoking, Socioeconomic factors
Graphical abstract
Highlights
-
•
The sleep quality of German descendants in southern Brazil is still unknown.
-
•
One third of the participants reported poor sleep quality, which was worse in women and older adults.
-
•
Clinical conditions (depression, polypharmacy and poor self-perceived health) were associated with poor sleep quality.
-
•
Social factors (being at work) and cultural factors (German culture) were inversely associated with poor sleep quality.
1. Introduction
Adequate duration and depth of sleep are necessary for body properly function [1]. Poor sleep quality is associated with increased mortality and higher prevalence of metabolic syndrome, type 2 diabetes, hypertension, coronary heart disease and depression [[2], [3], [4], [5]]. In addition, changes in sleep quality can affect cognitive functions, such as the ability to concentrate and learn, as well as family and social relationships [6].
Sleep problems can be related to various determinants such as individual characteristics (age, sex, ethnicity, marital status, chronic diseases), lifestyle (smoking, alcohol consumption, physical activity), living conditions and socioeconomic factors (education, per capita income, place of residence) [7]. In a Brazilian population, a nationwide survey found a prevalence of 65.5 % of poor sleepers [8]. These studies suggest that women have more sleep problems and that older women use more sleeping pills [9], but the link between sleep and age remains controversial [8,10,11].
Brazil has a population of diverse genomic ancestry, with a European predominance in southern Brazil [12] due to several waves of migrants from Portugal, Italy and Germany, who brought their own habits and cultures. Nevertheless, studies on the quality of sleep in populations of mostly German origin in the southern region of Brazil are still little explored. It is not known how the quality of sleep in these individuals relates to the different local factors following immigration from Europe and its descendants [13].
The aim of this study was to analyze sleep quality and possible associations with socio-demographic and lifestyle characteristics in a city in southern Brazil originally colonized by Germans.
2. Methods
This is a cross-sectional population-based study of participants in the baseline of the Study of Health in Pomerode (SHIP-Brazil).
2.1. Sample procedures and data collection
This is a cohort study established by the University of Blumenau (FURB) in collaboration with the University Medicine Greifswald (Germany). The methods have been described elsewhere [14]. Briefly, a representative sample of 3678 participants was estimated, stratified by sex and age group from 20 to 79 years. Participants had to live in Pomerode for at least 6 months and sign the informed consent form. Individuals with cognitive and/or communication limitations, such as not speaking Portuguese, were excluded.
Data were collected between July 2014 and June 2018 using pre-tested questionnaires in home interviews. Participants also underwent various examinations at the Study Examination Centre at the University Hospital of Blumenau. The standard operating procedures are available at www.furb.br/vspomerode. In the end, 2488 people participated. The study was approved by the Ethics Committee of the University of Blumenau (2.969.842).
2.2. Dependent variable
Sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI). The PSQI consists of 19 questions covering seven domains: subjective sleep quality (very good, fairly good, fairly bad, very bad), sleep latency (less than 15 min, 16 to 30 min, 31 to 60 min and 60 and more minutes), sleep duration (more than 7 h, 6 to 7 h, 5 to 6 h, less than 5 h), habitual sleep efficiency (more than 85 %, 75 to 84 %, 65 to 74 % and less than 65 %), sleep disturbances (less than once a month, less than once a week, once or twice a week, three time or more in a week), use of sleep medications (less than once a month, less than once a week, once or twice a week, three time or more in a week), and daytime dysfunction (less than once a month, less than once a week, once or twice a week, three time or more in a week). This results in a global score ranging from zero (best quality) to 21 (worst quality). A global PSQI score greater than 5 represents a good sensitivity/specificity cut-off point between “good sleepers” and “poor sleepers” [15].
2.3. Independent variables
The socio-demographic characteristics analyzed were sex (male/female), age (in years and age groups), marital status (single/separated/widowed or married). German culture was defined by considering participants who spoke German regularly at home [16]. Education was estimated in years of schooling. For employment status, participants were asked whether they were working or not. Ethnicity/color was self-reported (white/non-white) [17].
Participants were classified as current smokers, former smokers or no smokers. The International Physical Activity Questionnaire (IPAQ) was used to assess physical activity [18]. Those who performed moderate or vigorous physical activity at least five times a week for a total of at least 150 min were considered to be sufficiently active [18]. Alcohol consumption patterns were assessed for frequency and quantity using the Alcohol Use Disorders Identification Test (AUDIT-C) [19].
Some self-reported health conditions were assessed by the question “Has a doctor told you that you have … ", hypertension (yes/no), diabetes mellitus (yes/no), depression (yes/no). Multimorbidity was defined as the simultaneous presence of two or more conditions and polypharmacy as the use of 5 or more concurrent medications. Self-perceived health was defined by the question “In general, how do you think your health is?” and could vary from very good, good, fair, poor or very poor.
Body weight was measured using a W300 electronic scale (Welmy Balanças, Santa Barbara do Oeste, Brazil) with a total capacity of 300 kg and an accuracy of 50 g. Height was measured using a stadiometer with a pole attached to the scale. Participants were examined wearing minimal clothing and no jewellery. Body mass index (BMI) was calculated by dividing body mass (kg) by height squared (meters) and classified as eutrophic (less than 25), overweight (25 to less than 30) and obesity (30 and more) [20].
2.4. Statistical analysis
The SHIP-Brazil study sample differed in terms of age and sex from the Pomerode population. Inverse probability weighting technique was used to minimize this potential bias [21]. In short, the probability of being selected was calculated for each participant. The weight, which is the inverse of the selection probability, was calculated and included in the analysis. In this way, each selected participant was considered not only for its own value, but also for those with characteristics that were not selected.
Variables were tested for normality using the Shapiro-Wilk test. The internal consistency of the PSQI was estimated using the Cronbach's alpha test. The association between the overall sleep quality score (median and interquartile range [IQR]) by sex and age group was estimated using the Wilcoxon test. Comparisons between the frequencies of the response categories for the seven components are presented overall and stratified by sex and age group using Pearson's chi-squared test. The frequency of poor sleep quality was estimated from the sleep quality score (cut-off point of five or more). Prevalence ratios were estimated using Poisson regression models with backward stepwise technique. Variables with a p-value ≥0.20 were included in the multivariate analysis and those with a p-value <0.05 estimated by the maximum likelihood ratio test were included in the final model. This manuscript was written according to the STROBE statement. All statistical analyses were performed using the Stata 11.0 application (Stata Corp., College Station, TX, USA). A significance level of p<0.05 was accepted.
3. Results
In the whole sample (n = 2333) the participants were slightly predominantly female, with a mean age of 43.3 years (95 % confidence interval [CI]: 43.2- 43.4), self-identified as white, married and of Germanic culture. Most of the respondents belonged to the middle socio-economic status, had an elementary education and had some form of employment. In terms of lifestyle, most were sufficiently active, reported low amounts of alcohol consumption and had never smoked. Details of the participant characteristics are shown in Table 1.
Table 1.
Study participants by age group, SHIP-Brazil, 2014-2018.
| Variables | Age group |
|||
|---|---|---|---|---|
| Total (%) | 20 a 59 (%) | 60 a 79 (%) | p | |
| Sex (n = 2333) | ||||
| Male | 49.1 | 49.5 | 46.1 | <0.001 |
| Female | 50.9 | 50.5 | 53.9 | |
| Marital status (n = 2329) | ||||
| Single/Separated/Widow | 28.4 | 29.0 | 25.1 | 0.0539 |
| Married | 71.6 | 71.0 | 74.9 | |
| Germanic culture (n = 2328) | ||||
| No | 38.0 | 42.0 | 15.7 | <0.001 |
| Yes | 62.0 | 58.0 | 84.3 | |
| Race/color self-declared (n = 2326) | ||||
| Not white | 8.6 | 9.4 | 4.0 | <0.001 |
| White | 91.4 | 90.6 | 96.0 | |
| Education in years (n = 2265) | ||||
| 12 and more | 18.8 | 21.7 | 3.1 | <0.001 |
| 9 to 11 | 34.9 | 40.2 | 5.4 | |
| 0 to 8 | 46.3 | 38.1 | 91.5 | |
| Working (n = 2323) | ||||
| No | 34.6 | 24.9 | 89.4 | <0.001 |
| Yes | 65.4 | 75.1 | 10.6 | |
| Physical activity (n = 2047) | ||||
| Sufficiently Active | 67.1 | 67.6 | 64.2 | 0.151 |
| Insufficiently active | 32.9 | 32.4 | 35.8 | |
| Alcohol consumption (n = 2318) | ||||
| Moderate/High/Severe | 35.2 | 38.4 | 17.7 | <0.001 |
| Low risk | 64.8 | 61.6 | 82.3 | |
| Smoking (n = 2326) | ||||
| Never smoke | 69.7 | 72.2 | 55.7 | <0.001 |
| Ex-smoker | 19.9 | 17.9 | 31.1 | |
| Current smoker | 10.4 | 9.9 | 13.2 | |
| Hypertension (self-reported) (n = 2047) | ||||
| No | 75.4 | 80.7 | 46.0 | <0.001 |
| Yes | 24.6 | 19.3 | 54.0 | |
| Diabetes (self-reported) (n = 2118) | ||||
| No | 94.2 | 96.6 | 80.5 | <0.001 |
| Yes | 5.8 | 3.4 | 19.5 | |
| History of Depression (self-reported) (n = 2324) | ||||
| No | 81.9 | 83.9 | 70.7 | <0.001 |
| Yes | 18.1 | 16.1 | 29.3 | |
| Current depression PHQ-9 (n = 1908) | ||||
| No | 92.9 | 93.8 | 87.7 | <0.001 |
| Yes | 7.1 | 6.2 | 12.3 | |
| Nutritional status | ||||
| Eutrophic | 31.0 | 32.2 | 24.5 | |
| Overweight | 38.3 | 34.6 | 57.9 | |
| Obesity | 30.7 | 33.2 | 17.6 | <0.001 |
| Multimorbidity (n = 1887) | ||||
| No illness | 23.3 | 26.5 | 5.2 | <0.001 |
| One disease | 24.8 | 27.3 | 10.0 | |
| Two or more diseases | 51.9 | 46.2 | 84.8 | |
| Polypharmacy (n = 2238) | ||||
| 0 a 4 | 83.5 | 88.6 | 54.7 | <0.001 |
| 5 and/or more | 16.5 | 11.4 | 45.3 | |
| Self-perception of health (n = 2322) | ||||
| Very good | 61.8 | 65.4 | 41.9 | <0.001 |
| Fair | 32.0 | 29.0 | 48.6 | |
| Bad/very bad | 6.2 | 5.6 | 9.5 | |
While among the older adults aged 60 to 79, there was a higher proportion of females, of Germanic culture, and who had only completed elementary school, among the participants aged 20-59 years, there was a higher proportion with a job. There was a higher proportion of medical diagnoses of hypertension, depression and type 2 diabetes, as well as those reporting two or more conditions, taking five or more medications, and having a worse perception of their health among participants aged 60-79 years.
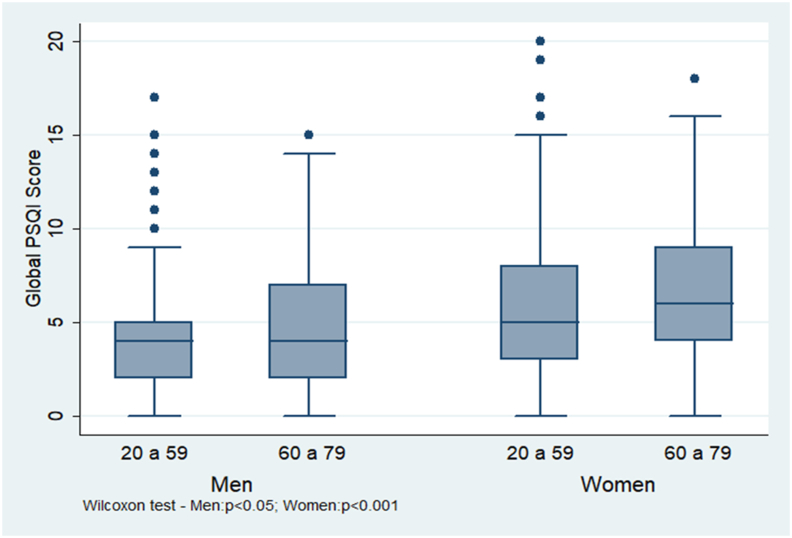
The internal consistency of the PSQI in this study was α = 0.68. The median total PSQI score was 4 (IQR = 3-7). In men, the total PSQI score differed between adults (4, IQR = 2-5) and older adults (4, IQR = 2-7) (p = 0.0462). In women, the median PSQI total score was 5 (IQR = 3-8) in the 20-59 age group and 6 (IQR = 4-9) in the 60-79 age group (p<0.0001). Details of the Global Sleep Quality Score by sex and age group are shown in Fig. 1.
Fig. 1.
“Pittsburgh Sleep Quality Index” Sleep Quality Global Score by sex and age group, SHIP-Brazil, 2014-2018 (n = 2333).
Very bad subjective sleep quality was higher in people aged 20 to 59 years (4.3 % vs 1.6 %, p<0.0001) and in women (25.0 % vs 18.1 %, p<0.0001). Sleep latency (more than 60 min) was higher in older people (14.5 % vs 9.5 %, p<0.0001) and in women (13.8 % vs 6.7 %, p<0.0001). Sleep duration less than 6 h was more frequent among people aged 20 to 59 years (13.3 % vs 10.0 %, p<0.0001). Sleep efficiency less than 85 % was more common in women (10.5 % vs 4.7 %, p<0.0001). People aged 60 to 79 years (26.7 % vs 15.0 %, p<0.0001) and women (22.0 % vs 11.3 %, p<0.0001) had sleep disturbances more than once a week. Older adults (33.8 % vs 8.8 %, p<0.0001) and women (16.7 % vs 8.4 %, p<0.0001) used more sleeping medication (three times a week or more). Finally, women reported more daytime dysfunction (16.7 % vs 10.1 %, p<0.0001). There was no difference in sleep efficiency and daytime dysfunction between adults and the older adults. Sleep duration did not differ between the sexes. More details about the seven components of PSQI are available in the Supplementary Material.
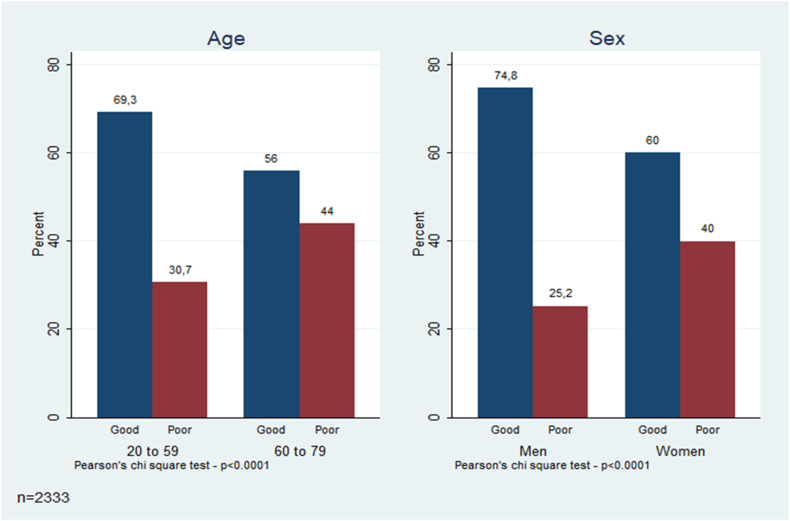
The frequency of poor sleep quality was 32.7 % (95%CI 30.7-34.4). Poor quality was higher in people aged 60-79 years (44.0 % vs 30.7 %, p<0.0001) and in women (40.0 % vs 25.2 %, p<0.0001) as showed on Fig. 2.
Fig. 2.
“Prevalence of Poor Sleep Quality by age group and sex, SHIP-Brazil, 2014-2018 (n = 2333).
Table 2 shows the prevalence of poor sleep quality and associated factors.
Table 2.
Prevalence of poor sleep quality and associated factors, SHIP-Brazil, 2014-2018.
| Variables | Prevalence |
Crude PR |
Adjusted PR |
||
|---|---|---|---|---|---|
| PR (95%CI) | p | PR (95%CI) | p | ||
| Sex | |||||
| Male | 25.2 | 1 | <0.001 | 1 | <0.001 |
| Female | 40.0 | 1.6 (1.4-1.8) | 1.3 (1.1-1.5) | ||
| Age | |||||
| 20-59 | 30.7 | 1 | <0.001 | ||
| 60-79 | 44.0 | 1.43 (1.3-1.6) | |||
| Marital status | |||||
| Single/separated/widow | 34.3 | 1 | 0.343 | ||
| Married | 32.0 | 0.9 (0.8-1.0) | |||
| Germanic culture | |||||
| No | 36.9 | 1 | 1 | <0.001 | |
| Yes | 30.1 | 0.8 (0.7-0.9) | 0.002 | 0.8 (0.7-0.9) | |
| Race/Color(self-declared) | |||||
| White | 32.0 | 1 | 0.044 | ||
| Non-white | 39.9 | 1.2 (1.0-1.5) | |||
| Education (in Years) | |||||
| 12 and more | 28.3 | 1 | 1 | ||
| 9 to 11 | 26.5 | 0.9 (0.7-1.2) | 0.593 | 0.8 (0.6-1.0) | 0.046 |
| 0 to 8 | 39.1 | 1.4 (1.1-1.7) | 0.002 | 0.7 (0.6-1.0) | 0.025 |
| Working | |||||
| No | 43.1 | 1 | <0.001 | 1 | 0.002 |
| Yes | 27.2 | 0.6 (0.5-0.7) | 0.8 (0.7-0.9) | ||
| Physical Activity | |||||
| Sufficiently active | 31.0 | 1 | 0.062 | ||
| Insufficiently active | 35.2 | 1.2 (1.0-1.3) | |||
| Alcohol consumption | |||||
| Moderate/High | 27.0 | 1 | <0.001 | ||
| Low risk | 36.0 | 1.3 (1.1-1.6) | |||
| Smoking | |||||
| Never smoke | 29.5 | 1 | 1 | ||
| Ex-smoker | 39.2 | 1.3 (1.1-1.5) | <0.001 | 1.2 (1.0-1.4) | 0.014 |
| Current smoker | 41.9 | 1.4 (1.2-1.7) | <0.001 | 1.3 (1.1-1.5) | 0.006 |
| Hypertension (self-reported) | |||||
| No | 28.1 | 1 | <0.001 | ||
| Yes | 43.8 | 1.6 (1.4-1.8) | |||
| Diabetes (self-reported) | |||||
| No | 31.4 | 1 | <0.001 | ||
| Yes | 45.4 | 1.5 (1.2-1.7) | |||
| Depression (self-reported) | |||||
| No | 26.0 | 1 | <0.001 | 1 | <0.001 |
| Yes | 63.0 | 2.4 (2.2-2.7) | 1.5 (1.3-1.7) | ||
| Nutritional status | |||||
| Eutrophic | 28.1 | 1 | 0.066 | ||
| Overweight | 33.3 | 1.2 (1.0-1.4) | |||
| Obesity | 35.5 | 1.3 (1.1-1.5) | 0.014 | ||
| Multimorbidity | |||||
| No illness | 16.7 | 1 | |||
| One disease | 25.4 | 1.5 (1.1-2.1) | 0.014 | ||
| Two or more diseases | 41.2 | 2.5 (1.8-3.2) | <0.001 | ||
| Polypharmacy | |||||
| 0 a 4 | 27.8 | 1 | <0.001 | 1 | 0.001 |
| 5 and/or more | 57.8 | 2.1 (1.9-2.3) | 1.2 (1.1-1.4) | ||
| Self-perception of health | |||||
| Very good | 19.4 | 1 | <0.001 | 1 | |
| Fair | 49.7 | 2.6 (2.2-2.9) | 2.1 (1.8-2.4) | <0.001 | |
| Bad/very bad | 78.1 | 4.0 (3.5-4.7) | 2.6 (2.1-3.1) | <0.001 | |
Multivariate analysis showed that women (PR = 1.3; 95 % CI 1.1-1.5), former (PR = 1.2; 95 % CI 1.0-1.4) or current smokers (PR = 1.3; 95 % CI 1.1-1.5), those with depression (PR = 1.5; 95 % CI 1.3-1.7), taking five or more medications (PR = 1.2; 95 % CI 1.1-1.4), and having a fair (PR = 2.1; 95 % CI 1.8-2.4) or poor/very poor (PR = 2.6; 95 % CI 2.1-3.1) self-perceived health were risk factors for poor sleep quality. However, people from a Germanic culture (PR = 0.8; 95 % CI 0.7-0.9), with a medium (PR = 0.8; 95 % CI 0.6-1.0) or primary school education (PR = 0.7; 95 % CI 0.6-1.0) or being at work (PR = 0.8; 95 % CI 0.7-0.9) have a lower risk of poor sleep quality.
4. Discussion
Approximately one-third of the participants experiences poor sleep quality. Women and individuals aged 60 to 79 reported taking longer to fall asleep, experiencing more sleep disorders, and using more sleep medication. Women also reported worse sleep efficiency and a higher frequency of daytime dysfunctions. Individuals aged 20 to 59 reported shorter sleep duration and poorer subjective sleep quality. The study found that poor sleep quality was associated with being female, smoking, self-reported depression, taking five or more medications, and poor self-perceived health. On the other hand, better sleep quality was associated with having a job, being from a Germanic culture, and having less schooling.
The study found that 32.7 % of participants reported poor sleep quality. A nationwide study of 2635 adults of both sexes in Brazil found a higher prevalence of poor sleep quality of 65.5 % and an average PSQI global score of 7.3 [8]. In a medium-sized city in central Brazil, the prevalence was 57.4 % [1]. In large cities in the Brazilian southeast, the prevalence rate ranges from 29.1 % in Campinas [22] to 46.7 % in São Paulo [23]. The prevalence of poor sleep quality in European countries were reported to be 38 % in Germany [24], 38.2 % in Spain [25], and 72.9 % in Finland [26]. The prevalence in this study was comparable to that found in Germany, despite differences in geography and population.
The study found that women experienced lower overall and subjective sleep quality, longer sleep latency, lower sleep efficiency, and higher frequencies of sleep medication use, daytime dysfunctions, and sleep disorders. The prevalence of poor sleep quality was higher in women (40 %, PR = 1.3; 95 % CI 1.1-1.5), which is consistent with findings from other studies conducted in Brazil [7,22]. A recent nationwide study conducted by Araújo et al. [7] found that 41.8 % of women experienced poor sleep quality. Hormonal and physiological changes common during pregnancy and menopause may lead to greater changes in sleep patterns [27]. According to Xu et al. [28], menopausal women experienced poorer sleep quality than non-menopausal women. A study has revealed a significant and positive association between dehydroepiandrosterone and awakening after sleep onset in women [29]. Furthermore, it has been found that women have a higher prevalence of multimorbidity and report experiencing more mental health issues related to poor sleep quality, including anxiety, depression, and stress [30]. In addition to physiological factors, women may also face the burden of caring for children and family members who are in poor health. This can lead to an accumulation of social roles and result in a professional and domestic overload, which may interfere with their quality of sleep [22].
We found that older age was associated with poorer overall sleep quality, longer sleep latency, and higher frequency of sleep disorders and use of sleep medications. One study shows a strong association between sleep quality and age [28]. In Spain, a study demonstrated that perceptions of sleep quality did not differ significantly with increasing age, despite worsening sleep latency and efficiency and an increase in the prevalence of sleep disorders [25]. In Brazil, older adults reported decreased sleep duration, sleep latency, difficulty falling asleep (with recurrence more than three times per week), and moderate or severe discomfort with daily activities [31]. Physiological changes during ageing lead to changes in sleep architecture, meaning that sleep is shorter, more superficial, fragmented and of poorer quality [1,10].
Working seems to be a protective factor against poor sleep quality, in line with the results of other studies [22,[32], [33], [34]]. Sleep in unemployed people aged 41-64 years is less efficient, more fragmented and shifted towards the end of the night [32]. In Japan, unemployed men (OR = 2.5; 95%CI 1.8-3.4) or those unable to work (OR = 2.1; 95%CI 1.2-3.7) had a higher risk of insomnia-related symptoms, while for unemployed women the OR was 1.9 (95%CI 1.5-2.5) [34]. On the other hand, employed people had a lower risk of reporting poor sleep quality among men (OR = 0.49; 95%CI 0.33-0.68) and women (OR = 0.48; 95%CI 0.39-0.63) in China [33]. Having a job may affect the regularity of daily activities and sleep, and may represent financial security and better socioeconomic conditions, reducing negative effects on sleep quality.
German culture, used as a proxy for German ancestry, was associated with a lower risk of poor sleep quality. Systematic reviews of twin studies have shown that sleep quality and duration can be explained, at least in part, by genetics [35,36]. However, studies have found that Latinos sleep less and worse than Caucasians, suggesting that not only genetics, but also social position and culture can affect sleep quality and duration [[37], [38], [39]]. Pomerode was founded around 1860 by immigrants from Pomerania. Their descendants are the most representative group, with a social network closer to these inhabitants. Although ancestry may play a role in sleep quality, socio-economic factors and the fact that the descendants of the Germans have lived in the same region for a long time may contribute to better sleep quality compared to more recent immigrant groups.
Poor sleep quality was found in former and current smokers. A systematic review of 19 studies from 10 countries (n = 15,245) found that tobacco smoking impairs sleep quality, duration, and maintenance, more so in women, heavy smokers, and those with nicotine dependence [40]. Kim et al. [41] found that smoking causes oedema and thickening of the airway mucosa, resulting in upper airway narrowing, which is a potential trigger for sleep disturbance and a risk factor for moderate or severe obstructive sleep apnoea syndrome. In addition, nicotine is a stimulant responsible for changes in sleep architecture, such as its fragmentation and reduced efficiency [7].
In addition to socioeconomic and lifestyle factors, clinical conditions may influence sleep quality. Poor sleep quality was associated with two or more conditions. This association is consistent with population-based studies in Japan [42], China [43], Peru [30] and Brazil [22]. Smith et al. [39] found that pain (24 %), anxiety (21 %), depression (11.2 %) and stress (10.4 %) explained most of the association between multimorbidity and sleep disorders in a cross-sectional study of 46 low- and middle-income countries. However, despite finding a significant association between multimorbidity and sleep quality, the results of the studies vary because they use different methods to collect data and define cut-off points. It remains unclear how the quality of health care might minimize this negative association.
In our study, depression was significantly associated with poor sleep quality. The presence and frequency of sleep disturbances are criteria for the diagnosis of depression (DSM-5). Poor sleep quality was significantly present in individuals with common mental disorders (PR = 2.70; 95 % CI 2.38–3.08) [22]. Byrne et al. [44] found a 2.3 times higher risk of being diagnosed with depression in people with sleep disorders. Another study found a negative association between sleep quality and depressive symptoms [24]. It is important to note that people being treated for depression use mood medications with different effects (sedatives or stimulants), which can reduce sleep onset latency and wakefulness [45].
We found that using five or more medications was associated with a higher prevalence of poor sleep quality. A Spanish study found that participants who were more likely to use five or more medications did not sleep between seven and 8 h per night [46]. A direct relationship was found between the number of medications, the use of sleeping pills and the number of health consultations [9,47]. Women and older adults used to have a higher number of medical consultations and more regular follow-ups and are therefore more likely to use sleeping pills chronically, which negatively affects sleep quality.
People who perceived their health as fair or poor/very poor had twice the prevalence of poor sleep quality. Poor self-perceived health has been associated with poor sleep quality worldwide [22,27,[48], [49], [50]]. This association appears to be bidirectional. Insomnia and poor sleep health were independent factors associated with poor self-perceived health [51,52]. Further studies are needed to better understand the mechanisms relating self-perceived health to sleep quality.
Our findings confirm that some groups (such as women and older adults) and some clinical conditions (such as smokers, people with depression, polypharmacy and poor self-perceived health) were associated with poor sleep quality and should be prioritised by the public health system. Brazil has one of the largest public health systems in the world with universal coverage based on family health strategies. General practitioners in these primary care teams should focus preventive efforts on these groups such as promoting educational programs on sleep hygiene and rational use of medication.
As this is a cross-sectional study, it is not possible to investigate causal relationships between the variables studied and sleep quality, such as the direction of the association between self-perceived health and poor sleep quality. In addition, sleep quality was estimated based on participants' self-reports rather than objective measures such as actigraphy or polysomnography [53]. Self-reported data in interviews may be subject to memory bias. However, the practice of using previously validated questionnaires (such as the one used in this study) has been widely used in epidemiological studies around the world because of their ease of use and low cost. In this study, the PSQI showed good internal consistency, like other population studies [47]. However, the use of different instruments limits the comparability of study results in different contexts. This problem may explain the wide range of prevalence observed between Brazilian studies.
5. Conclusions
Poor sleep quality affected about one third of participants and was more common among women and older adults. Sociocultural and lifestyle factors (not working, not belonging to the German culture and smoking) and health conditions (history of depression, use of 5 or more medications and poor self-perceived health) are the main risk factors for poor sleep quality in a city of German descendants in southern Brazil. A longitudinal approach may help to clarify these associations.
CRediT authorship contribution statement
Ernani Tiaraju de Santa Helena: Writing – review & editing, Writing – original draft, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. Nicolas Boeira Machado: Writing – review & editing, Writing – original draft, Formal analysis, Conceptualization. Rafael Tadao Sakae: Writing – review & editing, Writing – original draft, Formal analysis, Conceptualization. Clovis Arlindo de Sousa: Writing – review & editing, Supervision, Project administration, Investigation, Formal analysis, Conceptualization. Carlos Roberto de Oliveira Nunes: Writing – review & editing, Supervision, Investigation, Conceptualization. Henry Völzke: Writing – review & editing, Conceptualization. Ralf Ewert: Writing – review & editing, Conceptualization. Marcello Ricardo Paulista Markus: Writing – review & editing, Supervision, Formal analysis, Conceptualization.
Funding
SHIP-Brazil was supported by Foundation for the Support of Scientific and Technological Research of the State of Santa Catarina (FAPESC) (Call PPSUS 003/2012), the University of Blumenau, and the City of Pomerode.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Ralf Ewert reports a relationship with Lungpacer Medical Inc, OMT, AOP Orphan, AstraZeneca, Boehringer Ingelheim, Jassen Pharmaceutical, Berlin Chemie that includes: consulting or advisory and speaking and lecture fees. If there are other authors, they declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We thank colleagues from Graduate Program of Public Health of the University of Blumenau and the Institute for Community Medicine of the University Medicine Greifswald that help us with knowledge and experience. We also thank all health workers and study participants and families.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.sleepx.2024.100133.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Simões N.D., Monteiro L.H.B., Lucchese R., De Amorim T.A., Denardi T.C., Vera I., et al. Quality and sleep duration among public health network users. Acta Paul Enferm. 2019;32:530–537. https://www.scielo.br/j/ape/a/QKqNHBBqVVdNCwSSn3kJDZm/?lang=en [Internet] [cited 2024 Mar 12] [Google Scholar]
- 2.Hublin C., Partinen M., Koskenvuo M., Kaprio J. Heritability and mortality risk of insomnia-related symptoms: a genetic epidemiologic study in a population-based twin cohort. Sleep. 2011;34:957. doi: 10.5665/SLEEP.1136. [Internet] [cited 2024 Mar 12]. Available from:/pmc/articles/PMC3119838/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Troxel W.M., Buysse D.J., Matthews K.A., Kip K.E., Strollo P.J., Hall M., et al. Sleep symptoms predict the development of the metabolic syndrome. Sleep [Internet] 2010;33:1633. doi: 10.1093/sleep/33.12.1633. [cited 2024 Mar 12]. Available from:/pmc/articles/PMC2982733/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lo K., Woo B., Wong M., Tam W. Subjective sleep quality, blood pressure, and hypertension: a meta-analysis. J Clin Hypertens. 2018;20:592–605. doi: 10.1111/jch.13220. https://pubmed.ncbi.nlm.nih.gov/29457339/ [Internet] [cited 2024 Mar 12] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baglioni C., Battagliese G., Feige B., Spiegelhalder K., Nissen C., Voderholzer U., et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135:10–19. doi: 10.1016/j.jad.2011.01.011. https://pubmed.ncbi.nlm.nih.gov/21300408/ [Internet] [cited 2024 Mar 12] [DOI] [PubMed] [Google Scholar]
- 6.Simões A.D., Machado Júnior Á.N., Oliveira AB. da S., Pereira A.C.P., Figueiredo BQ de, Pinheiro FE. da S., et al. Principais distúrbios do sono e seus impactos na qualidade de vida humana: uma revisão sistemática de literatura. Res, Soc Dev. 2022;11 [Google Scholar]
- 7.Araújo M.F.S., de Souza T.A., de Almeida Medeiros A., de Souza J.C., Barbosa I.R. Factors associated with sleep problems and sleeping pill use in Brazilians. Rev Saude Pub [Internet] 2022;56:68. doi: 10.11606/s1518-8787.2022056004088. https://www.scielo.br/j/rsp/a/cVZKrdGVd9kyvCxgB67TSjt/ [cited 2024 Mar 12] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Drager L.F., Pachito D.V., Morihisa R., Carvalho P., Lobao A., Poyares D. Sleep quality in the Brazilian general population: a cross-sectional study. Sleep Epidemiol. 2022;2 [Google Scholar]
- 9.Seixas B.V. Prevalence and factors associated with use of sleeping pills among older adults in Brazil. Int J Pharm Pract [Internet] 2021;29:235–244. doi: 10.1093/ijpp/riab003. https://pubmed.ncbi.nlm.nih.gov/33793814/ [cited 2024 Mar 12] [DOI] [PubMed] [Google Scholar]
- 10.Brewster G.S., Riegel B., Gehrman P.R. Insomnia in the older adult. Sleep Med Clin [Internet] 2018;13:13–19. doi: 10.1016/j.jsmc.2017.09.002. https://pubmed.ncbi.nlm.nih.gov/29412980/ [cited 2024 Mar 12] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Araújo M.F.S., de Souza T.A., de Almeida Medeiros A., de Souza J.C., Barbosa I.R. Factors associated with sleep problems and sleeping pill use in Brazilians. Rev Saude Pub [Internet] 2022;56:68. doi: 10.11606/s1518-8787.2022056004088. https://www.scielo.br/j/rsp/a/cVZKrdGVd9kyvCxgB67TSjt/ [cited 2024 Mar 12] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Souza A.M., Resende S.S., de Sousa T.N., de Brito C.F.A. A systematic scoping review of the genetic ancestry of the brazilian population. Genet Mol Biol. Braz J Genet. 2019:495–508. doi: 10.1590/1678-4685-GMB-2018-0076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kondo J., Tempaku P.F., D'Almeida V., Kakazu V.A., Andersen M.L., Tufik S., et al. Sleep patterns according to genetically determined ethnicity in the population of São Paulo, Brazil. Sleep Med. 2024;113:242–248. doi: 10.1016/j.sleep.2023.11.036. [DOI] [PubMed] [Google Scholar]
- 14.Santa Helena ET., Sousa C.A., Silveira J.L.G.C., Nunes C.R.O., Azevedo L.C., Nilson L.G., et al. Study of Health in Pomerode (SHIP-Brazil): aims, methodological issues and descriptive results. Scielo Preprints. 2023 doi: 10.1590/SciELOPreprints.7276. [Internet] [DOI] [Google Scholar]
- 15.Buysse D.J., Reynolds C.F., Monk T.H., Berman S.R., Kupfer D.J. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatr Res [Internet] 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. https://pubmed.ncbi.nlm.nih.gov/2748771/ [cited 2024 Mar 12] [DOI] [PubMed] [Google Scholar]
- 16.Maltzahn P. The German language as a defining feature of ethnic identity in Pomerode. Pandaemonium Ger. 2017;21:113–135. [Google Scholar]
- 17.IBGE. Censo. 2010. https://censo2010.ibge.gov.br/coleta/questionarios.html Questionários. [Internet]. 2010 [cited 2013 Sep 5]. Available from:
- 18.Matsudo S., Araujo T., Matsudo V., Andrade D. Questionário Internacional de Atividade Física (IPAQ): estudo de validade e reprodutibilidade no Brasil. Rev Bras Ativ Fis Saude. 2001;6:5–18. [Google Scholar]
- 19.Meneses-Gaya C., Zuardi A.W., Loureiro S.R., Crippa J.A.S. Alcohol Use Disorders Identification Test (AUDIT): an updated systematic review of psychometric properties. Psychol Neurosci. 2009;2:83–97. [Google Scholar]
- 20.WHO Expert Committee on Physical Status . 1995. Physical Status: the use and interpretation of anthropometry. Geneva. [PubMed] [Google Scholar]
- 21.Nohr E.A., Liew Z. How to investigate and adjust for selection bias in cohort studies. Acta Obstet Gynecol Scand. 2018;97:407–416. doi: 10.1111/aogs.13319. [DOI] [PubMed] [Google Scholar]
- 22.Barros M.B. de A., Lima M.G., Ceolim M.F., Zancanella E., Cardoso T.A.M. de O. Quality of sleep, health and well-being in a population-based study. Rev Saude Pub [Internet] 2019;53:82. doi: 10.11606/s1518-8787.2019053001067. https://www.scielo.br/j/rsp/a/tsYyRNmY7Lj9tLLDnCLMg3b/abstract/?lang=en [cited 2024 Mar 12] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zanuto A.C.E., De Limai C.S.M., De Araújo G.R., Da Silva P.E., Anzolin C.C., Araujo Y.C.M., et al. Sleep disturbances in adults in a city of Sao Paulo state. Rev Brasil de Epidemiol [Internet] 2015;18:42–53. doi: 10.1590/1980-5497201500010004. https://www.scielo.br/j/rbepid/a/vSP6hXD67sdWD3xjkNQL8YH/?lang=en [cited 2024 Mar 12] [DOI] [PubMed] [Google Scholar]
- 24.Lacruz M.E., Schmidt-Pokrzywniak A., Dragano N., Moebus S., Deutrich S.E., Möhlenkamp S., et al. Depressive symptoms, life satisfaction and prevalence of sleep disturbances in the general population of Germany: results from the Heinz Nixdorf Recall study. BMJ Open. 2016;6(1) doi: 10.1136/bmjopen-2015-007919. https://pubmed.ncbi.nlm.nih.gov/26729376/ [Internet] [cited 2024 Mar 12]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Madrid-Valero J.J., Martínez-Selva J.M., Ribeiro do Couto B., Sánchez-Romera J.F., Ordoñana J.R. Age and gender effects on the prevalence of poor sleep quality in the adult population. Gac Sanit [Internet] 2017;31:18–22. doi: 10.1016/j.gaceta.2016.05.013. https://pubmed.ncbi.nlm.nih.gov/27474487/ [cited 2024 Mar 12] [DOI] [PubMed] [Google Scholar]
- 26.Aydinlar E.I., Dikmen P.Y., Kosak S., Kocaman A.S. OnabotulinumtoxinA effectiveness on chronic migraine, negative emotional states and sleep quality: a single-center prospective cohort study. J Headache Pain [Internet] 2017;18 doi: 10.1186/s10194-017-0723-4. [cited 2024 Mar 12]. Available from:/pmc/articles/PMC5315653/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baker F.C., Wolfson A.R., Lee K.A. Association of sociodemographic, lifestyle, and health factors with sleep quality and daytime sleepiness in women: findings from the 2007 National Sleep Foundation “Sleep in America Poll.”. J Womens Health (Larchmt) 2009;18:841–849. doi: 10.1089/jwh.2008.0986. https://pubmed.ncbi.nlm.nih.gov/19514826/ [Internet] [cited 2024 Mar 12] [DOI] [PubMed] [Google Scholar]
- 28.Xu M., Bélanger L., Ivers H., Guay B., Zhang J., Morin C.M. Comparison of subjective and objective sleep quality in menopausal and non-menopausal women with insomnia. Sleep Med [Internet] 2011;12:65–69. doi: 10.1016/j.sleep.2010.09.003. https://pubmed.ncbi.nlm.nih.gov/21147026/ [cited 2024 Mar 12] [DOI] [PubMed] [Google Scholar]
- 29.Kische H., Ewert R., Fietze I., Gross S., Wallaschofski H., Völzke H., et al. Sex hormones and sleep in men and women from the general population: a cross-sectional observational study. J Clin Endocrinol Metab [Internet] 2016;101:3968–3977. doi: 10.1210/jc.2016-1832. https://pubmed.ncbi.nlm.nih.gov/27403929/ [cited 2024 Mar 12] [DOI] [PubMed] [Google Scholar]
- 30.Méndez-Flores J.J., Marroquín-Cosar R.E., Bernabé-Ortiz A. Multimorbidity and sleep patterns among adults in a Peruvian semi-urban area. Sleep Sci [Internet] 2023;16:51–58. doi: 10.1055/s-0043-1767755. https://pubmed.ncbi.nlm.nih.gov/37151763/ [cited 2024 Mar 12] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mugeiro M.J.C., Martins R.M.L. [Viseu]: Instituto Politécnico de Viseu; 2011. Qualidade do sono nos idosos [internet]http://hdl.handle.net/10400.19/1658 [cited 2024 Mar 12]. Available from: [Google Scholar]
- 32.Greissl S., Mergl R., Sander C., Hensch T., Engel C., Hegerl U. Is unemployment associated with inefficient sleep habits? A cohort study using objective sleep measurements. J Sleep Res [Internet] 2022;31(3) doi: 10.1111/jsr.13516. https://pubmed.ncbi.nlm.nih.gov/34773314/ [cited 2024 Mar 12]. Available from: [DOI] [PubMed] [Google Scholar]
- 33.Wu W., Wang W., Dong Z., Xie Y., Gu Y., Zhang Y., et al. Sleep quality and its associated factors among low-income adults in a rural area of China: a population-based study. Int J Environ Res Public Health [Internet] 2018;15 doi: 10.3390/ijerph15092055. https://pubmed.ncbi.nlm.nih.gov/30235864/ [cited 2024 Mar 12] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Maeda M., Filomeno R., Kawata Y., Sato T., Maruyama K., Wada H., et al. Association between unemployment and insomnia-related symptoms based on the Comprehensive Survey of Living Conditions: a large cross-sectional Japanese population survey. Ind Health [Internet] 2019;57:701. doi: 10.2486/indhealth.2018-0031. [cited 2024 Mar 12]. Available from:/pmc/articles/PMC6885596/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Madrid-Valero J.J., Rubio-Aparicio M., Gregory A.M., Sánchez-Meca J., Ordoñana J.R. Twin studies of subjective sleep quality and sleep duration, and their behavioral correlates: systematic review and meta-analysis of heritability estimates. Neurosci Biobehav Rev [Internet] 2020;109:78–89. doi: 10.1016/j.neubiorev.2019.12.028. https://pubmed.ncbi.nlm.nih.gov/31899301/ [cited 2024 Mar 12] [DOI] [PubMed] [Google Scholar]
- 36.Kocevska D., Barclay N.L., Bramer W.M., Gehrman P.R., Van Someren E.J.W. Heritability of sleep duration and quality: a systematic review and meta-analysis. Sleep Med Rev [Internet] 2021;59 doi: 10.1016/j.smrv.2021.101448. https://pubmed.ncbi.nlm.nih.gov/33636423/ [cited 2024 Mar 12] [DOI] [PubMed] [Google Scholar]
- 37.Roncoroni J., Okun M., Hudson A. Systematic review: sleep health in the US Latinx population. Sleep [Internet] 2022;45(7) doi: 10.1093/sleep/zsac092. https://pubmed.ncbi.nlm.nih.gov/35460556/ [cited 2024 Mar 12]. Available from: [DOI] [PubMed] [Google Scholar]
- 38.Aqua J.K., White K., Johnson D.A. A systematic review of acculturation and sleep health among adult immigrants in the United States. Sleep Health [Internet] 2023;9:288–305. doi: 10.1016/j.sleh.2023.01.007. https://pubmed.ncbi.nlm.nih.gov/36849283/ [cited 2024 Mar 12] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Smith J.P., Hardy S.T., Hale L.E., Gazmararian J.A. Racial disparities and sleep among preschool aged children: a systematic review. Sleep Health. 2019;5:49–57. doi: 10.1016/j.sleh.2018.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.da Silva e Silva W.C., Costa N.L., Rodrigues D. da S., da Silva M.L., Cunha K. da C. Sleep quality of adult tobacco users: a systematic review of literature and meta-analysis. Sleep Epidemiol. 2022;2 [Google Scholar]
- 41.Kim K.S., Kim J.H., Park S.Y., Won H.R., Lee H.J., Yang H.S., et al. Smoking induces oropharyngeal narrowing and increases the severity of obstructive sleep apnea syndrome. J Clin Sleep Med [Internet] 2012;8:367. doi: 10.5664/jcsm.2024. [cited 2024 Mar 12]. Available from:/pmc/articles/PMC3407254/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hayashino Y., Yamazaki S., Takegami M., Nakayama T., Sokejima S., Fukuhara S. Association between number of comorbid conditions, depression, and sleep quality using the Pittsburgh Sleep Quality Index: results from a population-based survey. Sleep Med. 2010;11:366–371. doi: 10.1016/j.sleep.2009.05.021. https://pubmed.ncbi.nlm.nih.gov/20219425/ [Internet] [cited 2024 Mar 12] [DOI] [PubMed] [Google Scholar]
- 43.Lin Y., Hu Y., Guo J., Chen M., Xu X., Wen Y., et al. Association between sleep and multimorbidity in Chinese elderly: results from the Chinese longitudinal healthy longevity survey (CLHLS) Sleep Med. 2022;98:1–8. doi: 10.1016/j.sleep.2022.06.007. https://pubmed.ncbi.nlm.nih.gov/35753186/ [Internet] [cited 2024 Mar 12] [DOI] [PubMed] [Google Scholar]
- 44.Byrne E.M., Timmerman A., Wray N.R., Agerbo E. Sleep disorders and risk of incident depression: a population case-control study. Twin Res Hum Genet [Internet] 2019;22:140–146. doi: 10.1017/thg.2019.22. https://pubmed.ncbi.nlm.nih.gov/31203833/ [cited 2024 Mar 12] [DOI] [PubMed] [Google Scholar]
- 45.Buysse D.J., Tyagi S. Principles and Practice of Sleep Medicine; 2017. Clinical pharmacology of other drugs used as hypnotics; pp. 432–445.e7. [Google Scholar]
- 46.Hernández-Aceituno A., Pérez-Tasigchana R.F., Guallar-Castillón P., López-García E., Rodríguez-Artalejo F., Banegas J.R. Combined healthy behaviors and healthcare services use in older adults. Am J Prev Med [Internet] 2017;53:872–881. doi: 10.1016/j.amepre.2017.06.023. https://pubmed.ncbi.nlm.nih.gov/28774549/ [cited 2024 Mar 12] [DOI] [PubMed] [Google Scholar]
- 47.Mollayeva T., Thurairajah P., Burton K., Mollayeva S., Shapiro C.M., Colantonio A. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: a systematic review and meta-analysis. Sleep Med Rev. 2016;25:52–73. doi: 10.1016/j.smrv.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 48.Duncan M.J., Oftedal S., Rebar A.L., Murawski B., Short C.E., Rayward A.T., et al. Patterns of physical activity, sitting time, and sleep in Australian adults: a latent class analysis. Sleep Health [Internet] 2020;6:828–834. doi: 10.1016/j.sleh.2020.04.006. https://pubmed.ncbi.nlm.nih.gov/32819888/ [cited 2024 Mar 12] [DOI] [PubMed] [Google Scholar]
- 49.Leitaru N., Kremers S., Hagberg J., Björklund C., Kwak L. Associations between job-strain, physical activity, health status, and sleep quality among Swedish municipality workers. J Occup Environ Med [Internet] 2019;61(2):E56–60. doi: 10.1097/JOM.0000000000001516. https://pubmed.ncbi.nlm.nih.gov/30540651/ [cited 2024 Mar 12] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Brasil C.H.G., Maia L.C., Caldeira A.P., Brito M.F.S.F., de Pinho L. Positive self-perception of health among non-long-lived and long-lived older adults and associated factors. Cien Saude Colet [Internet] 2021;26:5157–5170. doi: 10.1590/1413-812320212611.3.06352020. https://www.scielo.br/j/csc/a/PFy9tr6WgbCyyyVjBvpgLNp/?lang=en [cited 2024 Mar 12] [DOI] [PubMed] [Google Scholar]
- 51.Dalmases M., Benítez I., Sapiña-Beltran E., Garcia-Codina O., Medina-Bustos A., Escarrabill J., et al. Impact of sleep health on self-perceived health status. Sci Rep. 2019;9:1. doi: 10.1038/s41598-019-43873-5. https://www.nature.com/articles/s41598-019-43873-5 [Internet]. 2019 [cited 2024 Mar 12];9:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Silva J., Truzzi A., Schaustz F., Barros R., Santos M., Laks J. Impact of insomnia on self-perceived health in the elderly. Arq Neuropsiquiatr. 2017;75:277–281. doi: 10.1590/0004-282X20170031. https://pubmed.ncbi.nlm.nih.gov/28591386/ [Internet] [cited 2024 Mar 12] [DOI] [PubMed] [Google Scholar]
- 53.Stubbe B., Penzel T., Fietze I., Obst A., Garcia C., Zim-Mermann S., et al. Polysomnography in a large population based study-the study of health in pomerania protocol. J Sleep Disord Manag. 2016;2:10. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.