Abstract
This report presents a novel anatomical variant of the second dorsal metacarpal artery (SDMA). In this unique case, the SDMA abnormally penetrates the second dorsal interosseous muscle (SDIM), dividing into two major branches. A deep dorsal branch of the SDMA (dbSDMA) is located within the SDIM and extends to the distal end of the metacarpal. The other branch forms a perforating branch called the P-SDMA, which anastomoses with the palmar metacarpal artery branch (PMAb) and the deep palmar arch branch (DPAcb) in the deep palmar area. The discovery of this SDMA variant is significant for procedures involving complex hand surgeries such as DMA flaps. Understanding this anatomical variation is crucial for accurate surgical planning and can help avoid potential complications during surgery. To elucidate these unique variations, we employ three-dimensional (3D) imaging techniques, demonstrating the potential of these technologies to advance the visualization of anatomical structures and enhance medical education. 3D imaging also facilitates augmented reality applications and 3D printing. Our findings underscore the possible applications of 3D imaging in medical practice and education, potentially transforming anatomy education and surgical planning.
Keywords: Anatomical variations, Dorsal metacarpal artery, 3D imaging, Anatomical education, Case report
Graphical abstract
Highlights
-
•
The U-SDMA extended into the SDIM.
-
•
The perforating branch of SDMA forming a trifurcation in deep palmar area.
-
•
A 3D image of the SDMA variation can promote anatomical knowledge and learning.
1. Introduction
The dorsal metacarpal arteries (DMAs) usually comprise four branches, with the first dorsal metacarpal artery (FDMA) originating directly from the radial artery (RA). In contrast, the remaining branches usually originate from the dorsal carpal arch (DCA). Typically, the second DMAs (SDMAs) originate from the DCA. However, Omokawa et al. report cases where the SDMA directly arises from the RA [1]. Numerous gross anatomy reports indicate that the SDMA progresses distally on the dorsal aspect of the second dorsal interosseous muscle (SDIM), extending through the space between the second and third metacarpal [2]. Clinically, dorsal hand skin flaps are frequently used to repair skin defects in the hand, making the hand's vascular system a focus of interest in hand surgery [3]. This preference is due to the typically stable vascular distribution of the FDMA and SDIM, making them popular for vascular grafts in hand surgery [4]. The SDMA has an extensive branching network under the skin, forming a network of fine blood vessels that supply the skin, containing perforating branches that pass through the SDIM to reach the palm [[5], [6], [7]]. The perforating branch from the DMAs anastomose with the corresponding palmar metacarpal artery (PMA) located deep in the midpalmar space [8]. Our reported case demonstrates that the SDMA, in addition to its typical distribution over the fascia of the muscle, can also delve into the SDIM and traverse deeply within the muscle. Furthermore, after passing through the SDIM, the perforating branch from the SDMA connects to the atypical first palmar metacarpal artery (FPMA) and the atypical deep palmar arch (DPA). These three vessels diverge in three different directions at this point.
These variations can lead to unexpected 'adverse events' during surgeries [9]. Due to the focus on 'typical' anatomical structures in foundational education, newly graduated medical students often need to learn more about individual unique characteristics to enhance diagnostic acuity [10]. Therefore, the teaching of anatomical variations is increasingly garnering attention in the educational process of anatomy [11,12]. Modern anatomical education places greater emphasis on applying new imaging technologies like augmented reality (AR) and virtual reality (VR) [13,14]. In addition to reporting a rare vascular variation in the hand, we created a 3D image using a light detection and ranging (LiDAR) camera that provides detailed information on hand vascular variations for AR/VR-based educational materials and enables remote replication of this variation.
2. Materials and methods
2.1. Cadaveric study
During the 2023 academic year, a unique vascular anomaly in the dorsum of the hand was discovered in a 54-year-old Taiwanese Han male cadaver at the Taipei Medical University. This discovery was made during routine anatomical education sessions focusing on the upper limb anatomy. Arterial embalming was performed by injecting formalin through the femoral artery, allowing the solution to perfuse the entire body via the vascular network. Finally, the cadaver was immersed in formalin for preservation for two years. Vessel diameters and lengths were measured using a digital caliper (LandM Tools, Taiwan) as a reference.
2.2. 3D imaging creation
To capture 3D images of cadaveric hand anomalies, a camera equipped with LiDAR technology was employed, and the images were processed using Metascan software (V2.9.6, Abound Labs Inc.). The P-SDMA represents a notable variation from the dorsal to the palmar side of the hand. To precisely document and display this rare variation, we captured images of the hand and used them to construct 3D representations of both the hand's posterior and anterior parts. To create a detailed and comprehensive visual representation, at least 20 photographs were edited for each 3D image. The output of these images was formatted in three types: mp4 files for video presentations, USDZ files for AR displays, and STL files for 3D printing applications.
The following are the Supplementary data related to this article:
3. Results
3.1. Dorsal hand vasculature variation
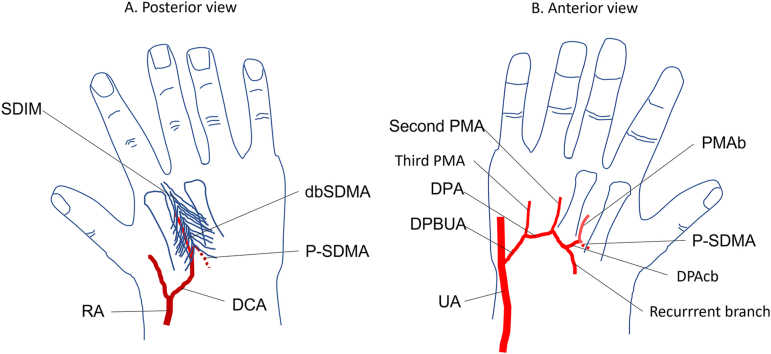
We observed SDMA abnormalities in the right hand. In contrast to its typical extension along the surface of the SDIM between the second and third metacarpals, we find a case in which the SDMA does not extend forward as usual. Instead, it has only one perforating branch extending into the SDIM near the proximal part of the metacarpals, specifically at the level of the capitate and trapezoid bones (Fig. 1A). Upon dissecting this SDMA, we find that it originates from the RA and extends via the dorsal carpal arch (DCA). After further dissection of the SDIM, it is found that the SDMA divides into two branches. One branch extends distally along the second metacarpal in the SDIM, and is called the deep dorsal branch of the SDMA (dbSDMA). The other branch extends deeper into the SDIM and is called the perforating branch of SDMA (P-SDMA) (Fig. 1B). Measurements showed that the diameter of the RA was about 2.0 mm and that of the DCA was slightly smaller, at about 1.5 mm. This diameter was maintained up to the entry point of the SDIM. The length of the vessels from the RA to the P-SDMA, including the DCA and SDMA, is approximately 25.3 mm.
Fig. 1.
Vascular variation of the dorsal hand.
This figure shows the vascular distribution on the dorsum of the hand after the skin is reflected. (A) The SDMA originates from the DCA, a branch of the RA. (B) The SDMA enters the SDIM near the base of the metacarpals, bifurcating into two branches. One branch runs distally through the SDIM along the second metacarpal, termed the deep dorsal branch of the SDMA (dbSDMA). The other is the perforating branch of the SDMA that heads towards the palmar aspect. APL, abductor pollicis longus muscle; DCA, dorsal carpal arch; ED, extensor digitorum muscle; EI, extensor indicis muscle; EPB, extensor pollicis brevis muscle; EPL, extensor pollicis longus muscle; FDIM, first dorsal interosseous muscle; FDMA, first dorsal metacarpal artery; MB2, second metacarpal; RA, radial artery; SDIM, second interosseous muscle; dbSDMA, deep dorsal branch of the SDMA; P-SDMA, perforating branch of the SDMA.
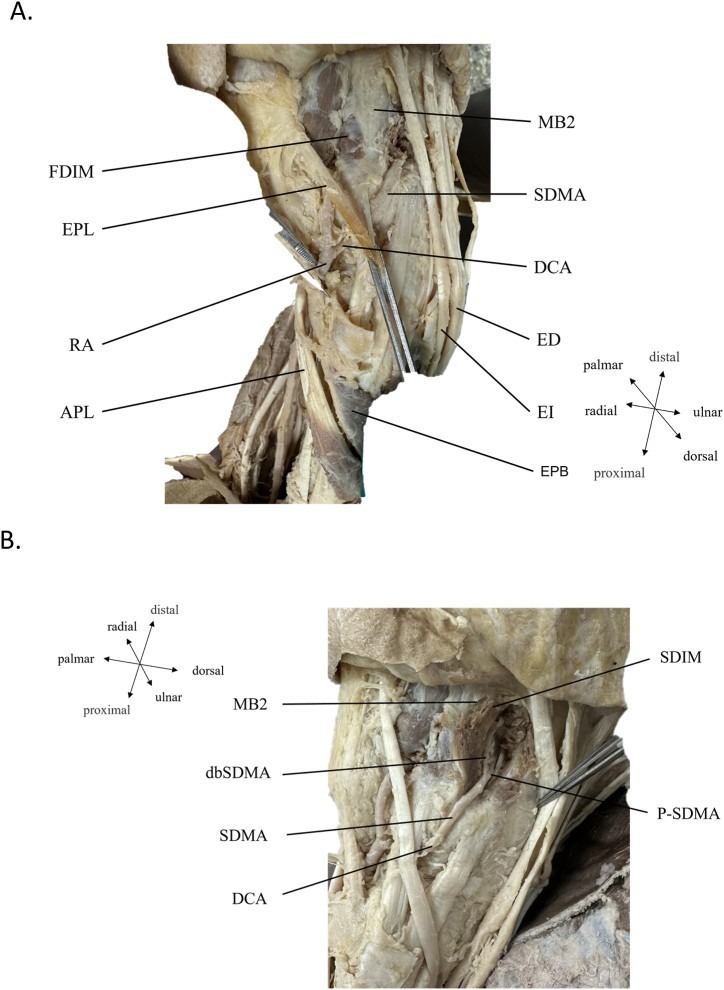
3.2. Palmar hand vasculature variation
To further identify the endpoint of the P-SDMA, the surrounding SDIM is dissected to confirm that the P-SDMA is a perforating artery (Fig. 2A). After opening the muscle tissue of the palm, it is observed that the P-SDMA penetrates from the dorsal side and extends distally between the second and third metacarpals to form the palmar metacarpal artery branch (PMA; PMAb) (Fig. 2B). In addition, the P-SDMA is also found to be connected to the DPA through the connecting branch (DPAcb). The three-way connection point formed by the P-SDMA, DPAcb, and PMAb is called the anastomosis point of the P-SDMA (enlarged in Fig. 2B). It is also observed that the deep palmar arch (DPA) is normally sourced from the ulnar artery and, near the ulnar side, is referred to as the deep palmar branch of the ulnar artery (DPBUA). The DPA also extends toward the third carpal bone at the position of the third metacarpal, which is the recurrent branch (Fig. 2B). Another feature of this vascular variant is that the first PMA in the deep midpalmar space originates from the P-SDMA, while the other PMA still originated from the DPA. The diameter of the ulnar artery (UA) measured approximately 2.3 mm, while the DPA was around 0.7 mm. The diameters of the second and third PMA were reduced to approximately 0.5 mm. Additionally, the PMAb measured about 0.8 mm, and the DPAcb was approximately 0.6 mm (Fig. 2B).
Fig. 2.
Course of the perforating branch of the second dorsal metacarpal artery (SDMA; P-SDMA).
(A) Muscle dissection around the P-SDMA reveals its trajectory towards the deep palmar area. (B) After severing and removing the tendons in the anterior aspect of the forearm and hand and displacing the median nerve and superior palmar arch, we observed the distribution of the P-SDMA in the deep palmar area. The P-SDMA forms an anastomosis with the PMAb and the DPAcb. The PMAb extends distally, while the DPAcb extends proximally to anastomose with the DPA. The enlarged boxed area in the figure highlights these vessels' anastomosis points, showing the branches' convergence from the posterior side, the PMA, and the connecting branch. DPAcb, deep palmar arch connecting branch; DPBUA, deep palmar branch of ulnar artery; ED, extensor digitorum muscle; PMAb, palmar metacarpal artery branch; SDIM, second dorsal interosseous muscle; dbSDMA, deep dorsal branch of the second dorsal metacarpal artery; UA, ulnar artery; APB, abductor pollicis brevis muscle; FPB, flexor pollicis brevis muscle.
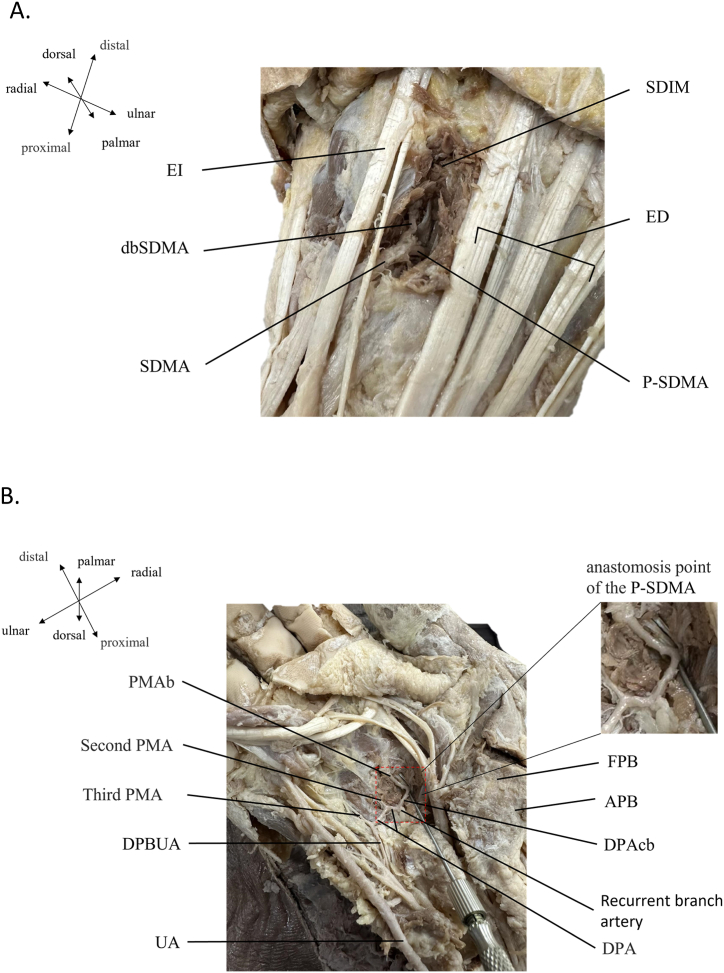
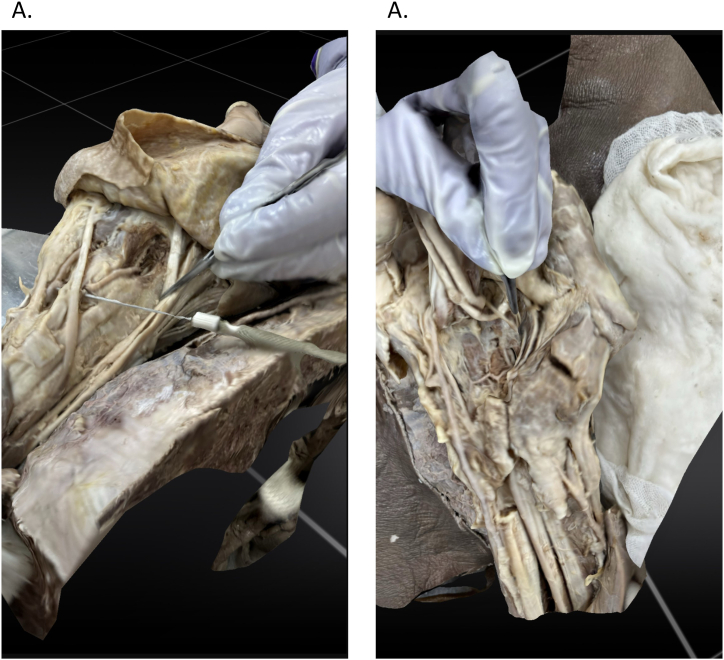
3.3. Creation of 3D images
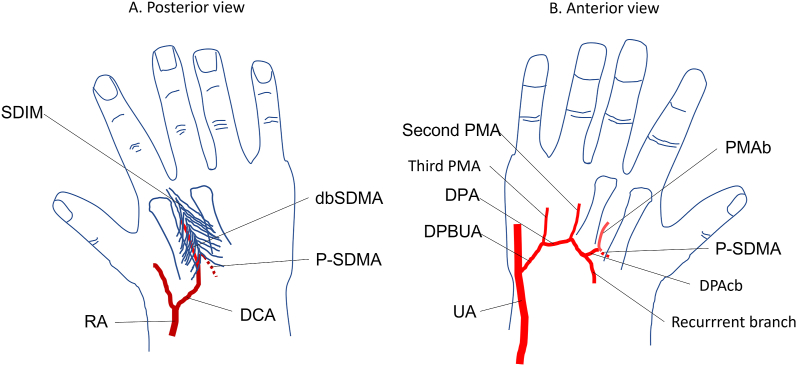
We created 3D images of both the dorsal (Fig. 3A) and palmar (Fig. 3B) aspects of the hand and captured single frames to show the different angles of the variant vessels in the 3D images. Videos are produced to showcase vascular distributions of the hand's posterior view (Supplementary File 1) and anterior view (Supplementary File 2). Additionally, these images are converted into USDZ file format for use in AR applications, with Supplementary File 3 representing the hand's posterior view and Supplementary File 4 depicting the anterior view. STL file format is utilized for 3D printing, with Supplementary File 5 for the hand's posterior view and Supplementary File 6 for the anterior view. (Original files are attached within 3D model files.)
Fig. 3.
3D imaging of anatomical vascular variations in the hand.
(A) A 3D image displaying anatomical details of the dorsal aspect. (B) A 3D image illustrating the anatomy of the perforating branch of the second dorsal metacarpal artery in the palm.
4. Discussion
The most common origin of the SDMA is as an origin from the RA, specifically the DCA. On the dorsal side, after passing through the anatomical snuffbox, the RA forms two branches: the FDMA and the DCA [15]. In most individuals, DMA branches originating from the DCA typically extend distally through the middle and superficial layers of the dorsal interosseous muscles. In addition, perforating arteries on the dorsal side of the hand originate from the DCA and form anastomoses with the PMA in the deep in the midpalmar space [16]. Dawani et al. report a variant case where the perforating branch formed by the SDMA only connects with the UA and not with the RA, which they refer to as an incomplete DPA (Dawani et al., 2022). In this study, we observe that the SDMA enters the SDIM in proximally in the second web space and bifurcated into two branches: one in the deep layer of the SDIM extending distally to form the dbSDMA (Fig. 1B), The other formed a perforating branch toward the deep in the midpalmar space, termed the P-SDMA (Fig. 1B). We also find that the diameters of the SDMA and DCA are similar and not reduced. The P-SDMA forms a new distribution after passing through the deep palm area. This new distribution has two main features. The first point is that the P-SDMA extends distally along the space between the second and third metacarpals in the deep palm area, which is called the PMAb. This means that the origin of this PMAb changes from the DPA to the P-SDMA. Another characteristic is that a connecting branch is formed between the PMAb and the DPA, also known as the DPAcb. Therefore, the P-SDMA, PMAb, and DPAcb in the deep palm area form a unique trigeminal vascular distribution (Fig. 2B, enlarged view). This study demonstrates an atypical pathway and distribution of the SDMA to the DPA (Fig. 4), which has not previously been documented in the literature to our knowledge.
Fig. 4.
Atypical pathway and distribution from the second dorsal metacarpal artery (SDMA) to the deep palmar artery (DPA).
On the dorsal side of the hand, the vascular path of the radial artery (RA)-dorsal carpal arch (DCA)-SDMA enters the second dorsal interosseous muscle (SDIM) after reaching the proximal end of the metacarpal. After that, the SDMA forms two branches: the deep dorsal branch of the SDMA (dbSDMA) and perforating branch of the (P)-SDMA. After the P-SDMA penetrates into the deep areas of the palm, the palmar metacarpal artery branch (PMAb) is formed. the PMA and DPA are connected through the DPA connecting branch (DPAcb). Therefore, a unique trifurcated distribution of the P-SDMA, PMAb, and DPAcb is formed in the deep palm area.
Traditional anatomical education predominantly utilizes 2D illustrations, such as schemes or photographs, which can often lead to difficulties in comprehending complex structures [17]. This is particularly true for unique variations, typically represented only in 2D imagery, potentially prolonging the learning process for newcomers to medical or anatomical studies [12,18]. Modern imaging technology has enabled the creation of 3D images, which greatly enhance the understanding of detailed anatomical variations. Furthermore, these 3D images can be incorporated into AR platforms, providing an innovative approach to teaching gross anatomy [14]. Despite advancing and promoting 3D and VR imaging methods in educational settings, the practical teaching of gross anatomy through cadaveric dissection remains indispensable [19]. This necessity arises partly because current educational imaging systems rely primarily on cartoon-like representations and often lack detailed neurovascular variations. These limitations can result in medical students needing more essential preclinical exposure to physical structures and their variations. Our study, which focuses on vascular variations of the hand requiring dissection of both the dorsal and palmar aspects, underscores the complexities associated with 3D spatial changes of these vessels. The 3D videos we developed articulate these spatial relationships and can be displayed through AR software. Beyond this, 3D printing technology allows remote learners to physically recreate and interact with these complex structures. 3D imagery can be established for anatomical knowledge assessment and clinical skill training. Documenting cadaveric dissections in 3D imagery can significantly enhance students' understanding and learning of complex anatomical structures. Moreover, the study of these variations can aid clinical physicians in understanding clinical conditions and fulfilling the individual clinical needs of each patient [10].
5. Conclusions
This report documents a rare vascular variation in the hand involving the DMA extending into the deep palmar area as the PMA. This variation is primarily characterized by the SDMA extending through the deep part of the second dorsal interosseous muscle, along with a unique distribution pattern where the perforating branch of the SDMA passes through the entire SDIM into the midpalmar space and anastomoses with the DPA. Given the frequent utilization of the SDMA as a source for flaps in hand surgical procedures, this case enhances surgeons' understanding of the dorsal hand vasculature, potentially increasing safety during operations.
Furthermore, we develop a detailed 3D representation of this vascular anomaly, which could serve as a valuable adjunct in medical education and for 3D printing applications. This approach allows for an accurate replication of the variation, which can be particularly beneficial for advancing medical education and clinical skill development. Our findings highlight the importance of recognizing and understanding vascular variations in hand surgery and their potential to enrich teaching resources in medical anatomy.
CRediT authorship contribution statement
Shin-Yun Chen: Visualization, Investigation, Data curation. Wei-Ta Chen: Writing – review & editing. Tsorng-Harn Fong: Formal analysis. Jiun-Lin Horng: Writing – review & editing. Cheng-Ying Chu: Data curation. Haojan Yang: Writing – original draft, Methodology. Tien-Chun Yang: Writing – review & editing, Supervision, Methodology, Conceptualization.
Data availability
Due to concerns about personal privacy and ethical considerations, the data from this study have not been made publicly available. However, the data can be provided upon reasonable request. Researchers interested in accessing the data are welcome to contact the authors to discuss the possibility of obtaining the necessary permissions and access rights.
Ethics statement
This study was reviewed and approved by Taipei Medical University Joint Institutional Review Board with the approval number: N202404151, dated 2024/05/14. The requirement for patient written informed consent was waived by the ethics committee.
Funding
This work was supported by the National Science and Technology Council [grant numbers: NSTC 112-2314-B-038-043]
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Tien-Chun Yang reports financial support was provided by National Science and Technology Council. If there are other authors, they declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2024.e40106
Appendix A. Supplementary data
The following is the supplementary data to this article.
References
- 1.Omokawa S., Tanaka Y., Ryu J., Kish V.L. The anatomical basis for reverse first to fifth dorsal metacarpal arterial flaps. J Hand Surg Br. 2005;30(1):40–44. doi: 10.1016/j.jhsb.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 2.Miletin J., Sukop A., Baca V., Kachlik D. Arterial supply of the thumb: systemic review. Clin. Anat. 2017;30(7):963–973. doi: 10.1002/ca.22973. [DOI] [PubMed] [Google Scholar]
- 3.Webster N., Saint-Cyr M. Flaps based on the dorsal metacarpal artery. Hand Clin. 2020;36(1):75–83. doi: 10.1016/j.hcl.2019.09.001. [DOI] [PubMed] [Google Scholar]
- 4.de Rezende M.R., Mattar Júnior R., Cho A.B., Hasegawa O.H., Ribak S. Anatomic study of the dorsal arterial system of the hand. Rev Hosp Clin Fac Med Sao Paulo. 2004;59(2):71–76. doi: 10.1590/s0041-87812004000200005. [DOI] [PubMed] [Google Scholar]
- 5.Liu P., Deng Z., Zhang T., Li X. Anatomical characteristics of cutaneous branches extending from the second dorsal metacarpal artery. Front. Bioeng. Biotechnol. 2020;8:995. doi: 10.3389/fbioe.2020.00995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu P., Qin X., Zhang H., Sun C., Zheng Y., Xu Y., Ding Z. The second dorsal metacarpal artery chain-link flap: an anatomical study and a case report. Surg. Radiol. Anat. 2015;37(4):349–356. doi: 10.1007/s00276-014-1372-9. [DOI] [PubMed] [Google Scholar]
- 7.Tan R.E.S., Lahiri A. Vascular anatomy of the hand in relation to flaps. Hand Clin. 2020;36(1):1–8. doi: 10.1016/j.hcl.2019.08.001. [DOI] [PubMed] [Google Scholar]
- 8.Olave E., Prates J.C., Gabrielli C., Mandiola E. Perforating branches: important contribution to the formation of the dorsal metacarpal arteries. Scand. J. Plast. ReConstr. Surg. Hand Surg. 1998;32(2):221–227. doi: 10.1080/02844319850158859. [DOI] [PubMed] [Google Scholar]
- 9.Regenbogen S.E., Greenberg C.C., Studdert D.M., Lipsitz S.R., Zinner M.J., Gawande A.A. Patterns of technical error among surgical malpractice claims: an analysis of strategies to prevent injury to surgical patients. Ann. Surg. 2007;246(5):705–711. doi: 10.1097/SLA.0b013e31815865f8. [DOI] [PubMed] [Google Scholar]
- 10.Cheung C.C., Bridges S.M., Tipoe G.L. Why is anatomy difficult to learn? The implications for undergraduate medical curricula. Anat. Sci. Educ. 2021;14(6):752–763. doi: 10.1002/ase.2071. [DOI] [PubMed] [Google Scholar]
- 11.Alraddadi A. Literature review of anatomical variations: clinical significance, identification approach, and teaching strategies. Cureus. 2021;13(4) doi: 10.7759/cureus.14451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nzenwa I.C., Iqbal H.A., Bazira P.J. Exploring the inclusion of anatomical variation in medical education. Anat. Sci. Educ. 2023;16(3):531–546. doi: 10.1002/ase.2254. [DOI] [PubMed] [Google Scholar]
- 13.Chytas D., Johnson E.O., Piagkou M., Mazarakis A., Babis G.C., Chronopoulos E., Nikolaou V.S., Lazaridis N., Natsis K. The role of augmented reality in Anatomical education: an overview. Ann. Anat. 2020;229 doi: 10.1016/j.aanat.2020.151463. [DOI] [PubMed] [Google Scholar]
- 14.Taylor L., Dyer T., Al-Azzawi M., Smith C., Nzeako O., Shah Z. Extended reality anatomy undergraduate teaching: a literature review on an alternative method of learning. Ann. Anat. 2022;239 doi: 10.1016/j.aanat.2021.151817. [DOI] [PubMed] [Google Scholar]
- 15.Dauphin N., Casoli V. The dorsal metacarpal arteries: anatomical study. Feasibility of pedicled metacarpal bone flaps. J Hand Surg Eur. 2011;36(9):787–794. doi: 10.1177/1753193411412872. [DOI] [PubMed] [Google Scholar]
- 16.Poirot Y., Duparc F., Hue A.G., Gandolfi S., Dacher J.N., Auquit-Aukbur I. Cutaneous vascularization of the proximal two-thirds of the dorsal aspect of the hand: descriptive anatomical study of a perforating arterial arch. Surg. Radiol. Anat. 2023;45(9):1073–1081. doi: 10.1007/s00276-023-03185-w. [DOI] [PubMed] [Google Scholar]
- 17.Berney S., Bétrancourt M., Molinari G., Hoyek N. How spatial abilities and dynamic visualizations interplay when learning functional anatomy with 3D anatomical models. Anat. Sci. Educ. 2015;8(5):452–462. doi: 10.1002/ase.1524. [DOI] [PubMed] [Google Scholar]
- 18.Yang D., Morris S.F. Reversed dorsal digital and metacarpal island flaps supplied by the dorsal cutaneous branches of the palmar digital artery. Ann. Plast. Surg. 2001;46(4):444–449. doi: 10.1097/00000637-200104000-00017. [DOI] [PubMed] [Google Scholar]
- 19.Triepels C.P.R., Smeets C.F.A., Notten K.J.B., Kruitwagen R., Futterer J.J., Vergeldt T.F.M., Van Kuijk S.M.J. Does three-dimensional anatomy improve student understanding? Clin. Anat. 2020;33(1):25–33. doi: 10.1002/ca.23405. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Due to concerns about personal privacy and ethical considerations, the data from this study have not been made publicly available. However, the data can be provided upon reasonable request. Researchers interested in accessing the data are welcome to contact the authors to discuss the possibility of obtaining the necessary permissions and access rights.