Abstract
Introduction
1 mm cerclage cables have been introduced that can be placed under plates and hold reduction of periprosthetic femur fractures (PPFFx) around total hip arthroplasty (THA). Their utilization remains controversial due to the risk of nonunion secondary to periosteal stripping associated for their application. We compared surgical outcomes in patients with THA PPFFx treated with open reduction internal fixation (ORIF) and cables vs patients with PPFFx treated with ORIF without cables. We hypothesized that cable use would decrease hardware failure and nonunion rates.
Materials & Methods
We retrospectively reviewed 42 cases of PPFFx around THA performed from 2015 to 2021. Twenty-three PPFFx were treated with plate and 1 mm cerclage cables, and 19 PPFFx were treated with plate without cables. Primary surgical outcomes included hardware failure, nonunion, reoperation, and time to radiographic union.
Results
There was no significant difference in nonunion rates: 9% in the cerclage cable group vs 16% in the plate-only group (P = .64). The average time to union was 6.0 months among 17 observed unions in the cerclage cable group, vs 8.0 months among 15 observed unions in the plate-only group, but this failed to reach significance (P = .12). There was no statistical difference in overall complication rates (13% cerclage vs 16% plate) requiring reoperation (P = 1.0).
Discussion & Conclusion
The utilization of 1 mm cerclage cables to hold reduction of PPFFx provides an easy method to hold fixation with a low overall complication rate and no significant differences in nonunion rate or time to union when compared to cases performed without cables.
Keywords: periprosthetic fracture, femur fracture, plate, fixation, cerclage cables
Introduction
The current rate of periprosthetic femur fractures (PPFFx) associated with total hip arthroplasty (THA) is 1% for primary and 4% for revision THA, respectively. Although rare, this rate is expected to rise with the combination of an aging population and a growing prevalence of THA. 1 Surgical management of PPFFx is technically demanding given the poor bone quality, altered anatomy, and need to consider management of both the prosthesis and fracture. The Vancouver classification is classically used to differentiate PPFFx types and guide treatment. 2
PPFFx with a stable prosthesis are generally treated with open reduction internal fixation (ORIF), while revision arthroplasty with or without ORIF is chosen for fractures with an unstable prosthesis. In both situations, an adequate reduction is necessary and must be held to allow for hardware placement. This may be done with clamps, provisional plates, lag screws, or cerclage cables. Open cerclage cable techniques are well known for treatment of PPFFx, particularly long oblique, spiral, and some wedge-type fractures. 3 Early PPFFx plates and allograft strut-augments utilized only cable fixation. 4 These methods gave poor fixation and were associated with high failure rates. 4 Cable use has also been associated with high complication rates, most notably nonunion, but not limited to iatrogenic neurovascular injury, fraying, failure and consequent migration, and injury to the surgical team.5-11 Despite studies demonstrating similar fracture healing and minimal disruption in periosteal blood supply from cable fixation, this remains a point of contention.5,12-14
Recently, smaller cables have been designed to allow for placement underneath plates used to fix PPFFx. This allows for robust provisional fixation without the need for lag screws or small plates. The plate can be easily placed on top, and screws can be angled around the existing prosthesis. There is limited literature assessing clinical outcomes when using the combination of an open approach and application of cerclage cables to treat PPFFx. It is possible that this could increase periosteal stripping or lead to metal wear on the undersurface of the plate, resulting in higher rates of nonunion or failure. We aim to identify patients with PPFFx around a THA treated with cerclage cables and assess clinical outcomes, comparing this group to patients with PPFFx around a THA without cerclage cables. We hypothesize that the addition of cerclage cables provides a stable peri-implant fixation while preventing hardware failure and nonunion risk compared to patients treated for PPFFx without cerclage cables.
Materials & Methods
Following Institutional Review Board approval, a retrospective review of medical records was conducted to identify all patients with THA PPFFx treated surgically with ORIF using either plate and cerclage cables or plate-only at a single academic level-1 trauma center from 1/1/2015 to 12/31/2021. Inclusion criteria was limited to THA PPFFx treated with ORIF. Exclusion criteria included patients with PPFFx in the setting of ongoing infection, and patients under the age of 18.
PPFFx were treated with revision arthroplasty surgery if the stem was radiographically loose. If the treating surgeon deemed the stem stable, ORIF was performed in a lateral position on a radiolucent table. Infrequently, a combination revision and ORIF procedure was performed. In all cases, a traditional open approach, including elevating the vastus to expose the femur while preserving the origin of the vastus from the greater trochanter was utilized for fracture reduction, cerclage cable application, and plate fixation. The stem was checked for stability under direct visualization and intra-operative testing. The fracture was then reduced using clamps, and 1.0 mm cerclage cables (DePuy Synthes, Westchester, PA) were used to hold the reduction with the bone out to length. Fluoroscopy was used to assess reduction. In 34 cases, a condylar plate (4.5 mm VA-LCP Curved Condylar Plate, DePuy Synthes Trauma, Westchester, PA) was selected. In 8 cases, a curved locking compression plate (4.5 mm LCP, DePuy Synthes Traum, Westchester, PA) was selected. The plate was then contoured and placed to avoid stripping of the vastus insertion into the trochanter. The plate was applied and brought to the bone with cortical screws. Locking screws were placed in the condylar portion of the distal femur, if appropriate. When further purchase was required around a stem, one or two outrigger devices (locking attachment plate, LAP, DePuy Synthes, Warsaw, IN) were also applied. An example of pre-operation and post-operation radiographs are shown for a PPFFx treated with plate and cables in Figures 1–3 compared to a PPFFx treated with plate-only in Figures 4–6.
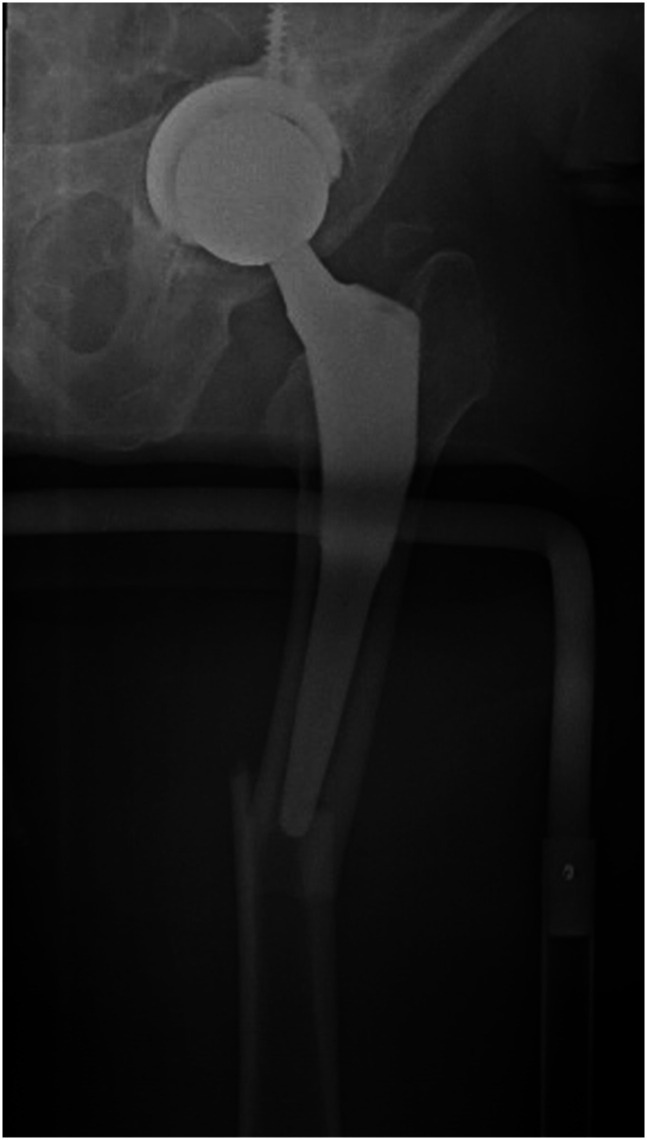
Figure 1.
Pre-operative AP radiograph of a left hip demonstrating a displaced, spiral PPFFx around a THA (Vancouver B1 classification).
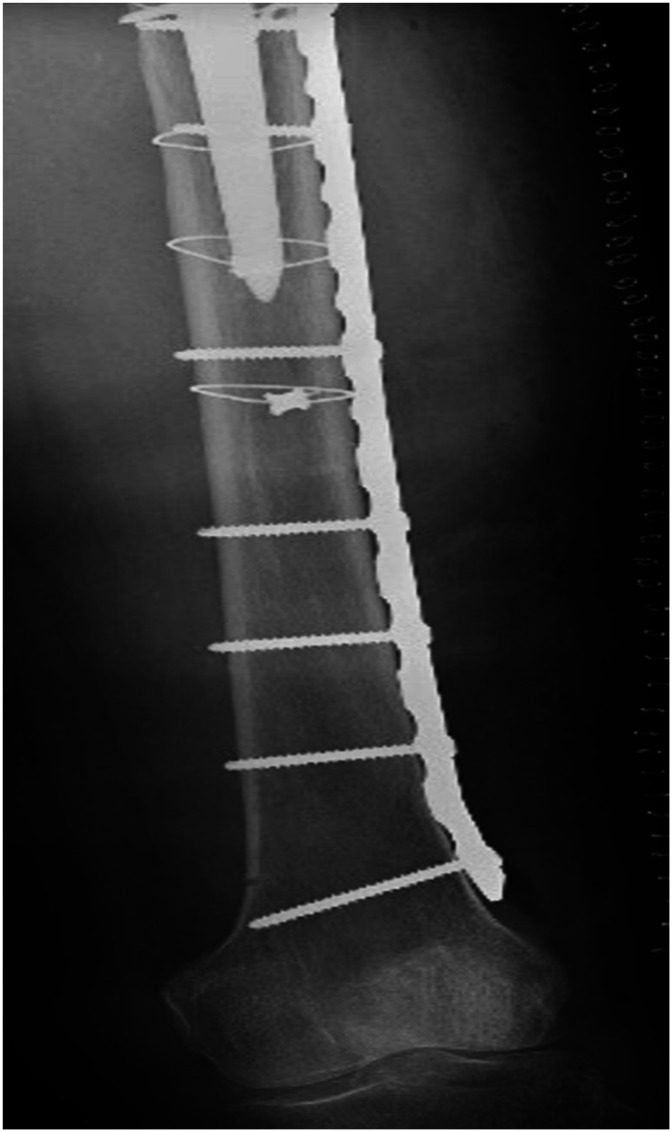
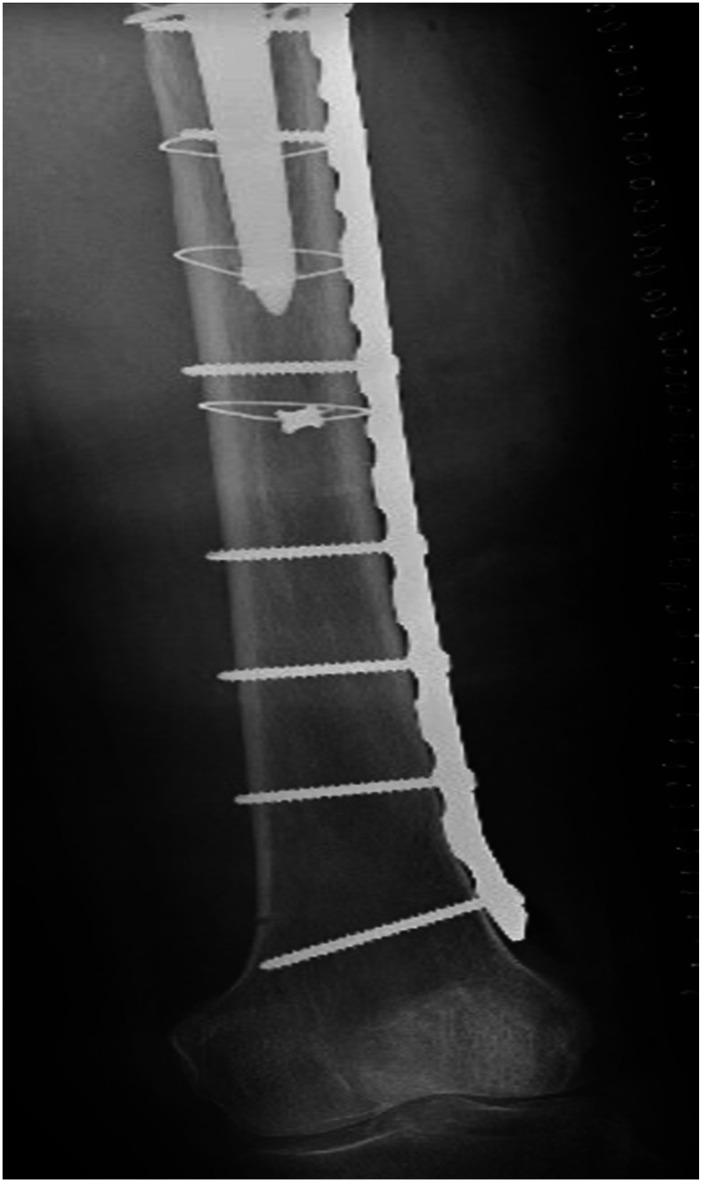
Figure 2.
Postoperative AP radiographs of the left hip and femur demonstrating final implant construct utilizing four 1.0 mm cerclage cables to hold initial reduction and a large fragment plate with two locking attachment plates for fixation.
Figure 3.
Postoperative AP radiographs of the left hip and femur demonstrating final implant construct utilizing four 1.0 mm cerclage cables to hold initial reduction and a large fragment plate with two locking attachment plates for fixation.
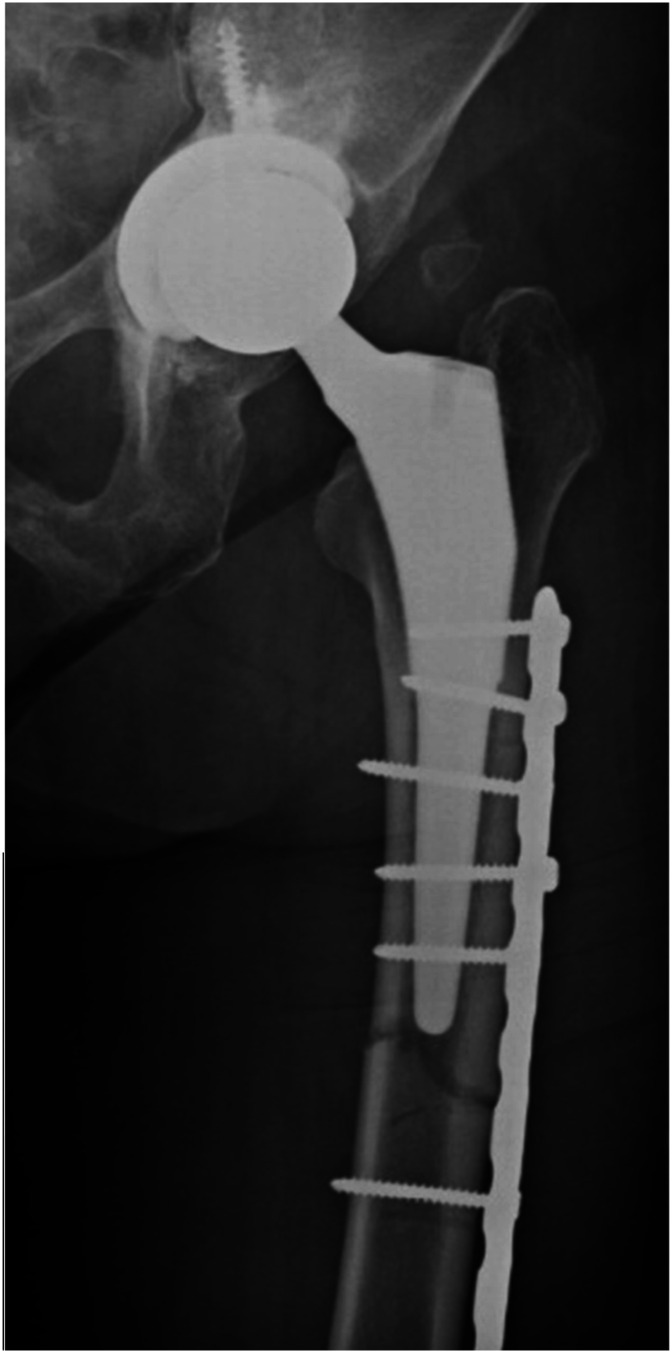
Figure 4.
Post-operative AP radiographs of the left hip and femur demonstrating final implant construct with a large fragment LCP alone.
Figure 5.
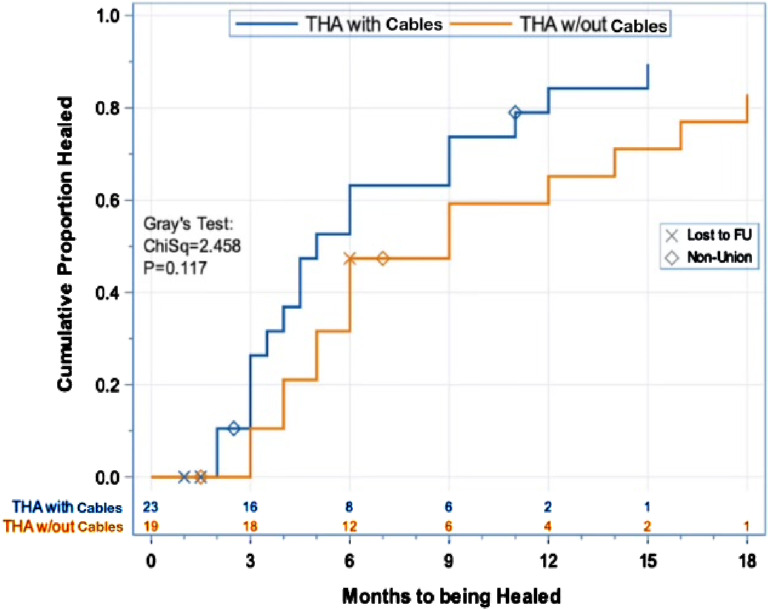
Proportion of individuals healed vs time to fracture union, showing a quicker time to heal and higher percentage of cases resulting in union for the cerclage-cable group (P = .12). “Lost to FU” means lost to follow-up.
Figure 6.
Proportion of individuals healed vs time to fracture union, showing a quicker time to heal and higher percentage of cases resulting in union for the cerclage-cable group (P = .12). “Lost to FU” means lost to follow-up.
Patients were separated into two groups. The first group was comprised of PPFFx treated with plate fixation and 1.0 mm cerclage cables for reduction, and the second group contained PPFFx treated with plate-only fixation. Charts were reviewed to record demographic values such as age, sex, race, and body mass index (BMI). Patient addresses were recorded to determine individual State and National Area Deprivation Index (ADI), a marker of socioeconomic status. 15 Comorbidities such as tobacco use, diabetes, peripheral vascular disease, and chronic kidney disease were recorded. Injury radiographs were reviewed to identify fracture location and classified using the Vancouver Classification system. 2 Operative notes were reviewed to determine whether final operative treatment was ORIF or a revision + ORIF. When cerclage cables were used, the total number of cables and their location (in relation to the fracture) were recorded. Primary outcome measures included variables most related to fixation achieved, including hardware failure, nonunion, reoperation, and time to radiographic union. Secondary outcomes recorded were less directly associated with fixation, including infection and prosthesis loosening. A review of medical records was performed to determine length of total follow-up and weight-bearing status at 3 and 12 months post-operation.
Statistical Analysis
Demographic variables including age, BMI, state ADI, and national ADI were summarized as means and standard deviations and compared for group differences with the Kruskal-Wallis test, which is appropriate for small sample sizes that will likely have non-normally distributed data. Categorical variables were summarized as numbers and percentages, where, depending on the variable, percentage was calculated based on the number of patients, the number of fractures, or the number of non-missing values. Pearson’s chi-square test was used to compare groups for differences in gender, whereas Fisher’s exact test was used to compare groups for differences in all other categorical variables because of sparseness. Time to healing was visualized using Kaplan-Meier cumulative-incidence curves with nonunion and loss to follow-up as competing risks, and groups were compared for differences in time to healing with Gray’s test, which accounts for competing risks. A P-value <.05 was set as the threshold for statistical significance.
Results
In total, 42 THA PPFFx were treated surgically with either plate and cerclage cable construct or plate fixation only from January 1st, 2015, to December 31st, 2021 by seven different surgeons. One individual in the cerclage cable group presented with bilateral PPFFx, so each femur was considered a separate case, giving the study 42 cases in 41 individuals. Of the 42 PPFFx treated surgically, 23 utilized plate and cerclage cables and 19 were treated with plate-only. Patient demographics and comorbidity data are shown for each group in Table 1. Of the 23 fractures in the cerclage cable group, 16 were Vancouver B1, one Vancouver B2, one Vancouver B3, and five Vancouver C types. Twenty fractures were treated with plate and cables, and 3 fractures were treated with revision arthroplasty in addition to plate and cables. The average number of total cerclage cables used for these fractures was 2.4 (ranging from 1-6). In the cerclage cable group, there were 13 females and 9 males. The average age at surgery was 71.9 years, and the mean BMI was 27.7 kg/m2.
Table 1.
Patient Demographics.
| Total | ORIF + Cables | ORIF | P † | |
|---|---|---|---|---|
| Number of Patients | 41 | 22 | 19 | |
| Number of Fractures | 42 | 23 | 19 | |
| Fracture Classification, N (%)2 | .002 | |||
| Vancouver B1 | 22 (52) | 17 (74) | 5 (26) | |
| Vancouver B2 | 2 (5) | 1 (4) | 1 (5) | |
| Vancouver B3 | 1 (2) | 1 (4) | 0 (0) | |
| Vancouver C | 17 (40) | 4 (17) | 13 (68) | |
| Gender, N (%)1 | .938* | |||
| Female | 24 (59) | 13 (59) | 11 (58) | |
| Male | 17 (41) | 9 (41) | 8 (42) | |
| Race, N (%)1 | 1.000 | |||
| White | 35 (85) | 19 (86) | 16 (84) | |
| African-American | 6 (15) | 3 (14) | 3 (16) | |
| Mean (SD) age at surgery (years) | 69.8 (14.9) | 71.9 (15.6) | 67.3 (14.0) | .150** |
| Mean (SD) BMI (kg/m2) | 28.6 (7.1) | 27.7 (6.4) | 29.6 (8.0) | .638** |
| Mean (SD) State ADI (decile) | 5.0 (3.1) | 5.3 (3.2) | 4.7 (3.1) | .518** |
| Mean (SD) National ADI (percentile) | 70.8 (23.8) | 72.3 (24.5) | 68.9 (23.6) | .472** |
| Diabetic, N (%)1 | .703 | |||
| Yes | 8 (20) | 5 (23) | 3 (16) | |
| No | 33 (80) | 17 (77) | 16 (84) | |
| Peripheral Vascular Disease, N (%)1 | 1.000 | |||
| Yes | 1 (2) | 1 (5) | 0 (0) | |
| No | 41 (98) | 21 (95) | 19 (100) | |
| Chronic Kidney Disease N (%)1 | 1.000 | |||
| Yes | 4 (10) | 2 (9) | 2 (11) | |
| No | 37 (90) | 22 (91) | 17 (89) | |
| Tobacco Use, N (%)3 | .606 | |||
| Never | 20 (53) | 12 (57) | 8 (47) | |
| Quit | 12 (32) | 7 (33) | 5 (29) | |
| Smoker | 6 (16) | 2 (10) | 4 (24) | |
| (Missing) | (3) | (1) | (2) | |
| ORIF vs Revision + ORIF, N (%)2 | .614 | |||
| ORIF only | 38 (90) | 20 (87) | 18 (95) | |
| Revision + ORIF | 4 (10) | 3 (13) | 1 (5) |
ORIF, Open Reduction Internal Fixation; BMI, Body Mass Index; ADI, Area Deprivation Index. 1: percent based on number of patients. 2: percent based on number of fractures. 3: percent based on number of non-missing values. †P-values are from the Fisher exact test, *Chi-square test, or **Kruskal-Wallis test.
Of the 19 fractures in the plate-only group, five were Vancouver B1, one Vancouver B2, and 13 Vancouver C. Eighteen of these fractures were treated with plate-only, and one fracture was treated with revision arthroplasty in addition to plate fixation. In the group without cerclage cables, there were 11 females and 8 males. The average age at surgery was 67.3, and the mean BMI was 29.6. When comparing the demographic data between the group with cables vs without cables (Table 1), there were no significant differences observed for age (P = .15), sex (P = .94), race (P = 1.0), BMI (P = .64), state ADI (P = .52), or national ADI (P = .47). There was a difference in fracture classification between groups (P = .003), with a higher percentage of Vancouver B fractures (83% of 23) in the cerclage group and more Vancouver C fractures (68% of 19) in the group without cables. In comparing comorbidity data between the group with cables vs without cables, there were no significant differences observed for tobacco usage (P = .61), diabetes (P = .70), peripheral vascular disease (P = 1.0), or chronic kidney disease (P = 1.00).
Postoperatively, patients were mobilized, and weight-bearing restrictions varied between surgeons: out of the 42 cases, 14 were 50% weight-bearing (WB), 10 were touch-down WB, 10 were non-WB, and 8 were WB as tolerated.
The average follow-up for all patients was 15.1 months. In the cerclage group, follow-up was 11.5 months on average, ranging from 3 weeks to 42 months. In the plate-only group, the average follow-up was 19.4 months, ranging from 2.2 to 74 months. Five patients had incomplete follow-up: four in the cerclage group and one in the plate-only group.
There were no observed cerclage cable failures or complications unique to the 1.0 mm cerclage cables at the most recent follow-up. There was a higher nonunion rate in the plate-only group, 16% (3/19) vs 9% (2/23) in the cerclage group; however, this difference failed to reach significance (P = .64). When radiographic union was observed, the times to union had an average ± SD of 6.0 ± 3.8 months among 17 cerclage-cable unions, vs 8.0 ± 4.9 months among 15 plate-only unions, although this too failed to reach significance (Gray’s test P = .12). This is plotted in Figure 7, demonstrating the time to radiographic healing with nonunion and incomplete follow-up as competing events. In each group there were 3 patients that required reoperations (P = 1.00).
Figure 7.
Proportion of individuals healed vs time to fracture union, showing a quicker time to heal and higher percentage of cases resulting in union for the cerclage-cable group (P = .12). “Lost to FU” means lost to follow-up.
The overall complication rate for the cerclage group was 13% (3/23). In addition to the two nonunions, there was one patient with a loose femoral prosthesis, with all three femurs requiring reoperation. Both nonunions occurred in patients with Vancouver B1 fractures. The first, occurring at three months post-operation, was a high-energy, comminuted fracture. Failure occurred at the transverse portion of the fracture near the tip of the stem. Proximally, the cerclage cable maintained reduction of the oblique portion of the fracture around the prosthesis. This also resulted in hardware failure, as the plate was pulled off the bone. The second nonunion, which occurred around a revision stem without hardware failure, was observed at 11 months post-operation. The patient developed pain at the fracture site, and CT confirmed nonunion. Immediately after the patient’s index surgery, the patient was referred to endocrinology for osteoporosis and Vitamin D deficiency and started supplementation. The third complication occurred in a Vancouver B2 fracture who developed a subsided femoral prosthesis two months post-operation, despite having a radiographically healed fracture.
In the plate-only group, the overall complication rate was 16% (3/19) and included three nonunions with hardware failure; two of these nonunions had broken plates and all three cases with complications required reoperations. The first case with a complication occurred at 8 months post-operation in a patient with a high-energy, comminuted, Vancouver C fracture. Prior to plate fracture at the nonunion, the patient was electively bone-grafted for a large bone defect associated with the initial injury. The second was a nonunion with plate fracture, occurring in a patient with a Vancouver B1 fracture at 6 weeks post-operation despite no falls or trauma. The third complication was a nonunion occurring at 7 months post-operation in a Vancouver C fracture. Radiographs demonstrated screw pullout as early as 2 months post-operation, and there was ultimately a loss of fixation.
Tables 2 and 3 demonstrate rates of implant failure and reoperations between groups. Prosthesis loosening was not included as implant failure but was included as a complication requiring reoperation. There was no significant difference between observed rates of implant failure (P = .64) or reoperation (P = 1.0) between groups.
Table 2.
Implant Outcomes.
| Post-Surgical Implant Failure | |||||||
|---|---|---|---|---|---|---|---|
| No | Yes | Total | Fisher’s | ||||
| Hips | % of Total | Hips | % of Total | Hips | % of Total | Exact P | |
| Both Groups | 37 | 88 | 5 | 12 | 42 | 100 | |
| Type of THA | .644 | ||||||
| THA w/Cables | 21 | 91 | 2 | 9 | 23 | 100 | |
| THA w/out Cables | 16 | 84 | 3 | 16 | 19 | 100 | |
THA, Total Hip Arthroplasty.
Table 3.
Reoperation Outcomes.
| Was a Re-Operation Required? | |||||||
|---|---|---|---|---|---|---|---|
| No | Yes | Total | Fisher’s | ||||
| Hips | % of Total | Hips | % of Total | Hips | % of Total | Exact P | |
| Both Groups | 36 | 86 | 6 | 14 | 42 | 100 | |
| Type of THA | 1.000 | ||||||
| THA w/Cables | 20 | 87 | 3 | 13 | 23 | 100 | |
| THA w/out Cables | 16 | 84 | 3 | 16 | 19 | 100 | |
THA, Total Hip Arthroplasty.
Discussion
In our comparison of 23 PPFFx treated surgically with a cerclage-cable construct and 19 PPFFx treated with plate-only, we observed more nonunions, a longer time to radiographic healing, and higher overall rates of complications in the group without cables. Three out of nineteen fractures (16%) treated without cables developed nonunion, two of which had associated plate breakage. Two out of twenty-three fractures (9%) treated with cables developed nonunion, one of which had a plate breakage. The group without cables had an average time to union of 8.0 months compared to a shorter time to union of 6.0 months in the group with cables. Although these differences between groups failed to reach statistical significance, we believe this is clinically relevant. These results suggest that the application of the cerclage cable provided a stable peri-implant construct that did not appear to have a detrimental effect on fracture healing. Furthermore, there were no complications directly associated with the application of the cerclage cables, and overall complication rate requiring reoperation was low.
There are several biomechanical studies demonstrating mixed results comparing various methods of fixation in PPFFx, which is not always feasible in the setting of an intramedullary implant. In these situations, cerclage-cable constructs can add stability to fixation, often combined with locking plate fixation.16-19 Current literature directly comparing clinical outcomes of PPFFx treated with and without the addition of cerclage cables is limited. In Ebraheim et al’s study, 47 patients with PPFFx around both THA and total knee arthroplasties (TKA) were treated after low energy, ground level falls. Twenty-four of these patients (10 THA and 14 TKA) were treated with a single lateral locking plate, and 23 patients (21 THA and 2 TKA) were treated with plate and cerclage cables. In their study, two cables were added above and below the fracture after the application of plate and screws to aid in overall construct stability which differed from our technique in which cables were applied first to maintain fracture reduction. They observed no difference in overall union rate (95.8% plate group vs 95.7% plate + cable group). 20 There was, however, a significant difference observed in time to union: 4.8 +/− 2.6 months in the plate-only group and 3.6 +/− 1 month in the plate and cerclage group (P = .046). 20 Four patients without cables required revision surgery due to screw pull-out and failed fixation. They concluded that the cerclage cables increased the stability of fixation, and if applied at the time of index procedure, would have prevented revision surgery. 20 Their study was conducted retrospectively with a small sample size and had an additional limitation of lack of fracture complexity as they included several fractures described as nondisplaced. Our study demonstrated similar trends in union rate and time to union while contributing several high-energy, complex fractures, some of which also required revision surgery in addition to fixation. In our cerclage group, nonunions were observed in only two instances. The first, a high energy comminuted Vancouver B1 fracture with failure occurring at the transverse portion of the fracture near the tip of the stem, a known high-risk pattern with nonunion rates documented as high as 42.9% in one study. 21 The second nonunion occurred in a Vancouver B1 fracture around a revision stem in a patient with significant, neglected osteoporosis, yet another well-known risk for nonunion. 22 More recently, Malige et al reviewed the surgical fixation of Vancouver B fractures utilizing no cerclage cables, cerclage-only with revision arthroplasty, and combination of cerclage and plate fixation in a multicenter study including 295 patients. They similarly found no differences in nonunion rates or time to union between the groups. 14 They did however find an association between older age and females and higher union rates. 14 In addition to these studies, our series further supports that cerclage cables offer a stable construct without compromising fracture healing while also adding complex PPFFx.
Along with adding construct stability, cerclage cables are particularly useful to achieve and maintain reduction in PPFFx. Traditionally, this is achieved via a direct, open approach such as in this study. Historically, this has been viewed as a dangerous insult to the biology, resulting in significant soft tissue and periosteal stripping, increasing the risk for bone necrosis and nonunion. 5 Proposed mechanisms for this include contact between the cerclage and bone surface, the strangulation of periosteal blood vessels, and the “gigli saw” or cutting effect from passing the cerclage around the bone.23,24 However, a deeper understanding of the blood supply suggests that blood flow through the cortex is centrifugal and circumferential from the medulla to the periosteum.5,25 Cadaveric studies have further supported that there is adequate femoral perfusion through compensatory anastomosis channels with the use of cerclage cables.12,13 It is proposed the greater threat to the biology instead comes from excessive soft tissue stripping during fracture exposure. 13 Although this was our preferred technique, care was taken to avoid extended stripping of the soft tissues during exposure and cables were passed meticulously to avoid moving the cable up and down the bone while only placing the cables tight enough to hold the reduction. Our results suggest that this approach did not have a deleterious effect on the local fracture biology to hinder fracture healing. Several other studies have also demonstrated this technique to be effective for other challenging fracture patterns about the femur. Lee et al compared the clinical and radiographic results of geriatric spiral, wedge, and oblique distal femoral fractures treated with open reduction and cerclage wiring combined with locked plate to locked plates alone and found no differences. 26 Similarly, Wang et. Al utilized the same cerclage technique in comminuted femoral shaft fractures, and found no differences in union rates. 27 A meta-analysis on subtrochanteric and reverse oblique intertrochanteric femur fractures associated shorter time to union, lower rates of mal-reduction, and lower rates of complications requiring reoperation with fractures treated with cerclage and intramedullary nail (IMN) compared to those treated with IMN alone. 28 These studies further highlight the role for cerclage in any segment of the femur.
While the subject remains a point of debate, more biologically friendly approaches have been described. Minimally invasive plate osteosynthesis (MIPO) describes a closed reduction by indirect methods with the application of a plate sub-muscularly via smaller proximal and distal incisions, preserving fracture hematoma, periosteum, and soft tissues. 29 Mini-open approaches can be viewed as a hybrid between traditional open and MIPO by adding a third small incision at the level of the fracture. 30 While these studies have certainly shown equivalent radiographic and clinical outcomes while also significantly reducing operation time and blood loss, these techniques are technically challenging and may potentially increase the risk of malunion and fixation failure necessitating reoperation.29-31 Some limitations of the MIPO approach specific to treating PPFFx are highlighted in Byung-Woo, et al’s study comparing MIPO and traditional ORIF with locking compression plate in Vancouver B1 fractures. Twenty-one patients with Vancouver B1 PPFFx were treated utilizing the MIPO technique with locking compression plate (LCP) and a minimum one-year follow-up. These patients were retrospectively compared to a similar group of patients treated with traditional ORIF. Results demonstrated equivalent radiographic and clinical outcomes and the only complication observed in the MIPO group was fixation failure with stem subsidence. 32 Authors determined stem stability by comparing radiographs before and after injury, admitting that it can be difficult to differentiate between Vancouver B1 and B2 fractures on imaging alone. Another limitation in this approach realized by authors was the inability to achieve indirect reduction of transverse and short oblique fractures occurring close to the tip of the stem. 32 In several cases, this required conversion to an open approach for reduction. These fractures have been noted to have a high degree of instability and complications including nonunion and plate fracture.21,33 Additionally, while utilizing less invasive approaches, these studies still employed cerclage cables to facilitate fracture reduction percutaneously. It is important to highlight that, while this technique is thought to lower the biologic insult, it is not without additional risk. Several case reports have been published presenting cases of iatrogenic injury to the femoral artery including deep and superficial branches as well as the sciatic nerve with percutaneous application of cerclage cables.6-8 One cadaveric study even highlights the variability that exists in the deep perforator arterial supply and suggests that there is no definitive safe zone along the posteromedial aspect of the body of the femur from 14 cm to 36.5 cm distal to the anterior superior iliac spine. 34 Our approach in PPFFx addresses these concerns by allowing direct assessment of prosthesis stability, visualization for anatomic reductions around the tip of the stem, and safe application of cerclage wires, minimizing risk for iatrogenic neurovascular injury.
Limitations of this consecutive case series are inherent to the retrospective nature, small sample (42 total cases), and short-term average follow-up (15.1 months). A retrospective study design was used to maximize the number of patients included over a 7-year period. Still, the sample size was small and no power analysis was done to determine an optimal sample size, which may have limited the ability to reliably detect significant differences if they were present. Having long term follow up is important in this setting as potential complications not previously mentioned such as fraying, third-body generation, and accelerated wear of the bearing surface of the prothesis can take some time before becoming clinically apparent. 10 There was also a difference in fracture types between groups. The cerclage group consisted of 83% Vancouver B type fractures and the plate-only group consisted of 68% Vancouver C type fractures. Distal femur fractures treated with lateral locked plates, such as the Vancouver C fractures in our series, have demonstrated reoperation rates of 19% for nonunion. 35 Techniques such as nail plate combination and distal femur replacement have been developed to address high failure rates associated with these complex fractures in patients with osteoporosis.36,37 This may have contributed to selection bias and contributed to the higher nonunion rate in the plate-only group of our study. In addition, our series consisted of multiple surgeons with varying decision making. Therefore, the number and location of cerclage cables used was variable and resulted in lack of uniform treatment between cases.
Conclusion
In conclusion, this study suggests that 1.0 mm cerclage cables are a useful option to hold reduction, and they allow for easy plate placement over the top of the cable. This facilitates further placement of screws around the stem of the prosthesis in the treatment of complex PPFFx. When applied via a traditional open approach, cables can safely be used as a reduction aid while providing a stable fixation with no increased nonunion risk or cable breakage. Although the most common complication remained nonunion, this was at a low rate, and there were no associations with cerclage cable use. While this is valuable initial data, further prospective studies or multicenter studies with larger sample sizes are needed to enhance the reliability of the results.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Consent to participate:Not applicable; this study is retrospectiveConsent for publication:Not applicableDeclaration of conflicting interest:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. The project described was supported in part by the Translational Research Institute (TRI), grant UL1 TR003107 through the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. In addition, the Bill and Betty Petty Research Fund at the University of Arkansas for Medical Sciences supported this work.
Ethical Statement
Ethical Approval
Institutional Review Board approval was granted before beginning data collection and manuscript preparation.
ORCID iDs
Simon C. Mears https://orcid.org/0000-0002-0068-0283
Eric R. Siegel https://orcid.org/0000-0001-9824-6612
Jeffrey B. Stambough https://orcid.org/0000-0003-0950-5227
References
- 1.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780-785. [DOI] [PubMed] [Google Scholar]
- 2.Brady OH, Garbuz DS, Masri BA, Duncan CP. The reliability and validity of the Vancouver classification of femoral fractures after hip replacement. J Arthroplasty. 2000;15(1):59-62. [DOI] [PubMed] [Google Scholar]
- 3.Angelini A, Battiato C. Past and present of the use of cerclage wires in orthopedics. Eur J Orthop Surg Traumatol. 2015;25(4):623-635. [DOI] [PubMed] [Google Scholar]
- 4.Dennis MG, Simon JA, Kummer FJ, Koval KJ, DiCesare PE. Fixation of periprosthetic femoral shaft fractures occurring at the tip of the stem: a biomechanical study of 5 techniques. J Arthroplasty. 2000;15(4):523-528. [DOI] [PubMed] [Google Scholar]
- 5.Perren SM, Fernandez Dell'Oca A, Lenz M, Windolf M. Cerclage, evolution and potential of a Cinderella technology. An overview with reference to periprosthetic fractures. Acta Chir Orthop Traumatol Cech. 2011;78(3):190-199. [PubMed] [Google Scholar]
- 6.Orapiriyakul W, Chewakidakarn C, Dissaneewate K, Dissaneewate P, Kritsaneephaiboon A. Silent iatrogenic pseudoaneurysm after intertrochanteric fracture fixation with proximal femoral nailing and cerclage wiring: case report and review of literature. Eur J Orthop Surg Traumatol. 2023;33(6):2667-2681. [DOI] [PubMed] [Google Scholar]
- 7.Devendra A, Avinash M, Chidambaram D, Dheenadhayalan J, Rajasekaran S. Vascular injuries due to cerclage passer: relevant anatomy and note of caution. J Orthop Surg. 2018;26(1):2309499018762616. [DOI] [PubMed] [Google Scholar]
- 8.Nakamura Y, Tada K, Murai A, Tsuchiya H. Iatrogenic sciatic nerve injury due to cerclage wiring for proximal periprosthetic femoral fracture: a rare case report. JPRAS Open. 2022;32:54-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Silverton CD, Jacobs JJ, Rosenberg AG, Kull L, Conley A, Galante JO. Complications of a cable grip system. J Arthroplasty. 1996;11(4):400-404. [DOI] [PubMed] [Google Scholar]
- 10.Speranza A, Massafra C, Pecchia S, Di Niccolo R, Iorio R, Ferretti A. Metallic versus non-metallic cerclage cables system in periprosthetic hip fracture treatment: single-institution experience at a minimum 1-year follow-up. J Clin Med. 2022;11(6):1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Direder M, Naß C, Andresen JR, et al. Distal femoral fractures: periprosthetic fractures have four times more complications than non-periprosthetic fractures and cerclage should be avoided: retrospective analysis of 206 patients. J Orthop Traumatol. 2024;25(1):41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Forsh S, Sandriesser S, Fenwick A, Mayr E. Impairment of the blood supply by cerclages: myth or reality? An overview of the experimental study situation. Unfallchirurg. 2021;124:231-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Apivatthakakul T, Phaliphot J, Leuvitoonvechkit S. Percutaneous cerclage wiring, does it disrupt femoral blood supply? A cadaveric injection study. Injury. 2013;44(2):168-174. [DOI] [PubMed] [Google Scholar]
- 14.Malige A, Beck M, Mun F, Goss M, Boateng H, Nwachuku C. Stabilization of Vancouver B periprosthetic femur fractures with cerclage wiring: a retrospective chart review. Cureus. 2022;14(5):e25063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kind AJH, Buckingham W. Making neighborhood disadvantage metrics accessible: the neighborhood atlas. N Engl J Med. 2018;378:2456-2458. University of Wisconsin School of Medicine Public Health. 2015 Area Deprivation Index v2.0. Downloaded from: https://www.neighborhoodatlas.medicine.wisc.edu (23 May 2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Graham SM, Mak JH, Moazen M, et al. Periprosthetic femoral fracture fixation: abiomechanical comparison proximal locking screws and cables. J Orthop Sci. 2015;20(5):875-880. [DOI] [PubMed] [Google Scholar]
- 17.Lewis GS, Caroom CT, Wee H, et al. Tangential bicortical locked fixation improves stability in Vancouver B1 periprosthetic femur fractures: a biomechanical study. J Ortho Trauma. 2015;29:e364-e370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lenz GS, Perren SM, Gueorguiev B, et al. A biomechanical study on proximal plate fixation techniques in periprosthetic femur fracturs. Injury. 2014;45:S71-S75. [DOI] [PubMed] [Google Scholar]
- 19.Griffiths JT, Taheri A, Day RE, Yates PJ. Better axial stiffness of a bicortical screw construct compared to a cable construct for comminuted Vancouver B1 proximal femoral fractures. J Arthroplasty. 2015;30:2333-2337. [DOI] [PubMed] [Google Scholar]
- 20.Ebraheim NA, Sochacki KR, Liu X, Hirschfeld AG, Liu J. Locking plate fixation of periprosthetic femur fractures with and without cerclage wires. Orthop Surg. 2013;5(3):183-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Min B-W, Lee K-J, Cho C-H, Lee I-G, Kim B-S. High failure rates of locking compression plate osteosynthesis with transverse fracture around a well-fixed stem tip for periprosthetic femoral fracture. J Clin Med. 2020;9(11):3758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gausden EB, Bedard NA, Gililland JM, Haidukewych GJ. What’s new in periprosthetic femur fractures? J Arthroplasty. 2024. [DOI] [PubMed] [Google Scholar]
- 23.Bliemel C, Anrich D, Knauf T, et al. More than a reposition tool: additional wire cerclage leads to increased load to failure in plate osteosynthesis for supracondylar femoral shaft fractures. Arch Orthop Trauma Surg. 2021;141:1197-1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Angelini A, Battiato C. Combination of low-contact cerclage wiring and osteosynthesis in the treatment of femoral fractures. Eur J Orthop Surg Traumatol. 2016;26:397-406. [DOI] [PubMed] [Google Scholar]
- 25.Pazzaglia UE, Congiu T, Raspanti M, Ranchetti F, Quacci D. Anatomy of the intracortical canal system: scanning electron microscopy study in rabbit femur. Clin Orthop Relat Res. 2009;467(9):2446-2456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee JH, Park KC, Lim SJ, Kwon KB, Kim JW. Surgical outcomes of simple distal femur fractures in elderly patients treated with the minimally invasive plate osteosynthesis technique: can percutaneous cerclage wiring reduce the fracture healing time? Arch Orthop Trauma Surg. 2020;140:1403-1412. [DOI] [PubMed] [Google Scholar]
- 27.Wang TH, Chuang HC, Kuan FC, et al. Role of open cerclage wiring in patients with comminuted fractures of the femoral shaft treated with intramedullary nails. J Orthop Surg Res. 2021;16(1):480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hantouly AT, Salameh M, Toubasi AA, et al. The role of cerclage wiring in the management of subtrochanteric and reverse oblique intertrochanteric fractures: a meta-analysis of comparative studies. Eur J Orthop Surg Traumatol. 2023;33(4):739-749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, Tscherne H. Minimally invasive plate osteosynthesis: does percutaneous plating disrupt femoral blood supply less than. The traditional technique? J Orthop Trauma. 1999;13(6):401-406. [DOI] [PubMed] [Google Scholar]
- 30.De Fortuny LM, Leal AC, Sanchez-Soler JF, Martinez-Diaz S, Leon A, Lopez FM. Mini-invasive approach vs. traditional open reduction for periprosthetic hip fracture osteosynthesis with the NCB plate. Injury. 2023;54(2):706-711. [DOI] [PubMed] [Google Scholar]
- 31.Zlowodzki M, Vogt D, Cole PA, Kregor PJ. Plating of femoral shaft fractures: open reduction and internal fixation versus submuscular fixation. J Trauma. 2007;63(5):1061-1065. [DOI] [PubMed] [Google Scholar]
- 32.Min B-W, Cho C-H, Son E-S, Lee K-J, Lee S-W, Min K-K. Minimally invasive plate osteosynthesis with locking compression plate in patients with Vancouver type B1 periprosthetic femoral fractures. Injury. 2018;49(7):1336-1340. [DOI] [PubMed] [Google Scholar]
- 33.Graham SM, Moazen M, Leonidou A, Tsiridis E. Locking plate fixation for Vancouver B1 periprosthetic femoral fractures: a critical analysis of 135 cases. J Orthop Sci. 2013;18(3):426-436. [DOI] [PubMed] [Google Scholar]
- 34.Pretterklieber B, Pablik E, Dorfmeister K, Pretterklieber ML. There are no safe areas for avoiding the perforating arteries along the proximal part of the femur: a word of caution. Clin Anat. 2020;33(4):507-515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ricci WM, Streubel PN, Morshed S, Collinge C, Nork SE, Gardner MJ. Risk factors for failure of locked plate fixation of distal femur fractures: an analysis of 335 cases. J Orthop Trauma. 2014;28(2):83-89. [DOI] [PubMed] [Google Scholar]
- 36.Liporace FA, Tang A, Jankowski JM, Yoon RS. Distal femur: nail plate combination and the linked construct. OTA Int. 2022;5(3):e172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bettin CC, Weinlein JC, Toy PC, Heck RK. Distal femoral replacement for acute distal femoral fractures in elderly patients. J Orthop Trauma. 2016;30(9):503-509. [DOI] [PubMed] [Google Scholar]