Abstract
Background
Diarrhea remains a significant health threat to children under five years of age. The study aims to systematically elucidate the global burden of diarrhea in children, providing scientific insights for effective prevention and control strategies.
Methods
The data from the Global Burden of Disease (GBD) 2021 study was analyzed to assess the trends in incidence, prevalence, mortality, and disability-adjusted life years (DALYs) of diarrhea in children under five years across the globe, 21 geographical region, and 204 countries and territories, stratified by age group, sex, and socio-demographic index (SDI) levels. The trend of the disease burden for childhood diarrhea from 1990 to 2021 was described and estimated using the average annual percent change (AAPC), and a Bayesian age-period-cohort (BAPC) model was employed to predict the future burden of diarrhea in children.
Results
From 1990 to 2021, there was a significant decline in the global burden of diarrhea among children under five years of age. The AAPC for incidence (−4092.18, 95% confidence interval [CI]: −4224.60 to −3959.76), prevalence (−70.98, 95% CI: −72.67 to −69.28), mortality (−6.89, 95% CI: −6.95 to −6.83), and DALYs rate (−621.79, 95% CI: −627.20 to −616.38) of diarrhea in children all showed a marked downward trend. Diarrheal incidence (r = −0.782, P < 0.001), prevalence (r = −0.777, P < 0.001), mortality (r = −0.908, P < 0.001), and DALYs rate (r = −0.904, P < 0.001) were negatively correlated with the SDI. Between 2022 and 2035, the global incidence, prevalence, and mortality rates of diarrhea in children under five years are projected to continue declining. The leading causes of diarrheal mortality in children include wasting, underweight, and non-exclusive breastfeeding. Rotavirus remains the predominant pathogen associated with diarrhea-related mortality rate and DALY rate.
Conclusion
Although the global burden of diarrhea in children under five has steadily declined, it remains a significant health threat. Rotavirus is the leading pathogen, highlighting the importance of expanding rotavirus vaccination. Additionally, improving nutritional status, increasing exclusive breastfeeding rates, and enhancing access to sanitation and clean drinking water are crucial measures that, when widely implemented, can effectively reduce the health risks posed by diarrhea in children.
Keywords: Diarrheal disease, Children, Global Burden of Disease study 2021, Projections, One Health
1. Introduction
Diarrhea is characterized by passing stool more than three times a day, with abnormally loose or watery consistency [[1], [2], [3]]. The causes of diarrhea are diverse and include food allergies, irritable bowel syndrome, gastrointestinal tumors, and infections of the digestive tract [4,5]. Among these, gastrointestinal infections are one of the leading causes. Pathogens responsible for diarrhea include viruses (e.g., rotavirus, norovirus, astrovirus, and adenovirus), bacteria (e.g., enteropathogenic Escherichia coli, Shigella, Campylobacter, non-typhoidal Salmonella, and Clostridium difficile), and parasites (e.g., Entamoeba histolytica, Cryptosporidium, Giardia lamblia, helminths, worms, etc.) [2,[6], [7], [8], [9]].
Diarrhea poses a significant health threat to children under five years of age. It can cause substantial loss of fluids and electrolytes, leading to dehydration, which may result in shock, organ failure, or even death [5,10]. In addition, diarrhea impairs nutrient absorption, contributing to malnutrition, which not only affects growth and development but can also lead to underweight and stunted growth [5,10]. Recurrent diarrhea weakens the immune system, making children more susceptible to other infections, creating a vicious cycle of immune dysfunction [11]. Certain pathogens, such as Shigella or Campylobacter, can cause severe complications, including sepsis, intestinal perforation, and acute kidney failure [12]. Diarrhea remains one of the leading causes of child mortality globally, with an estimated 500,000 children under five dying each year from diarrhea and its complications, particularly in low- and middle-income countries, with the highest burden seen in Sub-Saharan Africa and South Asia [3,13,14].
A comprehensive understanding of the burden and epidemiological trends of diarrheal disease among children under five is critical for guiding the development of effective control policies and strategies. Since the 1990s, many studies have aimed to estimate the global burden of diarrheal disease in children. However, systematic and comparative studies of the global burden of childhood diarrhea remain inconsistent. The Global Burden of Disease (GBD) study has provided a comprehensive and systematic approach to evaluate a wide range of global health issues since 1990 [[15], [16], [17], [18], [19]]. Therefore, the data from the GBD was used to analyze the incidence, prevalence, mortality, and disability-adjusted life years (DALYs) of diarrheal disease in children under five years, stratified by sex, socio-demographic index (SDI), and etiology at the range of global, super-region, and 204 countries and territories, from 1990 to 2021 [18,19]. The study aims to provide data on the burden of diarrheal diseases in children under five for international organizations, governments, health agencies, researchers, and clinicians. The findings will help identify the epidemiological characteristics and burden of diarrheal diseases in children, providing evidence for the formulation of scientific prevention and control strategies.
2. Methods
2.1. Data source
The GBD study 2021 assessed the disease burden of 371 diseases and injuries and 88 risk factors across the globe, super-region, and 204 countries and territories [18,19]. The incidence, prevalence, mortality, and DALYs of each disease for different age groups and regions were model-based estimate. The study utilized the Disease Modeling-Bayesian Meta-Regression (DisMod-MR) tool (version 2.1), employing Bayesian priors, regularization, and multi-dimensional smoothing modeling. Mortality data in GBD 2021 were primarily sourced from national death registration systems, maternal and child health surveillance networks, and population census data. Incidence and prevalence data were derived from disease surveillance systems, national health surveys, and published literature. The burden of disability was estimated using data from case notifications, hospital discharge databases, household surveys, and cohort studies [18,19]. Detailed information on the study design, data collection, and estimation methods can be found elsewhere [18,19].
From the disease in the GBD study 2021, data from the Global Enteric Multicenter Study (GEMS)—a seven-site case–control study on moderate-to-severe diarrhea in children under five years—were utilized to calculate odds ratios for diarrheal pathogens [2,9,10]. The raw data were systematically reanalyzed, ensuring representation of the distribution of cases and controls by age and site, with pathogens detected using quantitative polymerase chain reaction (qPCR) [20]. For data that did not employ qPCR, adjustments were made for sensitivity and specificity prior to modeling to standardize the data across different detection methods. This pre-modeling adjustment improved consistency, particularly for non-qPCR datasets, and provided more accurate control of extreme values, while capturing uncertainty in the model [[18], [19], [20]].
The SDI is a composite measure that reflects the social and economic conditions affecting health outcomes in different locations. It is calculated as the geometric mean of three indicators: total fertility rate among individuals younger than 25 years, mean years of education for those aged 15 years or older, and lag-distributed income per capita [18,19]. In the GBD study 2021, SDI values were multiplied by 100 to provide a scale ranging from 0 to 100 [18,19]. They are grouped into five development levels: low (< 0.46), low-middle (0.46–0.60), middle (0.61–0.69), high-middle (0.70–0.81), and high (> 0.81) [16,18,19].
2.2. Data sources
Data were obtained from the Institute for Health Metrics and Evaluation website (https://vizhub.healthdata.org), including the incidence, prevalence, mortality, and DALYs rates and numbers for children under five years with 95% uncertainty intervals (UIs), disaggregated by sex, region, super-region, and 204 countries and territories from 1990 to 2021 [18,19]. The classification of diarrheal diseases followed the International Classification of Diseases (ICD) by the World Health Organization (WHO), using ICD-9 codes 001–009.9 and ICD-10 codes A00–A09 [18,19].
2.3. Statistical analysis
The percentage changes in the numbers and rates (incidence, prevalence, mortality, and DALYs) between 1990 and 2021 were calculated using the following formula [18,19]:
| Percentage change = (value2021-value1990)/ value2021 × 100% |
The GBD study 2021 database reports UIs rather than precise statistical values. As a result, statistical significance cannot be directly calculated when comparing two numerical values (e.g., numbers, rates, or percentages). Overlapping UIs indicate no significant difference (P > 0.05), whereas non-overlapping UIs suggest a statistically significant difference (P < 0.05) [15,16].
In addition, the estimated annual percentage changes (EAPCs) for rates and numbers were calculated to illustrate trends [21]. The EAPC was derived using the formula: EAPC = 100 × (eβ-1), where the 95% confidence intervals (CIs) for the EAPC were based on the estimation of β. An increasing trend was indicated if both the EAPC estimate and the lower limit of its 95% CI were greater than zero. Conversely, a decreasing trend was identified if both the EAPC estimate and the upper limit of its 95% CI were below zero. If neither condition was met, the trend was considered stable [22].
Smoothing spline models were employed to assess the association between the burden of diarrheal disease (rates) and the SDI across the globe, five SDI regions, 21 geographical regions, and 204 countries and territories [15,23,24]. Locally weighted scatterplot smoothing was applied, with the degree, number, and location of knots automatically determined based on the data and the span parameter [15,23]. Spearman's rank correlation coefficient was used to confirm the correlation between burden of diarrheal disease (rates) and SDI [15,23]. A P-value of <0.05 was considered statistically significant.
The joinpoint regression model provides a detailed linear analysis of the long-term trends in the incidence, prevalence, mortality, and DALYs rates of diarrheal diseases for children under five years [25]. The standard error was calculated using the formula:
| Standard error= (upper limit-lower limit) / (1.96 × 2) |
The joinpoint regression model divides the trend lines into distinct phases, calculating the average annual percent change (AAPC) to represent the overall change of rate across the entire period, and the annual percent change (APC) to capture rate variations within specific time intervals [26,27]:
In this model, the number and position of the joinpoint was determined using the grid search method (GSM) [28]. In the model, i is the number of segments, βi corresponds to the regression coefficients for each linear segment of the data. Wi is the regression coefficient weights represented by the length of each corresponding segment. Model selection was optimized using the Monte Carlo permutation test and the modified Bayesian Information Criterion, with the model that minimized the mean squared error being selected [29]. Both the APC and AAPC are unitless relative measures that indicate the direction and rate of trend changes. A negative AAPC or APC, with the upper limit of the 95% CI below zero, suggests a declining trend over time. Conversely, a positive AAPC or APC, with the lower limit of the 95% CI above zero, indicates an increasing trend. If neither condition is met, the rate is considered stable, with no significant change over the observed period [30,31].
The Bayesian age-period-cohort (BAPC) model was used to predict the global incidence, prevalence, and mortality of diarrheal disease from 2022 to 2035, with 95% CIs calculated [32]. The BAPC model accounts for age, period, and cohort factors. Age is a key risk factor for many diseases, while period and birth cohort serve as proxies for other unmeasured factors. The BAPC model is a log-linear Poisson model that assumes multiplicative effects of age, period, and cohort [15,16,32]:
In this model, i (1 ≤ i ≤ I) represents the time points, (1 ≤ ≤ ) represents the age groups, α denotes the intercept, μi indicates the age effect, βj represents the period effect, γk denotes the cohort effect. BAPC model utilized integrated nested laplace approximation (INLA) to approximate the posterior marginal distribution, thereby avoiding issues related to mixing and convergence, and demonstrating relatively low error rates [33]. The prior distribution for age, period, and cohort effects was set as an inverse gamma distribution. A second-order random walk model was applied to adjust for overdispersion. Predictions were made using the R-BAPC and R-INLA packages [15,16].
All statistical analyses were performed using R software (version 4.4.1, R Foundation for Statistical Computing, Vienna, Austria; available at https://cran.r-project.org).
3. Results
3.1. Global
The incidence rate of diarrhea in children under five years decreased from 190,036.82 per 100,000 population in 1990 (95% UI: 161,363.74–220,431.93 per 100,000 population) to 59,677.27 per 100,000 population in 2021 (95% UI: 149,246.22–70,442.60 per 100,000 population), showing a significant downward trend (AAPC = −4092.18, 95% CI: −4224.60 to −3959.76) (Table 1). The number of cases declined from 1.18 billion in 1990 (95% UI: 1.00–1.37 billion) to 392.78 million in 2021 (95% UI: 324.12–463.63 million), also demonstrating a clear decreasing trend (Table S1).
Table 1.
The incidence rate of diarrheal disease among children under five years in 1990 and 2021, and the changing trend of incidence rate across different GBD regions.
| Location | Incidence rate per 100,000 population (95% UI) in 1990 | Incidence rate per 100,000 population (95% UI) in 2021 | Percentage change of incidence rate (95% UI) in 1990–2021/% | AAPC of incidence rate (95% CI) in 1990–2021/% |
|---|---|---|---|---|
| Global | 190,036.82 (161,363.74–220,431.93) | 59,677.27 (49,246.22–70,442.60) | −68.60 (−70.19 to −66.63) | −4092.18 (−4224.60 to −3959.76) |
| East Asia | 104,006.49 (82,013.64–131,205.90) | 14,742.90 (10,627.07–19,781.98) | −85.83 (−87.88 to −83.24) | −2960.49 (−3003.42 to −2917.57) |
| Southeast Asia | 248,000.47 (212,584.70–281,001.18) | 111,478.52 (91,322.47–135,033.26) | −55.05 (−58.67 to −50.41) | −4164.92 (−4302.15 to −4027.69) |
| Oceania | 187,663.02 (163,852.48–213,114.60) | 128,542.07 (107,231.53–150,654.43) | −31.50 (−38.15 to −23.93) | −2167.86 (−2294.18 to −2041.53) |
| Central Asia | 142,467.30 (125,857.87–160,469.60) | 18,127.20 (14,904.27–21,608.89) | −87.28 (−88.75 to −85.87) | −3973.18 (−4028.19 to −3918.18) |
| Central Europe | 22,642.57 (17,810.52–28,421.52) | 9106.30 (7028.84–11,423.00) | −59.78 (−61.76 to −57.92) | −425.85 (−446.07 to −405.63) |
| Eastern Europe | 116,613.14 (92,852.91–145,267.41) | 26,040.53 (19,294.85–33,600.13) | −77.67 (−79.85 to −74.91) | −2939.59 (−2987.84 to −2891.34) |
| High-income Asia Pacific | 67,374.35 (47,636.16–91,142.81) | 84,612.72 (60,477.92–112,172.01) | 25.59 (17.49–34.20) | 561.60 (498.80–624.41) |
| Australasia | 32,930.58 (23,674.52–43,552.97) | 11,196.47 (8319.09–14,674.70) | −66.00 (−68.95 to −62.97) | −654.46 (−723.85 to −585.08) |
| Western Europe | 84,540.02 (59,028.64–114,761.61) | 73,024.26 (52,433.84–96,060.38) | −13.62 (−17.84 to −9.58) | −567.95 (−687.11 to −448.78) |
| Southern Latin America | 11,2707.95 (92,207.81–136,429.58) | 24,808.92 (18,397.90–32,314.12) | −77.99 (−80.47 to −75.21) | −2780.67 (−2901.99 to −2659.35) |
| High-income North America | 34,799.33 (23,898.70–48,779.02) | 3133.27 (2437.97–3988.19) | −91.00 (−92.05 to −89.65) | −1134.00 (−1256.87–1011.14) |
| Caribbean | 119,415.30 (101,792.96–137,246.08) | 38,349.64 (31,329.31–46,183.04) | −67.89 (−70.71 to −65.02) | −2600.47 (−2650.35 to −2550.59) |
| Andean Latin America | 298,341.14 (274,448.62–320,996.02) | 30,127.88 (23,855.90–37,159.56) | −89.90 (−91.64 to −88.05) | −8789.01 (−8902.36 to −8675.65) |
| Central Latin America | 140,741.46 (115,360.75–168,584.09) | 32,084.93 (25,506.19–39,269.03) | −77.20 (−79.06 to −75.06) | −3509.99 (−3690.22 to −3329.77) |
| Tropical Latin America | 168,221.48 (134,782.50–204,546.76) | 33,785.22 (25,772.38–42,958.65) | −79.92 (−81.54 to −78.28) | −4458.78 (−4559.19 to −4358.36) |
| North Africa and middle East | 207,714.03 (180,852.51–235,848.08) | 52,841.49 (43,771.71–62,111.00) | −74.56 (−76.41 to −72.61) | −4995.55 (−5083.05 to −4908.06) |
| South Asia | 245,339.91 (201,409.66–288,523.89) | 67,464.36 (55,874.31–80,365.75) | −72.50 (−75.24 to −69.61) | −5795.93 (−5938.69 to −5653.16) |
| Central Sub-Saharan Africa | 284,869.93 (251,509.28–313,343.25) | 78,226.09 (65,314.85–91,468.22) | −72.54 (−75.31 to −69.23) | −7202.70 (−7457.16 to −6948.23) |
| Eastern Sub-Saharan Africa | 287,099.13 (253,703.12–315,663.24) | 65,906.62 (56,815.54–75,948.77) | −77.04 (−78.88 to −74.92) | −7186.52 (−7278.08 to −7094.96) |
| Southern Sub-Saharan Africa | 276,250.38 (238,171.64–307,177.75) | 58,170.76 (48,238.40–69,008.00) | −78.94 (−81.30 to −76.09) | −7184.05 (−7293.31 to −7074.78) |
| Western Sub-Saharan Africa | 302,392.13 (270,575.89–329,265.97) | 87,324.99 (73,552.10–102,170.00) | −71.12 (−74.03 to −67.42) | −6978.14 (−7072.77 to −6883.51) |
| High-middle SDI region | 103,449.61 (83,384.50–126,918.36) | 28,839.35 (21,847.11–37,098.64) | −72.12 (−74.63 to −69.08) | −2393.91 (−2453.79 to −2334.03) |
| High SDI region | 60,947.41 (44,147.87–81,455.25) | 40,284.05 (28,810.45–53,250.29) | −33.90 (−37.97 to −29.85) | −699.24 (−791.83 to −606.64) |
| Low-middle SDI region | 251,624.87 (215,250.71–286,288.87) | 69,133.80 (58,047.60–81,026.57) | −72.53 (−74.24 to −70.53) | −6050.90 (−6171.98 to −5929.81) |
| Low SDI region | 279,033.44 (244,801.18–310,490.10) | 79,236.37 (66,678.62–92,048.61) | −71.60 (−73.63 to −69.15) | −6591.68 (−6706.93 to −6476.43) |
| Middle SDI region | 176,443.85 (146,844.76–208,421.94) | 49,207.02 (40,006.75–59,304.93) | −72.11 (−73.49 to −70.54) | −3972.06 (−4045.51 to −3898.61) |
Abbreviations: GBD, Global Burden of Disease; AAPC, average annual percent change; CI, confidence interval; UI, uncertainty interval; SDI, socio-demographic index.
The prevalence rate of diarrhea among children under five decreased from 3138.81 per 100,000 population in 1990 (95% UI: 2749.19–3557.51 per 100,000 population) to 885.07 per 100,000 population in 2021 (95% UI: 755.93–1029.39 per 100,000 population), showing a significant downward trend (AAPC = −70.98, 95% CI: −72.67 to −69.28) (Table 2). The number of prevalent cases also declined, from 19.46 million in 1990 (95% UI: 17.04–22.05 million) to 5.83 million in 2021 (95% UI: 4.98–6.78 million), demonstrating a clear decrease (Table S2).
Table 2.
The prevalence rate of diarrheal disease among children under five years in 1990 and 2021, and the changing trend of prevalence rate across different GBD regions.
| Location | Prevalence rate per 100,000 population (95% UI) in 1990 | Prevalence rate per 100,000 population (95% UI) in 2021 | Percentage change of prevalence rate (95% UI) in 1990–2021/% | AAPC of prevalence rate (95% CI) in 1990–2021/% |
|---|---|---|---|---|
| Global | 3138.81 (2749.19–3557.51) | 885.07 (755.93–1029.39) | −71.80 (−73.52 to −69.93) | −70.98 (−72.67 to −69.28) |
| East Asia | 1724.34 (1364.10–2142.63) | 212.38 (157.97–279.26) | −87.68 (−89.71 to −85.51) | −49.49 (−50.17 to −48.81) |
| Southeast Asia | 4300.84 (3797.58–4793.93) | 1727.26 (1465.46–2061.26) | −59.84 (−63.83 to −54.78) | −87.72 (−91.19 to −84.25) |
| Oceania | 3039.81 (2742.84–3358.90) | 1942.08 (1684.67–2228.69) | −36.11 (−42.01 to −29.43) | −39.83 (−41.91 to −37.76) |
| Central Asia | 2416.84 (2225.11–2638.90) | 259.89 (222.13–301.55) | −89.25 (−90.52 to −87.95) | −68.46 (−69.50 to −67.42) |
| Central Europe | 388.80 (318.60–470.24) | 139.56 (112.90–171.80) | −64.10 (−66.60 to −61.91) | −8.00 (−8.30 to −7.71) |
| Eastern Europe | 1899.31 (1553.15–2327.27) | 383.97 (295.49–486.54) | −79.78 (−81.81 to −77.67) | −47.23 (−48.20 to −46.25) |
| High-income Asia Pacific | 1040.13 (769.11–1389.91) | 1263.44 (952.92–1640.22) | 21.47 (10.95–31.13) | 7.57 (6.53–8.61) |
| Australasia | 498.27 (375.67–670.19) | 171.89 (134.37–223.82) | −65.50 (−68.76 to −62.23) | −9.85 (−10.86 to −8.85) |
| Western Europe | 1264.65 (918.55–1727.32) | 1117.42 (825.03–1473.44) | −11.64 (−16.81 to −4.75) | −7.15 (−9.23 to −5.07) |
| Southern Latin America | 1693.70 (1434.36–1983.09) | 357.15 (277.40–448.02) | −78.91 (−81.49 to −76.08) | −41.69 (−43.73 to −39.65) |
| High-income North America | 559.59 (388.05–788.05) | 52.37 (41.84–65.49) | −90.64 (−92.05 to −88.96) | −18.26 (−20.29 to −16.23) |
| Caribbean | 1801.51 (1612.10–1992.35) | 547.47 (466.73–643.56) | −69.61 (−72.13 to −67.00) | −39.81 (−40.79 to −38.83) |
| Andean Latin America | 5405.56 (5039.58–5758.60) | 428.94 (353.58–508.88) | −92.06 (−93.29 to −90.55) | −161.67 (−162.87 to −160.48) |
| Central Latin America | 2208.59 (1880.05–2588.08) | 474.81 (395.55–565.60) | −78.50 (−80.13 to −76.74) | −56.10 (−58.38 to −53.83) |
| Tropical Latin America | 2814.90 (2335.91–3351.51) | 495.70 (388.32–618.03) | −82.39 (−84.07 to −80.85) | −76.90 (−78.57 to −75.23) |
| North Africa and middle East | 3581.24 (3225.41–3957.60) | 786.81 (683.37–907.98) | −78.03 (−79.87 to −76.23) | −90.56 (−92.52 to −88.60) |
| South Asia | 3801.35 (3222.38–4445.53) | 985.91 (839.65–1163.61) | −74.06 (−76.55 to −71.21) | −91.97 (−94.10 to −89.84) |
| Central Sub-Saharan Africa | 5081.00 (4605.53–5537.31) | 1125.27 (972.04–1309.66) | −77.85 (−80.23 to −74.90) | −137.79 (−142.18 to −133.39) |
| Eastern Sub-Saharan Africa | 5027.46 (4575.44–5510.32) | 974.18 (866.67–1102.37) | −80.62 (−82.35 to −78.58) | −132.66 (−134.11 to −131.20) |
| Southern Sub-Saharan Africa | 4596.87 (3988.59–5179.94) | 895.13 (771.03–1037.96) | −80.53 (−82.82 to −77.73) | −122.28 (−124.15 to −120.41) |
| Western Sub-Saharan Africa | 5262.77 (4744.19–5735.65) | 1277.72 (1119.73–1472.29) | −75.72 (−78.25 to −72.55) | −129.52 (−131.52 to −127.53) |
| High-middle SDI region | 1659.29 (1366.30–2012.20) | 423.52 (334.16–530.67) | −74.48 (−77.06 to −71.95) | −39.91 (−40.54 to −39.27) |
| High SDI region | 939.43 (708.39–1250.85) | 608.41 (456.01–799.00) | −35.24 (−39.71 to −31.09) | −10.91 (−12.41 to −9.42) |
| Low-middle SDI region | 4144.11 (3663.65–4673.73) | 1032.66 (899.96–1189.28) | −75.08 (−76.88 to −73.06) | −103.49 (−105.57 to −101.42) |
| Low SDI region | 4752.56 (4299.25–5224.10) | 1157.71 (1014.17–1325.92) | −75.64 (−77.63 to −73.17) | −115.73 (−116.98 to −114.48) |
| Middle SDI region | 2903.06 (2479.77–3362.19) | 736.45 (620.83–875.57) | −74.63 (−76.16 to −73.08) | −67.39 (−68.78 to −66.00) |
Abbreviations: GBD, Global Burden of Disease; AAPC, average annual percent change; CI, confidence interval; UI, uncertainty interval; SDI, socio-demographic index.
The mortality rate of diarrhea in children under five fell from 263.95 per 100,000 population in 1990 (95% UI: 207.34–311.47 per 100,000 population) to 51.72 per 100,000 population in 2021 (95% UI: 38.13–70.54 per 100,000 population), reflecting a significant decline (AAPC = −6.89, 95% CI: −6.95 to −6.83) (Table 3). The number of deaths decreased from 1.64 million in 1990 (95% UI: 1.29–1.93 million) to 0.34 million in 2021 (95% UI: 0.25–0.46 million), showing a consistent downward trend (Table S3).
Table 3.
The mortality rate of diarrheal disease among children under five years in 1990 and 2021, and the changing trend of the mortality rate across different GBD regions.
| Location | Mortality rate per 100,000 population (95% UI) in 1990 | Mortality rate per 100,000 population (95% UI) in 2021 | Percentage change of mortality rate (95% UI) in 1990–2021/% | AAPC of mortality rate (95% CI) in 1990–2021/% |
|---|---|---|---|---|
| Global | 263.95 (207.34–311.47) | 51.72 (38.13–70.54) | −80.40 (−85.53 to −74.04) | −6.89 (−6.95 to −6.83) |
| East Asia | 62.68 (46.37–79.32) | 0.99 (0.75–1.36) | −98.42 (−98.85 to −97.85) | −2.01 (−2.05 to −1.96) |
| Southeast Asia | 292.38 (182.00–379.88) | 24.34 (18.27–31.88) | −91.68 (−94.09 to −86.71) | −8.63 (−8.79 to −8.47) |
| Oceania | 191.18 (133.17–280.73) | 91.31 (55.02–142.36) | −52.24 (−68.61 to −30.03) | −3.29 (−3.48 to −3.09) |
| Central Asia | 143.58 (129.43–160.05) | 17.17 (12.41–23.07) | −88.04 (−91.60 to −83.93) | −4.20 (−4.36 to −4.04) |
| Central Europe | 8.46 (7.53–9.51) | 3.31 (2.70–3.90) | −60.81 (−68.35 to −52.61) | −0.15 (−0.16 to −0.14) |
| Eastern Europe | 8.04 (7.62–8.48) | 0.90 (0.80–1.00) | −88.79 (−90.02 to −87.57) | −0.22 (−0.24 to −0.20) |
| High-income Asia Pacific | 1.69 (1.41–2.12) | 0.66 (0.58–0.75) | −60.87 (−68.89 to −50.71) | −0.03 (−0.03 to −0.03) |
| Australasia | 0.89 (0.78–1.01) | 0.33 (0.27–0.41) | −62.68 (−71.23 to −52.29) | −0.02 (−0.02 to −0.01) |
| Western Europe | 0.73 (0.67–0.80) | 0.63 (0.53–0.73) | −14.15 (−28.08 – 1.33) | −0.00 (−0.01 to −0.00) |
| Southern Latin America | 16.71 (15.34–18.20) | 2.07 (1.63–2.64) | −87.60 (−90.39 to −83.86) | −0.47 (−0.51 to −0.44) |
| High-income North America | 1.03 (0.97–1.10) | 0.57 (0.49–0.65) | −45.15 (−53.05 to −37.00) | −0.01 (−0.02 to −0.01) |
| Caribbean | 303.39 (248.83–360.48) | 102.75 (68.75–142.91) | −66.13 (−77.85 to −53.29) | −7.00 (−8.10 to −5.90) |
| Andean Latin America | 149.07 (124.59–178.45) | 9.16 (5.99–12.99) | −93.86 (−95.92 to −91.48) | −5.21 (−5.59 to −4.84) |
| Central Latin America | 172.73 (159.29–188.61) | 14.45 (10.50–19.28) | −91.64 (−94.03 to −88.71) | −4.95 (−5.09 to −4.81) |
| Tropical Latin America | 184.75 (157.68–212.97) | 4.35 (3.40–5.50) | −97.65 (−98.21 to −96.93) | −5.88 (−5.97 to −5.79) |
| North Africa and middle East | 176.43 (132.04–226.29) | 18.77 (13.22–28.93) | −89.36 (−92.17 to −85.78) | −5.04 (−5.11 to −4.97) |
| South Asia | 390.69 (311.63–469.33) | 35.41 (21.76–51.39) | −90.94 (−94.54 to −86.77) | −11.67 (−11.86 to −11.48) |
| Central Sub-Saharan Africa | 583.73 (406.19–736.64) | 63.63 (39.01–98.54) | −89.10 (−92.81 to −82.07) | −16.57 (−17.02 to −16.11) |
| Eastern Sub-Saharan Africa | 566.66 (357.13–776.49) | 104.50 (72.49–151.08) | −81.56 (−88.54 to −69.62) | −15.14 (−15.42 to −14.85) |
| Southern Sub-Saharan Africa | 316.37 (273.20–364.18) | 100.89 (74.14–134.47) | −68.11 (−75.32 to −59.32) | −7.42 (−7.90 to −6.95) |
| Western Sub-Saharan Africa | 810.81 (566.21–1007.66) | 197.35 (132.88–287.80) | −75.66 (−82.55 to −65.46) | −20.36 (−20.76 to −19.96) |
| High-middle SDI region | 35.61 (28.39–42.82) | 2.40 (1.86–3.00) | −93.27 (−94.67 to −91.63) | −1.07 (−1.09 to −1.05) |
| High SDI region | 3.39 (2.62–4.57) | 0.79 (0.68–0.89) | −76.71 (−82.78 to −69.55) | −0.08 (−0.09 to −0.08) |
| Low-middle SDI region | 426.17 (343.75–497.47) | 44.63 (33.79–59.80) | −89.53 (−92.28 to −85.54) | −12.42 (−12.50 to −12.34) |
| Low SDI region | 630.33 (459.39–790.35) | 137.15 (96.81–190.65) | −78.24 (−84.66 to −67.94) | −16.30 (−16.57 to −16.03) |
| Middle SDI region | 143.86 (110.85–170.60) | 14.40 (11.00–18.93) | −89.99 (−92.05 to −87.70) | −4.18 (−4.24 to −4.12) |
Abbreviations: GBD, Global Burden of Disease; AAPC, average annual percent change; CI, confidence interval; UI, uncertainty interval; SDI, socio-demographic index.
The DALY rate due to diarrhea in children under five years dropped from 23,838.68 per 100,000 population in 1990 (95% UI: 18,844.31–28,015.78 per 100,000 population) to 4699.58 per 100,000 population in 2021 (95% UI: 3512.49–6376.29 per 100,000 population), indicating a significant reduction (AAPC = −621.79, 95% CI: −627.20 to −616.38) (Table 4). Correspondingly, the number of DALYs decreased from 147.79 million in 1990 (95% UI: 116.82–173.68 million) to 30.93 million in 2021 (95% UI: 23.12–41.97 million), showing a marked decline (Table S4).
Table 4.
The DALY rate of diarrheal disease among children under five years in 1990 and 2021, and the changing trend of the DALY rate across different GBD regions.
| Location | DALY rate per 100,000 population (95% UI) in 1990 | DALY rate per 100,000 population (95% UI) in 2021 | Percentage change of DALY rate (95% UI) in 1990–2021/% | AAPC of DALY rate (95% CI) in 1990–2021/% |
|---|---|---|---|---|
| Global | 23,838.68 (18,844.31–28,015.78) | 4699.58 (3512.49–6376.29) | −80.29 (−85.31 to −74.05) | −621.79 (−627.20 to −616.38) |
| East Asia | 5773.92 (4343.03–7250.92) | 113.43 (88.33–146.69) | −98.04 (−98.55 to −97.41) | −182.65 (−186.59 to −178.71) |
| Southeast Asia | 26,528.93 (16,790.15–34,260.42) | 2369.54 (1810.56–3036.72) | −91.07 (−93.54 to −86.03) | −775.81 (−790.43 to −761.20) |
| Oceania | 17,364.81 (12,219.49–25,393.35) | 8346.77 (5149.29–12,916.15) | −51.93 (−67.92 to −30.27) | −297.12 (−314.42 to −279.83) |
| Central Asia | 13,085.32 (11,796.98–14,569.95) | 1560.82 (1130.19–2084.09) | −88.07 (−91.56 to −84.07) | −380.85 (−395.97 to −365.73) |
| Central Europe | 801.57 (719.75–889.34) | 312.79 (259.04–365.82) | −60.98 (−68.12 to −53.19) | −14.36 (−15.56 to −13.17) |
| Eastern Europe | 938.96 (853.08–1040.35) | 125.33 (108.31–146.80) | −86.65 (−87.88 to −85.30) | −25.19 (−27.12 to −23.26) |
| High-income Asia Pacific | 272.31 (218.13–347.37) | 206.46 (151.52–289.02) | −24.18 (−37.59 to −11.91) | −1.95 (−2.14 to −1.76) |
| Australasia | 137.34 (112.21–170.14) | 49.68 (40.50–62.37) | −63.83 (−69.43 to −57.52) | −2.44 (−2.72 to −2.16) |
| Western Europe | 213.08 (155.79–299.23) | 186.70 (139.28–255.69) | −12.38 (−18.24 to −5.92) | −0.91 (−1.17 to −0.66) |
| Southern Latin America | 1689.92 (1545.58–1834.86) | 226.52 (182.24–284.02) | −86.60 (−89.22 to −83.26) | −47.27 (−50.37 to −44.17) |
| High-income North America | 158.08 (132.02–196.26) | 56.86 (49.47–64.72) | −64.03 (−71.06 to −56.84) | −2.60 (−2.93 to −2.27) |
| Caribbean | 27,250.03 (22,428.55–32,314.72) | 9223.41 (6206.31–12,811.86) | −66.15 (−77.81 to −53.38) | −617.10 (−708.91 to −525.29) |
| Andean Latin America | 13,878.76 (11,671.16–16,409.75) | 864.33 (585.62–1205.73) | −93.77 (−95.75 to −91.49) | −481.71 (−515.64 to −447.77) |
| Central Latin America | 15,646.98 (14,444.86–17,085.79) | 1341.72 (988.75–1779.40) | −91.43 (−93.80 to −88.54) | −447.65 (−459.90 to −435.40) |
| Tropical Latin America | 16,850.51 (14,389.96–19,365.06) | 445.65 (359.78–547.28) | −97.36 (−97.96 to −96.61) | −534.89 (−542.59 to −527.19) |
| North Africa and middle East | 16,145.92 (12,173.72–20,601.85) | 1765.15 (1280.13–2658.66) | −89.07 (−91.82 to −85.63) | −458.07 (−464.41 to −451.73) |
| South Asia | 35,198.65 (28,119.06–42,176.67) | 3267.38 (2066.25–4691.40) | −90.72 (−94.25 to −86.59) | −1059.87 (−1073.45 to −1046.28) |
| Central Sub-Saharan Africa | 52,503.20 (36,619.49–66,048.00) | 5792.12 (3593.83–8926.64) | −88.97 (−92.65 to −82.04) | −1484.40 (−1527.11 to −1441.69) |
| Eastern Sub-Saharan Africa | 50,923.68 (32,335.09–69,517.88) | 9397.03 (6544.95–13,553.68) | −81.55 (−88.49 to −69.79) | −1360.55 (−1387.67 to −1333.43) |
| Southern Sub-Saharan Africa | 28,744.38 (24,826.34–33,039.04) | 9097.62 (6720.75–12,075.27) | −68.35 (−75.43 to −59.79) | −676.66 (−719.40 to −633.92) |
| Western Sub-Saharan Africa | 72,528.16 (50,849.28–89,903.72) | 17,660.54 (11,989.31–25,664.69) | −75.65 (−82.50 to −65.57) | −1821.49 (−1857.50 to −1785.47) |
| High-middle SDI region | 3363.08 (2698.52–3993.35) | 263.00 (209.92–317.77) | −92.18 (−93.64 to −90.41) | −99.71 (−101.50 to −97.91) |
| High SDI region | 411.72 (327.99–521.11) | 141.50 (114.58–177.12) | −65.63 (−73.97 to −57.68) | −8.53 (−8.73 to −8.32) |
| Low-middle SDI region | 38,408.45 (31,009.23–44,777.94) | 4094.07 (3122.24–5451.19) | −89.34 (−92.05 to −85.39) | −1117.08 (−1124.50 to −1109.66) |
| Low SDI region | 56,518.92 (41,443.09–70,762.92) | 12,309.84 (8752.12–17,028.51) | −78.22 (−84.56 to −68.10) | −1460.37 (−1482.60 to −1438.14) |
| Middle SDI region | 13,147.99 (10,248.57–15,528.01) | 1368.86 (1065.51–1754.18) | −89.59 (−91.57 to −87.38) | −378.62 (−384.03 to −373.20) |
Abbreviations: DALY, disability-adjusted life year; GBD, Global Burden of Disease; AAPC, average annual percent change; CI, confidence interval; UI, uncertainty interval; SDI, socio-demographic index.
3.2. SDI regions
In 2021, the incidence rate of diarrhea among children under five years was highest in the low SDI region, at 79,236.37 per 100,000 population (95% UI: 66,678.62–92,048.61 per 100,000 population). From 1990 to 2021, the incidence rate showed a significant decline across all five SDI regions, with the smallest reduction observed in the high SDI region (AAPC = −699.24, 95% CI: −791.83 to −606.64) and the largest in the low SDI region (AAPC = −6591.68, 95% CI: −6706.93 to −6476.43) (Table 1, Fig. S1).
Similarly, the prevalence rate of diarrhea in 2021 was highest in the low SDI region, at 1157.71 per 100,000 population (95% UI: 1014.17–1325.92 per 100,000 population). Between 1990 and 2021, the prevalence rate significantly decreased across all SDI regions, with the smallest reduction in the high SDI region (AAPC = −10.91, 95% CI: −12.41 to −9.42) and the largest in the low SDI region (AAPC = −115.73, 95% CI: −116.98 to −114.48) (Table 2, Fig. S1).
The mortality rate of diarrhea among children under five in 2021 was also highest in the low SDI region, at 137.15 per 100,000 population (95% UI: 96.81–190.65 per 100,000 population). From 1990 to 2021, the mortality rate declined in all SDI regions, with the smallest reduction in the high SDI region (AAPC = −0.08, 95% CI: −0.09 to −0.08) and the largest in the low SDI region (AAPC = −16.30, 95% CI: −16.57 to −16.03) (Table 3, Fig. S1).
The DALY rate for diarrhea in children under five in 2021 was highest in the low SDI region, at 12,309.84 per 100,000 population (95% UI: 8752.12–17,028.51 per 100,000 population). Between 1990 and 2021, the DALY rate declined across all SDI regions, with the smallest decrease observed in the high SDI region (AAPC = −8.53, 95% CI: −8.73 to −8.32) and the largest in the low SDI region (AAPC = −1460.37, 95% CI: −1482.60 to −1438.14) (Table 4, Fig. S1).
3.3. Geographical regions
In 2021, the incidence rate of diarrhea among children under five years was highest in Oceania (128,542.07 per 100,000 population, 95% UI: 107,231.53–150,654.43 per 100,000 population) and lowest in high-income North America (3133.27 per 100,000 population, 95% UI: 2437.97–3988.19 per 100,000 population). Between 1990 and 2021, the incidence rate of diarrheal diseases decreased in 20 out of the 21 regions, with the exception of high-income Asia Pacific, where it increased (AAPC = 561.60, 95% CI: 498.80–624.41). The largest decrease was observed in Andean Latin America (AAPC = −8789.01, 95% CI: −8902.36 to −8675.65) (Table 1).
In 2021, the prevalence rate of diarrhea for children under five years was also highest in Oceania (1942.08 per 100,000 population, 95% UI: 1684.67 to 2228.69 per 100,000 population) and lowest in high-income North America (1263.44 per 100,000 population, 95% UI: 952.92–1640.22 per 100,000 population). From 1990 to 2021, the prevalence rate of diarrhea in children under five years declined in all regions except high-income Asia Pacific, where it increased (AAPC = 7.57, 95 % CI: 6.53–8.61). The largest reduction occurred in Andean Latin America (AAPC = −161.67, 95% CI: −162.87 to −160.48) (Table 2).
In 2021, the mortality rate due to diarrhea in children under five years was highest in Western Sub-Saharan Africa (197.35 per 100,000 population, 95% UI: 132.88–287.80 per 100,000 population) and lowest in Australasia (0.33 per 100,000 population, 95% UI: 0.27–0.41 per 100,000 population). Between 1990 and 2021, the mortality rate decreased in all 21 regions, with the greatest decline seen in Western Sub-Saharan Africa (AAPC = −20.36, 95% CI: −20.76 to −19.96) (Table 3).
The DALY rate for diarrhea in children under five years in 2021 was highest in Western Sub-Saharan Africa (17,660.54 per 100,000 population, 95% UI: 11,989.31–25,664.69 per 100,000 population) and lowest in Australasia (49.68 per 100,000 population, 95% UI: 40.50–62.37 per 100,000 population). From 1990 to 2021, the DALY rate declined in all regions, with Western Sub-Saharan Africa showing the largest decrease (AAPC = −1821.49, 95% CI: −1857.50 to −1785.47) (Table 4).
3.4. Countries and territories
In 2021, the highest incidence rate of diarrhea in children under five years was observed in the Netherlands, at 166,208.95 per 100,000 population (95% UI: 111,931.07–220,944.04 per 100,000 population). The highest number of cases occurred in Cambodia at 1.23 million cases (95% UI: 1.04–1.42 million). Among 204 countries and territories, the incidence rate of diarrhea increased in 11 countries, remained relatively stable in two, and decreased in 191. The largest increase was seen in Taiwan, China (AAPC = 2124.30, 95% CI: 2026.29–2222.31), while Paraguay experienced the largest decrease (AAPC = −10,077.81, 95% CI: −10,215.92 to −9939.70) (Table S5, Fig. S1).
In 2021, the highest prevalence rate of diarrhea was also reported in the Netherlands, at 2622.19 per 100,000 population (95% UI: 1800.27–3559.28 per 100,000 population). India had the highest number of prevalent cases: 1.15 million cases (95% UI: 1.00–1.37 million). Across the 204 countries and territories, the prevalence rate increased in nine countries, remained stable in six, and decreased in 189. The largest increase in prevalence rate was in the Netherlands (AAPC = 28.15, 95% CI: 21.96–34.33), while Paraguay had the greatest decline (AAPC = −187.35, 95% CI: −189.36 to −185.35) (Table S6, Fig. S2).
In terms of mortality rate in 2021, Chad had the highest diarrhea-related mortality rate, at 560.45 per 100,000 population (95% UI: 373.77–952.59 per 100,000 population), while Nigeria had the highest number of deaths: 97.68 thousand (95% UI: 63.51–141.99 thousand). Mortality rates increased in 11 countries, remained stable in 13, and declined in 180 countries. The largest increase in mortality was observed in Tokelau (AAPC = 1.82, 95% CI: 1.42–2.22), while Niger showed the greatest decline (AAPC = −40.09, 95% CI: −41.01 to −39.18) (Table S7, Fig. S2).
Chad had the highest DALY rate for diarrhea in 2021: 49,921.52 per 100,000 population (95% UI: 33,399.80–84,699.30 per 100,000 population). Nigeria had the highest number of DALYs: 8.74 million (95% UI: 5.71–12.65 million). Among the 204 countries and territories, DALY rates increased in 7 countries, remained stable in 11, and decreased in 186. The largest increase in DALY rates was recorded in Tokelau (AAPC = 159.74, 95% CI: 123.56–195.91), while Niger saw the largest decrease (AAPC = −3552.02, 95% CI: −3635.36 to −3468.68) (Table S8, Fig. S2).
3.5. Global trends by age-gender
In 2021, there were no significant differences in the incidence, prevalence, mortality, or DALY rates of diarrheal disease between males and females across age groups <1 year, 1–2 years, 2–4 years, and <5 years. In addition, the number of male and female children affected by diarrhea showed no significant differences across these age groups (Fig. S3A–D).
3.6. The association between rate and SDI
In 2021, there was a negative correlation between the SDI and the rates of diarrheal disease in children under five years across 204 countries and territories. Specifically, incidence rate (r = −0.204, P < 0.001), prevalence rate (r = −0.193, P < 0.001), mortality rate (r = −0.879, P < 0.001), and DALY rate (r = −0.855, P < 0.001) were all negatively correlated with SDI (Fig. S4A–D).
From 1990 to 2021, a similar negative correlation was observed globally between SDI and diarrheal disease rates in children under five. Incidence (r = −0.782, P < 0.001), prevalence (r = −0.777, P < 0.001), mortality (r = −0.908, P < 0.001), and DALY rates (r = −0.904, P < 0.001) were all negatively associated with SDI over this period (Fig. S5A–D).
3.7. Risk factors
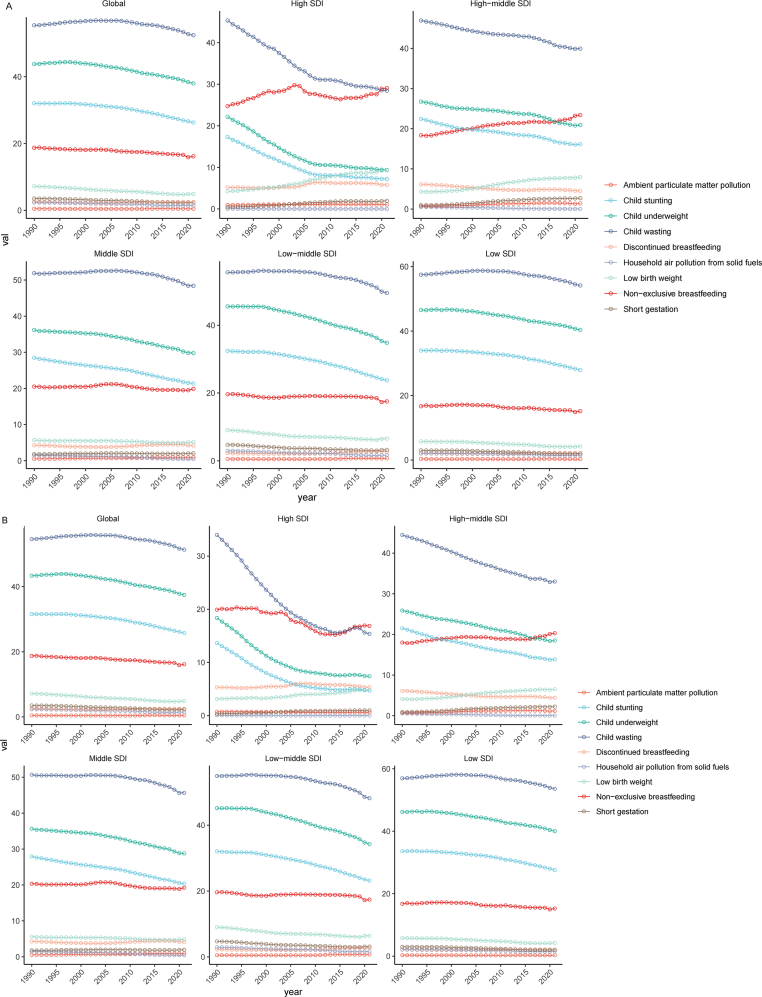
At the global level, from 1990 to 2021, child wasting consistently remained the leading cause of diarrhea-related deaths among children under five, followed by child underweight, child stunting and non-exclusive breastfeeding. The contribution of these four factors to diarrhea-related mortality has been gradually declining. Similar trends were observed in middle SDI, low-middle SDI, and low SDI regions. In contrast, in high SDI regions, non-exclusive breastfeeding emerged as the second leading cause of diarrhea-related deaths in children under five years, with its contribution steadily increasing from 1990 to 2021. In high-middle SDI regions, deaths attributed to non-exclusive breastfeeding have risen consistently and, since 2015, it has become the second most significant cause of diarrhea-related mortality in children under five years (Fig. 1A).
Fig. 1.
The changing trend of risk factors leading to mortality rate and DALY rate of children under five years old with diarrheal disease from 1990 to 2021. A: mortality rate. B: DALY rate. Abbreviations: DALYs, disability-adjusted life years; SDI, socio-demographic index.
At the global level, from 1990 to 2021, the primary risk factors contributing to diarrhea-related DALY rates among children under five years were child wasting, child underweight, child stunting and non-exclusive breastfeeding, with the contribution of these factors gradually decreasing over time. Notably, non-exclusive breastfeeding became the leading risk factor after 2020 in high SDI regions, it has ranked second since 2018 and continues to show a slow upward trend in high-middle SDI regions. In additions, the ranking and trends of major risk factors align with global patterns in middle SDI, low-middle SDI, and low SDI regions (Fig. 1B).
3.8. Projecting
The study, using the BACP model, projects a significant decline in the incidence rate, prevalence rate, and mortality rate of diarrhea among children under five years from 2022 to 2035. Globally, the incidence rate in 2035 is expected to be 15,974.66 per 100,000 population (95% CI: 6801.97–25,147.36 per 100,000 population). The EAPC for the incidence rate over this period is −8.97% (95% CI: −9.02% to −8.92%). The prevalence rate in 2035 is projected to be 220.74 per 100,000 population (95% CI: 83.30–358.19 per 100,000 population), with an EAPC of −9.41% (95% CI: −9.46% to −9.36%). The mortality rate for 2035 is expected to be relatively low, at 17.77 per 100,000 population (95% CI: 0.00–118.29 per 100,000 population), and the EAPC for mortality is projected at −7.32% (95% CI: −7.37% to −7.26%) (Fig. 2, Table 5).
Fig. 2.
The prediction of global burden of diarrheal diseases among children under five years for 2022–2035 based on the Bayesian age-period-cohort model. A: incidence rate. B: prevalence rate. C: mortality rate.
Table 5.
The prediction of global burden of diarrheal disease among children under five years for 2022–2035 based on the BAPC model.
| Disease | Index | Incidence | Prevalence | Death |
|---|---|---|---|---|
| Diarrheal disease (<5 years) | Rate per 100,000 population (95% CI) in 2035 | 15,974.66 (6801.97–25,147.36) | 220.74 (83.3–358.19) | 17.77 (0.00–118.29) |
| EAPC (95% CI) in 2022–2035/% | −8.97 (−9.02 to −8.92) | −9.41 (−9.46 to −9.36) | −7.32 (−7.37 to −7.26) |
Abbreviations: BAPC, Bayesian age-period-cohort; CI, confidence interval; EAPC, estimated annual percentage change.
3.9. Global trends in pathogens
In 2021, rotavirus was the leading pathogen responsible for diarrhea-related deaths rate among children under five years globally, across all age groups, followed by Shigella and adenovirus (Fig. 3A). From 1990 to 2021, among 13 common diarrhea-related pathogens, mortality rate due to all but C. difficile decreased in children under five across all age groups (Table 6, Fig. 3A). In addition, in 2021, rotavirus accounted for the highest number of deaths in children under five years across all age groups. While the number of mortality cases due to C. difficile increased in children aged <5 years, 1–2 years, and 2–4 years from 1990 to 2021, it showed a declining trend in infants under 1 year. Apart from C. difficile, the number of mortality cases caused by the other 12 pathogens continued to decline over this period (Table S9, Fig. 3B).
Fig. 3.
The diarrhea-related mortality and DALY in children under five years of age attributed to specific pathogens globally in 2021 year. A: mortality rate. B: mortality number. C: DALY rate. D: DALY number. Abbreviations: DALY, disability-adjusted life year.
Table 6.
The changing trend of mortality rate of children under five years old attributed to specific diarrheal pathogens across the globe from 1990 to 2021.
| Age group | Pathogen | Mortality rate per 100,000 population (95% UI) in 1990 | Mortality rate per 100,000population (95% UI) in 2021 | AAPC of mortality rate (95% CI) in 1990–2021/% |
|---|---|---|---|---|
| <5 years | Vibrio cholerae | 17.76 (14.75–21.43) | 3.92 (2.81–5.31) | −0.47 (−0.49 to −0.45) |
| Non-typhoidal Salmonella | 8.16 (1.20–17.77) | 1.8 (0.24–4.17) | −0.21 (−0.21 to −0.20) | |
| Shigella | 48.35 (29.24–78.08) | 12.42 (7.28–20.96) | −1.19 (−1.20 to −1.18) | |
| Enteropathogenic Escherichia coli | 26.83 (15.46–42.14) | 7.04 (3.95–11.59) | −0.32 (−0.32 to −0.31) | |
| Enterotoxigenic Escherichia coli | 29.72 (17.32–47.09) | 6.96 (3.83–11.72) | −0.67 (−0.68 to −0.66) | |
| Campylobacter | 22.98 (10.17–42.4) | 3.84 (1.56–7.41) | −0.64 (−0.65 to −0.63) | |
| Entamoeba | 12.28 (5.88–23.03) | 2.44 (1.07–4.91) | −0.32 (−0.32 to −0.31) | |
| Cryptosporidium | 38.32 (23.65–59.95) | 10.4 (5.91–16.65) | −0.90 (−0.93 to −0.87) | |
| Rotavirus | 100.31 (74.21–127.24) | 18.21 (12.63–25.74) | −2.62 (−2.66 to −2.58) | |
| Aeromonas | 8.31 (3.62–15.15) | 1.63 (0.73–3.07) | −0.22 (−0.22 to −0.22) | |
| Clostridium difficile | 0.02 (0.01–0.03) | 0.02 (0.01–0.03) | −0.00 (−0.00 – 0.00) | |
| Norovirus | 22.35 (7.64–40.06) | 4.49 (1.47–8.36) | −0.58 (−0.58 to −0.57) | |
| Adenovirus | 56.78 (32.7–90.28) | 12.32 (6.82–20.21) | −1.47 (−1.49 to −1.44) | |
| <1 years | Vibrio cholerae | 43.56 (34.48–53.92) | 9.9 (6.66–13.81) | −1.17 (−1.22 to −1.12) |
| Non-typhoidal Salmonella | 23.1 (3.87–51.69) | 5.27 (0.87–12.21) | −0.58 (−0.59 to −0.57) | |
| Shigella | 134.35 (75.91–227.36) | 36.67 (19.98–64.09) | −3.29 (−3.35 to −3.22) | |
| Enteropathogenic Escherichia coli | 90.1 (47.49–152.77) | 25.17 (12.41–44.49) | −2.23 (−2.28 to −2.17) | |
| Enterotoxigenic Escherichia coli | 89.15 (49.43–150.83) | 21.45 (11.09–36.92) | −2.22 (−2.25 to −2.20) | |
| Campylobacter | 80.75 (33.33–153.56) | 14.36 (5.6–28.61) | −2.21 (−2.25 to −2.17) | |
| Entamoeba | 35.36 (15.94–69.56) | 7.57 (3.12–15.31) | −0.91 (−0.92 to −0.90) | |
| Cryptosporidium | 113.18 (67.77–180.94) | 33.37 (18.9–54.53) | −2.63 (−2.69 to −2.57) | |
| Rotavirus | 309.15 (230.49–390.99) | 61.26 (42.73–85.95) | −8.05 (−8.13 to −7.97) | |
| Aeromonas | 17.05 (4.23–40.96) | 3.54 (0.89–8.95) | −0.45 (−0.45 to −0.44) | |
| Clostridium difficile | 0.02 (0.01–0.04) | 0.02 (0.01–0.04) | −0.00 (−0.00 to −0.00) | |
| Norovirus | 42.75 (14.17–89.68) | 9.2 (3.02–19.17) | −1.11 (−1.12 to −1.10) | |
| Adenovirus | 182.36 (104.36–288.12) | 43.1 (24.47–71.98) | −4.71 (−4.79 to −4.63) | |
| 1–2 years | Vibrio cholerae | 22.05 (18.04–27.06) | 4.93 (3.41–6.95) | −0.58 (−0.60 to −0.56) |
| Non-typhoidal Salmonella | 9.21 (0.00–26.42) | 2.14 (0.00–6.5) | −0.23 (−0.23 to −0.23) | |
| Shigella | 53.2 (27.47–88.29) | 14.32 (7.17–24.46) | −1.28 (−1.29 to −1.26) | |
| Enteropathogenic Escherichia coli | 24.28 (8.61–46.29) | 6.65 (2.51–12.62) | −0.59 (−0.61 to −0.58) | |
| Enterotoxigenic Escherichia coli | 30.13 (14.72–54.09) | 7.64 (3.64–15.01) | −0.74 (−0.75 to −0.72) | |
| Campylobacter | 16.31 (2.68–41.62) | 2.96 (0.48–7.19) | −0.44 (−0.45 to −0.44) | |
| Entamoeba | 12.75 (5.45–25.13) | 2.62 (1.09–5.4) | −0.32 (−0.33 to −0.32) | |
| Cryptosporidium | 39.91 (18.32–73.82) | 10.81 (4.95–20.12) | −0.94 (−0.97 to −0.92) | |
| Rotavirus | 97.6 (67.12–134.72) | 18.33 (11.56–27.33) | −2.56 (−2.60 to −2.52) | |
| Aeromonas | 12.76 (4.86–25.52) | 2.62 (0.96–5.38) | −0.33 (−0.33 to −0.33) | |
| Clostridium difficile | 0.02 (0.01–0.03) | 0.02 (0.01–0.04) | 0.00 (−0.00 – 0.00) | |
| Norovirus | 35.41 (5.09–66.56) | 7.47 (1.09–14.23) | −0.91 (−0.91 to −0.90) | |
| Adenovirus | 51.01 (24.04–96.47) | 11.59 (5.39–20.71) | −1.29 (−1.33 to −1.26) | |
| 2–4 years | Vibrio cholerae | 7.34 (5.59–9.34) | 1.71 (1.11–2.45) | −0.18 (−0.19 to −0.18) |
| Non-typhoidal Salmonella | 2.61 (0.00–7.64) | 0.6 (0.00–1.87) | −0.06 (−0.06 to −0.06) | |
| Shigella | 16.82 (7.91–28.91) | 4.2 (2.00–7.96) | −0.41 (−0.41 to −0.40) | |
| Enteropathogenic E coli | 5.7 (1.85–11.34) | 1.47 (0.49–2.98) | −0.14 (−0.14 to −0.14) | |
| Enterotoxigenic E coli | 8.93 (4.34–15.47) | 2.18 (1.00–4.13) | −0.22 (−0.22 to −0.22) | |
| Campylobacter | 5.16 (0.85–13.21) | 0.82 (0.13–2.05) | −0.14 (−0.14 to −0.14) | |
| Entamoeba | 4.11 (1.87–8.12) | 0.78 (0.33–1.61) | −0.11 (−0.11 to −0.11) | |
| Cryptosporidium | 11.76 (5.81–20.97) | 3.05 (1.38–5.61) | −0.28 (−0.28 to −0.27) | |
| Rotavirus | 28.64 (18.74–39.96) | 4.64 (2.74–7.36) | −0.78 (−0.79 to −0.76) | |
| Aeromonas | 3.76 (1.52–7.14) | 0.71 (0.28–1.38) | −0.10 (−0.10 to −0.10) | |
| Clostridium difficile | 0.01 (0.01–0.02) | 0.01 (0.01–0.02) | 0.00 (0.00–0.00) | |
| Norovirus | 10.83 (1.59–20.77) | 2.06 (0.28–4.12) | −0.28 (−0.28 to −0.28) | |
| Adenovirus | 15.09 (7.91–28.6) | 2.88 (1.34–5.68) | −0.39 (−0.40 to −0.38) |
Abbreviations: AAPC, average annual percent change; CI, confidence interval; UI, uncertainty interval.
In 2021, rotavirus was the leading pathogen responsible for diarrhea-related DALY rate among children under five years globally, and across all age groups, followed by Shigella and adenovirus (Fig. 3C). From 1990 to 2021, among 13 common diarrhea-related pathogens, DALY rate due to all but C. difficile decreased in children under five years across all age groups (Table 7, Fig. 3C).
Table 7.
The changing trend of DALY rate of children under five years old attributed to specific diarrheal pathogens across the globe from 1990 to 2021.
| Age group | Pathogen | DALY rate per 100,000 population (95% UI) in 1990 | DALY rate per 100,000 population (95% UI) in 2021 | AAPC of DALY rate (95% CI) in 1990–2021/% |
|---|---|---|---|---|
| <5 years | Vibrio cholerae | 1575.87 (1308.45–1902.79) | 346.9 (248.99–470.04) | −41.66 (−43.11 to −40.21) |
| Non-typhoidal Salmonella | 731 (113.22–1582.89) | 161.27 (23.62–371.93) | −18.55 (−18.81 to −18.29) | |
| Shigella | 4335.87 (2629.83–6993.84) | 1115.88 (656.16–1879.92) | −106.47 (−107.57 to −105.38) | |
| Enteropathogenic E coli | 2408.14 (1394.59–3779.64) | 633.5 (355.65–1039.61) | −60.15 (−61.62 to −58.68) | |
| Enterotoxigenic E coli | 2672.46 (1562.18–4230.62) | 627.43 (346.64–1054.51) | −67.02 (−68.26 to −65.78) | |
| Campylobacter | 2079.31 (919.26–3814.44) | 351.75 (148.74–670.26) | −57.52 (−58.43 to −56.62) | |
| Entamoeba | 1098.71 (532.34–2054.85) | 218.96 (96.64–438.05) | −28.38 (−28.62 to −28.14) | |
| Cryptosporidium | 3424.61 (2116.35–5352.33) | 930.43 (531.16–1485.32) | −80.78 (−82.88 to −78.69) | |
| Rotavirus | 9007.42 (6678.68–11,403.73) | 1639.23 (1142.33–2309.77) | −244.22 (−247.75 to −240.70) | |
| Aeromonas | 741.45 (323.64–1356.03) | 145.98 (65.69–274.51) | −19.37 (−19.53 to −19.22) | |
| Clostridium difficile | 1.36 (0.78–2.24) | 1.33 (0.71–2.31) | −0.00 (−0.00 – 0.00) | |
| Norovirus | 2014.44 (708.88–3584.62) | 407.8 (139.96–750.81) | −52.13 (−52.53 to −51.73) | |
| Adenovirus | 5096.4 (2936.66–8125.49) | 1111.51 (614.84–1818.75) | −131.36 (−133.93 to −128.79) | |
| <1 years | Vibrio cholerae | 3904.1 (3090.53–4832.81) | 887 (597.18–1237.54) | −105.10 (−109.47 to −100.72) |
| Non-typhoidal Salmonella | 2083.02 (354.11–4655.53) | 476.31 (81.05–1099.29) | −52.43 (−53.08 to −51.77) | |
| Shigella | 12,097.51 (6852–20,472.58) | 3308.52 (1813.52–5770.21) | −296.09 (−302.08 to −290.10) | |
| Enteropathogenic E coli | 8118.21 (4289.57–13,763.74) | 2274.13 (1125.26–4014.16) | −200.31 (−205.28 to −195.34) | |
| Enterotoxigenic E coli | 8036.45 (4454.42–13,589.24) | 1941.88 (1004.18–3342.16) | −200.24 (−202.77 to −197.72) | |
| Campylobacter | 7310.49 (3044.88–13,859.00) | 1313.38 (519.37–2598.01) | −199.77 (−203.14 to −196.40) | |
| Entamoeba | 3181.15 (1436.82–6249.22) | 681.67 (285.4–1379) | −81.74 (−82.46 to −81.02) | |
| Cryptosporidium | 10,181.56 (6102.04–16,277.96) | 3005.9 (1704.14–4908.93) | −236.31 (−241.52 to −231.10) | |
| Rotavirus | 27,834.31 (20,775.62–35,185.09) | 5525.18 (3856.62–7740.15) | −745.66 (−756.89 to −734.43) | |
| Aeromonas | 1539.31 (387.65–3685.93) | 321.27 (81.76–806.22) | −40.29 (−40.70 to −39.87) | |
| Clostridium difficile | 1.87 (0.98–3.27) | 1.66 (0.77–3.16) | −0.01 (−0.01 to −0.00) | |
| Norovirus | 3899.48 (1328.05–8110.4) | 848.46 (295.15–1748.08) | −100.61 (−101.60 to −99.61) | |
| Adenovirus | 16,426.59 (9406.54–25,933.84) | 3899.63 (2217.01–6494.46) | −419.46 (−430.10 to −408.82) | |
| 1–2 years | Vibrio cholerae | 1954.06 (1599.16–2398.53) | 437.05 (302.2–615.47) | −51.20 (−53.09 to −49.31) |
| Non-typhoidal Salmonella | 821.49 (2.27–2346.49) | 191.04 (0.52–577.72) | −20.37 (−20.68 to −20.07) | |
| Shigella | 4759.44 (2454.2–7910.36) | 1281.3 (642.51–2187.36) | −114.27 (−115.49 to −113.06) | |
| Enteropathogenic E coli | 2168.71 (777.14–4135.2) | 594.2 (225.27–1123.12) | −52.98 (−54.03 to −51.94) | |
| Enterotoxigenic E coli | 2704.44 (1325.95–4863.62) | 686.68 (327.6–1338.74) | −66.60 (−67.83 to −65.37) | |
| Campylobacter | 1470.75 (263.61–3716.06) | 268.21 (49.01–642.88) | −39.82 (−40.51 to −39.13) | |
| Entamoeba | 1136.25 (490.3–2237.42) | 233.62 (98.18–479.35) | −28.97 (−29.26 to −28.67) | |
| Cryptosporidium | 3552.89 (1633.35–6563.07) | 962.53 (439.94–1791.8) | −83.46 (−85.82 to −81.10) | |
| Rotavirus | 8742.92 (6019.98–12,049.5) | 1642.9 (1038.59–2441.12) | −229.16 (−232.89 to −225.44) | |
| Aeromonas | 1136.27 (439.8–2274.34) | 233.68 (85.83–478.19) | −29.30 (−29.57 to −29.04) | |
| Clostridium difficile | 1.75 (1.01–2.88) | 1.75 (0.86–3.12) | −0.00 (−0.00 – 0.00) | |
| Norovirus | 3173.34 (490.82–5937.67) | 670.36 (105.43–1277.7) | −81.11 (−81.82 to −80.41) | |
| Adenovirus | 4562.01 (2159.96–8573.63) | 1039.57 (483.04–1852.35) | −116.00 (−118.42 to −113.57) | |
| 2–4 years | Vibrio cholerae | 638.48 (486.3–812.44) | 148.41 (96.52–212.25) | −15.98 (−16.41 to −15.55) |
| Non-typhoidal Salmonella | 230.44 (1.45–667.06) | 52.77 (0.4–163.88) | −5.88 (−6.00 to −5.76) | |
| Shigella | 1494.76 (701.1–2580.79) | 373.97 (177.81–709.31) | −36.19 (−36.63 to −35.75) | |
| Enteropathogenic E coli | 504.81 (164.11–996.79) | 130.32 (44.25–261.93) | −12.31 (−12.46 to −12.16) | |
| Enterotoxigenic E coli | 797.4 (390.65–1371.39) | 195.38 (91.98–368.78) | −19.44 (−19.60 to −19.27) | |
| Campylobacter | 467.57 (88.59–1171.02) | 76.1 (15.97–182.84) | −12.67 (−12.81 to −12.53) | |
| Entamoeba | 362.24 (165.81–709.37) | 68.85 (29.75–141.16) | −9.41 (−9.51 to −9.31) | |
| Cryptosporidium | 1032.78 (511.49–1840.26) | 267.83 (122.04–490.1) | −24.37 (−25.16 to −23.59) | |
| Rotavirus | 2553.92 (1685.08–3549.22) | 416.6 (250.34–652.14) | −69.01 (−70.24 to −67.79) | |
| Aeromonas | 330.3 (134.04–623.28) | 62.95 (25.58–121.15) | −8.60 (−8.70 to −8.51) | |
| Clostridium difficile | 1.05 (0.54–1.87) | 1.1 (0.56–1.94) | 0.00 (0.00–0.00) | |
| Norovirus | 966.41 (163.36–1832.82) | 185.64 (30.89–361.7) | −24.98 (−25.29 to −24.68) | |
| Adenovirus | 1339.84 (703.97–2532.56) | 258.05 (122.32–503.3) | −34.58 (−35.26 to −33.91) |
Abbreviations: DALY, disability-adjusted life year; AAPC, average annual percent change; CI, confidence interval; UI, uncertainty interval.
In addition, in 2021, rotavirus accounted for the highest DALY numbers in children under five years across all age groups. During the period from 1990 to 2021, DALY numbers caused by C. difficile increased in children under five years and in the 2–4 years age group, while a declining trend was observed in infants under 1 year and in children aged 1–2 years. Apart from C. difficile, DALY numbers associated with the other 12 pathogens continued to decrease during this period (Table S10, Fig. 3D).
4. Discussion
The study reveals that, despite a decline in the burden of diarrheal disease among children under five over the past few decades, diarrhea remains a serious health threat, especially in low- and low-middle income regions. Low birth weight and poor child development remain the leading causes of diarrhea-related deaths, with rotavirus still being the primary pathogen. These findings are of significant importance for international organizations, governments, researchers, and healthcare professionals in the effective prevention and control of diarrhea, ultimately reducing the global burden of diarrheal disease.
It highlighted the significant role of various pathogens in the burden of diarrheal disease, particularly the dominance of viral pathogens such as rotavirus in childhood diarrhea. Bacterial pathogens, including Shigella and E. coli, as well as parasitic infections, have also substantially contributed to the diarrhea burden in specific regions [34,35]. While the mortality and DALYs associated with viral and bacterial diarrhea have been declining, special attention must be given to the rising incidence of C. difficile infections [36]. A key risk factor for C. difficile infections is the widespread use of antibiotics, particularly broad-spectrum antibiotics, which disrupt the balance of gut microbiota and allow C. difficile to proliferate, causing severe intestinal infections [37]. The misuse of antibiotics has increased the risk of C. difficile infections, leading to rising incidence and mortality rates. Additionally, in some developing countries and resource-limited settings, C. difficile infections are often underestimated or misdiagnosed, resulting in delayed treatment and high mortality rates. In many cases, the diagnosis and treatment of diarrheal disease in children focus primarily on other pathogens such as rotavirus, Shigella and E. coli, overlooking the possibility of C. difficile infection [38]. Moreover, many healthcare facilities, particularly in resource-limited regions, lack effective infection control measures, including proper hand hygiene, environmental sanitation, and isolation practices, which increases the risk of C. difficile transmission in hospitals, making children more vulnerable to infection [39]. Furthermore, C. difficile has a high recurrence rate, and recurrent infections are more challenging to treat, contributing to increased mortality rates [40].
The study identified rotavirus and Shigella as the leading pathogens responsible for diarrhea-related deaths. Reducing diarrhea-related mortality requires a multi-tiered approach with comprehensive interventions [[41], [42], [43], [44]]. First, promoting widespread rotavirus vaccination remains the most effective strategy for preventing rotavirus-induced diarrhea [45], and the development of a Shigella vaccine holds promise for further reducing mortality rates [46]. Second, improving access to clean drinking water, enhancing basic sanitation infrastructure, and promoting health education can significantly curb the transmission of pathogens [47]. In addition, nutritional support, such as breastfeeding and zinc supplementation, can boost children's immune systems, reducing both the incidence and severity of diarrhea [48]. In terms of treatment, the use of oral rehydration salts and targeted antibiotics is key to lowering diarrhea-related mortality [49]. In conclusion, global cooperation and financial support are essential for promoting vaccination, improving sanitation, and strengthening community health education [50]. Such preventive measures can significantly reduce the global burden of diarrheal diseases among children under five years of age.
The study has several limitations. Firstly, the analysis relies on data from the GBD study 2021, which may vary in quality and coverage, particularly in developing and low-income countries where data may be incomplete or inaccurate, potentially affecting the reliability of the findings [18,19,51]. Secondly, the GBD study 2021 database is based on model estimations rather than real-world data, which may lead to overestimation or underestimation of the disease burden [18,19,51]. Thirdly, the study focuses primarily on children under five, excluding adolescents, adults, and the elderly. Forth, the predictive models used in this study, such as the BAPC model, while sophisticated, depend on the quality of available data and historical trends [15,16]. Given that the occurrence and transmission of childhood diarrhea are influenced by numerous factors, including climate change and population movement, these models may not fully account for future variations, leading to some uncertainty in the predictions.
5. Conclusion
The study reveals that the global incidence, prevalence, mortality, and DALY rates associated with diarrhea in children under five years have significantly declined from 1990 to 2021. However, children in regions with low SDI, particularly in Sub-Saharan Africa and South Asia, continue to bear a high burden of diarrheal disease. Child wasting and underweight remain key risk factors for diarrhea-related mortality. Rotavirus is the leading pathogen responsible for such deaths. Therefore, expanding rotavirus vaccination, improving sanitation, and ensuring access to clean drinking water are critical interventions to effectively reduce the burden of diarrheal disease in children.
CRediT authorship contribution statement
Chu Chu: Writing – review & editing, Writing – original draft, Visualization, Validation, Software, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Guobing Yang: Writing – review & editing, Writing – original draft, Visualization, Validation, Software, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Jian Yang: Writing – review & editing, Writing – original draft, Visualization, Validation, Software, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Defeng Liang: Writing – review & editing, Writing – original draft, Visualization, Validation, Software, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Ruitao Liu: Visualization, Validation, Software, Methodology, Investigation, Data curation. Guanhua Chen: Visualization, Validation, Software, Methodology, Investigation, Data curation. Jichun Wang: Validation, Supervision, Methodology. Guisheng Zhou: Validation, Supervision, Methodology. Hongli Wang: Validation, Supervision, Methodology.
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors consent for publication.
Data availability statement
The datasets analyzed during the current study are available at http://ghdx.healthdata.org/gbd-results-tool.
Funding sources
The study was supported by the fund of Shanghai Natural Science Foundation (grant number 23ZR1464000), and the Talent Fund of Longhua Hospital affiliated to Shanghai University of Traditional Chinese Medicine (grant number LH001.007), and the Science and Technology Support Project of Taizhou city (SSF20210070).
Declaration of competing interest
The authors declare that they have no competing interests.
Acknowledgements
The authors appreciate the works by the GBD Study 2021 collaborators.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.soh.2024.100086.
Contributor Information
Chu Chu, Email: 47223439@njucm.edu.cn.
Guobing Yang, Email: gostly_1@163.com.
Jian Yang, Email: yangjian@chinacdc.cn.
Defeng Liang, Email: feng6689196@foxmail.com.
Ruitao Liu, Email: 734161711@qq.com.
Guanhua Chen, Email: simonlasker@163.com.
Jichun Wang, Email: wangjc@chinacdc.cn.
Guisheng Zhou, Email: zhouguisheng1@njucm.edu.cn.
Hongli Wang, Email: 2019760935@gzhmu.edu.cn.
Appendix A. Supplementary data
The following is/are the supplementary data to this article:
References
- 1.Kotloff K.L., Nataro J.P., Blackwelder W.C., Nasrin D., Farag T.H., Panchalingam S., et al. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): a prospective, case-control study. Lancet. 2013;382(9888) doi: 10.1016/S0140-6736(13)60844-2. 209–22, [DOI] [PubMed] [Google Scholar]
- 2.Levine M.M., Nasrin D., Acácio S., Bassat Q., Powell H., Tennant S.M., et al. Diarrhoeal disease and subsequent risk of death in infants and children residing in low-income and middle-income countries: analysis of the GEMS case-control study and 12-month GEMS-1A follow-on study. Lancet Glob. Health. 2020;8(2):e204–e214. doi: 10.1016/S2214-109X(19)30541-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Black R.E., Perin J., Yeung D., Rajeev T., Miller J., Elwood S.E., et al. Estimated global and regional causes of deaths from diarrhoea in children younger than 5 years during 2000-21: a systematic review and Bayesian multinomial analysis. Lancet Glob. Health. 2024;12(6):e919–e928. doi: 10.1016/S2214-109X(24)00078-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tickell K.D., Sharmin R., Deichsel E.L., Lamberti L.M., Walson J.L., Faruque A.S.G., et al. The effect of acute malnutrition on enteric pathogens, moderate-to-severe diarrhoea, and associated mortality in the Global Enteric Multicenter Study cohort: a post-hoc analysis. Lancet Glob. Health. 2020;8(2):e215–e224. doi: 10.1016/S2214-109X(19)30498-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gill C.J., Young M., Schroder K., Carvajal-Velez L., McNabb M., Aboubaker S., et al. Bottlenecks, barriers, and solutions: results from multicountry consultations focused on reduction of childhood pneumonia and diarrhoea deaths. Lancet. 2013;381(9876):1487–1498. doi: 10.1016/S0140-6736(13)60314-1. [DOI] [PubMed] [Google Scholar]
- 6.Zhang S.X., Zhou Y.M., Xu W., Tian L.G., Chen J.X., Chen S.H., et al. Impact of co-infections with enteric pathogens on children suffering from acute diarrhea in southwest China. Infect. Dis. Poverty. 2016;5(1):64. doi: 10.1186/s40249-016-0157-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang T., Wang G., Shan C.X., Sun Y.Q., Ren X., Yu L.J., et al. Comparative study on epidemiological and etiological characteristics of patients with acute diarrhea with febrile or non-febrile symptoms in China. Infect. Dis. Poverty. 2023;12(1):62. doi: 10.1186/s40249-023-01108-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khalil I.A., Troeger C., Blacker B.F., Rao P.C., Brown A., Atherly D.E., et al. Morbidity and mortality due to shigella and enterotoxigenic Escherichia coli diarrhoea: the global burden of disease study 1990-2016. Lancet Infect. Dis. 2018;18(11):1229–1240. doi: 10.1016/S1473-3099(18)30475-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zimmermann M., Kotloff K., Nasrin D., Roose A., Levine M.M., Rheingans R., et al. Household costs of diarrhea by etiology in 7 countries, the global enterics mulitcenter study (GEMS) Open Forum Infect. Dis. 2019;6(4):ofz150. doi: 10.1093/ofid/ofz150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kotloff K.L., Nasrin D., Blackwelder W.C., Wu Y., Farag T., Panchalingham S., et al. The incidence, aetiology, and adverse clinical consequences of less severe diarrhoeal episodes among infants and children residing in low-income and middle-income countries: a 12-month case-control study as a follow-on to the Global Enteric Multicenter Study (GEMS) Lancet Glob. Health. 2019;7(5):e568–e584. doi: 10.1016/S2214-109X(19)30076-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Erismann S., Knoblauch A.M., Diagbouga S., Odermatt P., Gerold J., Shrestha A., et al. Prevalence and risk factors of undernutrition among schoolchildren in the Plateau Central and Centre-Ouest regions of Burkina Faso. Infect. Dis. Poverty. 2017;6(1):17. doi: 10.1186/s40249-016-0230-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barrantes K., Achí R. The importance of integrons for development and propagation of resistance in Shigella: the case of Latin America. Braz. J. Microbiol. 2016;47(4):800–806. doi: 10.1016/j.bjm.2016.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang L.P., Zhou S.X., Wang X., Lu Q.B., Shi L.S., Ren X., et al. Etiological, epidemiological, and clinical features of acute diarrhea in China. Nat. Commun. 2021;12(1):2464. doi: 10.1038/s41467-021-22551-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walker C.L.F., Rudan I., Liu L., Nair H., Theodoratou E., Bhutta Z.A., et al. Global burden of childhood pneumonia and diarrhoea. Lancet. 2013;381(9875):1405–1416. doi: 10.1016/S0140-6736(13)60222-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang S.X., Wang J.C., Yang J., Lv S., Duan L., Lu Y., et al. Epidemiological features and temporal trends of the co-infection between HIV and tuberculosis, 1990-2021: findings from the Global Burden of Disease Study 2021. Infect. Dis. Poverty. 2024;13(1):59. doi: 10.1186/s40249-024-01230-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang S.X., Miao F.Y., Yang J., Zhou W.T., Lv S., Wei F.N., et al. Global, regional, and national burden of HIV-negative tuberculosis, 1990-2021: findings from the Global Burden of Disease Study 2021. Infect. Dis. Poverty. 2024;13(1):60. doi: 10.1186/s40249-024-01227-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.GBD 2021 Forecasting Collaborators Burden of disease scenarios for 204 countries and territories, 2022-2050: a forecasting analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403(10440):2204–2256. doi: 10.1016/S0140-6736(24)00685-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.GBD 2021 Diseases and Injuries Collaborators Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403(10440):2133–2161. doi: 10.1016/S0140-6736(24)00757-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.GBD 2021 Risk Factors Collaborators Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403(10440):2162–2203. doi: 10.1016/S0140-6736(24)00933-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu J., Platts-Mills J.A., Juma J., Kabir F., Nkeze J., Okoi C., et al. Use of quantitative molecular diagnostic methods to identify causes of diarrhoea in children: a reanalysis of the GEMS case-control study. Lancet. 2016;388(10051):1291–1301. doi: 10.1016/S0140-6736(16)31529-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang K., Kan C., Han F., Zhang J., Ding C., Guo Z., et al. Global, regional, and national epidemiology of diabetes in children from 1990 to 2019. JAMA Pediatr. 2023;177(8):837–846. doi: 10.1001/jamapediatrics.2023.2029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hu S., Wu X., Jiang H. Trends and projections of the global burden of thyroid cancer from 1990 to 2030. J. Glob. Health. 2024;14 doi: 10.7189/jogh.14.04084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen W., Chen Y., Cheng Z., Chen Y., Lv C., Ma L., et al. Global patterns of syphilis, gonococcal infection, typhoid fever, paratyphoid fever, diphtheria, pertussis, tetanus, and leprosy from 1990 to 2021: findings from the Global Burden of Disease Study 2021. Infect. Dis. Poverty. 2024;13(1):66. doi: 10.1186/s40249-024-01231-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xia W., Liu J., Liu C., Xu S., Wang K., Zhu Z., et al. Burden of neck pain in general population of China, 1990-2019: an analysis for the Global Burden of Disease Study 2019. J. Glob. Health. 2024;14:04066. doi: 10.7189/jogh.14.04066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cho S., Park W.J. Twenty-two-year incidence trend of urological cancers in the Republic of Korea: 1999-2020. Investig. Clin. Urol. 2024;65(1):23–31. doi: 10.4111/icu.20230247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bommersbach T.J., McKean A.J., Olfson M., Rhee T.G. National trends in mental health-related emergency department visits among youth, 2011-2020. JAMA. 2023;329(17):1469–1477. doi: 10.1001/jama.2023.4809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Leong E., Ong S.K., Si-Ramlee K.A., Naing L. Cancer incidence and mortality in Brunei Darussalam, 2011 to 2020. BMC Cancer. 2023;23(1):466. doi: 10.1186/s12885-023-10962-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang D., Hu X., Xu H., Chen Y., Wang S., Lin G., et al. Trend analysis and age-period-cohort effects on morbidity and mortality of liver cancer from 2010 to 2020 in Guangzhou, China. Front. Oncol. 2024;14 doi: 10.3389/fonc.2024.1387587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ye Y., Burkholder G.A., Wiener H.W., Griffin R., Aslibekyan S., Fry K., et al. Comorbidities associated with HPV infection among people living with HIV-1 in the southeastern US: a retrospective clinical cohort study. BMC Infect. Dis. 2020;20(1):144. doi: 10.1186/s12879-020-4822-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li Y.S., Zhang B.B., Zhang X., Fan S., Fei L.P., Yang C., et al. Trend in the incidence of hepatitis A in mainland China from 2004 to 2017: a joinpoint regression analysis. BMC Infect. Dis. 2022;22(1):663. doi: 10.1186/s12879-022-07651-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tuo Y., Li Y., Li Y., Ma J., Yang X., Wu S., et al. Global, regional, and national burden of thalassemia, 1990-2021: a systematic analysis for the global burden of disease study 2021. EClinicalMedicine. 2024;72 doi: 10.1016/j.eclinm.2024.102619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zou Z., Cini K., Dong B., Ma Y., Ma J., Burgner D.P., et al. Time trends in cardiovascular disease mortality across the BRICS: an age-periodperiod-cohort analysis of key nations with emerging economies using the global burden of disease study 2017. Circulation. 2020;141(10):790–799. doi: 10.1161/CIRCULATIONAHA.119.042864. [DOI] [PubMed] [Google Scholar]
- 33.Seide S.E., Röver C., Friede T. Likelihood-based random-effects meta-analysis with few studies: empirical and simulation studies. BMC Med. Res. Methodol. 2019;19(1):16. doi: 10.1186/s12874-018-0618-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Long K.Z., Gunanti I.R., Stride C., Sanchez J., Sur D., Manna B., et al. Identification of enteric pathogen reservoirs and transmission pathways associated with short childhood stature in the Kolkata Indian site of the global enteric multicenter study. Nutrients. 2024;16(16):2733. doi: 10.3390/nu16162733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Buchwald A.G., Verani J.R., Keita A.M., Jahangir Hossain M., Roose A., Sow S.O., et al. Etiology, presentation, and risk factors for diarrheal syndromes in 3 sub-saharan african countries after the introduction of rotavirus vaccines from the vaccine impact on diarrhea in Africa (VIDA) study. Clin. Infect. Dis. 2023;76(76 Suppl 1):S12–S22. doi: 10.1093/cid/ciad022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kelly C.R., Allegretti J.R. Review article: gastroenterology and Clostridium difficile infection: past, present, and future. Clin. Infect. Dis. 2023;77(Suppl 6):S463–S470. doi: 10.1093/cid/ciad644. [DOI] [PubMed] [Google Scholar]
- 37.Field D., Fernandez de Ullivarri M., Ross R.P., Hill C. After a century of nisin research - where are we now? FEMS Microbiol. Rev. 2023;47(3) doi: 10.1093/femsre/fuad023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Martin J.S., Monaghan T.M., Wilcox M.H. Clostridium difficile infection: epidemiology, diagnosis and understanding transmission. Nat. Rev. Gastroenterol. Hepatol. 2016;13(4):206–216. doi: 10.1038/nrgastro.2016.25. [DOI] [PubMed] [Google Scholar]
- 39.Elbeddini A., Gerochi R. Treatment of Clostridium difficile infection in community teaching hospital: a retrospective study. J. Pharm. Policy Pract. 2021;14(1):19. doi: 10.1186/s40545-020-00289-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Markantonis J.E., Fallon J.T., Madan R., Alam M.Z. Clostridioides difficile infection: diagnosis and treatment challenges. Pathogens. 2024;13(2):118. doi: 10.3390/pathogens13020118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang X.X., Li X.C., Zhang Q.Y., Liu J.S., Han L.F., Lederman Z., et al. Tackling global health security by building an academic community for One Health action. Infect. Dis. Poverty. 2023;12(1):70. doi: 10.1186/s40249-023-01124-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sayasone S., Vonghachack Y., Xia S., Lv S., Zhou X.N., Odermatt P. Integrated Eco-Health approach significantly reduces helminth infections in endemic Khong islands with emphasis on Schistosoma mekongi. Infect. Dis. Poverty. 2024;13(1):57. doi: 10.1186/s40249-024-01226-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wolf J., Hubbard S., Brauer M., Ambelu A., Arnold B.F., Bain R., et al. Effectiveness of interventions to improve drinking water, sanitation, and handwashing with soap on risk of diarrhoeal disease in children in low-income and middle-income settings: a systematic review and meta-analysis. Lancet. 2022;400(10345):48–59. doi: 10.1016/S0140-6736(22)00937-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Local Burden of Disease Diarrhoea Collaborators Mapping geographical inequalities in childhood diarrhoeal morbidity and mortality in low-income and middle-income countries, 2000-17: analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395(10239):1779–1801. doi: 10.1016/S0140-6736(20)30114-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Burnett E., Parashar U.D., Tate J.E. Real-world effectiveness of rotavirus vaccines, 2006-19: a literature review and meta-analysis. Lancet Glob. Health. 2020;8(9):e1195–e1202. doi: 10.1016/S2214-109X(20)30262-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brennhofer S.A., Platts-Mills J.A., Lewnard J.A., Liu J., Houpt E.R., McQuade Rogawski., Et Burden of diarrhea and antibiotic use among children in low-resource settings preventable by Shigella vaccination: a simulation study. PLoS Med. 2023;20(11) doi: 10.1371/journal.pmed.1004271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Merid M.W., Alem A.Z., Chilot D., Belay D.G., Kibret A.A., Asratie M.H., et al. Impact of access to improved water and sanitation on diarrhea reduction among rural under-five children in low and middle-income countries: a propensity score matched analysis. Trop. Med. Health. 2023;51(1):36. doi: 10.1186/s41182-023-00525-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lowe N.M., Hall A.G., Broadley M.R., Foley J., Boy E., Bhutta Z.A. Preventing and controlling zinc deficiency across the life course: a call to action. Adv. Nutr. 2024;15(3) doi: 10.1016/j.advnut.2024.100181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Choudhary T.S., Sinha B., Khera A., Bhandari N., Chu Y., Jackson B., et al. Factors associated with the decline in under-five diarrhea mortality in India: a LiST analysis. J Glob Health. 2019;9(2) doi: 10.7189/jogh.09.020804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sesay B.P., Hakizimana J.L., Elduma A.H., Gebru G.N. Assessment of water, sanitation and hygiene practices among households, 2019 - Sierra Leone: a community-based cluster survey. Environ. Health Insights. 2022;16 doi: 10.1177/11786302221125042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chen J., Gong Y., Chen Q., Li S., Zhou Y. Global burden of soil-transmitted helminth infections, 1990-2021. Infect. Dis. Poverty. 2024;13(1):77. doi: 10.1186/s40249-024-01238-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets analyzed during the current study are available at http://ghdx.healthdata.org/gbd-results-tool.