Abstract
A stricture of the bilioenteric anastomosis is a known complication of pancreaticoduodenectomy surgery and pediatric liver transplant. Occasionally, a complete biliary occlusion is encountered that cannot be treated utilizing endoscopic or conventional interventional radiology blunt recanalization techniques. In this article, we report 2 cases of successful sharp percutaneous ultrasound-guided retrograde creation of bilioenteric neoanastomosis in the setting of a complete biliary occlusion following Whipple surgery and liver transplant respectively. Percutaneous creation of bilioenteric neoanastomosis is a feasible minimally invasive therapeutic option alternative to surgical revision or when endoscopy is infeasible.
Keywords: Bilioenteric anastomosis, Hepatico-jejunal anastomosis, Percutaneous neoanastomosis, Endoscopic retrograde cholangiopancreatography (ERCP)
Introduction
A stricture of the bilioenteric anastomosis is a well known complication after a whipple surgery. The reported incidence is 2.6% following surgery, independent of benign or malignant disease [1]. An anastomotic stricture may progress to biliary occlusion due to an exhuberant fibrotic healing response or local tissue ischemia [2]. Initially, a biliary occlusion is often managed by endoscopy. However, in patients with surgically altered anatomy, endoscopy can be challenging or infeasible. If endoscopy fails, the occlusion is usually managed by percutaneous placement of an external biliary drainage catheter. However, an external biliary catheter is associated with complications that include: electrolytes imbalance, dehydration, malabsorption of fat-soluble vitamins, and poor quality of life [3]. Therefore, an internal biliary drainage catheter should be placed provided the occlusion can be transgressed. An internal catheter helps to restore bile acid in the hepato-enterological circulation and promote proliferation of goblet cells and expression of MUC2 which play an essential function in intestinal mucosa barrier protection. Additionally, an internal biliary drainage promotes recovery of immune function [4]. Placement of an internal biliary drainage catheter can be challenging in the setting of an occlusion of the bilioenteric anastomosis and often requires a multidisciplinary team approach. Surgical revision of the anastomosis is associated with a higher complication rate making minimally invasive approach preferable [5]. There are reports of creation of a bilioenteric neoanastamosis under fluoroscopy following identification of a safe pathway based on preprocedural cross sectional imaging. We report 2 cases of successful sharp percutaneous creation of a bilioenteric neoanastomosis utilizing ultrasound-guidance to identify and avoid vasculature including the hepatic artery, portal vein, and other collateral vessels along the tract.
Case 1
A 56-year-old woman with history of pancreatic adenocarcinoma, status post chemoradiation therapy, Whipple pancreaticoduodenectomy with Braun enteroenterostomy with separate right and left hepaticojejunal anastomoses presented with an occluded left biliary hepaticojejunal anastomosis. The patient's postoperative course was complicated by thrombosis of the hepatic artery, main portal vein, and proximal superior mesenteric vein. This lead to the development of cavernous transformation of the portal vein and multiple upper abdominal venous collaterals. The patient subsequently developed a right hepatic abscess, a stricture at the right hepaticojejunal anastomosis, and occlusion of the left hepaticojejunal anastomosis; these were managed by placement of a multipurpose abscess drainage catheter, a right internal/external and left external biliary drainage catheter, respectively. Review of the preprocedural cross-sectional imaging showed interposition of multiple peri-portal collateral veins and the hepatic artery along the expected location of the left biliary hepatojejunostomy (Fig. 1, Fig. 2). Our advanced endoscopists did not think an endoscopic approach would be feasible because of the patients anatomy. Given these findings, the technical challenges associated with endoscopy, and morbidity and mortality associated with surgical revision, a decision was made to proceed with percutaneous treatment of the occluded left biliary hepatojejunostomy. a decision was made to proceed with real-time ultrasound guidance with sharp recanalization to prevent inadvertent puncture of these vessels.
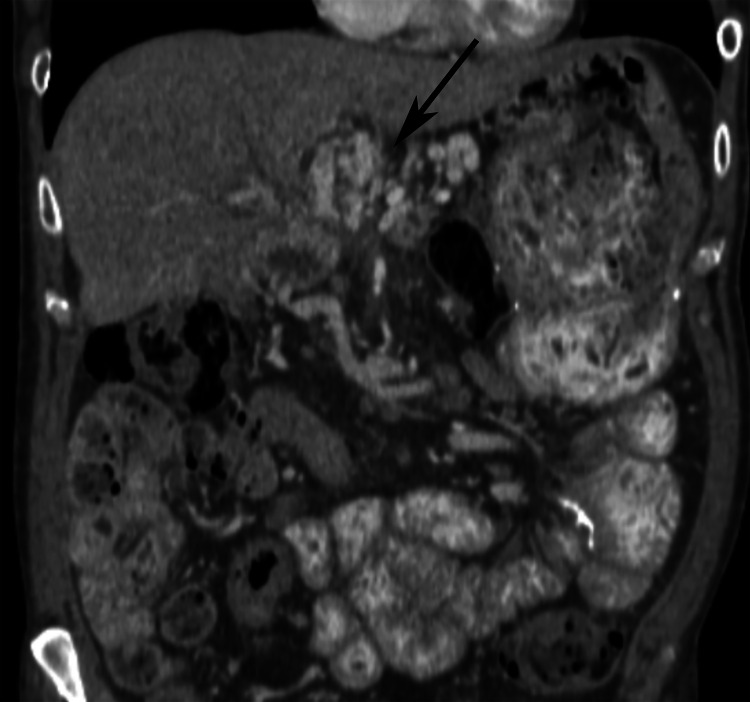
Fig. 1.
Preprocedure contrast enhanced coronal CT of the abdomen showing interposition of vascular structures along the projected neoanastomosis tract (black arrow).
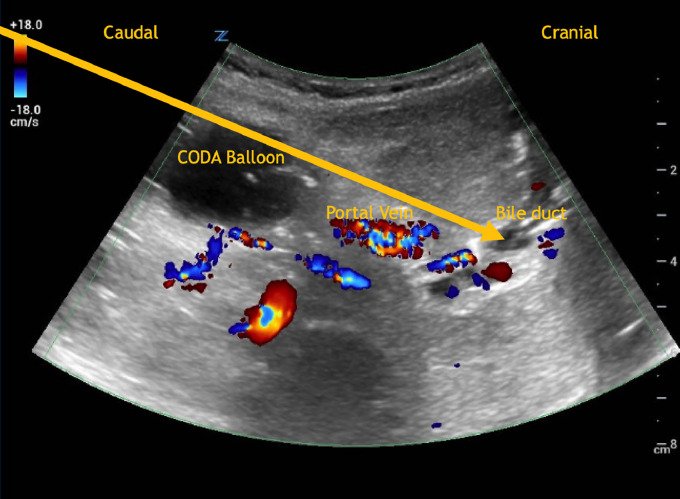
Fig. 2.
Doppler ultrasound of the abdomen showing interposition of vascular structures along the projected neoanastomosis tract.
Case 2
An 8-year-old child with history of liver failure of unknown etiology, status post liver liver transplantation 10 months ago with course complicated by T-cell mediated rejection and hepatic artery thrombosis. She developed biliary stricture 6 months following liver transplant. ERCP was performed with placement of a plastic stent. Her course was further complicated by stent migration, complete occlusion of the common bile duct and cholangitis. Bilateral external biliary drainage catheters were placed. Internalization utilizing endoscopic and conventional interventional radiology blunt recanalization techniques were unsuccessful due to complete common duct obstruction. Decision was to proceed with percutaneous sharp bilioenteric recanalization.
Procedure
Internal review board approval is not required for this submission. Written Informed consent was obtained from patient and parent prior to the procedure. The procedure was performed in a similar fashion in each case.
The procedure was performed in the interventional radiology suite under general anesthesia. One gram of ceftriaxone (Ceftriaxone sodium, Pfizer, USA) was given intravenously prior to the procedure. The right and left biliary catheters were removed over 180-cm-long Amplatz guidewires (Boston Scientific, Marlborough, MA) under fluoroscopic guidance. A 12 French sheath (Cook, Bloomington, USA) was placed from the right biliary access and a 5 French sheath (Terumo, Elkton, USA) from the left biliary access. Sheath cholangiograms revealed clearance of contrast medium from the right biliary system into the small bowel; however, there was no clearance of contrast medium from the left biliary system into the bowel. Several attempts were made to cross the hepatico-jejunal occlusion, using conventional methods with different catheters and wires which were unsuccessful. Therefore, a decision was made to proceed with sharp neoanastomosis creation.
A 32-mm-diameter Coda balloon (Cook, Bloomington, USA) was advanced through the right sheath and positioned in the proximal jejunum in the region of the left bilioenteric anastomosis (Fig. 3). The balloon was inflated with 15 ml of 20% diluted contrast material. A 15 mm snare was placed at the level of the left biliary occlusion. Using ultrasound and fluoroscopic guidance, a 21-gauge 15 cm Chiba needle (Cook, Bloomington, USA) was advanced in a retrograde fashion from a percutaneous approach through the Coda balloon (localized in the proximal jejunum) into the snare loop in the occluded left biliary duct (Fig. 4). Gray scale and color doppler ultrasound scanning was performed to guide needle and avoid puncture of the peri-portal venous collaterals and hepatic artery (Fig. 5). A V-18 wire (Boston Scientific, Heredia, Costa Rica) was advanced through the Chiba needle. The needle was retracted. The wire was grasped with the snare and pulled back through the left biliary sheath providing a through and through access. A 5 French Quick-cross catheter (Spectranetics, Colorado Springs, USA) was then advanced through the left sheath over the wire into the bowel and an Amplatz wire placed. The newly created left hepatico-jejunal neoanastomosis was dilated with a 4 mm x 4 cm Mustang balloon (Boston Scientific, Galway, Ireland) and an 8.5 French left internal-external biliary drainage catheter (Cook, Bloomington, USA) was placed. A 12 French right internal-external biliary drainage catheter (Cook, Bloomington, USA) was placed (Fig. 5). At 3 month follow-up, sheath cholangiogram showed a widely patent neoanastomosis.
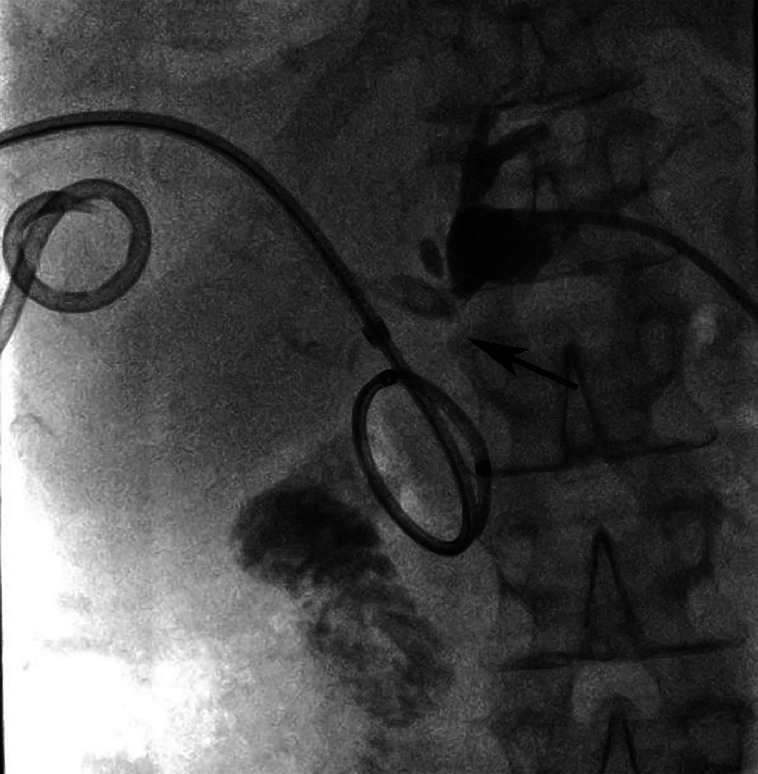
Fig. 3.
Frontal spot fluoroscopic image showing an abrupt cut-off of the left biliary system (black arrow). A right internal biliary drainage catheter is present along with a right hepatic abscess drainage catheter. Contrast in the loop of bowel is from the injection of the right tube.
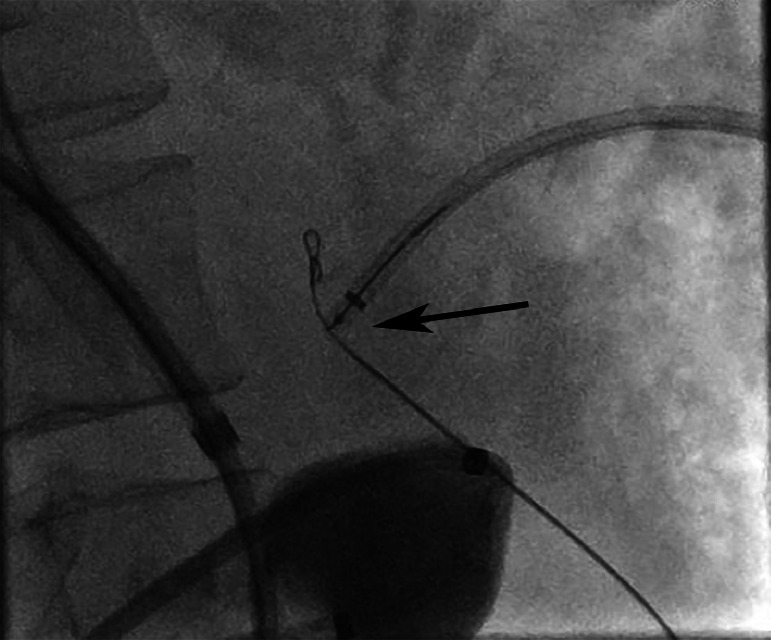
Fig. 4.
Oblique spot fluoroscopic images shows a 21-gauge chiba needle advanced through an inflated Coda balloon (localized in the proximal small bowel) into a 15 mm snare loop at the site of left duct occlusion (black arrow).
Fig. 5.
Spot fluoroscopic image after recanalization of the occluded left hepatic (black arrow) shows internal right and left biliary drainage catheters along with a right hepatic abscess drainage catheter.
Discussion
These 2 cases illustrate the use of ultrasound guidance in the creation of bilioenteric neoanastomosis when a safe direct pathway could not be identified on preprocedural imaging. No procedural related complications were observed. To our knowledge, there are no prior reports of a sharp bilioenteric neoanastomosis creation utilizing ultrasound guidance.
Since the first report of percutaneous transjejunal catherization of a Roux-en-Y biliary jejunal anastomosis in 1987, various percutaneous recanalization techniques have been reported in the literature for treatment of a biliary enteric anastomosis occlusion [[6], [7], [8]]. Given the close relationship of the portal vein and hepatic artery to the common bile duct serious complications of neoanastomosis creation can occur. A biliary leak, inadvertent vascular injury, and a bilio-vascular fistula have been reported. Previous reports have described the use of preoperative CT or MR to avoid vascular complications. Our technique provides real time ultrasound guidance of the needle through the course of the trajectory to avoid inadvertent puncture of vascular structures. This could be utilized in complex cases where surgical, endoscopic, or transhepatic techniques fail or are not an option. The technique is a better option than relying on CT or MRI to avoid vascular complications since they do not provide real time guidance.
Percutaneous endobiliary radiofrequency ablation for refractory benign hepaticojejunostomy and biliary strictures along with creation of an anastomosis using a magnetic compression have been reported in the literature. More recently, successful percutaneous biliary neo-anastomosis creation using a radiofrequency wire has been described for biliobiliary, biliogastric, and biliojejunal neoanastomosis creation with no report of major complications [3,5]. Our technique offers an additional treatment option in patients with a complete occlusion of the anastomosis.
Long-term follow-up is needed and a larger cohort sample is warranted to assess patency of the neo-anastomosis and recurrence rate.
In conclusion, real time ultrasound guidance for percutaneous creation of bilioenteric neoanastomosis offers an alternative management option of biliary occlusion when endoscopy is infeasible or conventional recanalization techniques fail.
Authors' contributions
Mamadou L Sanogo, MD, designed, wrote, and edited the manuscript. Jared Christensen, MD, Sahira Kazanjian, MD, Baljendra Kapoor, MD, Joseph Gemmete, MD1, Catalina Bautista, MD, and Hassan Anbari, MBChB edited the manuscript.
Patient consent
Written informed consent was obtained from each patient, parent or legal guardian prior to the procedure performed. This is stated in the manuscript.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.House MG, Cameron JL, Schulick RD, Campbell KA, Sauter PK, Coleman J, et al. Incidence and outcome of biliary strictures after pancreaticoduodenectomy. Ann Surg. 2006;243(5):576–578. doi: 10.1097/01.sla.0000216285.07069.fc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Larghi A, Tringali A, Rimbaş M, Barbaro F, Perri V, Rizzatti G, et al. Endoscopic management of benign biliary strictures after liver transplantation. Liver Transplant Off Publ Am Assoc Study Liver Dis Int Liver Transplant Soc. 2019;25(2):323–335. doi: 10.1002/lt.25358. [DOI] [PubMed] [Google Scholar]
- 3.Robins C, Xiao N, Salem R, Malik A, Keswani RN, Riaz A. Percutaneous biliary neo-anastomosis or neo-duct creation using radiofrequency wires. Cardiovasc Intervent Radiol. 2022;45(3):337–343. doi: 10.1007/s00270-022-03059-5. [DOI] [PubMed] [Google Scholar]
- 4.An J, Dong Y, Li Y, Han X, Sha J, Zou Z, et al. Retrospective analysis of T-lymphocyte subsets and cytokines in malignant obstructive jaundice before and after external and internal biliary drainage. J Int Med Res. 2021;49(2) doi: 10.1177/0300060520970741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Habibollahi P, Benjamin JL, X Bai H, Dagli MS, Shlansky-Goldberg RD. Percutaneous fluoroscopic-guided creation of neoanastomosis for the treatment of biliary occlusions. Cardiovasc Intervent Radiol. 2020;43(11):1671–1678. doi: 10.1007/s00270-020-02544-z. [DOI] [PubMed] [Google Scholar]
- 6.Chahal P, Baron TH, Topazian MD, Petersen BT, Levy MJ, Gostout CJ. Endoscopic retrograde cholangiopancreatography in post-Whipple patients. Endoscopy. 2006;38(12):1241–1245. doi: 10.1055/s-2006-945003. [DOI] [PubMed] [Google Scholar]
- 7.Paolantonio G, Pietrobattista A, Parapatt GK, Liccardo D, Natali GL, Candusso M, et al. Successful percutaneous transhepatic recanalization of a completely obstructed hepatico-jejunal anastomosis in a child with liver transplantation: unusual employment of the transseptal puncture system. Pediatr Transplant. 2018;22(8):e13293. doi: 10.1111/petr.13293. [DOI] [PubMed] [Google Scholar]
- 8.Maroney TP, Ring EJ. Percutaneous transjejunal catheterization of Roux-en-Y biliary-jejunal anastomoses. Radiology. 1987;164(1):151–153. doi: 10.1148/radiology.164.1.3588898. [DOI] [PubMed] [Google Scholar]