Abstract
Background
While the hidden curriculum (HC) is becoming recognized as an important component of medical education, ideal methods of assessing the HC are not well known. The aim of this study was to review the literature for methods of assessing the HC in the context of healthcare education.
Methods
We conducted a scoping review on methods to measure or assess the HC in accordance with the JBI Manual for Evidence Synthesis. Ovid MEDLINE, Ovid EMBASE, and ProQuest ERIC databases were searched from inception until August 2023. Studies which focused on healthcare education, including medicine, as well as other professions such as nursing, social work, pharmacy were included. We then obtained stakeholder feedback utilizing the results of this review to inform the ongoing HC assessment process within our own medical education program.
Results
Of 141 studies included for full text review, 41 were included for analysis and data extraction. Most studies were conducted in North America and qualitative in nature. Physician education was best represented with most studies set in undergraduate medical education (n = 21, 51%). Assessment techniques included interviews (n = 19, 46%), cross-sectional surveys (n = 14, 34%), written reflections (n = 7, 17%), and direct observation of the working environment (n = 2, 5%). While attempts to create standardized HC evaluation methods were identified, there were no examples of implementation into an educational program formally or longitudinally. No studies reported on actions taken based on evaluation results. Confidential stakeholder feedback was obtained from postgraduate medical learners in our program, and this feedback was then used to modify our longitudinal HC assessment process.
Conclusions
While the HC has as increasing presence in the medical education community, the ideal way to practically assess it within a healthcare education context remains unclear. We described the HC assessment process utilized at our program, which may be informative for other institutions attempting to implement a similar technique. Future attempts and studies would benefit from reporting longitudinal data and impacts of assessment results
Abstract
Contexte
Bien que le curriculum caché soit de plus en plus reconnu comme une composante importante de l'éducation médicale, ses méthodes idéales d'évaluation ne sont pas bien connues. L'objectif de cette étude était d’examiner la documentation sur les méthodes d'évaluation du curriculum caché dans le contexte de la formation dans les domaines de la santé.
Méthodes
Nous avons effectué un examen de la documentation sur les méthodes de mesure ou d'évaluation du curriculum caché conformément au JBI Manual for Evidence Synthesis. Les bases de données Ovid MEDLINE, Ovid EMBASE et ProQuest ERIC ont été consultées depuis le début jusqu'à août 2023. Les études portant sur l'enseignement des soins de santé, y compris la médecine, ainsi que sur d'autres professions telles que les soins infirmiers, le travail social et la pharmacie ont été incluses. Nous avons ensuite recueilli les commentaires des parties prenantes en utilisant les résultats de cette étude pour orienter le processus d'évaluation continue du curriculum caché au sein de notre propre programme d'éducation médicale.
Résultats
Sur les 141 études retenues pour l'examen du texte intégral, 41 ont été retenues pour l'analyse et l'extraction des données. La plupart des études ont été menées en Amérique du Nord et sont de nature qualitative. La formation des médecins était la mieux représentée, la plupart des études portant sur la formation médicale de premier cycle (n = 21, 51 %). Les techniques d'évaluation comprenaient des entretiens (n = 19, 46 %), des enquêtes transversales (n = 14, 34 %), des réflexions écrites (n = 7, 17 %) et l'observation directe du milieu de travail (n = 2, 5 %). Bien que des tentatives de création de méthodes d'évaluation normalisées du curriculum caché aient été identifiées, il n'y avait pas d'exemples de déploiement dans un programme d'enseignement de manière officielle ou longitudinale. Aucune étude n'a fait état de mesures prises basées sur les résultats de l'évaluation. Des commentaires confidentiels ont été recueillis auprès des apprenants en médecine de niveau postdoctoral de notre programme. Ces commentaires ont ensuite été utilisés pour modifier notre processus d'évaluation longitudinale du curriculum caché.
Conclusions
Bien que le curriculum caché soit de plus en plus présent au sein de l'éducation médicale, la façon idéale de l'évaluer de manière pratique dans un contexte de formation dans les domaines de la santé n'est pas encore claire. Nous avons décrit le processus d'évaluation du curriculum caché utilisé dans notre programme, ce qui peut être instructif pour d'autres établissements qui tentent de mettre en œuvre une technique similaire. Les futures tentatives et études bénificieraient de faire état de données longitudinales et de l'impact des résultats de l'évaluation.
Introduction
The hidden curriculum (HC) has gradually become recognized as an important component of medical education, with use of the term increasing substantially within the literature since 2012.1 While definitions vary, the HC is generally defined as implicit cultural norms, values, and skills that learners gain through observation and interaction with peers and teachers in the work and learning environment. The HC has often been viewed as a negative concept leading learners astray from ideal attitudes, behaviour and interactions.1,2 The HC has been implicated in poor professionalism, erosion of empathy, decreased learner wellbeing, increasing cynicism and burnout.3–5 While some positive impacts of the HC have been described (e.g., in relation to positive role modeling), examples are limited in the literature.1,5
Measuring the HC either qualitatively or quantitatively remains challenging despite its increasing presence in the medical education community and literature, by nature of it being largely an unspoken and unwritten phenomenon. While most medical education programs have well established methods of regularly evaluating the formal curriculum,6–8 few to none have the same for the HC. In addition, there remains debate on the definition of the HC, the role it plays in medical education, and its importance. Given this, we decided to conduct a scoping review on methods to measure and evaluate the HC, as part of our efforts to evaluate the HC in our own postgraduate medical residency training program. Our focus was to identify evaluation methods which could be feasibly implemented in a residency training program longitudinally, allowing for feedback and guidance on improving the program.
Methods
We conducted a scoping review in accordance with the Joanna Briggs Institute Manual for Evidence Synthesis.9 The focus of our review was specifically identifying studies focused on measuring or assessing the HC in the context of medical or physician education. Given the expected paucity of data in this field, we also chose to include studies investigating other healthcare and allied health professions, including but not limited to nursing, dentistry, pharmacy, and social work.
Literature search
We searched the Ovid MEDLINE, Ovid EMBASE, and ProQuest ERIC databases from inception up to August 2023. Our search strategy was refined over several iterations in consultation with a research librarian, referencing text words and index terms used in relevant articles. Full search strategies are included in Appendix 1. Synonyms or alternate terms for the “hidden” curriculum included “informal,” “implicit,” “unintended,” “implied,” “unspoken,” and “inferred.” Search results were limited to English language, due to the largely qualitative and contextual nature of studies involving the HC, and concerns regarding validity of measurement methods in varying languages. The final iteration of the search was run on August 28, 2023.
Selection criteria
We included studies with a stated goal of measuring or assessing the HC in relation to a healthcare professional education program. Studies were excluded if they did not measure the HC directly (e.g., instead they measured compassion or burnout felt to be a result of the HC).
Study selection and data abstraction
Results of our literature search were uploaded into Covidence (Veritas Health Innovation Ltd, Vic, Australia), a systematic review data management software, and duplicates were removed. A pilot test of screening 100 listings was performed, and two reviewers (GL and MS) met following this to discuss concordance and clarify any discrepancies. All further title and abstracts were then screened by two independent reviewers (GL and MS) against the selection criteria. Relevant sources were retrieved in full, and again independently reviewed for inclusion by two reviewers. Any disagreements were resolved through mutual discussion or through a third reviewer if needed. All sources that passed full text review had data abstracted using Covidence. Relevant data included details on study population, assessment creation, HC assessment method, results of the assessment, and actions based on these results. We did not critically appraise or assess the quality of included studies, as the goal of this study was to identify and summarize all methods used to assess the HC. This scoping review and protocol was registered with the Open Science Framework.10
Stakeholder feedback
As a final component of our review, we sought stakeholder feedback based on results of our scoping review, to inform the evolving HC assessment process at our own institution. This involved presenting the completed results of this review to all learners within our postgraduate medical education program (felt to be the most relevant stakeholders) during a mandatory scheduled teaching session, and allowing for asynchronous submission of anonymous feedback following this. The feedback was then used to modify and update our previously utilized assessment methodology (unpublished).
Results
Out of 2060 unique studies reviewed/screened, a final of 41 studies were included for data extraction and analysis. Figure 1 shows the flowchart for studies included in our review. A list of all included studies is available in Appendix B. Table 1 provides an overview of characteristics of included studies. The earliest study found was from 2004, and more studies were published in recent years, supporting the relatively new and growing interest in this topic. Most studies were conducted in North America (51%, n = 21). The most common study populations (in descending percentage, with some studies including more than one of each population) were medical students (51%, n = 21), medical residents (32%, n = 13), and staff or faculty physicians (22%, n = 9). Other healthcare professions included were social work students (10%, n = 4), nursing students (7%, n = 3), veterinary medicine students (5%, n = 2), and pharmacy residents/students (5%, n = 2). Twenty-seven studies used primarily qualitative methods (66%, n = 27), while 14 use primarily quantitative methods (34%, n = 14).
Figure 1.
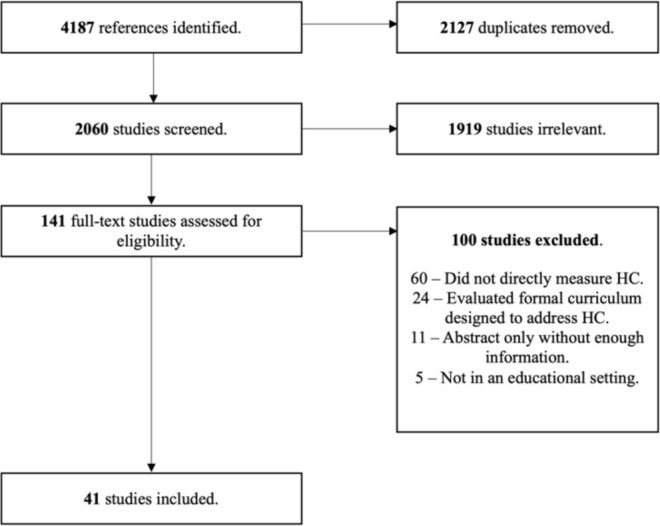
Flowchart of studies included for review
Table 1.
Overview of included studies (N = 41)
| Descriptor | Characteristic |
|---|---|
| Date Published | |
| 2004 – 2009 | n = 7 (17%) |
| 2011 – 2015 | n = 8 (20%) |
| 2015 - 2019 | n = 15 (36%) |
| 2021 – 2023 | n = 11 (27%) |
| Study Location | |
| North America | n = 21 (51%) |
| Asia | n = 8 (20%) |
| Europe | n = 6 (15%) |
| Australia and New Zealand | n = 5 (12%) |
| Africa | n = 1 (2%) |
| Study Population* | |
| Medical Students | n = 21 (51%) |
| Medical Residents | n = 13 (32%) |
| Staff/Faculty Physicians | n = 9 (22%) |
| Social Work Students | n = 4 (10%) |
| Nursing Students | n = 3 (7%) |
| Veterinary Students | n = 2 (5%) |
| Pharmacy Residents/Students | n = 2 (5%) |
| HC Measurement Method | |
| Qualitative | n = 27 (66%) |
| Quantitative | n = 14 (34%) |
| HC Measurement Technique** | |
| Interview/Focus Group | n = 19 (46%) |
| Cross Sectional Survey | n = 14 (34%) |
| Review of Written Reflections | n = 7 (17%) |
| Workplace Observation | n = 2 (5%) |
Assessment methods
Qualitative. The most frequently used method to assess or explore the HC involved conducting individual and/or focus group interviews (46%, n = 19), which would be recorded and transcribed for subsequent qualitative analysis.11–29 Reported interviews ranged from 15 minutes to over two hours and were often semi-structured in nature. Transcripts were then analyzed using methods such as grounded theory or thematic analysis to determine prominent themes. These themes could then be compared to stated objectives within the formal curriculum to identify any mismatches, or compared between groups of interviewees to identify differences in perception of the HC.
Beyond the use of interviews and focus groups, another common qualitative assessment method was through review of written reflections or narratives written by trainees, often mandatory as part of a reflective course, or as part of an end of term assessment (17%, n = 7).11,30–35 More resource intensive qualitative data collection methods included direct observation of the workplace (5%, n = 2).25,36,37 In these studies, authors would insert themselves as passive observers within a clinical teaching unit, creating field notes and documenting observed interactions between and reactions from participants. Finally, Cheng and Yang present a unique study by performing discourse analysis of posts from internet forums (bulletin or message boards) hosted my medical schools, where medical students would informally socialize amongst each other prior to the era of common social media usage.34
Quantitative. Fourteen identified studies employed a quantitative assessment method, all in the form of cross-sectional surveys.4,38–50 Within these studies, eight focused on the creation of a new validated measurement tool, while six attempted to evaluate or implement a previously created tool. A total of nine unique assessment tools were identified, and a summary of these is presented in Table 2.
Table 2.
Summary of identified hidden curriculum assessment tools
| Name of Tool | Original Authors | Target Demographic | Development Method | Domains | Contents |
|---|---|---|---|---|---|
| Communication, Curriculum, and Culture (C3) Instrument | Haidet, Kelly, and Chou 200543 |
Medical Students North America | Literature review, group consensus using modified Delphi technique, focus groups with target group and psychometrician |
|
29 items scored on either a 5- or 7-point Likert scale Both positive and negative items |
| Implicit Curriculum Survey (ICS) | Grady et al. 201140 |
Social Work Students North America | Literature review and group consensus |
|
67 quantitative items scored on a 5-point Likert scale, along with 15 qualitative items Neutral items |
| N/A | Billings et al. 20114 |
Internal Medicine Resident Physicians North America | Partially used pre-existing Maslach Burnout Inventory, as well as literature review and focus groups |
|
20 items scored on a 5-point Likert scale Negative items only |
| Hidden Informal Curriculum Assessment Tool (HICAT) | McGurgan, Carmody, and Tregonning 2015 |
Medical Students Australia |
Unknown (original publication not available) | N/A | 20 items scored on a 5-point Likert scale 10 positive and 10 negative items |
| N/A | Smith and Castanelli 201544 |
Anesthesia Resident Physicians Australia |
Literature review, pilot with convenience group of trainees, focus group with academic physicians |
|
38 items scored on a 5-point Likert scale Neutral items |
| Limited English Proficiency-Hidden Curriculum (LEP-HC) | Green et al. 201847 |
Medical Students North America |
Based on thematic analysis conducted from prior semi-structured interviews |
|
23 items scored on a 5-point Likert scale |
| Vienna Hidden Curriculum (VHC) | Ludwig et al. 201848 |
Medical Students Europe |
Literature review |
|
40 items scored on a non-dichotomous ordinal scale ranging from -3 to +3 Neutral items |
| N/A | Kaldjian et al. 201949 |
Medical Students, Resident Physicians, Faculty Physicians North America |
Content analysis on initial pilot survey using closed- and open-ended questions | N/A | 27 items scored on a 5-point Likert scale Neutral items |
| Hidden Curriculum Evaluation Scale in Nursing Education (HCES-N) | Akçakoca and Orgun 202145 |
Nursing Students Asia |
Literature review, group consensus between faculty members, pilot study with students |
|
43 items scored on a 5-point Likert scale Both positive and negative items |
Most tools were developed through literature review followed by group consensus. Certain tools such as the Implicit Curriculum Survey (ICS) and those created by Smith and Castanelli, and Kaldjian et al., generated several versions of the survey, refined through piloting sets of questions with either the target audience or faculty members.40,44,49 Only two tools, Kaldjian et al. and the Limited English Proficiency-Hidden Curriculum (LEP-HC) survey used thematic analysis of previous qualitative assessments to inform creation of their quantitative tools.47,49
The nine identified assessment tools consisted of between 20 to 82 questions or items. All tools utilized quantitative items, almost all scored using 5-point Likert scales. Only one tool (the Vienna Hidden Curriculum) employed a non-dichotomous ordinal scale ranging from -3 to +3.48 In addition, one tool (the ICS) included qualitative items (15 out of 82 total items). In general, tools utilized neutral or a combination of positive and negative wording for items, with the exception of the Billings et al. tool surveying trainees only on negative experiences.4 Seven of 9 tools also categorized assessment items into distinct domains. These domains were typically generated from literature review, and common domains that appeared include role modeling, workplace/learning environment, and social interactions.
Assessment results and outcomes
Using the above assessment tools, authors were able to identify various unique factors which contributed or detracted from their respective teaching and learning environments. While many studies targeted HC as a negative concept, several identified elements of the HC which contributed positively as well. Positive factors identified most often included positive role modeling from superiors, with regards to patient care, communication, and leadership.18,29,36 Examples of negative factors included observed or experienced disrespect amongst healthcare providers and learners, as well as with patients.4,34
While various statistical methods were used to validate the created tools, no studies offered longitudinal data or evidence that surveying the HC could lead to environmental or curricular reform. Grady et al. in 2020 reported on use of the ICS across four separate institutions over the course of two years, although results were not tracked longitudinally.38
While defining the HC was outside the scope of this present review, it is important to note that studies included in this scoping review did use a wide variety of definitions. The most common definition cited was Hafferty’s 1998 definition, in which the HC is defined as “a set of influences that function at the level of organizational structure and culture.”51
Stakeholder feedback
We presented the results of our scoping review to all learners within our postgraduate medical education program, during a scheduled mandatory session to discuss the HC. The feedback obtained from this process was collected in an anonymous and confidential fashion given the potential sensitivity of included topics, and therefore will not be included here. We discuss the impact of this feedback on our program’s evolving HC assessment process further in the following sections.
Discussion
The objective of our scoping review was to identify methods used to assess the hidden curriculum in medical education. We identified qualitative and quantitative assessment methods, in the setting of physician education, as well as social work, nursing, veterinary medicine, and pharmacy. Nine standardized quantitative assessment tools were identified, although there were no examples of tools implemented formally or longitudinally.
As the concept of the HC gains traction within the medical education community, literature has linked it to many phenomena, from attracting/dissuading students from pursuing certain specialties, to influencing how students and trainee physicians communicate or interact with patients.1,47 It is hypothesized that in some cases, the effects of the HC can be more influential than the formal curriculum itself, and can sometimes directly oppose what medical educators objectively set out to teach.1 Recognizing this potential significant influence of the HC, the next step in addressing the HC should be identifying and assessing it in a way that allows educators to leverage the positive impacts and minimize the negative impacts. Recognizing this, our scoping review was motivated by a desire to better understand and approach how the HC affects trainees within our own postgraduate medical education program. Within Canada, addressing/reflecting on the HC has become a standard part of undergraduate medical education, and this effort has expanded to postgraduate residency education as well.52 In particular, The Royal College of Physicians and Surgeons of Canada (RCPSC), which oversees the accreditation of all residency programs, has mandated the evaluation of the learning environment, including any influences resulting from the presence of the HC.6 In this setting, any possible evaluation tool should be carefully evaluated for feasibility prior to implementation, in terms of resources needed from the program, as well as from the trainee. Given the ambiguous nature of the HC, there may never be a true “gold standard” method for evaluating it, as areas that need assessing may vary significantly between programs and environments. In addition, unlike the formal curriculum, there are no pre-identified components or objectives of the HC, which could be used to direct assessments. As such, qualitative methods, which constituted 66% of the studies identified in our review, may provide a more nuanced and holistic assessment of the HC, at the cost of being significantly more resource intensive. For example, using the most common qualitative method of either one-on-one interviews or focus groups would require a substantial time requirement from program administrators and trainees. There may also be challenges in terms of scheduling these in-person sessions, in addition to concerns about confidentiality of interviews, particularly as many aspects of the HC are interpersonal in nature.
Conversely, a quantitative measurement tool would be much simpler to implement, requiring less person-hours from the program and would allow for anonymized results. Quantitative survey tools also allow trainees increased flexibility in completing the quantitative survey, as compared to scheduling in person interviews for qualitative assessments. However, quantitative HC tools need to address HC themes important for all trainees in the program and the HC tool needs flexibility for revisions as HC topics are dynamic and are expected to change over time.
A HC assessment tool in the context of medical education, could also utilize both qualitative and quantitative components. This could exist as a single tool such as the Implicit Curriculum Survey, which employs both closed- and open-ended questions, or perhaps a dynamically evolving tool which could be initially developed similar to the tools developed by Billings et al. and Smith & Castanelli,4,43,44 with the addition of then being refined on a regular basis. Ideally, a third-party unbiased participant (separate from faculty members and trainees) could conduct an initial exploratory analysis using qualitative methods such as interviews, focus groups, and/or workplace observation to identify the specific needs of each learning environment. This process would inform the development of a subsequent quantitative tool, to be used for several assessment cycles (e.g., academic year). Assuming the work environment and therefore HC is dynamic and subject to change, the initial qualitative analysis would then be repeated every 3-5 years (or as determined appropriate by the program) to update the quantitative tool.
While our review was able to identify several HC assessment tools, including tools which were used at different time points in different environments, there were no published examples of the results from these tools being used to implement curricular or environmental change. Given how recently the HC itself was acknowledged as an established concept, the use of these tools to draw attention to and bring awareness to the subject is nevertheless an important development.
The goal of this scoping review was to assess the current state of the literature as it pertains to measuring and assessing the HC, to inform our own programmatic efforts to address the HC. While we attempted to create thorough search strategies, our results were limited to the three databases used, as well as studies published in English. In addition, we did not critically appraise or assess the quality of included studies.
As a result of the previously discussed RCPSC requirement, our postgraduate training program utilized the results of this scoping review to inform our own assessment of the hidden curriculum. We utilized the following approach, with steps 1 to 6 having been established prior to completion of this review:
Trainee and Faculty education on the HC: We invited 3 HC experts (a health professions HC educator, a learner wellness leader, and a curriculum and evaluation leader) to give a 1-hour lecture on the HC.
HC assessment planning: An Academic Half Day was scheduled during which time, residents and one faculty member convened to discuss the HC and make a plan for measuring the HC in the program.
HC survey development: With a focus group of residents, HC items felt relevant for the training program were developed. Anonymous and confidential feedback from residents was collated by a resident representative. The final HC survey (unpublished and confidential) contained both positive and negative HC items. There were 34 questions in total, which covered Lawrence et al.’s (1) conceptual HC groupings: institutional-organizational, interpersonal-social, contextual-cultural, and motivational-psychological. All responses were based on one of 7 options (never, rarely, half the time, often, always, not sure, prefer not to say).
HC survey awareness: The HC survey was presented to faculty within the program prior to administering the survey.
HC survey administration: The survey was anonymously administered to all residents in the program.
HC survey result dissemination: The HC survey results were shared among the residents and faculty within the program.
HC survey updates and longitudinal assessment: We plan on yearly academic half day sessions to reflect on HC, which includes examining the results of the survey, reassessing the questions of the survey, and re-administering the HC survey yearly. The goal would be to assess for changes in key HC topics, identify areas for change and to gauge success of targeted interventions. The results of this scoping review were shared with all residents, to help gathering feedback on our previously utilized process. The feedback obtained (which is kept as confidential and unpublished) was used to modify the survey developed in step 3. The modifications were reviewed with resident leaders, as well as faculty leadership involved with the residency program. Importantly, modifications were made with attention to keeping consistency when possible, between versions, to allow for meaningful comparisons between previous and future results.
Conclusions
As the concept of HC continues to gain traction within the medical education community and literature, the definition of HC and how to assess and measure it remains somewhat ambiguous. While our review was able to identify many qualitative and some quantitative methods of measuring the HC, there were no examples of these being used to reform or address the HC. We share the methodology recently implemented at our institution, which has been informed by the results of this review, created with a focus on assessing the HC in a longitudinal manner. Future works in HC assessment should focus on clearly defining HC itself, the goals behind assessing the HC, and whether targeted interventions can successfully be applied as a result.
Appendix A. Search strategies
Database: Ovid MEDLINE(R) 1946 to August Week 4 2023
Search statements: ((hidden or informal or implicit or unintended or implied or unspoken or inferred) adj5 curricul*).tw,kf.
Database: Ovid EMBASE(R) 1947 to 2023 August 28
Search statements: ((hidden or informal or implicit or unintended or implied or unspoken or inferred) adj5 curricul*).tw,kf.
Database: Proquest ERIC, all available dates, searched Aug 28, 2023
Search statements: noft((hidden or informal or implicit or unintended or implied or unspoken or inferred) NEAR/5 curricul*)
Appendix B. Full list of included studies
| 1. | Cohen-Osher M, Lee AL, Erlich D. Revealing the hidden clerkship curriculum: a qualitative analysis. Fam Med. 2023;55(2):115–8. https://doi.org/10.22454/FamMed.2023.503671.30 |
|---|---|
| 2. | Lee CA, Wilkinson TJ, Timmermans JA, Ali AN, Anakin MG. Revealing the impact of the hidden curriculum on faculty teaching: a qualitative study. Med Educ. 2023;57(8):761–9. https://doi.org/10.1111/medu.1502611 |
| 3. | Grady MD, Swick DC, Powers JD. The implicit curriculum survey: an examination of the psychometric properties. J Soc Work Educ. 2018;54(2):261–9. https://doi.org/10.1080/10437797.2017.140452739 |
| 4. | Grady MD, Powers J, Despard M, Naylor S. Measuring the implicit curriculum: initial development and results of an msw survey. J Soc Work Educ. 2011;47(3):463–87. https://doi.org/10.5175/JSWE.2011.20090011940 |
| 5. | Grady MD, Rich Glass V, Lechner E, Naylor SM. What do MSW students say matters in MSW Programs? Results from a qualitative study of the implicit curriculum. J Soc Work Educ. 2020;56(3):560–75. https://doi.org/10.1080/10437797.2019.165658538 |
| 6. | Peterson NA, Farmer AY, Donnelly L, Forenza B. Assessing the implicit curriculum in social work education: heterogeneity of students’ experiences and impact on professional empowerment. J Teach Soc Work. 2014;34(5):460–79. https://doi.org/10.1080/08841233.2014.95594341 |
| 7. | Afridi A, Sethi A, Ahmed F, Kashif L. Assessment of hidden curriculum during clinical rotations of year 4 mbbs students using hidden informal curriculum assessment tool (Hicat). J Med Sci Peshawar. 2020;28(4):352–5. https://doi.org/10.52764/jms.20.28.4.1042 |
| 8. | Van Huyssteen M, Bheekie A. The hidden curriculum of work-based learning for pharmacy students in public sector pharmacies in South Africa. Pharm Educ. 2017;17(1):190–8.31 |
| 9. | Haidet P, Kelly PA, Chou C, Communication C and culture study group. Characterizing the patient-centeredness of hidden curricula in medical schools: development and validation of a new measure. Acad Med J Assoc Am Med Coll. 2005;80(1):44–50. https://doi.org/10.1097/00001888-200501000-0001243 |
| 10. | Wear D, Skillicorn J. Hidden in plain sight: the formal, informal, and hidden curricula of a psychiatry clerkship . Acad Med J Assoc Am Med Coll. 2009;84(4):451–8. https://doi.org/10.1097/ACM.0b013e31819a80b712 |
| 11. | Balmer DF, Master CL, Richards B, Giardino AP. Implicit versus explicit curricula in general pediatrics education: is there a convergence? Pediatrics. 2009;124(2):e347-54. https://doi.org/10.1542/peds.2009-017036 |
| 12. | Howard F, McKneally MF, Upshur REG, Levin AV. The formal and informal surgical ethics curriculum: views of resident and staff surgeons in Toronto. Am J Surg. 2012;203(2):258–65. https://doi.org/10.1016/j.amjsurg.2011.02.008.13 |
| 13. | Smith NA, Castanelli DJ. Measuring the clinical learning environment in anaesthesia. Anaesth Intensive Care. 2015;43(2):199–203. https://doi.org/10.1177/0310057X1504300209.44 |
| 14. | McKenna L, Williams B. The hidden curriculum in near-peer learning: an exploratory qualitative study. Nurse Educ Today. 2017;50(ned, 8511379):77–81. https://doi.org/10.1016/j.nedt.2016.12.010.14 |
| 15. | Choo Hwee P, Hwee Sing K, Yong Hwang MK, Mei AHY. The informal curriculum: what do junior doctors learn from a palliative care rotation?. BMJ Support Palliat Care. 2020;10(1):114–7. https://doi.org/10.1136/bmjspcare-2018-001625.15 |
| 16. | St-Amant O, Sutherland N. Unpacking the hidden curriculum in nursing education: clinical placements abroad. Int J Nurs Educ Scholarsh. 2020;17(1). https://doi.org/10.1515/ijnes-2019-0128.16 |
| 17. | Akcakoca B, Orgun F. Developing a measurement tool for evaluating the hidden curriculum in nursing education . Nurse Educ Today. 2021;97(ned, 8511379):104688. https://doi.org/10.1016/j.nedt.2020.104688.45 |
| 18. | Lempp H, Seale C. The hidden curriculum in undergraduate medical education: qualitative study of medical students’ perceptions of teaching. Br Med J. 2004;329(7469):770–3. https://doi.org/10.1136/bmj.329.7469.770.17 |
| 19. | Ozolins I, Hall H, Peterson R. The student voice: recognising the hidden and informal curriculum in medicine. Med Teach. 2008;30(6):606–11. https://doi.org/10.1080/01421590801949933.18 |
| 20. | Phillips CB. Student portfolios and the hidden curriculum on gender: Mapping exclusion. Med Educ. 2009;43(9):847–53. https://doi.org/10.1111/j.1365-2923.2009.03403.x.32 |
| 21. | Billings ME, Lazarus ME, Wenrich M, Curtis JR, Engelberg RA. The effect of the hidden curriculum on resident burnout and cynicism. J Grad Med Educ. 2011 Dec;3(4):503–https://doi.org/10. https://doi.org/10.4300/JGME-D-11-00044.1.4 |
| 22. | Al-Bawardy R, Blatt B, Al-Shohaib S, Simmens SJ. Cross-cultural comparison of the patient-centeredness of the hidden curriculum between a Saudi Arabian and 9 US medical schools. Med Educ Online. 2009;14((Al-Bawardy) Department of Medicine, School of Medicine and Health Sciences, The George Washington University, Washington, DC, USA.):19. https://doi.org/10.3402/meo.v14i.4655.46 |
| 23. | Karnieli-Miller O, Vu TR, Holtman MC, Clyman SG, Inui TS. Medical students’ professionalism narratives: a window on the informal and hidden curriculum . Acad Med. 2010;85(1):124–33. https://doi.org/10.1097/ACM.0b013e3181c42896.33 |
| 24. | Lamiani G, Leone D, Meyer EC, Moja EA. How Italian students learn to become physicians: a qualitative study of the hidden curriculum. Med Teach. 2011;33(12):989–96. https://doi.org/10.3109/0142159X.2011.577467.19 |
| 25. | Mossop L, Dennick R, Hammond R, Robbe I. Analysing the hidden curriculum: use of a cultural web. Med Educ. 2013;47(2):134–43. https://doi.org/10.1111/medu.12072.20 |
| 26. | Van Deven T, Hibbert K, Faden L, Chhem RK. The hidden curriculum in radiology residency programs: a path to isolation or integration? Eur J Radiol. 2013;82(5):883–7. https://doi.org/10.1016/j.ejrad.2012.12.001.21 |
| 27. | Cheng L-F, Yang H-C. Learning about gender on campus: an analysis of the hidden curriculum for medical students. Med Educ. 2015;49(3):321–31. https://doi.org/10.1111/medu.12628.34 |
| 28. | O’Brien BC, Hirsh D, Krupat E, et al. Learners, performers, caregivers, and team players: descriptions of the ideal medical student in longitudinal integrated and block clerkships. Med Teach. 2016;38(3):297–305.22 |
| 29. | Doja A, Bould MD, Clarkin C, Eady K, Sutherland S, Writer H. The hidden and informal curriculum across the continuum of training: a cross-sectional qualitative study. Med Teach. 2016;38(4):410–8. https://doi.org/10.3109/0142159X.2015.1073241.23 |
| 30. | Gerjevic KA, Rosenbaum ME, Suneja M. Resident perceptions of the impact of duty hour restrictions on resident-attending interactions: an exploratory study. BMC Med Educ. 2017;17(1):124. https://doi.org/10.1186/s12909-017-0963-7.24 |
| 31. | Roder CA, May SA. The hidden curriculum of veterinary education: mediators and moderators of its effects. J Vet Med Educ. 2017;44(3):542–51. https://doi.org/10.3138/jvme.0416-082.25 |
| 32. | Gardeshi Z, Amini M, Nabeiei P. The perception of hidden curriculum among undergraduate medical students: a qualitative study. BMC Res Notes. 2018;11(1):271. https://doi.org/10.1186/s13104-018-3385-7.26 |
| 33. | Doja A, Bould MD, Clarkin C, Zucker M, Writer H. Observations of the hidden curriculum on a paediatrics tertiary care clinical teaching unit. Paediatr Child Health Can. 2018;23(7):435–40. https://doi.org/10.1093/pch/pxx206.37 |
| 34. | Green AR, Rosu C, Kenison T, Nze C. Assessing the hidden curriculum for the care of patients with limited English proficiency: an instrument development. Educ Health Abingdon Engl. 2018;31(1):17–24. https://doi.org/10.4103/1357-6283.239042.47 |
| 35. | Ludwig B, Turk B, Seitz T, Klaus I, Loffler-Stastka H. The search for attitude-a hidden curriculum assessment from a central European perspective. Wien Klin Wochenschr. 2018;130(3–4):134–40. https://doi.org/10.1007/s00508-018-1312-5.48 |
| 36. | Kaldjian LC, Shinkunas LA, Reisinger HS, Polacco MA, Perencevich EN. Attitudes about sickness presenteeism in medical training: is there a hidden curriculum ? Antimicrob Resist Infect Control. 2019;8(1):149. https://doi.org/10.1186/s13756-019-0602-7.49 |
| 37. | Bigdeli S, Koohestani HR, Soltani Arabshahi SK, Keshavarzi MH. Lived experiences of undergraduate medical students about hidden curriculum: a phenomenological study. Acta Med Iran. 2019;57(5):308–15. https://doi.org/10.18502/acta.v57i5.1867.27 |
| 38. | Parekh R, Jones MM, Singh S, et al. Medical students’ experience of the hidden curriculum around primary care careers: a qualitative exploration of reflective diaries. BMJ Open. 2021;11(7):e049825. https://doi.org/10.1136/bmjopen-2021-049825.35 |
| 39. | Butler J, Kassel L, Miesner AR, Grady S, Wall GC. Incidence of a negative hidden curriculum, cynicism, and burnout within pharmacy resident education: a nationwide survey. Curr Pharm Teach Learn. 2021;13(8):922–7. https://doi.org/10.1016/j.cptl.2021.06.001.50 |
| 40. | Yahyavi ST, Hoobehfekr S, Tabatabaee M. Exploring the hidden curriculum of professionalism and medical ethics in a psychiatry emergency department. Asian J Psychiatry. 2021;66((Yahyavi, Hoobehfekr, Tabatabaee) Department of Psychiatry, Roozbeh Hospital, School of Medicine, Tehran University of Medical Sciences, Tehran, Iran, Islamic Republic of):102885. https://doi.org/10.1016/j.ajp.2021.102885.28 |
| 41. | MacNeil KA, Regehr G, Holmes CL. Contributing to the hidden curriculum: exploring the role of residents and newly graduated physicians. Adv Health Sci Educ Theory Pract. 2022;27(1):201–13. https://doi.org/10.1007/s10459-021-10081-8.29 |
Funding Statement
Funding:
None
Conflicts of Interest
None
Edited by
Marco Zaccagnini (senior section editor); Marcel D’Eon (editor-in-chief)
References
- 1.Lawrence C, Mhlaba T, Stewart KA, Moletsane R, Gaede B, Moshabela M. The hidden curricula of medical education: a scoping review. Acad Med J Assoc Am Med Coll. 2018. Apr;93(4):648–56. 10.1097/ACM.0000000000002004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sarikhani Y, Shojaei P, Rafiee M, Delavari S. Analyzing the interaction of main components of hidden curriculum in medical education using interpretive structural modeling method. BMC Med Educ. 2020. Jun 1;20:176. 10.1186/s12909-020-02094-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zgheib NK, Dimassi Z, Arawi T, Badr KF, Sabra R. Effect of targeted curricular reform on the learning environment, student empathy, and hidden curriculum in a medical school: a 7-year longitudinal study. J Med Educ Curric Dev. 2020. Aug 27;7:2382120520953106. 10.1177/2382120520953106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Billings ME, Lazarus ME, Wenrich M, Curtis JR, Engelberg RA. The effect of the hidden curriculum on resident burnout and cynicism. J Grad Med Educ. 2011. Dec;3(4):503–10. 10.4300/JGME-D-11-00044.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brown MEL, Coker O, Heybourne A, Finn GM. Exploring the hidden curriculum’s impact on medical students: professionalism, identity formation and the need for transparency. Med Sci Educ. 2020. Jul 24;30(3):1107–21. 10.1007/s40670-020-01021-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Canadian Residency Accreditation Consortium C . General Standards of Accreditation for Residency Programs. 2020. Available from: https://www.royalcollege.ca/content/dam/documents/accreditation/competence-by-design/non-resource-documents/canera/general-standards-accreditation-for-residency-programs-e.html#standard_9
- 7.Braund H, Patel V, Dalgarno N, Mann S. Exploring residents’ perceptions of competency-based medical education across Canada: a national survey study. MedEdPublish. 2024. Jan 8;14:2. 10.12688/mep.19247.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nidumolu A, Freedman D, Bosma M. From theory to practice: development and evaluation of a quality improvement curriculum for psychiatry residents. J Med Educ Curric Dev. 2024. Jan;11:23821205241228200. 10.1177/23821205241228200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peters M, Godfrey C, McInerney P, Munn Z, Trico A, Khalil H. Chapter 11: scoping reviews. In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis. JBI; 2020. 10.46658/JBIRM-20-01 [DOI] [Google Scholar]
- 10.George Li. A scoping review on measuring the hidden curriculum in medical education. 2022. Available from: https://osf.io/tbkaf [Accessed Apr 4, 2024].
- 11.Lee CA, Wilkinson TJ, Timmermans JA, Ali AN, Anakin MG. Revealing the impact of the hidden curriculum on faculty teaching: a qualitative study. Med Educ. 2023;57(8):761–9. 10.1111/medu.15026 [DOI] [PubMed] [Google Scholar]
- 12.Wear D, Skillicorn J. Hidden in plain sight: the formal, informal, and hidden curricula of a psychiatry clerkship. Acad Med J Assoc Am Med Coll. 2009;84(4):451–8. 10.1097/ACM.0b013e31819a80b7 [DOI] [PubMed] [Google Scholar]
- 13.Howard F, McKneally MF, Upshur REG, Levin AV. The formal and informal surgical ethics curriculum: views of resident and staff surgeons in Toronto. Am J Surg. 2012;203(2):258–65. 10.1016/j.amjsurg.2011.02.008 [DOI] [PubMed] [Google Scholar]
- 14.McKenna L, Williams B. The hidden curriculum in near-peer learning: an exploratory qualitative study. Nurse Educ Today. 2017;50(ned, 8511379):77–81. 10.1016/j.nedt.2016.12.010 [DOI] [PubMed] [Google Scholar]
- 15.Choo Hwee P, Hwee Sing K, Yong Hwang MK, Mei AHY. The informal curriculum: what do junior doctors learn from a palliative care rotation?. BMJ Support Palliat Care. 2020;10(1):114–7. 10.1136/bmjspcare-2018-001625 [DOI] [PubMed] [Google Scholar]
- 16.St-Amant O, Sutherland N. Unpacking the hidden curriculum in nursing education: clinical placements abroad. Int J Nurs Educ Scholarsh. 2020;17(1). 10.1515/ijnes-2019-0128 [DOI] [PubMed] [Google Scholar]
- 17.Lempp H, Seale C. The hidden curriculum in undergraduate medical education: qualitative study of medical students’ perceptions of teaching. Br Med J. 2004;329(7469):770–3. 10.1136/bmj.329.7469.770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ozolins I, Hall H, Peterson R. The student voice: recognising the hidden and informal curriculum in medicine. Med Teach. 2008;30(6):606–11. 10.1080/01421590801949933 [DOI] [PubMed] [Google Scholar]
- 19.Lamiani G, Leone D, Meyer EC, Moja EA. How Italian students learn to become physicians: a qualitative study of the hidden curriculum. Med Teach. 2011;33(12):989–96. 10.3109/0142159X.2011.577467 [DOI] [PubMed] [Google Scholar]
- 20.Mossop L, Dennick R, Hammond R, Robbe I. Analysing the hidden curriculum: use of a cultural web. Med Educ. 2013;47(2):134–43. 10.1111/medu.12072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Van Deven T, Hibbert K, Faden L, Chhem RK. The hidden curriculum in radiology residency programs: a path to isolation or integration? Eur J Radiol. 2013;82(5):883–7. 10.1016/j.ejrad.2012.12.001 [DOI] [PubMed] [Google Scholar]
- 22.O’Brien BC, Hirsh D, Krupat E, et al. Learners, performers, caregivers, and team players: descriptions of the ideal medical student in longitudinal integrated and block clerkships. Med Teach. 2016;38(3):297–305. [DOI] [PubMed] [Google Scholar]
- 23.Doja A, Bould MD, Clarkin C, Eady K, Sutherland S, Writer H. The hidden and informal curriculum across the continuum of training: a cross-sectional qualitative study. Med Teach. 2016;38(4):410–8. 10.3109/0142159X.2015.1073241 [DOI] [PubMed] [Google Scholar]
- 24.Gerjevic KA, Rosenbaum ME, Suneja M. Resident perceptions of the impact of duty hour restrictions on resident-attending interactions: an exploratory study. BMC Med Educ. 2017;17(1):124. 10.1186/s12909-017-0963-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roder CA, May SA. The hidden curriculum of veterinary education: mediators and moderators of its effects. J Vet Med Educ. 2017;44(3):542–51. 10.3138/jvme.0416-082 [DOI] [PubMed] [Google Scholar]
- 26.Gardeshi Z, Amini M, Nabeiei P. The perception of hidden curriculum among undergraduate medical students: a qualitative study. BMC Res Notes. 2018;11(1):271. 10.1186/s13104-018-3385-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bigdeli S, Koohestani HR, Soltani Arabshahi SK, Keshavarzi MH. Lived experiences of undergraduate medical students about hidden curriculum: a phenomenological study. Acta Med Iran. 2019;57(5):308–15. 10.18502/acta.v57i5.1867 [DOI] [Google Scholar]
- 28.Yahyavi ST, Hoobehfekr S, Tabatabaee M. Exploring the hidden curriculum of professionalism and medical ethics in a psychiatry emergency department. Asian J Psychiatry. 2021;66((Yahyavi, Hoobehfekr, Tabatabaee) Department of Psychiatry, Roozbeh Hospital, School of Medicine, Tehran University of Medical Sciences, Tehran, Iran, Islamic Republic of):102885. 10.1016/j.ajp.2021.102885 [DOI] [PubMed] [Google Scholar]
- 29.MacNeil KA, Regehr G, Holmes CL. Contributing to the hidden curriculum: exploring the role of residents and newly graduated physicians. Adv Health Sci Educ Theory Pract. 2022;27(1):201–13. 10.1007/s10459-021-10081-8 [DOI] [PubMed] [Google Scholar]
- 30.Cohen-Osher M, Lee AL, Erlich D. Revealing the hidden clerkship curriculum: a qualitative analysis. Fam Med. 2023;55(2):115–8. 10.22454/FamMed.2023.503671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Van Huyssteen M, Bheekie A. The hidden curriculum of work-based learning for pharmacy students in public sector pharmacies in South Africa. Pharm Educ. 2017;17(1):190–8. [Google Scholar]
- 32.Phillips CB. Student portfolios and the hidden curriculum on gender: Mapping exclusion. Med Educ. 2009;43(9):847–53. 10.1111/j.1365-2923.2009.03403.x [DOI] [PubMed] [Google Scholar]
- 33.Karnieli-Miller O, Vu TR, Holtman MC, Clyman SG, Inui TS. Medical students’ professionalism narratives: a window on the informal and hidden curriculum. Acad Med. 2010;85(1):124–33. 10.1097/ACM.0b013e3181c42896 [DOI] [PubMed] [Google Scholar]
- 34.Cheng L-F, Yang H-C. Learning about gender on campus: an analysis of the hidden curriculum for medical students. Med Educ. 2015;49(3):321–31. 10.1111/medu.12628 [DOI] [PubMed] [Google Scholar]
- 35.Parekh R, Jones MM, Singh S, et al. Medical students’ experience of the hidden curriculum around primary care careers: a qualitative exploration of reflective diaries. BMJ Open. 2021;11(7):e49825. 10.1136/bmjopen-2021-049825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Balmer DF, Master CL, Richards B, Giardino AP. Implicit versus explicit curricula in general pediatrics education: is there a convergence? Pediatrics. 2009;124(2):e347-54. 10.1542/peds.2009-0170 [DOI] [PubMed] [Google Scholar]
- 37.Doja A, Bould MD, Clarkin C, Zucker M, Writer H. Observations of the hidden curriculum on a paediatrics tertiary care clinical teaching unit. Paediatr Child Health Can. 2018;23(7):435–40. 10.1093/pch/pxx206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grady MD, Rich Glass V, Lechner E, Naylor SM. What do MSW students say matters in MSW Programs? Results from a qualitative study of the implicit curriculum. J Soc Work Educ. 2020;56(3):560–75. 10.1080/10437797.2019.1656585 [DOI] [Google Scholar]
- 39.Grady MD, Swick DC, Powers JD. The implicit curriculum survey: an examination of the psychometric properties. J Soc Work Educ. 2018;54(2):261–9. 10.1080/10437797.2017.1404527 [DOI] [Google Scholar]
- 40.Grady MD, Powers J, Despard M, Naylor S. Measuring the implicit curriculum: initial development and results of an msw survey. J Soc Work Educ. 2011;47(3):463–87. 10.5175/JSWE.2011.200900119 [DOI] [Google Scholar]
- 41.Peterson NA, Farmer AY, Donnelly L, Forenza B. Assessing the implicit curriculum in social work education: heterogeneity of students’ experiences and impact on professional empowerment. J Teach Soc Work. 2014;34(5):460–79. 10.1080/08841233.2014.955943 [DOI] [Google Scholar]
- 42.Afridi A, Sethi A, Ahmed F, Kashif L. Assessment of hidden curriculum during clinical rotations of year 4 mbbs students using hidden informal curriculum assessment tool (Hicat). J Med Sci Peshawar. 2020;28(4):352–5. 10.52764/jms.20.28.4.10 [DOI] [Google Scholar]
- 43.Haidet P, Kelly PA, Chou C, Communication C and culture study group . Characterizing the patient-centeredness of hidden curricula in medical schools: development and validation of a new measure. Acad Med J Assoc Am Med Coll. 2005;80(1):44–50. 10.1097/00001888-200501000-00012 [DOI] [PubMed] [Google Scholar]
- 44.Smith NA, Castanelli DJ. Measuring the clinical learning environment in anaesthesia. Anaesth Intensive Care. 2015;43(2):199–203. 10.1177/0310057X1504300209 [DOI] [PubMed] [Google Scholar]
- 45.Akcakoca B, Orgun F. Developing a measurement tool for evaluating the hidden curriculum in nursing education. Nurse Educ Today. 2021;97(ned, 8511379):104688. 10.1016/j.nedt.2020.104688 [DOI] [PubMed] [Google Scholar]
- 46.Al-Bawardy R, Blatt B, Al-Shohaib S, Simmens SJ. Cross-cultural comparison of the patient-centeredness of the hidden curriculum between a Saudi Arabian and 9 US medical schools. Med Educ Online. 2009;14((Al-Bawardy) Department of Medicine, School of Medicine and Health Sciences, The George Washington University, Washington, DC, USA.):19. 10.3402/meo.v14i.4655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Green AR, Rosu C, Kenison T, Nze C. Assessing the hidden curriculum for the care of patients with limited English proficiency: an instrument development. Educ Health Abingdon Engl. 2018;31(1):17–24. 10.4103/1357-6283.239042 [DOI] [PubMed] [Google Scholar]
- 48.Ludwig B, Turk B, Seitz T, Klaus I, Loffler-Stastka H. The search for attitude-a hidden curriculum assessment from a central European perspective. Wien Klin Wochenschr. 2018;130(3–4):134–40. 10.1007/s00508-018-1312-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kaldjian LC, Shinkunas LA, Reisinger HS, Polacco MA, Perencevich EN. Attitudes about sickness presenteeism in medical training: is there a hidden curriculum? Antimicrob Resist Infect Control. 2019;8(1):149. 10.1186/s13756-019-0602-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Butler J, Kassel L, Miesner AR, Grady S, Wall GC. Incidence of a negative hidden curriculum, cynicism, and burnout within pharmacy resident education: a nationwide survey. Curr Pharm Teach Learn. 2021;13(8):922–7. 10.1016/j.cptl.2021.06.001 [DOI] [PubMed] [Google Scholar]
- 51.Hafferty FW. Beyond curriculum reform: confronting medicine's hidden curriculum. Acad Med. 1998. Apr;73(4):403–7. 10.1097/00001888-199804000-00013 [DOI] [PubMed] [Google Scholar]
- 52.The Association of Faculties of Medicine of Canada A . The Future of Medical Education in Canada (FMEC). 2010. Available from: https://cou.ca/wp-content/uploads/2010/01/COU-Future-of-Medical-Education-in-Canada-A-Collective-Vision.pdf


