Abstract
Introduction
Septic pulmonary embolism is a serious and rare complication of orbital cellulitis. Orbital infection usually arises from adjacent soft tissue or hematogenous infections.
Case
A 2-year-old girl presented with high-grade fever, cough, and bilateral eyelid swelling for 5 days preceded by edema and a perinasal facial skin furuncle. Examination revealed bilateral axial proptosis and orbital and thoracic CT bilateral orbital cellulitis, septic pulmonary embolism, and bilateral pneumothorax.
Discussion
A rare but potentially fatal complication of periorbital cellulitis is septic embolism, which carries a high rate of morbidity and mortality. The infections that cause orbital cellulitis can be transmitted to the orbit through dehiscence of the bone wall or through venous drainage. This can lead to septicemia and subsequent serious complications, including septic pulmonary embolism, Cavernous sinus thrombosis, meningitis, and cerebral ischemia. Advanced and timely imaging is crucial to diagnose both orbital cellulitis and its thoracal complications.
Conclusion
Early diagnosis of orbital cellulitis, timely investigations of its extracranial complications, and multidisciplinary involvement in patient management are crucial to prevent or treat complications such as septic pulmonary embolism and may improve patient prognosis.
Keywords: Septic pulmonary embolism, SPE, Orbital cellulitis, OC and Pneumothorax, PTX
Introduction
Orbital cellulitis, a serious infection of the postseptal tissues of the orbit, is one of the most common causes of orbital inflammation. Adolescents and children are the most affected.1,2 This condition is thought to occur as a result of spread of infection from the blood, the adjacent nasal sinuses, and facial skin.1,2
A septic pulmonary embolism can result from infectious material entering the circulation and becoming lodged in lung tissue, leading to local infections and abscesses. ”While septic pulmonary embolism most commonly derives from right-sided endocarditis, infection of cardiac implantable electronic devices, or thrombophlebitis of large veins,3 in rare cases it can be associated with orbital cellulitis.4 Herein, we present a rare case of bilateral orbital cellulitis causing Septic pulmonary embolism and subsequent bilateral pneumothorax.
Case Report
A 2-year-old girl presented to emergency department with 5 days of high grade fever, cough and bilateral eyelid swelling. Prior to the onset of this illness, there were edema and a perinasal face skin furuncle. She had previously been otherwise healthy.
Physical examination revealed a very ill girl with periorbital and facial edema, high-grade fever, increased respiratory rate, decreased SpO2, and chest crepitation.
An eye exam revealed swelling around the eyes on both sides. Both globes showed axial proptosis. Examinations also showed injection, purulent discharge in both eyes with slow-reacting pupils, severe conjunctival chemosis, and external ophthalmoplegia affecting the third, fourth, and sixth cranial nerves.
The vertical disk ratio of the right eye was 0.3, while that of the left eye was 0.4. There was no evidence of engorged retinal veins or disc edema.
Laboratory investigations showed a significantly high white blood cell count (WBC = 32,000 cells/mm3), low hemoglobin (5.5 mg/dL), and high C-reactive protein (112 mg/L). Blood culture was negative.
Orbital CT demonstrated extensive bilateral periorbital soft tissue thickening and facial subcutaneous edema (Figure 1). In addition; Contrast enhanced CT of thorax revealed Multiple peripheral located cavitary lesions in the bilateral lungs (Septic emboli) and associated bilateral moderate pneumothorax with consolidation areas with air bronchogram in the left lower lung of the lung (Figure 2).
Figure 1.

Axial non-contrast orbital CT: bilateral extensive periorbital soft tissue swelling and fat stranding (bilateral orbital cellulitis).
Figure 2.
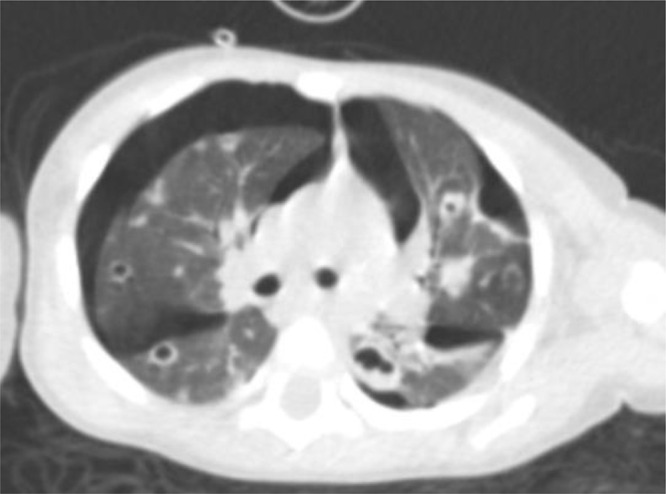
Axial thoracic CT demonstrated multiple peripherally located cavitary nodules in both lungs and moderate bilateral pneumothorax (septic pulmonary emboli complicated by pneumothorax).
The patient was admitted in the pediatric ICU and treatment was initiated with intravenous (IV) ceftriaxone 500mg 12 hourly, IV clindamycin 100mg 8 hourly, Voltaren eye drop 8 hourly, Lomefloxacin eye drop 12 hourly after an initial loading dose of one drop every 5 min for 25 min, chloramphenicol ointment nocte and oral ibuprofen syrup 8 hourly. Bilateral chest tube were inserted for pneumothorax decompression.
Her white blood cell count normalized and chest x ray was significantly improved. She was discharged from hospital after 15 days with orally administered antibiotic therapy (co_amoxiclav syrup 400mg) to be taken for one week.
Discussion
Orbital cellulitis is a common orbital disease, which is usually caused by the direct spread of a nearby infection and is more common in children than in adults.2 Orbital and periorbital soft tissue infections are serious conditions that require immediate treatment due to their potentially fatal consequences.1 These infections can be transmitted to the orbit through dehiscence of the bone wall or through venous drainage.1 Skin conditions such as eczema or facial cellulitis account for 16% of cases.4
Septic embolism is a rare but potentially fatal complication of periorbital cellulitis with a high morbidity and mortality rate.5 A septic embolism can result from infectious material moving through the bloodstream and becoming lodged in distant organs or tissues. This can lead to local infections or abscesses. Septic embolism due to periorbital cellulitis is a rare but potentially fatal disease.5
Septic pulmonary embolism (SPE) is a rare phenomenon caused by an infected thrombus migrating into the pulmonary vasculature, causing pulmonary embolism, focal pulmonary abscesses, and in some cases pneumothorax (PTX).6 Early recognition and appropriate treatment of periorbital cellulitis is crucial to prevent the development of septic embolism. Early implementation of an empirical antibiotic treatment is critical for controlling common pathogens including, but not limited to, Staphylococcus aureus and Streptococcus.5
The most common pathogens for non-hematogenous OC, also known as continuous spread OC, are Staphylococcus aureus, Streptococcus pneumoniae and Haemophilus influenzae. Anaerobic bacteria may also play a role in odontogenic infections causing OC.2 Pneumothorax is a rare but potentially fatal side effect of SPE that can occasionally occur on both sides. It is possible that an embolic bacterial cavity containing Staphylococcus aureus is the cause of the formation of a bronchopulmonary fistula.6,7 The prevalence of pneumothorax secondary to septic pulmonary embolism is only 3.4%, but the mortality rate is up to 28.2%.7
A rare consequence of SPE is secondary pneumothorax, which occurs seldom (3.4%) but has a very high in-hospital mortality rate (28.2%).1 Pneumothorax due to cavitation of nodular lesions can be caused by a number of mechanisms such as aseptic necrosis from compromised blood flow due to embolization, secondary infection due to bacterial embolization resulting from a check valve mechanism. As reported in a number of articles, infective endocarditis is the most common cause of SPE and secondary pneumothorax.7 Clinically, orbital cellulitis manifests itself as pain, proptosis, globe displacement, double vision and/or vision loss, chemosis and extraocular motility deficit (ophthalmoplegia).1
Radiologic findings, especially CT findings, are helpful in the differential diagnosis of SPE. Thoracic CT imaging is essential in septic pulmonary embolism diagnosis. Multiple nodular opacities are the most frequently seen radiographic signs, representing 66.42%, followed by cavitary lesions seen in 55.97%. In addition, local infiltrations, pleural effusions, feeding vessel signs, and peripheral wedge-shaped lesions are common findings.7
Radiological studies providing insight into intraorbital structures, such as contrast-enhanced CT and MIR, are essential to diagnose orbital cellulitis.They would have provided a clear picture of the changes within the orbit. Fever is as common as preseptal cellulitis in children (62%), while it may not occur in adults in 66% of cases.1 Early detection and treatment of periorbital cellulitis are essential to preventing major complications like SPE. Early initiation of empirical antibiotic therapy targeting the common causative pathogens, such as Staphylococcus aureus and Streptococcus species, is essential.5
Due to pulmonary lesions associated with SPE, the lung parenchyma is delicate and more susceptible to alveolopleural fistulas and pneumothorax at lower pressures than normal airway management. After the onset of a pneumothorax, patients undergoing mechanical ventilation should follow a conservative treatment plan that includes volume ventilation settings, limited airway pressure, and air drainage via one or more chest tubes.7
Conclusion
This case confirmed the rare but possible association of orbital cellulitis with potentially life threatening septic pulmonary emboli. To prevent fatal complications such as septicemia, septic pulmonary embolism, pneumothorax, cavernous thrombosis, meningitis, cerebral ischemia and death, a high index of suspicion for extracranial complications and a multidisciplinary treatment approach with aggressive antibiotics are required.
Ethical Approval
Institutional approval is not required for publication.
Consent from Patient Care Giver
Written informed consent was obtained from the patient’s care giver for the publication of this case reports and the accompanying images.
Disclosure
The authors report non-financial support from Mogadishu Somali Turk Hospital, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
- 1.Achigbu E, Achigbu K. Bilateral orbital cellulitis: a case report and management challenges. Niger J Ophthalmol. 2017;25(1):52. doi: 10.4103/0189-9171.207374 [DOI] [Google Scholar]
- 2.Xu-yuan T, Hui-yan L. A rare ocular complication of septicemia: a case series report and literature review. BMC Infect Dis. 2023;23(1):1–11. doi: 10.1186/s12879-023-08489-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Valerio L, Baddour LM. Septic Pulmonary Embolism: a Contemporary Profile. Semin Thromb Hemost. 2023;49(8):840–847. doi: 10.1055/s-0042-1758742 [DOI] [PubMed] [Google Scholar]
- 4.Allegrini D, Reposi S, Nocerino E, Pece A. Odontogenic orbital cellulitis associated with cavernous sinus thrombosis and pulmonary embolism: a case report. J Med Case Rep. 2017;11(1):1–4. doi: 10.1186/s13256-017-1309-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Restrepo Vanegas LC, Rojas Urrea A, Corredor Torres JM, García Agudelo L, Avellaneda Curcho LC. Septic embolism due to periorbital cellulitis caused by pimple drainage. Dermatology Rep. 2023. doi: 10.4081/dr.2023.9779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Montano M, Lee K, Patel K, Kioka M, Molnár Z. Septic Pulmonary Embolism Causing Recurrent Pneumothorax in an Intravenous Drug User without Right-Sided Valvular Vegetation in Infective Endocarditis. Case Reports Crit Care. 2021;2021:3–5. doi: 10.1155/2021/7050775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ikejiri K, Goto H, Usui M, et al. Septic pulmonary embolism and subsequent bilateral pneumothorax in patients undergoing chemoradiotherapy for head angiosarcoma: an autopsy case report and literature review. Med. 2022;101(45):E31755. doi: 10.1097/MD.0000000000031755 [DOI] [PMC free article] [PubMed] [Google Scholar]


