Abstract
Background
Dental extraction is the most common oral surgery, but it leads to the remodelling of the socket, such that an implant is required for repair. We performed meta-analysis to determine whether leucocyte- and platelet-rich fibrin (L-PRF) improves dental extraction.
Material and Methods
Following a search of Scopus, Web of science, ProQuest and PubMed, six relevant studies were included (239 patients treated with L-PRF after dental extraction).
Results
The results provide higher percentage of bone formation after dental extraction in L-PRF implant patients with a mean difference of -13.16 (-15.89, -10.43) than control. Socket filling and horizontal width were also higher in the L-PRF implant group. A sub-group meta-analysis showed a significantly higher healing index 7 and 14 days after dental extraction in the L-PRF-treated group. The VAS score for pain stimuli was lower in the L-PRF group with a mean difference of 1.26 (1.00, 1.51) than control group; the difference in the heterogeneity of the studies was significant.
Conclusions
These results show that L-PRF prevents ridge formation by improving the percentage of bone formation and socket width (improved horizontal width and socket filling). In such patients, the healing index was higher and the VAS score for pain stimuli lower than in the control group.
Key words:Dental extraction, L-PRF, socket filling, healing index.
Introduction
Following tooth extraction, the socket undergoes remodelling such that repair treatment requires an implant (1). Clinical studies that have examined the changes in the soft and hard tissues after tooth extraction have reported a reduction of bone (2) and thus a delay in the healing process (3). Post-extraction bone loss includes a reduction of the blood supply (4) and is aggravated by factors such as systemic diseases, smoking status, flap elevation, morphology of the socket and extraction of the neighbouring teeth (5). Pain intensity and healing, and thus the adequate use of analgesic drugs, are also important factors in ridge prevention following tooth extraction (6). However, while several techniques have been used to reduce pain, healing time and loss of bone after tooth extraction (7), none are particularly effective, either clinically or with respect to their cost.
L-PRF, derived from platelet concentrate and leucocytes, has been used to stimulate bone growth (8). This second-generation preparation is free of the limitations of the first-generation product and is both inexpensive and easy to obtain, without the need for biochemical handling. L-PRF induces protein synthesis and growth factor release, and promotes rapid cicatricial tissue remodelling, wound healing, cell proliferation and neovascularisation (9). However, its effects on bone formation is unclear (10); both ridge prevention and no effect on bone loss have been reported (11). Therefore, here, we performed systematic review and meta-analysis to determine effect of L-PRF on dental extraction.
Material and Methods
This study follows the guideline of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) for conducting and reporting meta-analyses and systematic reviews. The protocol of this study was registered with PROSPERO (CRD42022357723).
- Search Strategy
Databases of Scopus, Web of Science, ProQuest and PubMed were used to do detailed literature search. The following broad terms were searched with combinations of keywords: ridge prevention, healing index, oral implant with L-PRF.
All records from different databases were exported to Excel in CSV file format. After all four CSV file records from the different databases had been compiled, duplicate records were removed. All remaining records were screened by examining the titles and Abstracts of each one and removing insignificant records based on the criteria of inclusion and exclusion of our study. The remaining records were subjected to a full-text review before their inclusion in the analysis.
- Data extraction and risk of bias
Informations like first author, year of publication, country name, number of patients, mean age, proportion of males and females, socket width (L-PRF/control), healing index (L-PRF/control), VAS (L-PRF/control), conclusion and references were extracted from all the selected articles (12-17).
The risk of bias were assessed by 2 reviewers from all included studies, using Cochrane Collaboration RoB 2. A randomised controlled trial (RCT) checklist was used to evaluate all of the included studies as per directions. If all criteria were met, the study was rated as having a low risk of bias considered when all the criteria met; risk of bias considered high, in case of one or more criteria didn’t meet; unclear considered based on unclear domain more than one. Moreover third reviewer consult, if there is disagreement between the first two reviewer.
- Selection criteria
Studies with the following features were included: comparison of ridge prevention, i.e., socket dimension, healing index and Visual Analogue Scale (VAS); randomised clinical trial including split-mouth studies; clinical studies. Studies with the following features were excluded: comparison of pain sensation using different scales; patients with comorbidities; pre-clinical studies. In all, on inclusion criteria 239 articles were excluded. Ultimately, six full text articles were included in the meta-analysis was performed on six full test.
- Statistical analysis
Results are represented as means±SD. A statistical evaluation indicated significant heterogeneity in effect size, and thus a random effects model was used. Differences in outcome between controls and an L-PRF group were represented using a forest plot, and a Q test and I2 index were used to assess statistical heterogeneity, expressed as a percentage of the variation (where I2=75% was high heterogeneity; I2=50% was moderate; I2=25% was low). Subgroup analyses were performed to determine the effect of L-PRF on socket width (horizontal width, vertical width, and socket fill) and the healing index (post-operative days 7 and 14) after dental extraction. Review Manager (RevMan 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) was used to perform statistical analysis.
Results
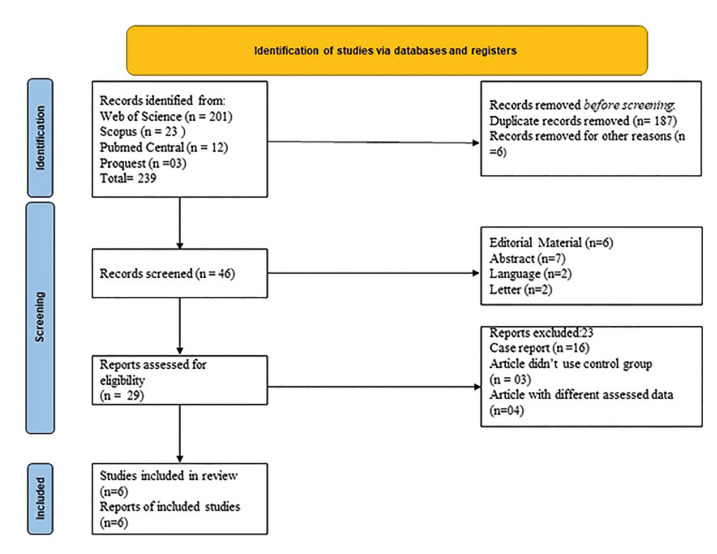
A review of the literature identified 239 potential, relevant articles; ultimately, 6 met all criteria, which used for meta-analysis (Fig. 1). The six studies included 153 patients who underwent dental extraction. Their characteristics are shown in Table 1. Most of the studies were from Brazil, Belgium and Italy. The healing index 7 and 14 days after dental extraction and the VAS score were compared in three studies; two studies of different cohorts reported differences in the percentage of bone formation, socket width, and socket fill between the control and L-PRF groups.
Figure 1.
Flowchart of the studies selected for review and analysis.
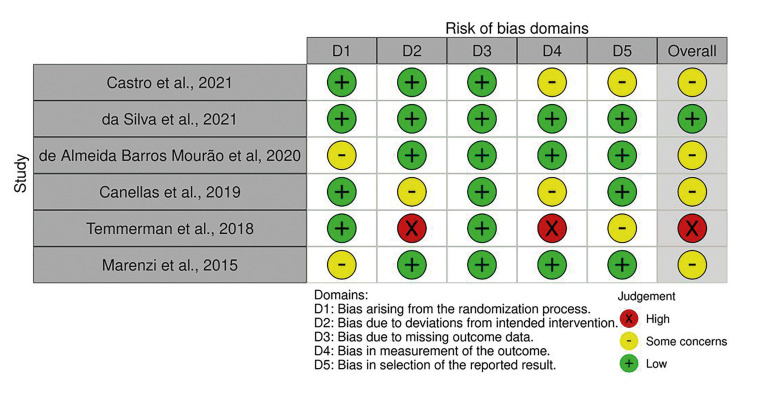
- Quality assessment
was used to quality assessment of the included RCTs were used Cochrane Collaboration’s tool to assess risk of bias. The observation suggest that one study had high risk of bias; One trial had a low risk of bias; and four trials an unclear risk of bias (Fig. 2).
Figure 2.
Risk of bias of included studies. Meta-analysis of socket width, socket filling and bone formation in control and L-PRF treated dental extraction patients (split mouth study).
- Meta-Analysis for socket width, socket filling and bone formation in control and L-PRF treated dental extraction (split mouth study)
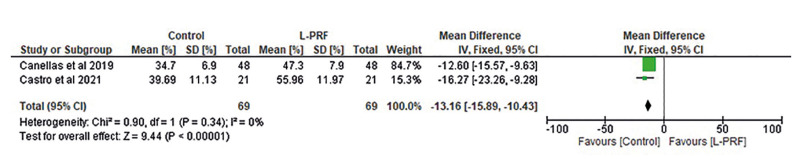
The percentage of bone formation after dental extraction in control and L-PRF-treated patients was compared in two studies. The results of the statistical analysis are shown in Fig. 3. L-PRF group indicates higher in bone formation than in controls, with a mean difference of -13.16 (-15.89, -10.43). The difference in heterogeneity between studies was significant (df=1; p<0.00001).
Figure 3.
Forest plot of studies reporting the percentage of bone formation in control and L-PRF treated dental extraction patients.
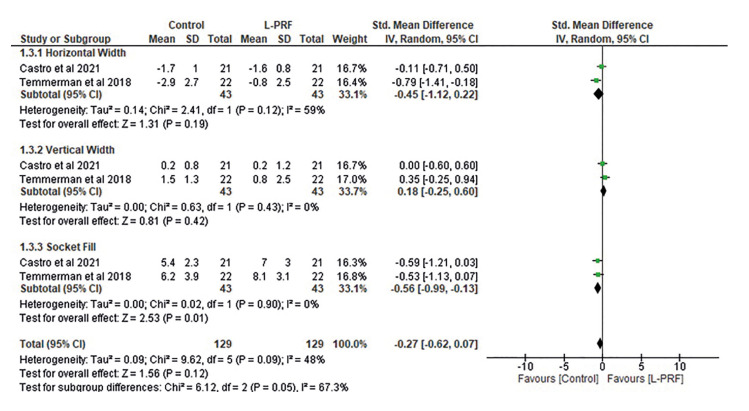
Fig. 4 shows the socket width based on a subgroup meta-analysis of the horizontal and vertical width and socket filling. The horizontal width was lower in controls than in the L-PRF group but the mean difference was small (-0.45 [-1.12, 0.22]) and the heterogeneity of the studies was moderate (I2 =59%). However, the vertical width was lower in treated patients than in controls, with a mean difference of 0.18 (-0.25, 0.6). The difference in heterogeneity was not significant (df=1; p=0.43; I2=0%). Conversely, socket filling was higher in the L-PRF group. The mean difference was -0.56 (-0.99, -0.13) and the difference in heterogeneity was not significant (df=1; p=0.90; I2=0%). Overall, the mean difference between groups in the subgroup analysis was low (-0.27 [-0.62, 0.07]) and the difference in heterogeneity was moderate (I2=48%), but not significant (p=0.09).
Figure 4.
Forest plot of studies comparing socket width in a subgroup analysis of horizontal width, vertical width, and socket filling.
- Meta-analysis of the healing index
The healing index was compared between groups in a subgroup analysis of days 7 and 14 after dental extraction based on three different studies (Supplement 1). The index was higher in the L-PRF group than in controls on both post-operative day 7 and post-operative day 14. Overall, the index declined and the difference in heterogeneity was significant.
- Meta-analysis of VAS score
The VAS score was used to determine the pain level on day 7 after surgery (Supplement 2), and was lower in treated patients. There was lower VAS observed in L-PRF implant treated dental extraction than control group. Mean difference was observed higher upto 1.26 [1.00, 1.51] and significant difference was observed in the heterogenicity between them (df = 1; p< 0.00001).
Discussion
Dental extraction is the most common form of oral surgery. Patients who undergo dental extraction experience discomfort for several days post-operatively due to swelling and pain in the vicinity of the surgical site (18). Bone loss during dental extraction also contributes to the discomfort, as the socket heals slowly. Implants to prevent ridge formation and bone loss and thereby promote healing and reduce discomfort have been proposed. L-PRF implants are rich in proteins and growth factors that promote wound healing (19), reduce postoperative pain and improve epithelialisation (20). L-PRF treatment may therefore improve the quality of life in early post-operative period of dental surgery patients. However, a recent study showed that it does not significantly improve pain and wound healing after dental extraction (8). We therefore conducted a meta-analysis to determine the effect of L-PRF on dental extraction.
Data from six studies were analysed to assess the factors that contribute to ridge prevention and wound healing. The respective studies were RCTs with a split-mouth design. L-PRF may play a role in soft-tissue regeneration by stimulating collagen synthesis and fibroblast proliferation (21). Clotting is an important process during surgery because it accelerates homeostasis. L-PRF contains concentrated thrombin and fibrinogen, and the complex trimolecular structure of the fibrin matrix resembles the natural tissue matrix but with higher elasticity and resistance (22). These features contribute to improved socket filling after dental extraction. The results of study indicated higher percentage of bone formation in the L-PRF group than controls. Socket width was also analysed, by determining the differences in the horizontal and vertical width, together with socket filling. Better results were obtained in the treated group. A metanalysis study on plasma concentrate (PC) like L-PRF and P-PRF has shown that spontaneous healing and alveolar ridges formation improved, however no differences observed among L-PRF and P-PRF (23). Data of our investigation supported by study of Caponio et al (23), difference between these studies, as it focus on L-PRF and P-PRF treatment on bone formation and our report majorly involve the assessment of L-PRF on new bone formation.
Post-operative pain and delayed wound healing contribute to the discomfort experienced by dental extraction patients, thus highlighting the importance of ridge prevention (24). L-PRF has been shown to relieve pain after tooth extraction (25). By sealing the socket with a membrane, L-PRF prevents the entry of debris and food and thus reduces pain stimuli (26). It also stimulates host defence mechanisms, by regulating the immune system, thus enhancing healing and relieving pain, in addition to warding off infection. These observations were supported by our meta-analysis, which showed a significantly higher healing index and better pain reduction in the L-PRF group.
Some limitations should be mentioned. First, only six publications were analysed and the patients were assessed for only 14 days. Also, many of the included studies had a moderate risk of bias. In addition, none of the studies assessed all parameters of interest.
Conclusions
In conclusion, our meta-analysis showed that the L-PRF implant prevents ridge formation by improving both the percentage of bone formation and socket width (improved horizontal width and socket filling). Moreover, it improves the healing index and reduces the VAS score significantly.
Table 1.
Characteristics of the studies comparing socket width, pain index (VAS) and Healing Index in Control and L-PRF treated dental implants included in the meta-analysis.
| Author, Year | Country | Study Design | Sample size | Socket width (mm) | Bone Formation (%) | VAS | Healing Index | Age | Gender (M/F) | Conclusion | Reference | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control | L-PRF | Control | L-PRF | Control | L-PRF | Control | L-PRF | ||||||||
| Castro et al., 2021 | Belgium | Randomized controlled clinical split-mouth trial | 21 | Socket filling= 5.4±2.3 Horizontal: -1.7±1.0 Vertical: 0.2±0.8 | Socket filling = 7.0±3.0 Horizontal: -1.6±0.8 Vertical: 0.2±1.2 | 39.69± 11.13 | 55.96± 11.97 | -- | -- | -- | -- | 64.4± 12 | 6/15 | No affect dimension, Superior socket healing Superior bone formation | (12) |
| Canellas et al., 2019 | Brazil | Single blind Randomized controlled clinical | 48 | -- | -- | 34.7± 6.9 | 47.3± 7.9 | -- | -- | -- | -- | 44.8± 26 | 21/27 | L-PRF should be always considered | (13) |
| Marenzi et al., 2015 | Italy | Randomized clinical trial | 26 | -- | -- | -- | -- | 4.5± 0.7 | 3.2± 0.3 | 7 Day: 4.9± 0.3 | 7 Day: 4.5± 0.5 | 53±4 | 9/17 | Use of L-PRF in post extraction sockets filling is efficient and useful procedure | (14) |
| 14 Day: 4.3± 0.3 | 14 Day: 4.2± 0.2 | ||||||||||||||
| da Silva et al., 2021 | Brazil | Randomize, double blinded, split mouth study | 20 | -- | -- | -- | -- | 0.37± 0.17 | 0.00± 0.0 | 7 Day: 3.64± 0.15 | 7 Day: 4.64± 0.14 | 23± 3.28 | 6/14 | Use of L-PRF improves soft tissue healing process and decrease post operative pain | (15) |
| 14Day: 4.48± 0.13 | 14Day: 4.9± 0.07 | ||||||||||||||
| de Almeida Barros Mourão et al, 2020 | Brazil | Randomized, double blinded, split mouth study | 16 | -- | -- | -- | -- | 5.12± 1.08 | 4± 1.15 | 7 Day: 3.18± 0.54 | 7 Day: 3.81± 0.65 | Control 38.1± 10.5 L-PRF 36.5± 11.4 | Control 9/7 L-PRF 10/6 | -- | (16) |
| 14Day: 4.5± 0.51 | 14Day: 4.75± 0.44 | ||||||||||||||
| Temmerman et al., 2018 | -- | Randomized, double blinded, split mouth study | 22 | Socket filling = 6.2±3.9 Horizontal: -2.9±2.7 Vertical: 1.5±1.3 | Socket filling = 8.1±3.1 Horizontal: -0.8±2.5 Vertical: 0.5±2.3 | -- | -- | -- | -- | -- | -- | 54±11 | 15/7 | -- | (17) |
Acknowledgement
All the author of given manuscript thankful to Shijiazhuang Fourth Hospital, China for providing necessary facility to conduct this work.
Institutional Review Board Statement
Declared none.
Data Availability Statement
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the Correspondence.
Author Contributions
Xu Wang collected literature and drafted the rough manuscript; Xin Fu analyses the data. Siwei Zhou conceptualize, guided and revised the manuscript.
Funding
None.
Conflict of interest
The authors declare no conflict of interest, financial or otherwise.
References
- 1.Srinivas B, Das P, Rana MM, Qureshi AQ, Vaidya KC, Ahmed Raziuddin SJ. Wound Healing and Bone Regeneration in Post extraction Sockets with and without Platelet-rich Fibrin. Ann Maxillofac Surg. 2018;8:28–34. doi: 10.4103/ams.ams_153_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.MacBeth N, Trullenque-Eriksson A, Donos N, Mardas N. Hard and soft tissue changes following alveolar ridge preservation: a systematic review. Clin Oral Implants Res. 2017;28:982–04. doi: 10.1111/clr.12911. [DOI] [PubMed] [Google Scholar]
- 3.Vieira AE, Repeke CE, Ferreira Junior Sde B, Colavite PM, Biguetti CC, Oliveira RC. Intramembranous bone healing process subsequent to tooth extraction in mice: micro-computed tomography, histomorphometric and molecular characterization. PLoS One. 2015;10:e0128021. doi: 10.1371/journal.pone.0128021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tanaka Y, Aung KT, Ono M, Mikai A, Dang AT, Hara ES. Suppression of Bone Necrosis around Tooth Extraction Socket in a MRONJ-like Mouse Model by E-rhBMP-2 Containing Artificial Bone Graft Administration. Int J Mol Sci. 2021;22:12823. doi: 10.3390/ijms222312823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Avila-Ortiz G, Elangovan S, Kramer KW, Blanchette D, Dawson DV. Effect of alveolar ridge preservation after tooth extraction: a systematic review and meta-analysis. J Dent Res. 2014;93:950–8. doi: 10.1177/0022034514541127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pozzi A, Gallelli L. Pain management for dentists: the role of ibuprofen. Ann Stomatol (Roma) 2011;2:3–24. [PMC free article] [PubMed] [Google Scholar]
- 7.Mamoun J. Dry Socket Etiology, Diagnosis, and Clinical Treatment Techniques. J Korean Assoc Oral Maxillofac Surg. 2018;44:52–8. doi: 10.5125/jkaoms.2018.44.2.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saluja H, Dehane V, Mahindra U. Platelet-Rich fibrin: A second generation platelet concentrate and a new friend of oral and maxillofacial surgeons. Ann Maxillofac Surg. 2011;1:53–7. doi: 10.4103/2231-0746.83158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roy S, Driggs J, Elgharably H, Biswas S, Findley M, Khanna S. Platelet-rich fibrin matrix improves wound angiogenesis via inducing endothelial cell proliferation. Wound Repair Regen. 2011;19:753–66. doi: 10.1111/j.1524-475X.2011.00740.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kökdere NN, Baykul T, Findik Y. The use of platelet-rich fibrin (PRF) and PRF-mixed particulated autogenous bone graft in the treatment of bone defects: An experimental and histomorphometrical study. Dent Res J (Isfahan) 2015;12:418–24. doi: 10.4103/1735-3327.166188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Francisco I, Vale F, Martin V, Fernandes MH, Gomes PS. From Blood to Bone-The Osteogenic Activity of L-PRF Membranes on the Ex Vivo Embryonic Chick Femur Development Model. Materials (Basel) 2021;14:7830. doi: 10.3390/ma14247830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Castro AB, Van Dessel J, Temmerman A, Jacobs R, Quirynen M. Effect of different platelet-rich fibrin matrices for ridge preservation in multiple tooth extractions: A split-mouth randomized controlled clinical trial. J Clin Periodontol. 2021;48:984–95. doi: 10.1111/jcpe.13463. [DOI] [PubMed] [Google Scholar]
- 13.Canellas JVDS, da Costa RC, Breves RC, de Oliveira GP, Figueredo CMDS, Fischer RG. Tomographic and histomorphometric evaluation of socket healing after tooth extraction using leukocyte- and platelet-rich fibrin: A randomized, single-blind, controlled clinical trial. J Craniomaxillofac Surg. 2020;48:24–32. doi: 10.1016/j.jcms.2019.11.006. [DOI] [PubMed] [Google Scholar]
- 14.Marenzi G, Riccitiello F, Tia M, di Lauro A, Sammartino G. Influence of Leukocyte- and Platelet-Rich Fibrin (L-PRF) in the Healing of Simple Postextraction Sockets: A Split-Mouth Study. Biomed Res Int. 2015;2015:369273. doi: 10.1155/2015/369273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.da Silva MT, de Almeida Barros Mourão CF, Mello-Machado RC, Montemezzi P, de Lima Barbosa R, Sartoretto SC. Effects of Leukocyte-Platelet-Rich Fibrin (L-PRF) on Pain, Soft Tissue Healing, Growth Factors, and Cytokines after Third Molar Extraction: A Randomized, Split-Mouth, Double-Blinded Clinical Trial. Appl Sci. 2021;11:1666. [Google Scholar]
- 16.de Almeida Barros Mourão CF, de Mello-Machado RC, Javid K, Moraschini V. The use of leukocyte- and platelet-rich fibrin in the management of soft tissue healing and pain in post-extraction sockets: A randomized clinical trial. J Craniomaxillofac Surg. 2020;48:452–7. doi: 10.1016/j.jcms.2020.02.020. [DOI] [PubMed] [Google Scholar]
- 17.Temmerman A, Cleeren GJ, Castro AB, Teughels W, Quirynen M. L-PRF for increasing the width of keratinized mucosa around implants: A split-mouth, randomized, controlled pilot clinical trial. J Periodontal Res. 2018;53:793–800. doi: 10.1111/jre.12568. [DOI] [PubMed] [Google Scholar]
- 18.Park WJ, Park IK, Shin KS, Choi EJ. Post-extraction pain in the adjacent tooth after surgical extraction of the mandibular third molar. J Dent Anesth Pain Med. 2019;19:201–8. doi: 10.17245/jdapm.2019.19.4.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Naik B, Karunakar P, Jayadev M, Marshal VR. Role of Platelet rich fibrin in wound healing: A critical review. J Conserv Dent. 2013;16:284–93. doi: 10.4103/0972-0707.114344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dragonas P, Katsaros T, Avila-Ortiz G, Chambrone L, Schiavo JH, Palaiologou A. Effects of leukocyte-platelet-rich fibrin (L-PRF) in different intraoral bone grafting procedures: a systematic review. Int J Oral Maxillofac Surg. 2019;48:250–62. doi: 10.1016/j.ijom.2018.06.003. [DOI] [PubMed] [Google Scholar]
- 21.Strauss FJ, Nasirzade J, Kargarpoor Z, Stähli A, Gruber R. Effect of platelet-rich fibrin on cell proliferation, migration, differentiation, inflammation, and osteoclastogenesis: a systematic review of in vitro studies. Clin Oral Investig. 2020;24:569–84. doi: 10.1007/s00784-019-03156-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mohan SP, Jaishangar N, Devy S, Narayanan A, Cherian D, Madhavan SS. Platelet-Rich Plasma and Platelet-Rich Fibrin in Periodontal Regeneration: A Review. J Pharm Bioallied Sci. 2019;11:S126–30. doi: 10.4103/JPBS.JPBS_41_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Caponio VCA, Baca-González L, González-Serrano J, Torres J, López-Pintor RM. Effect of the use of platelet concentrates on new bone formation in alveolar ridge preservation: a systematic review, meta-analysis, and trial sequential analysis. Clin Oral Investig. 2023;27:4131–46. doi: 10.1007/s00784-023-05126-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guo S, Dipietro LA. Factors affecting wound healing. J Dent Res. 2010;89:219–29. doi: 10.1177/0022034509359125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nourwali I. The effects of platelet-rich fibrin on post-surgical complications following removal of impacted wisdom teeth: A pilot study. J Taibah Univ Med Sci. 2021;16:521–28. doi: 10.1016/j.jtumed.2021.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kattimani VS, Lingamaneni KP, Kreedapathi GE, Kattappagari KK. Socket preservation using eggshell-derived nanohydroxyapatite with platelet-rich fibrin as a barrier membrane: a new technique. J Korean Assoc Oral Maxillofac Surg. 2019;45:332–42. doi: 10.5125/jkaoms.2019.45.6.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the Correspondence.