Abstract
Background:
This study aimed to evaluate and compare the outcomes of proximal row carpectomy (PRC) with interposition arthroplasty using dorsal wrist capsule interposition, lateral meniscus allograft, or dermal allograft in patients with lunate facet/capitate degeneration.
Methods:
Patients who underwent PRC with interposition arthroplasty between 2010 and 2022 at a single institution were identified. Preoperative and postoperative visual analog scale (VAS) pain, functional outcomes, and complications were recorded.
Results:
Twenty-one patients (11 dorsal capsule, 6 meniscus, 4 dermal matrix) were identified with a mean follow-up of 65.8 months. Postoperative pain and functional outcome scores significantly improved. The mean postoperative Quick Disabilities of the Arm, Shoulder, and Hand score was 20.3. In total, 89.5% of patients returned to work, including 75% of manual laborers.
Conclusions:
No significant differences were found between dorsal capsular flap versus allograft groups. Proximal row carpectomy with interposition arthroplasty is an effective motion-sparing procedure for patients with proximal capitate and/or lunate fossa arthritis, improving pain and function.
Keywords: proximal row carpectomy, PRC, interposition arthroplasty, meniscus allograft dermal matrix allograft, dorsal capsule, wrist arthritis
Introduction
Proximal row carpectomy (PRC) is recognized as an effective surgical option for managing wrist arthritis and has demonstrated functional range of motion, grip strength, and pain relief.1 -5 The PRC, however, is traditionally contraindicated in patients with degeneration of the proximal capitate and/or the lunate fossa of the distal radius due to increased peak joint contact pressures and reduced contact area compared with the normal wrist. 6 Limited or total wrist arthrodesis or arthroplasty has been the recommended treatment in these cases, but it has multiple disadvantages and complications, including prolonged immobilization, loss of motion, the risk of nonunion, symptomatic hardware, implant loosening, dislocation, or wear.7 -10
In patients with additional degenerative changes undergoing PRC, soft tissue interposition into the radiocapitate joint has been proposed.1,2,6,11 -13 Dorsal capsular flap interposition has shown improvements in pain, grip strength, arc of motion, and patient-reported outcome measures.14 -17 Nanavati et al 6 presented the use of lateral meniscus allograft as an interposition material, reporting restoration of near anatomical pressure and contact areas in cadaveric specimens. Furthermore, decellularized dermal allograft has been reported as an interposition material with comparable outcomes to PRC alone.12,18,19 However, studies on these procedures are limited, and to our knowledge, none have directly compared the outcomes of the 3 procedures.
The objective of this study is to evaluate and compare the outcomes of PRC with interposition arthroplasty using dorsal wrist capsular flap, lateral meniscus allograft, or dermal allograft in patients with advanced wrist arthritis involving the proximal capitate and/or lunate facet of the distal radius.
Methods
Study Design and Patient Selection
This single-center study was conducted at a tertiary care academic center after obtaining institutional review board approval. Patients who underwent PRC with interposition arthroplasty between January 1, 2010 and May 1, 2022 were identified from a surgical procedure database. Inclusion criteria were adult patients aged 18 years and older with osteoarthritis, posttraumatic arthritis, and inflammatory arthritis affecting the radiocarpal joint. The electronic medical record was reviewed to confirm the procedure performed and the presence of proximal capitate and/or lunate facet arthritis, based on direct intraoperative inspection of the cartilage surfaces, as the indication. Patients with less than 12 months of clinical follow-up were excluded from analysis. Dermal allograft materials used included AlloDerm regenerative tissue matrix (thickness: 1.6 ± 0.4 mm; Allergan Aesthetics, Irvine, California), Graftjacket regenerative tissue matrix (thickness: 3-4 mm; Wright Medical Group, Memphis, Tennessee), and ArthroFLEX decellularized dermal allograft (thickness: 0.5-3 mm; Arthrex, Naples, Florida). Where possible, the thickest graft was preferably used.
Data Collection
Patient demographic data, diagnosis, preoperative and postoperative visual analog scale (VAS) pain scores, ability to work, grip strength, and active wrist flexion and extension range of motion were collected. To assess patient-reported outcomes, patients were prospectively contacted by phone and the Quick Disabilities of the Arm, Shoulder, and Hand (QuickDASH) questionnaire and VAS pain scale were administered. Interviews were conducted to evaluate patient satisfaction as well as return to work and/or daily activities. Five attempts were made to contact the patients. Preoperative and postoperative Mayo wrist scores were calculated and preoperative radiographs were reviewed to classify capitate morphology as described by Yazaki et al. 20 Initial and final postoperative radiographs were reviewed to evaluate maintenance of the radiocapitate space, measured as the distance from the center of the articular portion of the capitate to the lunate facet of the distal radius on a standardized posterior-anterior radiograph and distances were calculated using standardized software within the electronic medical record system by a single nonblinded reviewer. 19
Statistical Analysis
Preoperative and postoperative variables were compared within the entire cohort to evaluate the effectiveness of PRC with interposition arthroplasty. Subgroup analyses compared the performance of the 3 interposition groups (dorsal capsule, lateral meniscus, and dermal allograft) to each other. Furthermore, the dorsal capsular flap was compared with allograft interposition (lateral meniscus and dermal). Normally distributed numerical variables, using the Shapiro-Wilk test, were reported as means and standard deviation and nonparametric variables using median and interquartile ranges. Categorical variables were expressed as the number (percentage) of participants in each category. Means of normally distributed numerical variables were compared using the Student t-test. Nonparametric variables were compared between groups using the Mann-Whitney test and paired samples were compared using the Wilcoxon signed rank test. Preoperative and postoperative categorical variables were compared using the McNemar test. A P value of <.05 was considered statistically significant.
Results
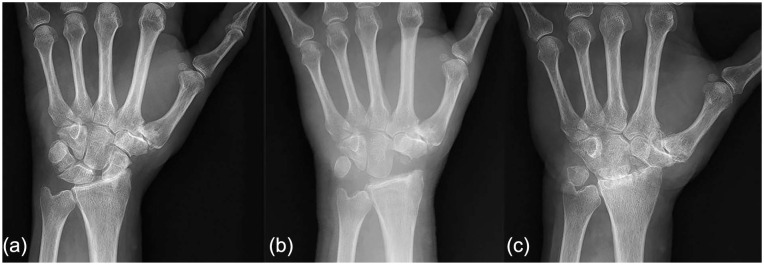
Twenty-one patients were included in the study. There were 11 patients in the dorsal capsule group (Figure 1), 6 patients in the lateral meniscus group, and 4 patients in the dermal matrix group. Nineteen patients (90.5%) were available for prospective data collection, with a mean total follow-up duration of 65.8 months (range: 12-128 months) and mean follow-up for the physical examination findings of 23.8 months (range: 12-122 months).
Figure 1.
Case example of a 59-year-old right-hand dominant patient with scapholunate advanced collapse and radioscaphoid arthritis (a). This patient underwent a proximal row carpectomy with dorsal capsular interposition. His 2-week postoperative radiographs demonstrate a preserved radiocapitate interval (b). Ten years postoperatively, this patient returned with recurrent wrist pain and radiographs showing radiocapitate arthritis with loss of the radiocapitate space (c).
The mean age at the time of surgery was 59.3 years (range: 33-73), with 47.6% patients being men. Eighteen of 21 patients (85.7%) were right-hand dominant and 9/21 (42.9%) were manual laborers. The manual laborer group comprised mechanics, carpenters, construction workers, and truck drivers. The patients presented with various diagnoses, including scapholunate advanced collapse (57.1%), primary osteoarthritis (19.1%), Kienböck disease (14.3%), and scaphoid nonunion advanced collapse (9.5%). None of the included patients had a past history of distal radius malunion.
Analysis of the entire cohort demonstrated significant improvements in patients’ function at final available postoperative follow-up. The mean VAS pain score decreased from 7.85 preoperatively to 1.85 postoperatively (P < .05). Mean Mayo wrist scores improved from 29.6 preoperatively to 65.7 postoperatively (P < .05). The mean postoperative QuickDASH score was 20.3 (Table 1). Mean grip strength improved from 51.6% to 73.9% of the contralateral side; however, this did not reach statistical significance (P = 0.06). The mean wrist flexion-extension arc was relatively unchanged with 60.7° preoperatively and 66.2° postoperatively (P = .42) (Table 2). Seventeen of 19 (89.5%) of the patients were able to return to work, with 75% returning to manual labor. There was no difference in return to work when comparing manual versus nonmanual laborers (P = .54). All 19 patients (100%) expressed satisfaction with the surgical outcomes and would have made the same decision in selecting this procedure. The nonmanual laborers had improved VAS pain, Mayo wrist, and QuickDASH scores, as well as grip strength and wrist flexion-extension arc, compared with the manual laborers; however, these differences did not reach statistical significance (Table 3). There were also no significant differences observed when comparing the patients who received dorsal capsular flap versus allograft (Table 4).
Table 1.
Comparison of Preoperative and Postoperative VAS Pain, Mayo Wrist, and QuickDASH Scores Between Groups.
| Interposition material | N (% male) | Mean follow-up months (range) | Age (mean) | Preop VAS (SD) | Postop VAS (SD) | P value | Preop mayo wrist (SD) | Postop mayo wrist (SD) | P value | Postop QuickDASH (SD) |
|---|---|---|---|---|---|---|---|---|---|---|
| All | 21 (66.7) | 65.8 (12-128) | 59.8 | 7.85 (1.39) | 1.85 (1.81) | <.001 | 29.6 (12.8) | 65.7 (15.2) | <.001 | 20.3 (17.85) |
| Allograft | 10 (60.0) | 70.6 (12-128) | 7.90 (1.52) | 2.30 (1.64) | <.001 | 28.6 (11.1) | 67.9 (11.1) | <.001 | 25.66 (19) | |
| Lateral meniscus | 6 (66.7) | 73.2 (53-126) | 57.4 | 8.17 (1.94) | 2.67 (1.37) | <.001 | 31.3 (13.2) | 61.3 (8.5) | .016 | 27.56 (13.67) |
| Dermal matrix | 4 (50.0) | 66.6 (12-128) | 61.2 | 7.50 (0.58) | 1.75 (2.06) | .011 | 25.0 (8.7) | 76.7 (7.6) | .004 | 23.29 (28.16) |
| Dorsal capsule | 11 (72.3) | 61.5 (16-123) | 59.7 | 7.80 (1.32) | 1.40 (1.96) | <.001 | 30.7 (15.1) | 63.6 (19.1) | .017 | 15.48 (15.19) |
Note. VAS = visual analog scale; QuickDASH = Quick Disabilities of the Arm, Shoulder, and Hand.
Table 2.
Comparison of Preoperative and Postoperative Wrist Motion and Grip Strength Between Groups.
| Interposition material | N | Mean follow-up months (range) | Preop flexion-extension arc, degrees (SD) | Postop flexion-extension arc, degrees (SD) | P value | Preop grip strength, % a (SD) | Postop grip strength, % a (SD) | P value |
|---|---|---|---|---|---|---|---|---|
| All | 21 | 23.8 (12-122) | 60.6 (26.3) | 66.2 (18.0) | .423 | 51.6 (24.5) | 73.9 (33.8) | .069 |
| Allograft | 10 | 28.0 (12-66) | 64.3 (27.5) | 72.0 (19.0) | .320 | 52.7 (20.5) | 80.1 (32.6) | .131 |
| Lateral meniscus | 6 | 33.3 (12-62) | 62.2 (30.5) | 68.3 (19.1) | .613 | 59.2 (6.9) | 60.5 (22.3) | .899 |
| Dermal matrix | 4 | 20.0 (12-66) | 67.5 (26.3) | 77.5 (20.2) | .320 | 44.1 (31.5) | 106.2 (25.6) | .107 |
| Dorsal capsule | 11 | 19.9 (12-122) | 57.0 (25.9) | 60.5 (15.7) | .776 | 50.6 (28.0) | 68.5 (36.1) | .331 |
Grip strength is reported as percentage of contralateral side.
Table 3.
Comparison of Postoperative Clinical, Functional, and Radiographic Outcomes Between Manual and Nonmanual Laborer Groups.
| Outcome measures | Manual | Nonmanual | P value |
|---|---|---|---|
| VAS pain, mean (SD) | 2.75 (1.98) | 1.25 (1.48) | .068 |
| QuickDASH, mean (SD) | 26.0 (16.5) | 16.2 (18.4) | .248 |
| Mayo wrist score, mean (SD) | 59.2 (19.6) | 70.6 (9.4) | .171 |
| Flexion-extension arc, mean (SD) | 60.6 (16.8) | 70.9 (18.3) | .208 |
| Grip strength, mean % a (SD) | 67.0 (31.4) | 84.1 (35.0) | .321 |
| Radiocapitate space, mm (SD) | 1.2 (1.5) | 0.9 (1.0) | .635 |
Note. VAS = visual analog scale; QuickDASH = Quick Disabilities of the Arm, Shoulder, and Hand.
Grip strength is reported as percentage of contralateral side.
Table 4.
Comparison of Postoperative Clinical, Functional, and Radiographic Outcomes Between Dorsal Capsule and Allograft Groups.
| Outcome measures | Allograft | Dorsal capsule | P value |
|---|---|---|---|
| VAS pain, mean (SD) | 2.30 (1.64) | 1.40 (1.96) | .279 |
| QuickDASH, mean (SD) | 25.7 (19.9) | 15.5 (15.2) | .224 |
| Mayo wrist score, mean (SD) | 67.9 (11.1) | 63.6 (19.1) | .617 |
| Flexion-extension arc, mean (SD) | 72.0 (19.0) | 60.5 (15.7) | .158 |
| Grip strength, mean % a (SD) | 82.6 (31.0) | 68.5 (36.1) | .415 |
| Radiocapitate space, mm (SD) | 0.8 (1.1) | 1.2 (1.4) | .459 |
Note. VAS = visual analog scale; QuickDASH = Quick Disabilities of the Arm, Shoulder, and Hand.
Grip strength is reported as percentage of contralateral side.
The mean follow-up for radiographic data was 19.9 months (range: 1-120 months). Most patients (71.4%) had flat capitate morphology, 23.8% had a spherical morphology, and 4.8% had V-shaped morphology. For the entire cohort, the mean initial radiocapitate space decreased from 3.4 mm (SD 1.9) to 1.2 mm (SD 1.2) at final follow-up (P < .001) (Table 5). In the dorsal capsule group, the initial radiocapitate space decreased from 3.9 mm (SD 2.3) to 1.2 mm (SD 1.4) (P < .001) (Table 5). Although there was a loss in radiocapitate space in the lateral meniscus and dermal matrix groups, this change was not statistically significant. Eleven of 19 (61.9%) patients had a preserved radiocapitate space and 8 (38.1%) patients had no radiocapitate space at final follow-up. In 1 patient, this occurred at 4 months postoperatively, and in the remaining 7 patients, this occurred more than 1 year postoperatively (range: 1-10 years). Despite this, all 19 patients (100%) expressed satisfaction with their surgical outcome. There was no difference in final radiocapitate space when comparing dorsal capsular flap versus allograft or manual versus nonmanual laborers (Tables 3 and 4). There were no differences in postoperative VAS pain, Mayo wrist, or QuickDASH scores, wrist arc of motion, grip strength, or final radiocapitate space when comparing patients with flat versus spherical capitate morphology.
Table 5.
Comparison of Preoperative and Postoperative RC Space Between Groups.
| Interposition material | N | Mean follow-up, months (range) | Immediate postop RC space, mm (SD) | Final follow-up postop RC space, mm (SD) | P value |
|---|---|---|---|---|---|
| All | 16 | 19.9 (1-120) | 3.4 (1.9) | 1.2 (1.2) | <.001 |
| Allograft | 7 | 17.4 (3-60) | 2.7 (1.1) | 1.2 (1.1) | .074 |
| Lateral meniscus | 3 | 24.2 (3-60) | 2.9 (0.7) | 1.7 (1.6) | .456 |
| Dermal matrix | 4 | 7.2 (3-12) | 2.6 (1.4) | 0.8 (0.5) | .151 |
| Dorsal capsule | 9 | 22.2 (1-120) | 3.9 (2.3) | 1.2 (1.4) | <.001 |
Note. RC = radiocapitate.
Two of the 21 patients (9.5%) required additional surgery for progressive symptomatic wrist arthritis. One patient underwent total wrist arthrodesis 37.2 months postoperatively, whereas another patient underwent revision interposition arthroplasty 120 months after the index procedure. Both patients were in the dorsal capsule group.
Discussion
This study aimed to evaluate and compare the outcomes of PRC with interposition arthroplasty using different tissues (dorsal capsular flap, lateral meniscus allograft, and dermal allograft) in patients with advanced wrist arthritis involving the proximal capitate and/or lunate fossa where this procedure is classically contraindicated. Patients undergoing PRC with interposition arthroplasty had significant improvements in pain and wrist function. All the patients were satisfied with the procedure and most were able to return to work. Manual laborers and patients with complete loss of radiocapitate space at final follow-up reported good functional outcomes, although these were greater in nonmanual workers.
The findings of this study align with previous literature that supports PRC as an effective surgical option for wrist arthritis. Proximal row carpectomy alleviates pain, while preserving functional range of motion and grip strength, and provides patients with an alternative to partial or total wrist arthrodesis, which may limit function.1 -5
Our results are also comparable with other studies in patients with advanced wrist arthritis that evaluate the use of various interposition materials with PRC. Kwon et al 16 reported the outcomes of 8 patients who underwent PRC with dorsal capsule interposition, demonstrating improved pain and patient-reported outcome scores without a change in motion or grip strength. Gaspar et al 14 compared the outcomes of PRC alone with PRC with dorsal capsule interposition and found improved postoperative grip strength, wrist flexion-extension arc, and patient-reported outcome scores in both groups, without a difference noted between the 2 groups. Lee et al 19 reported their experience with dermal allograft interposition in 9 patients, demonstrating a mean flexion-extension arc and grip strength of 95% and 84% relative to the contralateral side, as well as postoperative DASH score of 23.8. In 4 patients who had PRC with lateral meniscus allograft, Steiner et al 13 reported mean DASH and VAS pain scores of 24 and 3.6, respectively, with mean wrist flexion-extension arc and grip strength of 77% and 79% compared with the contralateral side. Although there was a 1 mm decrease in the radiocapitate space from initial postoperative imaging to final follow-up imaging, none of the patients went on to total wrist arthrodesis. 13 The authors cautioned against using the lateral meniscus allograft in patients with distal radius malunion or adaptive carpal instability, as the changes in contact pressures across the radiocarpal joint could cause excessive stress and result in early graft disintegration. 13
The complications of PRC with interposition arthroplasty appear to be similar to those associated with PRC alone.12,21 One potential complication that is specific to allograft interposition is foreign body reaction. Namdari et al 22 reported 2 cases of giant cell reaction after dermal allograft was used in patients undergoing glenoid resurfacing. Carlan et al 23 also reported an inflammatory reaction in 1 patient who underwent PRC with lateral meniscus allograft interposition. Foreign body reaction should therefore be included in the differential diagnosis when patients present with persistent pain after PRC with allograft interposition. In addition, tearing or displacement of the graft could also present a problem. Neither of these complications was noted in our patient series.
In our study, 2 of 21 patients (9.5%) underwent further surgery for progression of wrist arthritis, 1 patient at 3 years, and the other at 10 years after the index procedure. This is comparable with the limited literature available, as the reported incidence of conversion from PRC with interposition arthroplasty to total wrist arthrodesis ranges from 0% to 7%. After PRC alone, conversion to total wrist arthrodesis has been reported in up to 35% of patients.1,4 However, it is difficult to make a direct comparison, as one limitation in the current literature of PRC with interposition arthroplasty is the lack of long-term data.
Limitations of this study include a small sample size that precludes a power analysis and variations in interpositional material and surgeon technique. Furthermore, not all patients were available for prospective data collection due to the COVID pandemic. This was mitigated by conducting remote follow-up when possible. In addition, we were unable to evaluate the exact size of cartilage degeneration of the capitate and lunate; however, in reviewing the operative notes, all patients had descriptions of “mild to moderate” cartilage eburnation. This study also spanned over a 12-year period, and therefore, surgeon experience and techniques may have evolved over time, also introducing a potential source of bias. Notwithstanding these limitations, this study found all 3 methods of interposition to be effective as a motion-preserving procedure without significant differences between the 3 interposition materials (dorsal capsule, lateral meniscus allograft, and dermal allograft).
This study adds valuable evidence to the existing literature and supports the use of PRC with interposition arthroplasty as a viable treatment option for this patient population. Further research with larger cohorts and longer-term follow-up is warranted to assess the durability and longevity of the interposition arthroplasty materials.
Footnotes
Contributorship: All the named authors actively involved in the planning, enactment, and writing up of the study.
Ethical Approval: This study was approved by our institutional review board (IRB: 23-004012).
Statement of Human and Animal Rights: Procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 and 2008.
Statement of Informed Consent: Informed consent for research purposes was obtained per institutional protocol.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: SK is a consultant for Arthrex. The other author(s) declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Sanjeev Kakar  https://orcid.org/0000-0002-2886-1510
https://orcid.org/0000-0002-2886-1510
References
- 1. DiDonna ML, Kiefhaber TR, Stern PJ. Proximal row carpectomy: study with a minimum of ten years of follow-up. J Bone Joint Surg Am. 2004;86(11):2359-2365. [PubMed] [Google Scholar]
- 2. Jebson PJ, Hayes EP, Engber WD. Proximal row carpectomy: a minimum 10-year follow-up study. J Hand Surg Am. 2003;28(4):561-569. [DOI] [PubMed] [Google Scholar]
- 3. Tomaino MM, Miller RJ, Cole I, et al. Scapholunate advanced collapse wrist: proximal row carpectomy or limited wrist arthrodesis with scaphoid excision? J Hand Surg Am. 1994;19:134-142. [DOI] [PubMed] [Google Scholar]
- 4. Wall LB, Didonna ML, Kiefhaber TR, et al. Proximal row carpectomy: minimum 20-year follow-up. J Hand Surg Am. 2013;38(8):1498-1504. [DOI] [PubMed] [Google Scholar]
- 5. Wyrick JD, Stern PJ, Kiefhaber TR. Motion-preserving procedures in the treatment of scapholunate advanced collapse wrist: proximal row carpectomy versus four-corner arthrodesis. J Hand Surg Am. 1995;20(6):965-970. [DOI] [PubMed] [Google Scholar]
- 6. Nanavati VN, Werner FW, Sutton LG, et al. Proximal row carpectomy: role of a radiocarpal interposition lateral meniscal allograft. J Hand Surg. 2009;34:251-257. [DOI] [PubMed] [Google Scholar]
- 7. Enna M, Hoepfner P, Weiss APC. Scaphoid excision with four-corner fusion. Hand Clin. 2005;21:531-538. [DOI] [PubMed] [Google Scholar]
- 8. Mulford JS, Ceulemans LJ, Nam D, et al. Proximal row carpectomy vs four corner fusion for scapholunate (SLAC) or scaphoid nonunion advanced collapse (SNAC) wrists: a systematic review of outcomes. J Hand Surg Eup. 2009;34:256-263. [DOI] [PubMed] [Google Scholar]
- 9. Saltzman BM, Frank JM, Slikker W, et al. Clinical outcomes of proximal row carpectomy versus four-corner arthrodesis for post-traumatic wrist arthropathy: a systematic review. J Hand Surg Eur Vol. 2015;40(5):450-457. [DOI] [PubMed] [Google Scholar]
- 10. Wysocki RW, Cohen MS. Complications of limited and total wrist arthrodesis. Hand Clin. 2010;26(2):221-228. [DOI] [PubMed] [Google Scholar]
- 11. Oh S, Park HW, Kang SH, et al. Coexisting Kienböck’s and Preiser’s disease of the wrist: experience with proximal row carpectomy with dorsal capsular interposition technique. Orthop Surg. 2023;15(9):2477-2481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rabinovich RV, Lee SJ. Proximal row carpectomy using decellularized dermal allograft. J Hand Surg. 2018;43:392.e1-e9. [DOI] [PubMed] [Google Scholar]
- 13. Steiner M, Willsey M, Werner F, et al. Meniscal allograft interposition combined with proximal row carpectomy. J Wrist Surg. 2016;6:65-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gaspar MP, Pham PP, Pankiw CD, et al. Mid-term outcomes of routine proximal row carpectomy compared with proximal row carpectomy with dorsal capsular interposition arthroplasty for the treatment of late-stage arthropathy of the wrist. BJJ. 2018;100B:197-204. [DOI] [PubMed] [Google Scholar]
- 15. Eaton RG. Proximal row carpectomy and soft tissue interposition arthroplasty. Tech Hand Up Extrem Surg. 1997;1(4):248-254. [DOI] [PubMed] [Google Scholar]
- 16. Kwon BC, Choi SJ, Shin J, et al. Proximal row carpectomy with capsular interposition arthroplasty for advanced arthritis of the wrist. J Bone Joint Surg Br. 2009;91(12):1601-1606. [DOI] [PubMed] [Google Scholar]
- 17. Salomon GD, Eaton RG. Proximal row carpectomy with partial capitate resection. J Hand Surg Am. 1996;21(1):2-8. [DOI] [PubMed] [Google Scholar]
- 18. Carneiro Rdos S, Dias CE, Baptista CM. Proximal row carpectomy with allograft scaffold interposition arthroplasty. Tech Hand Up Extrem Surg. 2011;15(4):253-256. [DOI] [PubMed] [Google Scholar]
- 19. Lee SJ, Rabinovich RV, Kim A. Proximal row carpectomy using decellularized dermal allograft: preliminary results. J Wrist Surg. 2021;10(2):116-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yazaki N, Burns ST, Morris RP, et al. Variations of capitate morphology in the wrist. J Hand Surg Am. 2008;33(5):660-666. [DOI] [PubMed] [Google Scholar]
- 21. Fukushima WY, de Moraes VY, Penteado FT, et al. Does dorsal capsule interposition improve the results of proximal row carpectomy in Kienböck’s disease? One year randomized trial. SICOT J. 2015;1:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Namdari S, Melnic C, Huffman GR. Foreign body reaction to acellular dermal matrix allograft in biologic glenoid resurfacing shoulder. Clin Orthop Rel Res. 2013;471:2455-2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Carlan D, Boyer M, Gelberman R. Proximal row carpectomy: role of a radiocarpal interposition lateral meniscal allograft. J Hand Surg. 2009;34:157-158. [DOI] [PubMed] [Google Scholar]