The African continent is a crucial part of the historical and current narrative of mpox. The first human case of mpox (then termed monkeypox) was detected in 1970 in the Democratic Republic of the Congo (DRC), long before the recent spread of the disease to other parts of the world. Although mpox has been on the African continent for over five decades, it only gained worldwide attention when it began spreading to high-income countries in Europe and North America1. This is reminiscent of the global neglect of Ebola virus disease in the DRC and Sudan in the mid-1970s, which only gained international attention during the 2014–2015 Ebola outbreak when cases were exported to high-income countries. As with Ebola, mpox is emblematic of the global neglect of diseases that are endemic to Africa, up until they threaten the health security of the Global North. Progress must be made to control this disease and gaps need to be addressed to achieve global health security.
In recent years, Africa has experienced an upsurge in mpox cases, raising concerns about the potential of the virus to cause larger outbreaks. From 1 January 2022 to 31 November 2023, a cumulative total of 91,788 laboratory-confirmed cases of mpox, including 167 deaths, were reported from 116 countries, territories or areas2, 13 of which are African Union Member States (Fig. 1). Africa accounted for over 80% of all deaths from mpox reported globally during this period, but more than 199 suspected mpox deaths from the DRC were not counted owing to a lack of laboratory capacity for confirmation2. As of 25 November 2023, the African continent has seen a more than 200% increase in deaths from mpox reported compared to the same period in the previous year3,4. This increase shows that Africa is still plagued with a high burden of mpox even after cases have reduced elsewhere. It is unclear whether case numbers from Africa were considered when the decision was made to declare the end of mpox as a global public health emergency of international concern (PHEIC).
Fig. 1 |. Map shows distribution of mpox cases in Africa in 2022 and 2023.
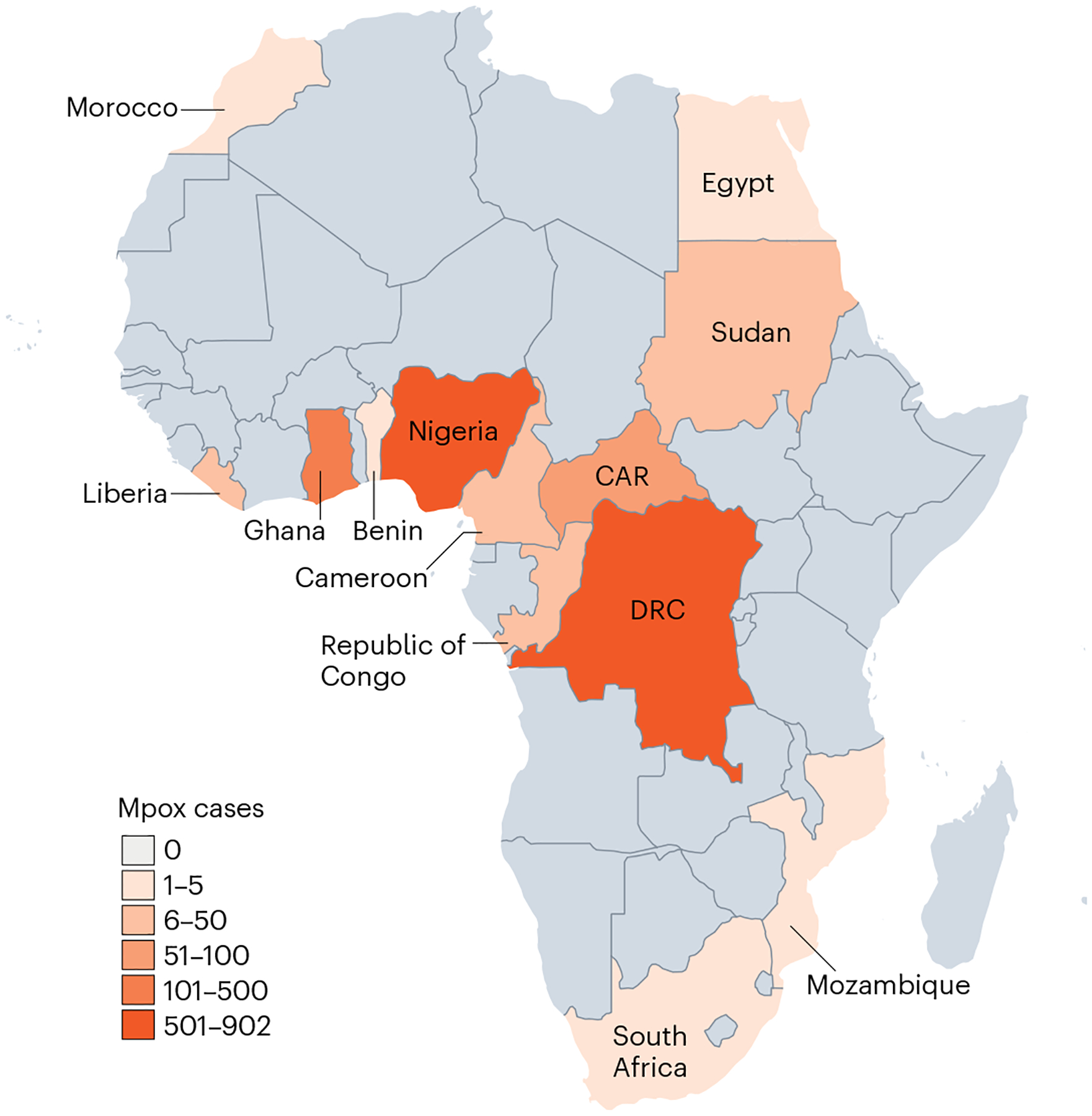
Laboratory-confirmed cases from 1 January 2022 to 25 November 2023. CAR, Central African Republic; DRC, Democratic Republic of the Congo.
Before the PHEIC was declared, Africa had registered several mpox outbreaks including the 2017 outbreak in Nigeria with 122 confirmed cases and 7 deaths (case fatality rate of 5.7%) from 17 states5. Similarly, between 2005 and 2007, at least 760 confirmed cases of mpox were reported from the DRC. Since then, the DRC has been reporting yearly increases in mpox cases (Table 1). Despite these high numbers, there was a global neglect of mpox outbreaks until the virus began spreading in the Global North (to access a more detailed dataset, please contact AfricaCDCEBS@africa-union.org).
Table 1 |.
Confirmed cases and deaths from mpox in Africa in 2022 (1 Jan–25 Nov) and 2023 (1 Jan–25 Nov)
| Confirmed cases | Deaths | |||
|---|---|---|---|---|
| 2022 | 2023 | 2022 | 2023 | |
| Benin | 3 | 0 | 0 | 0 |
| Cameroon | 18 | 27 | 3 | 0 |
| Republic of Congo | 8 | 67 | 2 | 2 |
| Central African Republic | 5 | 20 | 3 | 2 |
| DRC | 206 | 714 | 177 | 595 |
| Egypt | 2 | 0 | 0 | 0 |
| Ghana | 107 | 11 | 4 | 0 |
| Liberia | 3 | 10 | 0 | 0 |
| Morocco | 3 | 0 | 0 | 0 |
| Mozambique | 1 | 0 | 1 | 0 |
| Nigeria | 624 | 79 | 7 | 2 |
| South Africa | 5 | 0 | 0 | 0 |
| Sudan | 11 | 0 | 1 | 0 |
After the declaration of mpox as a PHEIC, global efforts focused on enhancing mpox surveillance and data sharing, accelerating vaccine development and deployment, providing financial and technical assistance to countries, and promoting access to mpox laboratory diagnostic kits and treatment interventions. These efforts led to enhanced surveillance with prompt laboratory confirmation of suspected cases in the Global North. However, these capacities were not homogenous globally, with countries such as the DRC reporting over 4,700 suspected cases yet only 270 confirmed cases in 2022, which indicates substantial gaps in laboratory capacity4. These capacity gaps made it challenging to compare the impacts of the outbreak across several countries, particularly in Africa. In addition, whereas other countries had access to stockpiles of vaccines to vaccinate health-care workers and high-risk groups, vaccines were not available to African countries during this period, further demonstrating a huge inequality in access1,6,7.
There is no doubt that the situation of mpox in Africa is deteriorating. On 23 November 2023, the World Health Organization (WHO) issued an outbreak news of the first cases of sexually transmitted clade I mpox virus in the DRC and the spread of mpox to new provinces in the country, which had not been reported during previous outbreaks8. This highlights the need for more in-depth investigation to better understand mpox transmission dynamics to guide controls and response plans. The ongoing outbreak also highlights the urgent need for enhanced surveillance, and equitable access to vaccines, diagnostics and treatments for all affected populations.
The mpox situation in Africa is worsening; attaining optimal global health security will entail a collaborative and collective effort. The spread of the disease from Africa to other parts of the world should lead to a renewed global commitment to foster a cooperative and coordinated agenda to strengthen health systems. Vulnerable populations worldwide must have access to life-saving interventions.
The African Union Commission (AUC) and Africa Centres for Disease Control and Prevention (Africa CDC) are making deliberate efforts by calling for a new public health order and advocating for governments as well as regional and global actors to support the full implementation of this initiative as a strategic step to attaining global health security9. This new order calls for: strengthening of African public health institutions; expanding local manufacturing of vaccines, diagnostics and therapeutics in the continent; investment in the public health workforce and leadership programs; increased domestic investment in health; and establishment and nurturing of equitable and effective partnerships.
Footnotes
Competing interests
The authors declare no conflict of interest.
References
- 1.Kirby T Lancet 402, 949–950 (2023). [DOI] [PubMed] [Google Scholar]
- 2.WHO. External situation report #30; https://go.nature.com/49LES7T (25 November 2023).
- 3.Africa CDC. Outbreak brief 26; https://go.nature.com/42UHONh (11 January 2023)
- 4.Africa CDC. Outbreak brief 16; https://go.nature.com/48IWgtj (27 October 2022)
- 5.Yinka-Ogunleye A et al. Lancet Infect. Dis 19, 872–879 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adetifa I, Muyembe JJ, Bausch DG & Heymann DL Lancet 401, 1822–1824 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ogunkola IO et al. Clin. Epidemiol. Glob. Health 22, 101313 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO. Disease outbreak news; https://go.nature.com/49MT00E (23 November 2023).
- 9.Africa CDC. Press release; https://go.nature.com/42Tdm64 (29 September 2022).


