Abstract
Background
In April 2019, Mozambique was hit by Cyclone Idai leaving substantial damage to infrastructure and nearly two million people in need of humanitarian assistance. Malaria risk has been associated with living in a rural setting, vicinity to water, and household structure, all factors which are impacted by severe storms. This study quantified the association between damage to infrastructure (health care facilities and schools) following Cyclone Idai and malaria outcomes: malaria incidence, severe malaria, and administration of intermittent preventative treatment in pregnancy (IPTp) in Sofala Province, Mozambique.
Methods
To quantify infrastructure damage, historical satellite imagery was assessed visually using Google Earth Pro®. Damage to 66 school and 105 health centres was assessed for severity and duration. Location data was imported to QGIS and joined with district level data on malaria outcomes and environmental covariates. Multivariable Poisson regression models were used to quantify the associations between facility damage and malaria incidence and severe malaria. Generalized linear models were used to determine the association between facility damage and changes in malaria incidence and administration of IPTp from 2018 to 2019.
Results
An increase in facility damage was associated with an increase in malaria incidence and severe malaria. An increase in proportion of facilities damaged by 10% was associated with a 7.3% (95% CI 6.8–7.8%) increase in malaria incidence. Risk of severe malaria was 2.16 (95% CI 1.42–3.32) times higher in districts with any damage compared to those with no damage. However, proportional facility damage was associated with decreased malaria incidence and increased access to IPTp from 2018 to 2019, but these were not statistically significant.
Conclusion
An increase in proportion of facilities damaged following Cyclone Idai was associated with increased risk of malaria and severe malaria at the district level. This may be a function of decreased access to healthcare and an increased exposure to risk factors for malaria. A non-statistically significant decrease in malaria incidence was also found at the district level from 2018 to 2019, indicating that malaria may have been underreported in 2019, likely again a function of decreased access to healthcare.
Background
On March 14, 2019, Cyclone Idai made landfall in Mozambique’s second largest city, Beira, making its way through Mozambique’s Sofala province into Manica province and eventually into Zimbabwe. Following Cyclone Idai, it was estimated that across Mozambique 1.85 million people were in need of urgent humanitarian assistance [1]. Destruction of homes, and flooding led to immediate displacement of families, leading to a higher risk of injury, and increased food insecurity. These factors compound on each other, increasing the risk of morbidity and mortality in areas most impacted by the storm. Increased malnutrition, poor housing quality, and exposure to nearby bodies of water are risk factors of malaria [2, 3]. Following Cyclone Idai, UNICEF expressed concerns regarding the risk of increased malaria incidence. In an effort to curb the anticipated increase in malaria cases, efforts to distribute insecticide-treated bed nets (ITNs), conduct indoor residual spraying of insecticide (IRS) and import additional malaria treatment in areas affected by the cyclone began [4, 5].
The World Health Organization (WHO) has a goal of 90% reduction in malaria incidence and elimination in 35 countries [6]. Mozambique accounts for 4% of global malaria cases with a countrywide prevalence of 32% as of 2020 [7]. The national prevalence of malaria is down from 49% in 2000, however increased from 30% in 2019 [7]. The prevalence of malaria in Mozambique’s Sofala Province was 31% in 2011 and in 2018 the prevalence of malaria in children under five was 29% [8, 9]. Malaria is considered endemic to Mozambique, but follows seasonal trends of the wet and dry season with more cases occurring in the wet season between November and March [10]. Understanding changing dynamics in malaria transmission that may occur following severe weather are essential to limit the burden of and control malaria in Mozambique. There is evidence that a combination of factors, including rising sea levels are leading to more severe tropical storms coming out of the Indian ocean [11]. Parts of eastern Africa saw increased rainfall throughout 2019, which was attributed to rising surface water temperatures throughout the Indian ocean [12]. Assuming changing weather patterns will continue to impact malaria transmission, it is important to understand the association between severe storms and malaria transmission in order to lead successful malaria control campaigns.
Following Cyclone Idai, the number of people in need of humanitarian assistance was indicative of those living without the normal safety of their home and subsequent protection from elements and mosquitoes. Living in a rural setting has been established as a risk factor for malaria with those in a rural setting having a near three-fold increase in their risk of malaria [8]. Defining a rural and urban setting can be challenging, but factors which can be considered in Mozambique include: access to healthcare, proximity to nearby water, and housing quality. The damage resulting from Idai put people living in an urban environment at risk for exposure to factors associated with malaria more often associated with rural communities. Living in a house with a thatched roof, earth floors, or mud walls is associated with an increased risk in malaria transmission compared to more modern housing [13]. According to the 2007 census, 21.4% of residents in Sofala were living in houses with a modern roof and only 15.8% were living in houses with modern walls [14]. Comparatively, in Beira District, 90.1% were living in a house with a modern roof and 59.6% were living in a house with modern walls [14].
Access to nearby healthcare is concern in the risk of the progression to severe malaria. A study completed in Yemen found that living further than two kilometres or a ten minute drive from a healthcare facility can lead to an increased risk for a severe malaria infection [2]. Prior to cyclone Idai, 50% of people in Mozambique lived further than 20 km from the nearest health centre [15]. Petricola et al. [16] determined that up to 1.03 million people across Mozambique saw increased walking times to health facilities, in some cases over five hours, and up to 800 thousand individuals saw an increase in drive time to a health facility following Idai. Damage to general infrastructure increased travel time to a health centre further increasing this burden following Idai [15]. Along with damage to general infrastructure, observed damage to healthcare facilities meant that the few health care facilities were no longer accessible following Idai, further decreasing access to healthcare in affected areas. Decreased access to healthcare following Idai may have contributed to the burden of malaria in Mozambique’s Sofala province due to an increased risk of severe malaria.
It is feasible to expect that the prevalence of malaria in Sofala was impacted by Cyclone Idai as a result of increased exposure to malaria risk factors. Reports expressed that there was an increase in malaria cases following the cyclone, however there are limitations in the quantification of these statements. UNICEF reported nearly 15,000 cases of malaria in Sofala province in the month following Idai as well as concerns of increase transmission due to excessive standing water; another source cited an “increased wave of infection” [5, 15]. Mugabe et al. [15] showed that in the months following Idai there was a decrease in suspected malaria cases compared to 2018 for four districts within Sofala. This was followed by a peak in suspected cases in May and June for these four districts, but there was not consistent evidence that case numbers through the year differed from 2018 numbers in each district. Challenges to properly quantifying incident malaria cases immediately following Idai may have also been a function of decreased access to healthcare and subsequent underreporting of infections.
This study focused on the damage to healthcare facilities and schools as a proxy for general infrastructure damage as well as a mechanism to model access to healthcare. The primary goal was to quantify how damage to infrastructure following cyclone Idai may have impacted susceptibility to malaria infection. Additionally, as damage to healthcare facilities was assessed as a predictor for malaria incidence, inferences can be drawn regarding decreased access to healthcare following cyclone Idai and malaria outcomes. Decreased access to healthcare, due to damaged facilities, was assessed as a predictor of severe malaria as well as completion of preventative treatment in pregnant people. All analysis of malaria related outcomes and their association with damage to facilities was completed at a district level.
Methods
Data collection
The primary exposure of interest analysed was damage to schools and health care facilities. A list of schools within Sofala Province was acquired from Open Street Maps and a list of health care facilities was acquired from a database published by Maina et al. assembled and published in 2019 [17]. These databases were used as a starting point for clinics and schools within the province; further inspection in Google Earth Pro® found that some GPS points representing clinics in this source appeared multiple times or the GPS locations did not fall on or near a clinic. The list of schools was limited and mostly covered schools in or near Beira. To supplement this list a search for “Schools” and “University” was completed in Google Earth Pro® [18]. Each point from Open Street Maps was examined, if there was not a health centre or school clearly associated with the GPS point a search was completed in Google Earth Pro® for that location by name. Additionally, if there was a clinic or school which was not in the Open Streets database but did show up while visually scanning Sofala province a point was marked, and the school or clinic was recorded. Each point associated with a school or health centre was labelled with a point marker in Google Earth Pro®. Each point was assigned unique identifying number in the order that they were assessed, and the facility name was recorded.
Analysis of damage to health centres and schools was assessed using historical satellite imagery available in Google Earth Pro®. Imagery of buildings from March 2019 or earlier was compared to imagery from April 2019 or later for evidence of either damage to a roof or clear evidence that a new roof had been installed shortly following the storm. Damage to the roof was qualified as clearly missing portions of the roof or if there were sections of the roof which were clearly new, such as brighter colored roofing material compared to older images or the rest of the roof (Fig. 1). Damage to buildings was assessed and categorized as no damage, minimal damage, partial damage, nearly complete damage, or complete damage. The time in months until evidence of complete repair was also recorded. For the purposes of this study, the maximum value for time until repair was 8 months which was the time (in months) after the storm to the end of the analysis period, December 2019. There was evidence that some buildings took much longer to repair, and others did not have satellite imagery showing evidence of repair following the storm as of December 2022. Additional notes such as cloud cover or new buildings being added to a facility were also recorded.
Fig. 1.

Pre and Post Cyclone Imagery of a rural health centre in Nhangau, Mozambique. Image A is taken from satellite imagery in March 2019 prior to Cyclone Idai. Image B was taken in July 2019 following the cyclone. There was blurry imagery from April 2019 that did not clearly depict the buildings. This is one of the buildings with insufficient imagery displaying damage, but there is clear evidence that the roof has been replaced due to damage
The highest quality imagery was available near population centres, such as Beira, (Fig. 2) where the imagery was higher resolution and more frequent. Areas that were less populated had lower resolution and less frequent imagery (Fig. 1). In these instances, evidence of new roofing was often used to assess if there had been damage following the storm. Figures 1 and 2 are both examples of facilities that were qualified as “complete damage” as there was evidence that the entire roof was lost (Fig. 2) or had been replaced (Fig. 1). Coordinates for each location were also recorded. The dataset assessing the damage to all facilities in Sofala province was imported into QGIS [19]. This was overlayed onto a map of districts within Sofala Province. The two layers were joined by location creating a new datafile. Health care facilities and schools were linked to their respective district for analysis. Each district had data for number of schools, number of health facilities, and number of facilities damaged. To aggregate damage data for the district level, damage to facilities was assessed as a binary variable: damaged or not damaged.
Fig. 2.

Pre and Post Cyclone Imagery of University in Beira, Mozambique. Image A is taken from satellite imagery in March 2019 prior to Cyclone Idai. Image B was taken in April 2019 immediately following the cyclone. Here there is clear evidence of complete damage to this facility following the storm
Malaria outcomes were extracted from the publicly available National Malaria Control Program Annual Report for Sofala Province [20]. These data are collected by local health facilities in Mozambique documenting weekly malaria case data which are then sent to district offices. This information is then sent to the Provincial health office, aggregated to monthly data and is reported in the annual report [20]. Annual incidence was then calculated using data from the 2017 census [21]. The data on malaria outcomes was reported at the district level for 2019 with some outcomes being reported for 2018 for comparison purposes. The malaria data used for this analysis was the district level monthly aggregated data.
Environmental factors were also collected as additional covariates. These were all factors that are known to be associated with survival of Anopheles mosquitoes and subsequentially malaria infection. These factors included density of rivers, land use, vegetation density, and elevation. Elevation data was extracted from United States Geological Survey (USGS) and joined with the district map of Sofala province in QGIS. The median elevation was calculated for each district. River data was imported into QGIS and the length of each river was calculated [22]. This was then joined with the district shapefile. The area of each district was also calculated in QGIS and river density (metres/km2) was calculated using SAS.
To analyse vegetation density in each district a vegetation density file was downloaded from the United States Geological Survey Earth Explorer tool [23]. This was a raster file which contained vegetation density data averaged from April 6th to April 15th 2019. The file was a Landsat Normalized Difference Vegetation Index (NDVI) file which measures vegetation density by greenness with a value ranging from − 10,000 to 10,000. This file was imported to QGIS, and the median greenness value was calculated for each district.
The final environmental factor assessed was land use. A shapefile downloaded through USGS contained polygons which were each classified by the use of that land. The original shapefile contained 30 different classifications, all types that were applicable to Sofala Province were reclassified to one of seven different classes in QGIS: cropland, shrubland, deciduous forest, flood-land, urban space, bare land, and water. Once reclassified, this shapefile was joined to the shapefile of the districts. Due to how the original land use file was created there were some large polygons which covered area in adjacent districts. This led to values of greater than 100% land usage per district in some districts when trying to aggregate land usage to the district level. In order to assess land use in each district, the frequency of each reclassified polygon per district was used as an aggregate measure of land use.
Household and demographic variables were aggregated to the district level to adjust for additional covariates known to be associated with malaria infection. Demographic data was extracted from the 2007 Mozambique census which was accessed through IPUMS International [14]. The following variables were extracted from the 2007 census: age, presence of a toilet, floor type, roofing material, and wall material. House structure characteristics were reclassified from multiple levels that had been taken in the census to binary variables. Flooring was classified as unfinished or finished (cement, wood, marble, tile, other finished). Roofing was classified as modern (concrete, tile, asbestos, zinc, or tin) or not modern (thatch or none). Walls were classified as modern (brick, cement, adobe, or other) or not modern walls (plastic sheeting, cardboard, wood, straw, reed, bamboo, or palm). Toilets were classified as yes (flush toilet or latrine) or no toilet. For each district a proportion with each household characteristic was calculated based on the 2007 population data. The median age was also calculated for each district.
Analysis
Analysis for the association between damaged facilities and malaria outcomes was completed at the district level. This covered the 13 districts in Sofala Province. Exploratory data analysis was completed using univariable models to determine the association between the main predictors (damage) and environmental covariates with each malaria outcome. The three outcomes assessed were: 2019 annual malaria incidence, 2019 severe malaria incidence, and percent of pregnant people who received a second dose of IPTp in 2019.
Both malaria incidence and severe malaria incidence were analysed using Poisson regression. Proportion of people who received IPTp was analysed using a generalized linear model which assessed the association between each covariate. Each of the models was adjusted for the X and Y coordinate value for the centroid of each district in order to account for spatial correlation between districts.
To assess demographic features of each district, median age, and proportion of people under 5 years old were analysed. To assess household characteristics, presence of a toilet, flooring type, flooring material, and wall material were analysed. To assess environmental factors, NDVI, elevation, proportion of land qualified as water, proportion of land qualified as flood land, and river density were analysed. Additionally, when modelling IPTp coverage as an outcome population density was considered as another variable to adjust for access to healthcare. This was not used in the models for malaria incidence as the Poisson models used include an offset variable accounting for population.
The primary predictors of interest were the variables assessing damage to healthcare facilities and schools. For univariable analyses, there were six different representations of facility damage assessed. The proportion of health facilities damaged, proportion of schools damaged, and proportion of all facilities damaged were each modelled as a predictor. The aggregate measure of facilities damaged was also modelled using a binary representation if there was any damage to facilities within the district. The mean time to facility repair across districts was also calculated and modelled as a predictor. Finally, the level of damage previously assigned to each facility was quantified. Facilities with no damage were given a value of “0” ranging to “4” if a facility was completely damaged. The mean value of damage was calculated for each district and modelled as a predictor.
Results from univariable models were used to establish associations between each covariate and the different malaria outcomes. This information was taken into account when building multivariable models. All covariates assessed in univariable models have shown some evidence of association to malaria outcomes in previous studies, which was the most influential consideration in model building. Before building multivariable models, a correlation matrix was used to assess collinearity between similar predictors. Environmental factors were compared, household factors were compared, and measures of damage to facilities were compared. To limit negative effects of collinearity on any final models, one of the highly collinear variables was selected based on model goodness of fit.
To model annual malaria incidence, facility damage covariates were added to the model first. In all multivariable models, the aggregate variable “proportion of facilities damaged” was used to represent infrastructure damage. Variables indicating severity or time of damage were highly correlated (> 85%), therefore, only “proportion of facilities damaged” was included on the model. Additionally, “proportion of facilities damaged” had the lowest − 2 log likelihood value and was chosen to represent damage to facilities as the primary predictor. Goodness of fit tests were repeated for each of the demographic variables: median age and proportion under five, as well as the household features: presence of a toilet, flooring type, flooring material, and wall material. The environmental features considered were not highly correlated, therefore, each was assessed based on goodness of fit as well as with consideration of the covariates confounding the association between facility damage and malaria incidence. This same process was completed for severe malaria incidence, once again adding variables based on their effect on goodness of fit and potential to confound the association between facility damage and severe malaria incidence. Each of the Poisson models were run with a log link function and the district population as an offset term. Each model was adjusted for the X and Y coordinate value for the centroid of each district in order to account for spatial correlation between districts.
Proportion of pregnant people who received a second dose of IPTp was analysed using multiple linear regression. Model building was done using a similar procedure as the Poisson, however the goodness of fit statistic used here was R2. When generating models, it was taken into account that in most instances adding a variable to the model will increase the goodness of fit, therefore, the potential of confounding and results from exploratory data analysis were taken into stronger consideration. The same process, starting with measures of facility damage and adding other covariates was used. In this model the binary predictor of facility damage did have a higher R2 value than proportion of facilities damaged, however the proportion of facilities damaged provides some more granularity and therefore was chosen for the multivariable model.
Change in proportion of pregnant people who received IPTp as well as change in malaria incidence from 2018 to 2019 were also modelled as secondary outcomes in order to assess changes in trends as a result of the storm. Since both measures were a continuous proportion, generalized linear models were used to model these two outcomes. The covariates determined to provide the best fitting model in assessing malaria incidence were used in the model assessing change in malaria incidence. Similarly, the covariates found to create the best fitting model of proportion of pregnant people who received IPTp was used to model the change in this value.
Results
This analysis investigated malaria outcomes across the 13 districts that make up Sofala Province. There were 105 health care facilities and 66 schools identified that could be assessed for damage using satellite imagery from Google Earth Pro®. Of these, 23 (22%) health care facilities had any level of damage, and 45 (68%) schools had any level of damage. There was some disparity in both the severity of damage and the time required to restore the buildings. Figure 1 displays images of the University of Beira, this building, near the coast, was in an area hit hardest by Idai. This is an example of a building that saw complete destruction of its roof following the storm. There was no evidence of complete restoration of this building until March of 2020, 11 months following Idai. Other facilities such as the rural health centre displayed in Fig. 2 were repaired much quicker. This facility had evidence of complete damage but had evidence of being completely repaired within 3 months of Idai.
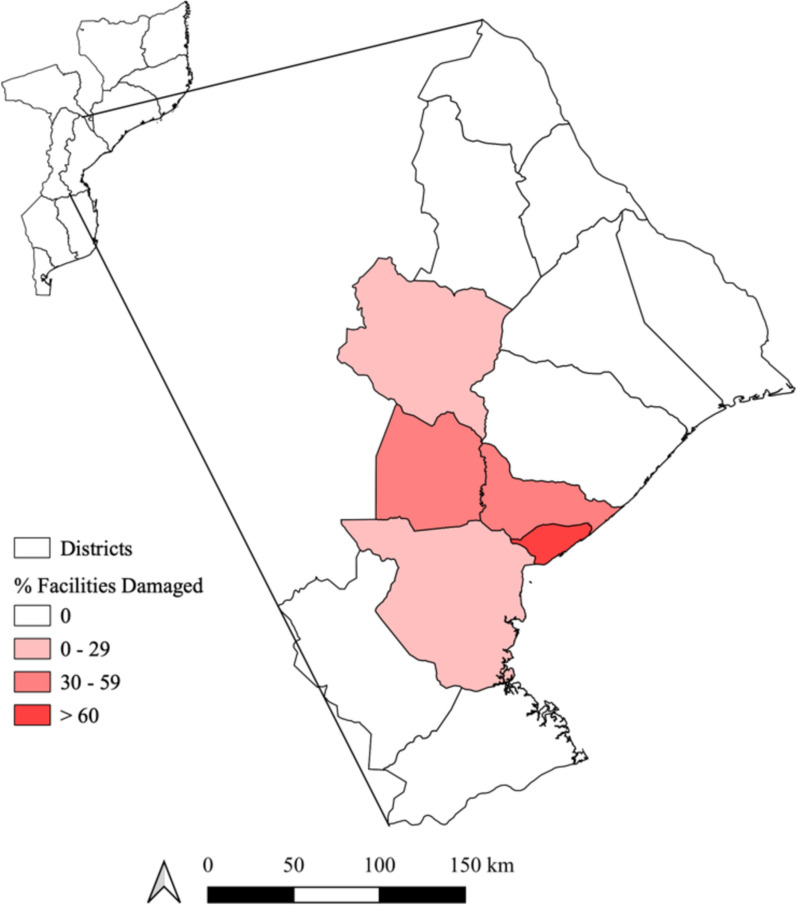
Most of the damage was isolated to the central corridor of Sofala Province. Idai hit the capitol city Beira in Beira district and moved inland to Dondo followed by Nhamatanda districts. These three districts accounted for 74 percent of the damage to health centres and 91 percent of the damage to schools. Figure 3 displays the proportion of facilities damaged in each district in Sofala Province. Beira district is the district with the most damage which is expected as it saw the direct impact of Idai. Gorongosa (north) and Buzi (south) are the other two districts which experienced damage following Idai. These two districts are directly adjacent to the central corridor and the path which Idai followed through Mozambique.
Fig. 3.
Distribution of damaged facilities in Sofala Province. The percent of facilities (school and health centres) damaged following cyclone Idai in each district
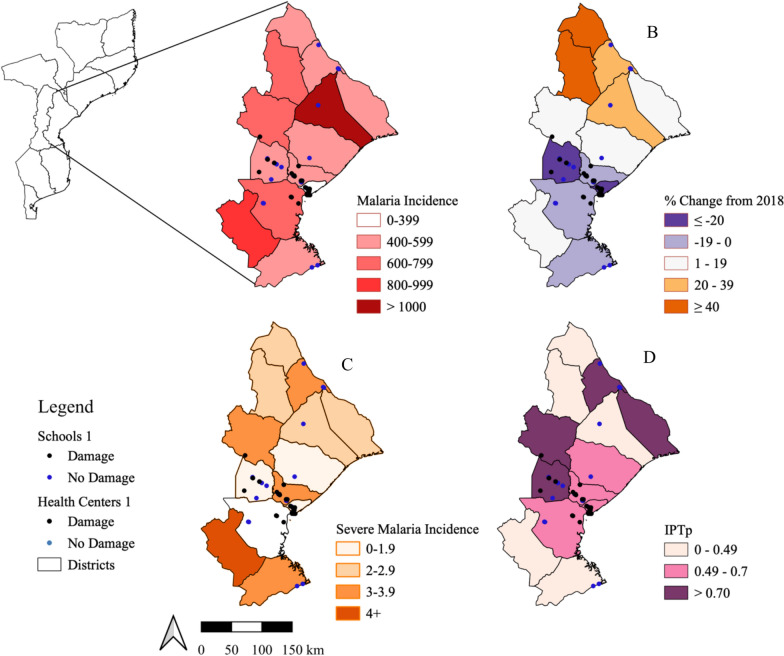
The distribution of each outcome of interest, extracted from the 2019 National Malaria Report for Sofala Province, are displayed in Fig. 4 and in Table 1. Each school and health care facility were also plotted on these maps. Of note, Beira district which was hit directly by Idai had the lowest malaria incidence in 2019, as well as the highest proportion of damaged facilities, marked with the black points in Fig. 4. Generally, the 2019 malaria incidence was lowest in areas most directly impacted by the cyclone as qualified by facility damage.
Fig. 4.
2019 malaria outcomes in Sofala Province. A. 2019 annual malaria incidence per 1000 people by district. B. Percent change in malaria incidence comparing 2019 to 2018 with purple representing a decrease in incident malaria and orange representing an increase in incident malaria. C. 2019 severe malaria incidence per 1000 people by district. D. Proportion of pregnant people who received intermittent preventative treatment (IPTp) in 2019 by district. Each map includes schools (dark blue) and health centres (light blue) which remained undamaged as well as all damaged facilities (black)
Table 1.
Basic demographics, health centre and school data, and malaria outcomes by district in Sofala Province
| District | Population Density* | Age (Median) | Health centres (Damaged)** | Schools (Damaged)** | Malaria annual incidence*** | Annual incidence change (%)+ | Severe malaria annual incidence *** | Preventative prophylaxis (%)++ |
|---|---|---|---|---|---|---|---|---|
| Buzi | 0.016 | 15 | 10 (0.10) | 5 (0.60) | 646 | − 8 | 1.4 | 70 |
| Caia | 0.055 | 13 | 9 (0) | 3 (0) | 455 | + 21 | 3.2 | 76 |
| Chemba | 0.022 | 13 | 5 (0) | 0 (0) | 598 | + 41 | 2.6 | 44 |
| Cheringoma | 0.008 | 13 | 5 (0) | 1 (0) | 1164 | + 38 | 2.5 | 43 |
| Chibabava | 0.020 | 14 | 6 (0) | 0 (0) | 871 | + 11 | 5.3 | 40 |
| Dondo | 0.079 | 17 | 12 (0.33) | 15 (0.73) | 452 | − 18 | 3.5 | 63 |
| Gorongosa | 0.027 | 13 | 6 (0.17) | 1 (1.00) | 726 | + 16 | 3.6 | 74 |
| Machanga | 0.010 | 15 | 6 (0) | 2 (0) | 596 | − 15 | 3.6 | 45 |
| Maringue | 0.016 | 12 | 1 (0) | 0 (0) | 718 | + 42 | 2.3 | 41 |
| Marromeu | 0.026 | 15 | 11 (0) | 0 (0) | 525 | + 14 | 2.8 | 80 |
| Muanza | 0.006 | 13 | 6 (0) | 1 (0) | 582 | + 15 | 2.0 | 70 |
| Nhamatanda | 0.079 | 15 | 11 (0.27) | 10 (0.60) | 472 | − 20 | 1.5 | 79 |
| Cidade da Beria | 0.811 | 19 | 17 (0.59) | 28 (0.86) | 138 | − 31 | 1.8 | 70 |
| Sofala Province | 0.090 | 16 | 105 (0.22) | 66 (0.68) | 611 | + 8 | 3.0 | 61 |
*Persons/km2 based on 2017 census24
**This count is based on facilities with sufficient satellite imagery to visualize and infer damage
***Incidence was calculated per 1000 people
+Percent change was calculated in comparison with 2018 incidence data
++This is the percent of pregnant people who received a second dose of preventative prophylaxis during pregnancy
Beira district also was one of two districts that saw a 20% or greater decrease in malaria incidence from 2018, Fig. 4, with a 31% decrease in incidence in from 2018, Table 1. Districts that saw a decrease in malaria incidence were those in the path of cyclone Idai and southern districts while northern districts saw an increase in malaria incidence in 2019 with an overall increase in incidence of 8% across Sofala Province.
The trends displayed for severe malaria incidence and proportion of pregnant people receiving IPTp in Fig. 4 followed a less distinct pattern. Beira and Nhamatanda along with Buzi districts, which all saw some levels of facility damage, had the lowest incidence of severe malaria in 2019. However, Dondo and Nhamatanda districts saw a higher incidence of severe malaria. Based on Fig. 4, the distribution of the proportion of pregnant people who received IPTp seemed even less associated with facilities damaged as a result of Idai.
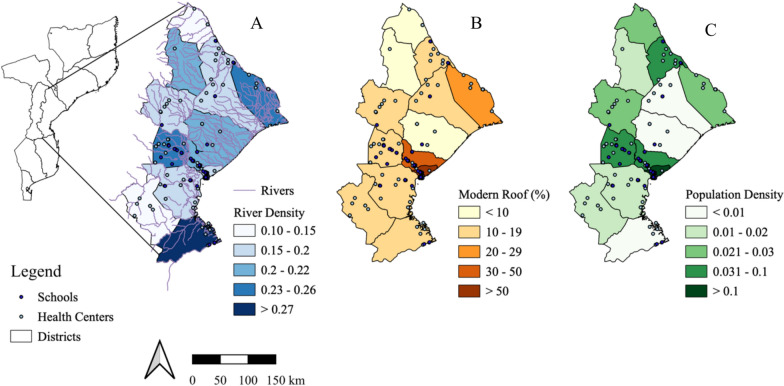
To further visualize covariates associated with malaria outcomes, three covariates representing environmental and demographic related features are displayed in Fig. 5. The density of rivers at the district level is visually not associated with patterns of malaria outcomes (Fig. 4). Beira and Dondo districts which have the highest population density and the highest proportion of households with modern roofs would be considered two of the most urban distracts in Sofala. These were two districts hit hardest by the storm in terms of proportion of facilities damaged (Fig. 3) and also saw a decrease in malaria incidence from 2018 to 2019 (Fig. 4B).
Fig. 5.
Covariates associated with Malaria outcomes broken down by district. Each map of Sofala province displays a different covariate found to be associated with malaria outcomes following Idai. A. Density of rivers per province (m/km2) B. Percent of households with a modern roof based on 2007 census data C. Population density (people/km2)
Results from exploratory univariable modelling are shown in Tables 2 and 3. Table 2 shows results from univariable Poisson regression models assessing the association between each covariate of interest and malaria incidence and severe malaria incidence in 2019. When assessing both malaria and severe malaria incidence, damaged healthcare facilities had a larger effect on incidence than schools. The effect of facility damage had a larger impact on malaria incidence than it did on severe malaria incidence in the univariate model. All univariable models assessing measures of damage found an increased level of damage was associated with a decreased in both malaria and severe malaria incidence. When assessing demographics, the association between age variables and malaria outcome behave as expected based on literature. An increase in median age was associated with a decreased risk in malaria and severe malaria and an increased proportion under five showed a large effect in the increasing the district wide risk of malaria.
Table 2.
Univariate analysis using Poisson regression
| 2019 Malaria incidence | 2019 Severe malaria incidence | |||||
|---|---|---|---|---|---|---|
| β | Risk ratio | 95% CI | β | Risk ratio | 95% CI | |
| Facilities damaged—binary | − 0.78 | 0.46 | (0.46, 0.46) | − 0.23 | 0.79 | (0.74, 0.85) |
| Health centres damaged* | − 2.42 | 0.09 | (0.09, 0.09) | − 0.58 | 0.56 | (0.49, 0.64) |
| Schools damaged* | − 0.93 | 0.39 | (0.39, 0.40) | − 0.12 | 0.89 | (0.82, 0.64) |
| Facilities damaged* | − 1.69 | 0.19 | (0.18, 0.19) | − 0.42 | 0.66 | (0.60, 0.73) |
| Mean facility damage value | − 0.64 | 0.53 | (0.53, 0.53) | − 0.14 | 0.87 | (0.84, 0.91) |
| Mean time until repair** | − 0.28 | 0.76 | (0.76, 0.76) | − 0.07 | 0.93 | (0.92, 0.95) |
| Median age | − 0.21 | 0.81 | (0.81, 0.81) | − 0.06 | 0.94 | (0.93, 0.960 |
| Under 5* | 10.00 | 21,912 | (20,746, 23,142) | 3.16 | 23.58 | (12.3, 45.3) |
| April vegetation (greenness) | 0.001 | 1.001 | (1.001, 1.001) | 0.0002 | 1.000 | (1.00, 1.00) |
| Elevation (median) | 0.004 | 1.004 | (1.004, 1.004) | 0.002 | 1.002 | (1.00, 1.00) |
| River density (m/km^2) | 2.42 | 11.20 | (10.8, 11.7) | 1.46 | 4.30 | (2.48, 7.43) |
| Bodies of water+ | − 0.28 | 0.76 | (0.76, 0.76) | − 0.07 | 0.93 | (0.91, 0.95) |
| Flood land+ | 2.12 | 8.29 | (8.08, 8.49) | − 0.28 | 0.755 | (0.56, 1.02) |
| Finished floors* | − 0.02 | 0.98 | (0.98, 0.98) | − 0.004 | 0.996 | (1.00, 1.00) |
| Modern roof* | − 0.02 | 0.98 | (0.98, 0.98) | − 0.003 | 0.997 | (1.00, 1.00) |
| Toilet—binary | − 0.02 | 0.98 | (0.98, 0.98) | − 0.004 | 0.996 | (1.00, 1.00) |
| Modern walls* | − 0.03 | 0.97 | (0.97, 0.97) | − 0.005 | 0.995 | (1.00, 1.00) |
Assessing the association between each covariate of interest and 2019 malaria incidence and as well as 2019 severe malaria incidence
*These values are proportions determined at the district level
**Maximum time to repair was 8 months representing through the end of 2019
+ Proportion of land use based on frequency of corresponding polygons in QGIS
Table 3.
Univariate analysis using multiple linear regression
| Proportion of pregnant people who received a second dose of preventative prophylaxis | ||
|---|---|---|
| β | 95% CI | |
| Facilities damaged—binary | 0.22 | (0.02, 0.43) |
| Health centres damaged* | 0.31 | (− 0.26, 0.89) |
| Schools damaged* | 0.26 | (− 0.01, 0.52) |
| Facilities damaged* | 0.26 | (− 0.14, 0.67) |
| Mean facility damage value | 0.12 | (− 0.03, 0.28) |
| Mean time until repair** | 0.05 | (− 0.02, 0.12) |
| Median age | 0.022 | (− 0.03, 0.08) |
| Under 5* | − 1.08 | (− 3.91, 1.74) |
| River density (m/km^2) | − 0.45 | (− 2.08, 1.18) |
| Bodies of water+ | 0.004 | (− 0.08, 0.09) |
| Flood land+ | 0.67 | (− 0.46, 1.79) |
| Finished floors* | 0.001 | (− 0.004, 0.006) |
| Modern roof* | 0.001 | (− 0.004, 0.006) |
| Toilet—binary | 0.002 | (− 0.003, 0.008) |
| Modern walls* | 0.003 | (− 0.003, 0.009) |
| Population density (persons/km2) | 0.12 | (− 0.38, 0.63) |
Assessing the association between each covariate of interest and administration of preventative prophylaxis in pregnant people.* These values are proportions determined at the district level
**Maximum time to repair was 8 months representing through the end of 2019
+ Proportion of land use based on frequency of corresponding polygons in QGIS
Based on univariable analysis using a generalized linear model to explore the crude associate between covariates and proportion of people receiving IPTp, there was a positive association between damage to facilities and administration of IPTp. An increase in the proportion of damaged facilities was associated with an increase in the proportion of pregnant people receiving IPTp (Table 3). The largest effect, similar to when assessing malaria incidence, was seen when assessing damage to healthcare facilities. In this univariable analysis, population density was also assessed for its association with administration of IPTp. Increased population density was positively associated with an increase in pregnant people receiving IPTp.
The final multivariable models assessing the association between the proportion of facilities damaged with malaria and severe malaria incidence in 2019 are displayed in Table 4. Proportion of facilities damaged was used in each of the models as the main predictor for damage as it gave the most accurate model when assessing goodness of fit (− 2 log likelihood) compared to other measures of damage severity. Given that there was a high correlation between housing features, a single feature was used in each model. River density, proportion of area which was considered flood land, April vegetation density, and median elevation all improved the fit of the model and were added to the model assessing malaria incidence. The final model assessing severe malaria incidence was similar however did not include median elevation as a covariate. After adjusting for median age, housing structure, and environmental factors it was found that an increase in proportion of facilities damaged by 100% was associated with a 73% (95% CI 68%, 78%) increase in risk of malaria infection across a district. To make this value more applicable, a 10% increase in proportion of facilities damaged in a district was associated with an increased risk of malaria incidence of 5.7%. When modelling the risk of severe malaria incidence in the multivariable Poisson model, an increased proportion in facilities damaged was also associated with an increased risk of severe malaria infection. An increase in facility damage of 100% was found to be associated with a risk of severe malaria 2.16 (95%CI 1.42, 3.32) times higher than a district with no facility damage. An increase in proportion of facilities damaged by 10% was found to be associated with an 8.0% increase in risk of severe malaria infection after adjusting for median age, household features, and environmental features at the district level.
Table 4.
Multivariable analysis using Poisson regression
| 2019 Malaria incidence | 2019 Severe malaria incidence | |||||
|---|---|---|---|---|---|---|
| β | Risk Ratio | 95% CI | β | Risk ratio | 95% CI | |
| Proportion facilities damaged | 0.55 | 1.733 | (1.68, 1.78) | 0.77 | 2.163 | (1.41, 3.32) |
| Median age | 0.71 | 2.026 | (2.01, 2.05) | 0.29 | 1.332 | (1.18, 1.50) |
| Modern roof | − 0.05 | 0.951 | (− 0.05, 0.95) | − 0.015 | 0.985 | (0.98, 0.99) |
| River density (m/km^2) | − 1.19 | 0.303 | (− 1.14, 0.32)) | 1.76 | 5.785 | (2.60, 13.52) |
| April vegetation (greenness) | 0.001 | 1.001 | (1.001, 1.001) | 0.0008 | 1.001 | (1.001, 1.001) |
| Flood land | − 4.14 | 0.016 | (0.015, 0.017) | − 3.27 | 0.038 | (0.02, 0.07) |
| Median elevation | − 0.001 | 0.999 | (0.999, 0.999) | N/A* | N/A* | N/A* |
Final models assessing the association between facilities damaged following cyclone Idai and incidence malaria and severe malaria cases
*Elevation was not found to improve fit of the model predicting severe malaria incidence
The multivariable model assessing the association between facility damage and administration of IPTp in pregnant people is displayed in Table 5. This table also displays the generalized linear model which assess how these same covariates were associated with a change in the administration of IPTp from 2018 to 2019. This model uses proportion of facilities damaged as the main predictor. After adjusting for median age, household features, environmental factors, and population density it was found that an increase in proportion of damaged facilities was associated with an increase in proportion of pregnant people who received IPTp. Based on this model, a 10% increase in proportion of facilities damaged was associated with a 7.1% increase (95% CI 4.1% decrease to 18.3% increase) in the proportion of pregnant people who received a second dose of IPTp at the district level. This association was not found to be statistically significant, however is still of interest as this model was underpowered due to a limited number of districts being analysed. An increase in proportion of facilities damaged was also found to have a weak positive association with an increase in administration of IPTp since 2018. A 10% increase in facilities damaged was associated with a 3.6% increase (95%CI 13.7% decrease, 20.8% increase) in proportion of pregnant people receiving IPTp from 2018 to 2019. The wide confidence interval found for this association indicates there is not evidence of an association between infrastructure damage and the change in rate of IPTp administration.
Table 5.
Multivariable analysis using multiple linear regression
| Proportion of pregnant people who received a second dose of preventative prophylaxis in 2019 | Change in proportion of pregnant people who received a second dose of preventative prophylaxis from 2018 | |||
|---|---|---|---|---|
| β | 95% CI | β | 95% CI | |
| Proportion facilities damaged | 0.71 | (− 0.41, 1.83) | 0.36 | (− 1.37, 2.08) |
| Median age | − 0.08 | (− 0.23, 0.07) | − 0.06 | (− 0.29, 0.17) |
| Modern walls | 0.01 | (− 0.00, 0.02) | 0.00 | (− 0.02, 0.02) |
| River density (m/km^2) | 0.49 | (− 1.55, 2.52) | − 0.63 | (− 3.76, 2.51) |
| Flood land | 1.31 | (0.03, 2.59) | 0.64 | (− 1.33, 2.61) |
| Population density (persons/km2) | − 0.33 | (− 1.19, 0.54) | 0.38 | (− 0.96, 1.71) |
Assessing the association between damaged facilities and the proportion of pregnant people in each district who received a second dose of preventative prophylaxis
The final outcome assessed was change in malaria incidence from 2018 to 2019, Table 6. This multiple linear regression model used that same covariates as were used in the Poisson models used to assess malaria and severe malaria incidence. This model found that an increase in proportion of facilities damaged was associated with a decrease in malaria incidence from 2018 to 2019. Based on this model, after adjusting for median age, household features, and environmental features a 10% increase in proportion of facilities damaged was associated with a 4.5% decrease (95% CI 10.2% decrease to 1.3% increase) in malaria incidence from 2018 to 2019 at the district level.
Table 6.
Multivariable analysis using multiple linear regression
| Percent change in malaria incidence from 2018 to 2019 | ||
|---|---|---|
| β | 95% CI | |
| Proportion facilities damaged | − 0.45 | (− 1.02, 0.13) |
| Median age | 0.061 | (− 0.10, 0.22) |
| Modern roof -binary | − 0.004 | (− 0.01, 0.01) |
| River density (m/km^2) | − 1.17 | (− 2.08, − 0.26) |
| April vegetation (greenness) | 0.00 | (0.00, 0.00) |
| Flood land | − 0.40 | (− 1.26, 0.47) |
| Median elevation | 0.002 | (− 0.001, 0.003) |
Assessing the association between damaged facilities and the change in malaria incidence from 2018 to 2019
Discussion
After adjusting for environmental covariates it was determined that an increased proportion of damaged health care facilities and schools was associated with an increased risk of malaria and severe malaria in the aftermath of cyclone Idai. The cyclone which hit central Mozambique in 2019 led to substantial damage to homes, schools, health centres, and other facilities in Mozambique’s Sofala Province. It is expected that with a changing climate there is an increased risk of tropical storms in the Indian Ocean [24]. This is an area which has endemic malaria, the results of a changing climate will alter the interactions people of Mozambique have with mosquitos, especially following a severe weather event. Building an understanding of the association between infrastructure damage following a tropical storm and risk of malaria infection was necessary in the short term for emergency response, and in the long term for control and elimination efforts. This analysis of the association of storm damage with multiple malaria outcomes quantified the impact of damaged facilities. Analyses were completed at the district level so should be considered under the ecological fallacy; these are trends at the district level not at the individual level.
In an unadjusted model assessing the associating between facility damage and malaria incidence the risk of malaria was found to decrease in districts with a higher proportion of facilities damaged. This can be observed in Figs. 3 and 4, Beira District was the only district with fewer than 400 indecent cases of malaria per 1000 people in 2019, and it was also the district with the highest proportion of facility damage. A similar trend is seen in surrounding districts which had damage to facilities. However, after adjusting for demographic and environmental covariates there was a positive association between the proportion of facilities damaged and the risk of malaria infection. The risk of progression to severe malaria was also positively associated with an increase in proportion of facilities damaged. This risk was greater even than the risk of a malaria infection associated with an increase in damage following Idai. These models demonstrated that when damage occurred following Idai there was an increased burden of malaria in the areas most damaged by the storm. The increased risk of malaria infection may be contributable to an increased exposure to environmental risk factors associated with increased risk of malaria as well as decreased access to protective equipment such as ITNs. The increased risk of progression to severe malaria demonstrates the burden of decreased access to healthcare as a result of the storm damaging infrastructure and health facilities.
The change in malaria incidence from 2018 to 2019 per district was modelled as an outcome to gain a broader picture of the change in malaria reporting prior to and after Idai. After adjusting for demographic and environmental factors the models suggest that an increase in proportion of facilities damaged at the district level was associated with a decrease in annual malaria incidence from 2018 to 2019. The negative association between facilities damaged and change in malaria incidence between 2018 and 2019 points again to access to healthcare being a substantial issue following Idai. There are limitations in the knowledge of malaria reporting following a severe storm. However, it is likely that malaria infections were underreported because access to healthcare was limited by damage as a result of cyclone Idai.
To further address the impact of damage following cyclone Idai on access to healthcare, the proportion of pregnant people per district who received a second dose of intermittent preventative treatment (IPTp) in 2019 was modelled as an outcome. Interestingly, districts with higher facility damage also showed an increased proportion of pregnant women receiving IPTp. This suggests that emergency responses may have successfully targeted these vulnerable populations, despite overall healthcare access being compromised. Following Cyclone Idai there was a large effort put forward by UNICEF to provide humanitarian relief to the people in Mozambique [5, 25]. There are limited details on the specifics of this response beyond the distribution of ITNs, but there is mention of further efforts being made. The distribution of IPTp to pregnant people is likely to have been part of this response effort.
Although ties have been made between the devastation caused by cyclone Idai and malaria outcomes in central Mozambique there is limited research on the direct effect of damage on malaria incidence. This paper presents a novel method of quantifying the risk of malaria with increased damage following a severe weather event. Previous research has shown that people living in rural areas are at a substantially higher risk of malaria infection compared to those in urban areas [8]. One large difference between many rural and urban communities is their access to healthcare. One study assessing damage following Idai found that areas affected by the cyclone saw a decrease in accessibility to healthcare from 78.8 to 52.5% due to infrastructure damage including transportation networks and facilities [26]. Similarly, the findings in this study suggest that there is an increased risk of severe malaria following storm damage which can be attributed, at least in part, to a decreased access to healthcare. The model comparing incident cases from 2018 to 2019 further supports these findings. An increased proportion of facilities damaged was associated with a decrease in malaria incidence from 2018 to 2019. Since there was an increase of incident malaria cases in district with higher levels of facility damage based on results of the Poisson model, the decrease in reported cases from 2018 to 2019 is likely attributable to a decrease in access to healthcare in those districts. The exception to this finding is the increase found in IPTp administration in districts that saw the most damage. However, if this was a function of the immediate response by UNICEF, there would be a small impact on incident malaria cases as pregnant mothers make up a small portion of the population. This may be more telling of the short-term success of the response and some possible downfalls in the long-term as the risk of malaria still increased.
This research assessed the 13 districts in Sofala Province meaning that linear models were underpowered, leading to inconclusive results in some models. The use of Poisson models to predict the relative risk of malaria incidence provided a non-parametric solution, however working with a sample of only 13 districts still has limitations. Additionally, the analysis only assessed outcomes seen in 2019. It would have been interesting to assess the trends into 2020 as severity of facility damage and time to repair data may have provided an interesting insight into the long-term malaria trends seen as a result of the storm damage. Also, this analysis only included damage to healthcare and educational facilities as surrogates of impacts to the entire community. This was done as there were publicly available enumeration lists of these facilities which included geographic coordinates. Additional research investigating other aspects of storm impacts on communities should be conducted.
Although there are limitations, this research provides insight into the direct effect of damage caused by Cyclone Idai on malaria outcomes in Sofala province at the district level. This insight can be useful in understanding what areas may be at highest risk of malaria infection following any future tropical storms. There are both short term and long-term implications for malaria in Sofala Province following this storm. A decreased access to healthcare means that there will be an increased disease burden. An account from a physician working in Beira highlighted that there was a substantial decrease in patients able to make their way to the clinic and those who did come in were the most vulnerable people [27]. In response effort to natural disasters when considering malaria, there is a clear need of immediate assistance to protect people from environmental risk factors associated with increased malaria infections. In the long term there is also evidence that efforts should be put in place to restore healthcare facilities or provide temporary facilities until repairs are completed in efforts to minimize the burden of malaria. These results highlight that damage to facilities and infrastructure are associated with an increased risk of malaria. The risk of long-term increased malaria incidence should be taken into account when planning response efforts.
Acknowledgements
Not applicable.
Author contributions
CG conducted the quantification of infrastructure damage, conducted data analyses, and drafted the manuscript. JLF provided malaria surveillance reports for Sofala Province and consulted on the identification of healthcare facilities and schools. KMS designed the study, piloted the methods, advised the analysis, and finalized the manuscript.
Funding
No funding was used for this manuscript.
Availability of data and materials
Data will be made available upon request to the corresponding author.
Declarations
Ethics approval and consent to participate
Not applicable: This study did not involve human subjects and only used publicly available data.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.ReliefWeb. 2018–2019 Mozambique Humanitarian Response Plan Revised following Cyclones Idai and Kenneth, May 2019 (November 2018 - June 2019), Mozambique. https://reliefweb.int/report/mozambique/2018-2019-mozambique-humanitarian-response-plan-revised-following-cyclones-idai. (2019).
- 2.Al-Taiar A, Jaffar S, Assabri A, Al-Habori M, Azazy A, Al-Ganadi M, et al. Who develops severe malaria? Impact of access to healthcare, socio-economic and environmental factors on children in Yemen: a case-control study. Trop Med Int Health. 2008;13:762–70. [DOI] [PubMed] [Google Scholar]
- 3.Zhou SS, Zhang SS, Wang JJ, Zheng X, Huang F, Li WD, et al. Spatial correlation between malaria cases and water-bodies in Anopheles sinensis dominated areas of Huang-Huai plain, China. Parasit Vectors. 2012;5:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.UNICEF. Mozambique Humanitarian Situation Report for Cyclone Idai. https://www.unicef.org/documents/mozambique-humanitarian-situation-report-1-may-2019. 2019
- 5.UNICEF. Nearly 15,000 cases of malaria reported in areas of Mozambique affected by Cyclone Idai. https://www.unicef.org/press-releases/nearly-15000-cases-malaria-reported-areas-mozambique-affected-cyclone-idai-unicef.
- 6.Patouillard E, Griffin J, Bhatt S, Ghani A, Cibulskis R. Global investment targets for malaria control and elimination between 2016 and 2030. BMJ Glob Health. 2017;2:e000176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO. World malaria report 2021. Geneva: World Health Organization; 2021. [Google Scholar]
- 8.Ejigu BA. Geostatistical analysis and mapping of malaria risk in children of Mozambique. PLoS ONE. 2020;15:e0241680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arroz JAH. Increase in cases of malaria in Mozambique, 2014: epidemic or new endemic pattern? Rev Saude Publica. 2016;50:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ferrão JL, Mendes JM, Painho M. Modelling the influence of climate on malaria occurrence in Chimoio Municipality, Mozambique. Parasit Vectors. 2017;10:260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gupta S, Jain I, Johari P, Lal M. Impact of climate change on tropical cyclones frequency and intensity on Indian coasts. In: Rao PJ, Rao KN, Kubo S, editors. Proceedings of international conference on remote sensing for disaster management. Cham: Springer Int Publish; 2019. p. 359–65. [Google Scholar]
- 12.Wainwright CM, Finney DL, Kilavi M, Black E, Marsham JH. Extreme rainfall in East Africa, October 2019–January 2020 and context under future climate change. Weather. 2021;76:26–31. [Google Scholar]
- 13.Snyman K, Mwangwa F, Bigira V, Kapisi J, Clark TD, Osterbauer B, et al. Poor housing construction associated with increased malaria incidence in a cohort of young Ugandan children. Am J Trop Med Hyg. 2015;92:1207–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Minnesota Population Center. Integrated Public Use Microdata Series, International: Version 7.3 . Minneapolis, MN: IPUMS, 2020. Https://Doi.Org/10.18128/D020.V7.3.
- 15.Mugabe VA, Gudo ES, Inlamea OF, Kitron U, Ribeiro GS. Natural disasters, population displacement and health emergencies: multiple public health threats in Mozambique. BMJ Glob Health. 2021;6:e006778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Petricola S, Reinmuth M, Lautenbach S, Hatfield C, Zipf A. Assessing road criticality and loss of healthcare accessibility during floods: the case of Cyclone Idai, Mozambique 2019. Int J Health Geogr. 2022;21:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maina J, Ouma PO, Macharia PM, Alegana VA, Mitto B, Fall IS, et al. A spatial database of health facilities managed by the public health sector in sub Saharan Africa. Sci Data. 2019;6:134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Google: Google Earth Pro (Version 7.3.6). CA, USA, 2022.
- 19.QGIS Version 3.26.3 2021. (2021).
- 20.Relatório’de Actividades Desenvolvidas Durante os Dose Meses de 2018–2019. (2020).
- 21.Divulgação os resultados preliminares, Censo 2017 IV Recenseamento Geral Da População e Habitação. (2017).
- 22.Rivers, Mozambique, 2013 - Digital Maps and Geospatial Data. Princeton University. https://maps.princeton.edu/catalog/stanford-wc571vr4663.
- 23.EarthExplorer. https://earthexplorer.usgs.gov/.
- 24.Hope M. Cyclones in Mozambique may reveal humanitarian challenges of responding to a new climate reality. Lancet Planet Health. 2019;3:e338–9. [DOI] [PubMed] [Google Scholar]
- 25.Cyclone Idai: More than 1.5 million children urgently need assistance across Mozambique, Malawi and Zimbabwe – UNICEF. https://www.unicef.org/press-releases/cyclone-idai-more-15-million-children-urgently-need-assistance-across-mozambique.
- 26.Hierink F, Rodrigues N, Muñiz M, Panciera R, Ray N. Modelling geographical accessibility to support disaster response and rehabilitation of a healthcare system: an impact analysis of Cyclones Idai and Kenneth in Mozambique. BMJ Open. 2020;10:e039138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lokotola CL, Uyttersprot T, Felimone P, Scheerens C. How did primary health care in Beira experience Cyclone Idai? Afr J Prim Health Care Fam Med. 2022;14:3626. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available upon request to the corresponding author.