Abstract
Sigmoid volvulus during pregnancy is an extremely rare condition that presents as intestinal obstruction and can lead to severe complications for both the mother and fetus if not promptly diagnosed and treated. To our knowledge, this is the first documented case in Yemen. We report a case of a 39-year-old pregnant woman at 32 weeks of gestation who presented with acute abdominal pain, constipation, and signs of peritonitis. Diagnostic imaging was limited due to the pregnancy, but an ultrasound revealed fluid collection in the pelvis and massive pneumoperitoneum, suggesting a rupture of the hollow viscus. An emergency exploratory laparotomy confirmed a perforated sigmoid volvulus with necrosis of the sigmoid wall; as a result, we resected a nonviable colon and performed Hartmann’s procedure. After five days, we discharged the patient in excellent condition, and the fetus was monitored as healthy. Diagnosis of sigmoid volvulus during pregnancy is challenging due to the overlap of symptoms with normal pregnancy. Prompt surgical intervention is crucial to prevent maternal and fetal complications. This case highlights the importance of a multidisciplinary approach involving general surgeons, obstetricians, and neonatologists in managing this rare condition. Early diagnosis and treatment are essential for improving maternal and fetal outcomes in cases of sigmoid volvulus during pregnancy.
Keywords: intestinal obstruction, peritonitis, pregnancy, sigmoid volovlus, yemen
Introduction
Intestinal obstruction is a surgical emergency condition that occurs due to the failure of forward movement of gastrointestinal contents, which can occur as a result of either a dynamic (occlusion of the intestinal lumen) or an adynamic (absent or disordered peristalsis) [1]. Volvulus is a Latin word that means twisting. Colonic volvulus refers to the rotation of a portion of the colon around its mesentery. Colonic volvulus ranks as the third most common cause of colonic obstruction worldwide [2]. Clinical presentations are unspecific, and diagnosis relies on high clinical suspicion. Sigmoid volvulus often manifests acutely as abdominal pain, distention, and vomiting, while its chronic form often presents insidiously with vague signs and symptoms at diagnosis [3].
Intestinal obstruction, or sigmoid volvulus, during pregnancy is an extremely rare event [4]. This disease generally presents as mechanical bowel obstruction, and the physiological symptoms of pregnancy may cloud the clinical picture [5]. Laboratory findings are not sufficient in situations where X-rays and CT scans are generally avoided to avoid risk. Ultrasonography is helpful in assessing fetal development and can diagnose intestinal obstruction in experienced hands [5]. Ultrasonography is useful for assessing fetal development and can diagnose intestinal obstruction in experienced hands. Ultrasonography can detect signs of intestinal obstruction, such as dilated loops, abnormal peristalsis, parietal and valvulae conniventes alterations, and the presence of free extraluminal fluid [6]. If not diagnosed and treated early, sigmoid volvulus can cause maternal complications such as perforation, peritonitis, sepsis, and death. Fetal complications include preterm delivery, intrauterine death, and neonatal sepsis [7]. The most common causes of intestinal obstruction during pregnancy include adhesion, volvulus of the intestine, carcinoma, herniation, and appendicitis [8]. Difficult presentation and delayed diagnosis are responsible for the high morbidity and mortality in this situation.
In this report, we present the case of a pregnant woman diagnosed with sigmoid volvulus with massive pneumoperitoneum and peritonitis who was treated with an open diagnostic laparotomy and underwent resection of the sigmoid colon and stoma formation.
Case presentation
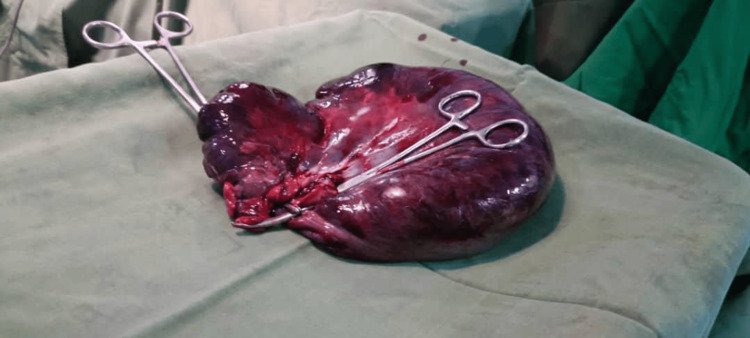
A 39-year-old pregnant woman, para 1 gravida 3, at 32 weeks of gestation, presented to the emergency department of Aden German International Hospital, Aden, Yemen, on May 22, 2024. She complained of severe acute abdominal pain. The pain gradually increased with time, starting two days prior to constipation associated with tachycardia (pulse rate was 150 bpm), indicating dehydration. The pain was colicky in nature and was not associated with nausea, vomiting, fever, or bleeding per rectum. She passed flatus 27 hours prior to presentation to the hospital, after which she developed absolute constipation for two days. The patient had no relevant medical history. On general examination, the patient appeared ill, tachypneic, and dehydrated. Abdominal examination revealed a distended generalized tender abdomen with hypokinetic bowel sounds showing signs of peritonitis; on digital rectal examination, the rectum was loaded with feces. The blood investigations showed slightly elevated white blood cells (11,800/mm3), mainly neutrophils (78%), platelet count (230,000/mm3), and a low hemoglobin level of 9.7 g/dL. The renal function test was slightly elevated (creatine was 270 µmol/L), with normal electrolytes: sodium (140 mmol/L), potassium (4.00 mmol/L), and chloride (101 mmol/L) (Table 1). Although a shot of an erect abdominal X-ray may be safe, we avoid X-ray radiography and CT scan images. Ultrasonography revealed fluid collection in the pelvis with massive pneumoperitoneum, which was suspected to be caused by rupture of the hollow viscus due to ischemia and necrosis (complicated intestinal obstruction). After resuscitation, we immediately transferred the patient to the operating room for an emergency exploratory laparotomy. The intraoperative diagnosis revealed a perforated sigmoid volvulus, along with sigmoid wall necrosis (Figure 1), with a moderately unpleasant odor, a dark color-free fluid collection, and multiple uncomplicated hydatid cysts in the right hepatic lobe. We resected the nonviable part of the colon and performed Hartmann’s procedure (Figure 2). Obstetrics and gynecology consultants monitored the patient closely. After five days of good condition, the patient was discharged for clinic follow-up. She had a normal vaginal delivery at the hospital and planned reanastomoses and colostomy closure.
Table 1. Investigation findings .
| Investigation | Findings | Reference range |
| Hemoglobin | 9.7 g/dL | 12.0-16.0 g/dL |
| White blood cells (WBC) | 11,800/mm3 | 4500-11,000/mm3 |
| Neutrophils | 78% | 55-70% |
| Platelets | 230,000/mm3 | 150,000-400,000/mm3 |
| Creatine | 270 µmol/L | 53-97.2 µmol/L |
| Sodium | 140 mmol/L | 136-145 mmol/L |
| Potassium | 4.00 mmol/L | 3.5-5.2 mmol/L |
| Chloride | 101 mmol/L | 96-106 mmol/L |
Figure 1. Intraoperative assessment showing a perforated sigmoid volvulus with necrosis of the sigmoid wall.
Figure 2. Resected nonviable part of the colon.
Discussion
In 1830, Houston was the first to report intestinal obstruction during pregnancy. The incidence is one in 66,431 deliveries [9]. Intestinal obstruction and considerable impact on bowel function can result from various factors, including but not limited to congenital malformations, adhesions, volvulus, intussusceptions, colonic tumors or cancer, appendicitis, and hernias [9]. Constipation, nausea, and bilious vomiting or bile-stained vomiting can develop gradually from colicky abdominal discomfort, a common indication of intestinal obstruction.
The severity of the symptoms can vary depending on the underlying cause of the intestinal obstruction, which could be adhesions, hernias, or tumors [10]. The mechanism that causes sigmoid volvulus during pregnancy is the displacement of a mobile sigmoid colon by an enlarging uterus, especially during the third trimester [11]. This causes the sigmoid colon to leave the pelvis and twist around its point and mesocolon.
Rarely, in late presentation of patients with complete intestinal obstruction, they may present with fever, dehydration, absence of bowel sound, peritonitis, and leukocytosis [12]. Because nausea, vomiting, and abdominal distension are common pregnancy symptoms, diagnosing sigmoid volvulus during pregnancy can be difficult. Subsequently, when a pregnant woman exhibits clinical symptoms of distention, extreme constipation, and stomach pain, a diagnosis should be considered [9].
High white blood cells can be a useful sign, but in the first phase of the disease, they can be normal or slightly elevated [13]. Using radiological investigations can be useful to establish the diagnosis, but many clinicians are restricting their use due to concerns regarding fetal complications. Radiation exposure may lead to chromosomal abnormalities, DNA mutations, and an increased risk of hematologic malignancies [5].
Patient management should include fluids, electrolyte balance correction, antibiotics, and nasogastric decompression. Intervention by an obstetrician should strictly depend on the condition of the fetus. Before terminating the pregnancy, we should administer steroids to enhance fetal lung maturity [14].
Delays in diagnosing and treating sigmoid volvulus can significantly impact the health of both the mother and her fetus, potentially leading to multiple organ failure, hypovolemic shock, septic shock, bowel infarction, and intestinal necrosis [15].
In pregnancy, the prognosis for sigmoid volvulus is poor [9,15]. This case presentation demonstrates the importance of early detection and appropriate care of sigmoid volvulus perforation in preventing maternal mortality.
Conclusions
Pregnancy-related sigmoid volvulus is a very uncommon disorder that needs multidisciplinary treatment by general surgeons, obstetricians, and neonatologists. Early diagnosis and treatment are critical to ensuring optimal well-being for the mother and fetus. Despite peritonitis symptoms, blood testing may be normal, so a clinical examination and exploratory laparotomy confirm the diagnosis.
Disclosures
Human subjects: Consent for treatment and open access publication was obtained or waived by all participants in this study. Ethical Committee of Aden German Hospital issued approval 01.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: Hebat Allah N. Fadhl, Mohammed A. Saghir, Sarah Mohammed, Abdurazaq Saeed
Acquisition, analysis, or interpretation of data: Hebat Allah N. Fadhl, Mohammed A. Saghir, Sarah Mohammed, Abdurazaq Saeed, Mariam Alsakkaf
Drafting of the manuscript: Hebat Allah N. Fadhl, Mohammed A. Saghir, Abdurazaq Saeed
Critical review of the manuscript for important intellectual content: Hebat Allah N. Fadhl, Mohammed A. Saghir, Sarah Mohammed, Mariam Alsakkaf
Supervision: Hebat Allah N. Fadhl, Mohammed A. Saghir
References
- 1.Epidemiology and causes of intestinal obstruction in Ethiopia: a systematic review. Fekadu G, Tolera A, Beyene Bayissa B, Merga BT, Edessa D, Lamessa A. SAGE Open Med. 2022;10:20503121221083207. doi: 10.1177/20503121221083207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WSES consensus guidelines on sigmoid volvulus management. Tian BW, Vigutto G, Tan E, et al. World J Emerg Surg. 2023;18:34. doi: 10.1186/s13017-023-00502-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sigmoid volvulus in an adolescent female: a case report. Kiyaka SM, Sikakulya FK, Masereka R, Okedi XF, Anyama P. Int J Surg Case Rep. 2021;87:106430. doi: 10.1016/j.ijscr.2021.106430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sigmoid volvulus in pregnancy. Atamanalp SS, Öztürk G. https://journals.tubitak.gov.tr/cgi/viewcontent.cgi?article=3412&context=medical Turk J Med Sci. 2012;42:9–15. [Google Scholar]
- 5.Sigmoid volvulus complicating pregnancy: a case report. Atamanalp SS, Kisaoglu A, Ozogul B, et al. Eurasian J Med. 2015;47:75–76. doi: 10.5152/eajm.2014.0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ultrasound of small bowel obstruction: a pictorial review. Rosano N, Gallo L, Mercogliano G, et al. Diagnostics (Basel) 2021;11:617. doi: 10.3390/diagnostics11040617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sigmoid volvulus in pregnancy: case report and review of literature. Serafeimidis C, Waqainabete I, Creaton A, Vakamacawai E, Kumar R. Clin Case Rep. 2016;4:759–761. doi: 10.1002/ccr3.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Volvulus complicating pregnancy and puerperium; report of three cases and review of literature. Harer WB Jr, Harer WB Sr. https://pubmed.ncbi.nlm.nih.gov/13590653/ Obstet Gynecol. 1958;12:399–406. [PubMed] [Google Scholar]
- 9.Intestinal obstruction complicating pregnancy. Perdue PW, Johnson HW Jr, Stafford PW. Am J Surg. 1992;164:384–388. doi: 10.1016/s0002-9610(05)80910-9. [DOI] [PubMed] [Google Scholar]
- 10.Volvulus of the colon. Incidence and mortality. Ballantyne GH, Brandner MD, Beart RW Jr, Ilstrup DM. Ann Surg. 1985;202:83–92. doi: 10.1097/00000658-198507000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Augustin G. Acute Abdomen During Pregnancy. Vol. 3. Cham, Switzerland: Springer; 2023. Intestinal obstruction; pp. 527–604. [Google Scholar]
- 12.Adhesive small bowel obstruction - an update. Tong JW, Lingam P, Shelat VG. Acute Med Surg. 2020;7:0. doi: 10.1002/ams2.587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Recurrent sigmoid volvulus in pregnancy: report of a case and review of the literature. Alshawi JS. Dis Colon Rectum. 2005;48:1811–1813. doi: 10.1007/s10350-005-0118-5. [DOI] [PubMed] [Google Scholar]
- 14.Gangrenous sigmoid volvulus in a pregnant woman. Joshi MA, Balsarkar D, Avasare N, et al. https://pubmed.ncbi.nlm.nih.gov/10695426/ Trop Gastroenterol. 1999;20:141–142. [PubMed] [Google Scholar]
- 15.Bowel obstruction in pregnancy. Connolly MM, Unti JA, Nora PF. Surg Clin North Am. 1995;75:101–113. doi: 10.1016/s0039-6109(16)46537-0. [DOI] [PubMed] [Google Scholar]