Abstract
Background
One of the contributing factors to the high maternal mortality rate is the failure of the referral system, which inhibits the management of obstetric emergencies. Health workers at primary healthcare facilities serve as the gatekeepers of this referral system, and they must be equipped to make referral decisions, prepare referrals, and transport women safely and quickly to the hospital.
Objective
This study aimed to explore the challenges faced by health workers in primary healthcare settings when implementing appropriate and rapid obstetric emergency referrals for women.
Methods
A descriptive qualitative study design was employed, utilizing in-depth interviews with open-ended questions directed at 12 midwives working in health centers and private clinics in urban and rural areas from January to March 2024. The collected data were analyzed manually using content analysis.
Results
Four themes were identified as challenges within the referral system: referral consent, pre-referral care ability, patient transfer to the hospital, and patient admission to the hospital. Factors that worsened the challenges for midwives in implementing obstetric emergency referrals were patients' perceptions of hospital care, the opinions of parents or family members, and levels of self-confidence. Additional factors included experience in emergency care, training, care guidelines, distance and travel time to the hospital, hospital refusals, patient handover mechanisms, and the attitudes of colleagues.
Conclusion
Midwives, as health workers in primary healthcare, are expected to be skilled in addressing various challenges due to their close relationships with women at the forefront of the referral system. Enhancing competence in basic obstetric emergency care, improving communication between health facilities, and encouraging community empowerment are essential. Therefore, effective referrals from these improvements would enable women to receive timely and comprehensive obstetric emergency care. This study provides a foundational framework for developing interventions in health facilities and the community to strengthen the referral system and reduce maternal mortality in Indonesia.
Keywords: Indonesia, referral, emergency medical services, midwifery, health facilities, maternal mortality, patient transfer, patient admission
Background
A reliable referral system can improve timely and appropriate access to quality emergency obstetric care and potentially reduce maternal morbidity and mortality (Adams et al., 2020). The World Health Organization (WHO) aims to provide at least 60% of the population with physical access to the nearest emergency obstetric health facilities within two hours of travel time to prevent avoidable maternal deaths (WHO, 2021). However, the current referral system has not effectively reduced maternal mortality rates, particularly in middle- and low-income countries (Ameyaw et al., 2020; Daniels & Abuosi, 2020). Indonesia has a high maternal mortality rate, ranking second among countries in Southeast Asia (ASEAN Secretariat, 2023). Meanwhile, the global referral system has been described by WHO as consisting of several interrelated components, including health systems, sender health facilities, recipient health facilities, referral practices, supervision, and capacity building, which help ensure the community receives the best care (WHO, 2007, as cited in Hort et al., 2019).
The referral system is structured in a pyramid-like manner, comprising primary, secondary, and tertiary health facilities. Primary health facilities provide Basic Emergency Obstetric Care (BEmOC), secondary health facilities deliver Comprehensive Emergency Obstetric Care (CEmOC), and tertiary health facilities, including provincial and national hospitals, offer the highest level of care (Ministry of Health, 2012). The government expects this referral system to enhance timely and appropriate access to quality emergency obstetric care to reduce maternal mortality effectively. Delays in referral are among the causes of maternal mortality because the referral system in Indonesia has not significantly improved access to CEmOC (Mahmood et al., 2021; Mahmood et al., 2018).
The three-delay model proposed by Thaddeus and Maine (1994) identifies barriers to obtaining effective interventions through health services to prevent maternal mortality. These delays include 1) deciding to seek help, 2) reaching the appropriate health facility, and 3) receiving adequate care at the health facility. The Indonesian Ministry of Health has established guidelines for referral procedures, which include patient/family consent, pre-referral care for stabilization, communication between health facilities, referral letters, transportation, patient reception, follow-up care, and referral feedback (Ministry of Health, 2012). Primary health facilities act as referral senders and bear significant responsibility, from preparing referrals to ensuring the patient is received at the hospital. However, not all facilities can perform these roles effectively due to the limited availability of medical equipment, medicines, staff, transportation resources, and barriers from women and the community (Hendarto et al., 2021).
Previous studies in Indonesia have highlighted the referral process as a contributing factor to maternal mortality (Anggondowati et al., 2022; Mahmood et al., 2021; Rambu Ngana & Eka Karyawati, 2021). However, only a few studies have specifically addressed the referral system, and even those have predominantly used quantitative research methods (Diba et al., 2019; Lubis & Ganap, 2023). While these studies provide information on the factors influencing the referral process based on the perceptions of health workers in hospitals, health centers, and private midwife clinics, they lack in-depth insights into the underlying causes of these factors or the specific challenges faced by health workers during the referral process.
Our study aimed to explore the challenges encountered by midwives at referral-sending health facilities, which serve as the entry point to the health system. The role of midwives as referral senders is crucial due to their responsibility to ensure that women receive appropriate and timely referrals to hospitals for optimal care. Providing a comprehensive understanding of the challenges faced by primary health workers is essential to identify barriers at the individual, community, health facility, and environmental levels, leading to more effective referrals. Improvements in the referral system will contribute to achieving Sustainable Development Goal 3, which focuses on ensuring healthy lives and promoting well-being for all ages, including reducing maternal deaths from preventable causes of pregnancy and childbirth (United Nations [UN], 2015).
Methods
Study Design
This study employed a qualitative descriptive design to comprehensively explore the behaviors, feelings, and experiences of midwives regarding the referral of women with obstetric emergencies from primary health facilities to secondary and tertiary health facilities (Doyle et al., 2020; Kim et al., 2017). Additionally, the report adheres to the Consolidated Criteria for Reporting Qualitative Research (COREQ) guidelines (Tong et al., 2007).
Participants
The study was conducted in a province in Sumatra, Indonesia, which has the highest number of maternal deaths compared to surrounding areas (Ministry of Health, 2024). The referral system is regulated by the government at the governor level, which includes the division of referral areas and the authority to provide Emergency Obstetric and Neonatal Services. Two regencies were intentionally selected based on their high maternal mortality cases in 2023 (Lampung Provincial Health Office, 2024). Both regencies were considered representative of the province’s topography: Regency A is an urban area, while Regency B is rural.
The study population consisted of health workers in primary health facilities in Regencies A and B. Purposive sampling was employed to select midwives who had referred patients to Regency government hospitals A and B between January and March 2024. The selection process began with a review of medical records at the hospitals to identify the sending health facilities. A total of 12 midwives from five health centers and seven private midwife clinics were selected as participants for in-depth interviews. The sample size was determined based on the saturation of responses provided by participants, which showed minimal variation (Saunders et al., 2018). During the study period, 12 referral cases involving obstetric emergencies were recorded, with five cases at Hospital A and seven at Hospital B.
Data Collection
Data were collected from January to March 2024 using the semi-structured in-depth interview method to explore the perspectives and thoughts of midwives regarding factors influencing the success of obstetric emergency referrals. Interviews were conducted face-to-face in the local counseling room using Indonesian, and no other participants were allowed to provide verbal or nonverbal responses during the process (Doyle et al., 2020). The interview guidelines were developed from a literature review exploring barriers to the referral process, with a focus on provider readiness (Alemayehu et al., 2022; Dzomeku et al., 2023; Mengist et al., 2024; Mselle et al., 2021). The questions included topics such as participant characteristics, referral preparation, patient/family consent, pre-referral care, hospitalization, hospital admission, and outcomes of the referral process.
Before the study, a pilot interview was conducted to develop the questions and refine communication skills. The results were discussed with the research team to refine the initial guidelines further and determine effective communication methods for the in-depth interviews. The interview guidelines were presented in Indonesian to match the language used by the participants.
In-depth interviews were conducted by the first investigator, a master’s degree graduate in midwifery who works as a lecturer at a health college, has a certificate in obstetric emergency care and has no prior relationship with the participants. A total of 12 interviews were conducted using a voice recorder, an Android smartphone, stationery, and field note sheets. The interviewer established rapport with the participants and explained the study's purpose, procedures, and benefits. Participation was voluntary, and participants were allowed to withdraw from the study at any time until the data analysis was completed.
After receiving an explanation of the study, participants signed a consent form, and the interviews lasted between 30 and 45 minutes without repetition. During the interviews, all processes were documented, including responses to questions, verbal and nonverbal communication, and key phrases used by participants. The data were discussed with the research team and considered saturated when the ninth participant was reached; however, interviews continued until a total of 12 participants were included.
Data Analysis
Content analysis using an inductive approach was conducted manually by re-reading the transcripts, taking notes, and understanding the text. This analysis followed Lundman’s guidelines (Graneheim & Lundman, 2004). The first step involved an in-depth interpretation of the text content by systematically grouping codes, resulting in a total of 97 codes. The second step included identifying patterns and condensing the collected data without losing quality. Data coding and analysis were performed manually using an inductive method. The main themes derived from the selected interview results effectively described the various themes and sub-themes, reflecting the most frequently stated by different participants.
Trustworthiness
The trustworthiness of this study was evaluated based on credibility, transferability, and confirmability (Lincoln & Guba, 1985). The credibility of the findings was assessed through data triangulation and participant examination. Data triangulation involved reviewing medical records and interviewing referral-receiving officers at the hospital, which included collecting information on diagnoses, pre-referral care, referral consent documents, letters, accompanying health workers, and financing. Meanwhile, participant examination was conducted by reviewing the recordings of the interviews before concluding each session, which helped verify the interviewer's understanding of the information provided. Transferability was evaluated by comprehensively describing the context, participants, and situations to enable readers to assess whether the findings could be applied to similar cases. Confirmability was ensured through an audit trail, which documented each step of the study, including decisions and data analysis. Peer reviews from discipline and midwifery professional organizations representatives were solicited to correct or add information supporting the research findings. All participants agreed on the concluded themes and sub-themes, while the experts convened to discuss the results and the necessity for further data collection and analysis. After thoroughly evaluating the various reviews, the experts reached a consensus on the formulated themes and sub-themes.
Ethical Considerations
Ethical review and approval, with the reference number KET-6/UN2.F10.D11/PPM.00.02/2024, were obtained from the ethics review board of the University of Indonesia on 10 January 2024. Ethical guidelines were strictly followed throughout the study. Participants had the autonomy to engage or withdraw from participation at any time and the right to refuse to answer questions or express opinions during the interviews. Informed consent was obtained from participants after explaining the background, objectives, benefits, procedures, risks, confidentiality, and compensation associated with the study.
Results
Table 1 presents the midwives aged between 27 and 56 years, with most holding a diploma qualification. Over half have more than 20 years of working experience. The majority of them work in private midwife clinics, and a significant number of them are based in rural areas. Only a smaller number have a professional qualification.
Table 1.
Characteristics of the participants
| Participant No. | Age | Education | Working Period | Workplace | Area |
|---|---|---|---|---|---|
| 1 | 45 | Diploma | 25 | Public Health Center | Rural |
| 2 | 40 | Profession | 22 | Public Health Center | Rural |
| 3 | 36 | Diploma | 12 | Private Midwife Clinic | Rural |
| 4 | 44 | Diploma | 23 | Private Midwife Clinic | Rural |
| 5 | 35 | Diploma | 11 | Private Midwife Clinic | Rural |
| 6 | 27 | Profession | 6 | Private Midwife Clinic | Urban |
| 7 | 56 | Diploma | 32 | Public Health Center | Urban |
| 8 | 50 | Diploma | 25 | Public Health Center | Urban |
| 9 | 40 | Diploma | 5 | Private Midwife Clinic | Urban |
| 10 | 50 | Diploma | 27 | Public Health Center | Rural |
| 11 | 49 | Diploma | 21 | Private Midwife Clinic | Rural |
| 12 | 47 | Diploma | 18 | Private Midwife Clinic | Rural |
Four main themes and corresponding sub-themes were identified from the data transcripts based on the participants' experiences in referring women with obstetric complications. These themes included Referral Consent, Pre-referral Care Ability, Patient Transfer to the Hospital, and Patient Admission to the Hospital (see Table 2).
Table 2.
Themes and sub-themes of challenges in obstetric emergency referrals
| Themes | Sub-themes |
|---|---|
| Referral Consent | Women’s concerns about surgery and the care process |
| Slow family consent | |
| Pre-Referral Care Ability | Lack of confidence in providing pre-referral care |
| Lack of emergency care experience | |
| Absence of standardized pre-referral care guidelines | |
| Patient Transfer to The Hospital | Complicated referral information system |
| The importance of establishing a relationship with an obstetrician at the hospital | |
| Damaged road conditions prolong travel time | |
| Patient Admission to The Hospital | Hospital refusal |
| Long waiting time for patient handover | |
| Unfriendly attitude of hospital staff |
Theme 1: Referral Consent
Obtaining patient consent for referral is the initial step in the referral process. Both the husband and wife hold the primary authority to decide whether to proceed with a referral, but making this decision can be challenging. The length of time required to make this decision was reported as one of the various obstacles encountered in the referral process. Women’s reluctance to accept referrals often was due to concerns about care, such as surgery. These concerns were related to issues such as the unfamiliar conditions of the operating room and equipment, the pain associated with surgical wounds, the unfriendly attitudes of hospital staff, and the overall environment of the treatment room. Many women expressed a desire to give birth in healthcare facilities near their homes despite the potential risks and consequences, including the risk of death.
“I explained that her condition does not allow for treatment here; therefore, she must be referred to the hospital, but she refuses. Her perception is that she will have surgery, which creates fear about the process of treating and healing the surgical wound. She worries about the wound bleeding, festering, stitches coming loose, prolonged pain, and the lengthy healing process. Women cannot immediately return to working in the fields, doing housework, or caring for children.” (Participant 5)
These expressed worries and fears often led participants to seek assistance from close family members to help convince patients that the referral decision was appropriate. Additional considerations mentioned by participants included the lack of funds for treatment and transportation.
“The husband fears being blamed by the family if something happens to his wife and baby. They contact their in-laws or parents to ask for their opinions. Furthermore, their parents consult some of their relatives.” (Participant 5)
“The woman came accompanied only by her younger sibling, older sibling, or even a neighbor while her husband was working out of town. She had difficulty contacting her husband, and there was no delegation of authority to make decisions on her behalf to her closest family members.” (Participant 7)
Theme 2: Pre-referral Care Ability
Pre-referral care aims to stabilize patients as an initial rescue effort; therefore, health workers need to be competent in handling early emergencies. This competency is crucial to ensure the safety and stability of patients until they arrive at the hospital. However, a lack of experience and training can lead to low confidence in providing effective pre-referral care.
“There is panic and fear when the patient is bleeding, especially if the blood is flowing heavily. I only put in an IV and give oxytocin. I also ask the family to give the mother something to drink and keep talking to her. As soon as possible, the mother is taken to the nearest hospital. I am not confident performing bimanual compression or uterine exploration because I have never done it before.” (Participant 12)
“If a patient experiences complications, I immediately call a senior midwife in this area. I have only been practicing for six years, so I am not confident in managing a patient with complications.” (Participant 6)
“In my place, the stock of emergency medications is limited. I only have oxytocin and IV fluids. Moreover, I do not feel confident using other medications. Besides, the hospital is nearby, so the patient is taken there directly.” (Participant 8)
The findings indicated that the absence of guidelines for stabilization care and a lack of clarity regarding the division of care responsibilities in the area are obstacles in the referral process. Existing care guidelines are sourced from books or training seminars attended by health workers, but there have been no meetings or socializations to discuss these guidelines.
“I provide care based on lessons learned during my midwifery education. I do not know the boundaries of authority between care in midwifery practice and hospitals. In my area, there are no emergency care guidelines for primary health facilities issued by the government or agreed upon.” (Participant 11)
Theme 3: Patient Transfer to the Hospital
Before transferring a patient to the hospital, the sending health facilities must communicate with the receiving health facilities. The government has developed an integrated referral system application to facilitate this communication. However, several obstacles hinder the process, including slow response times from recipient health facilities, unstable internet connections, a lack of staff available 24 hours a day, and the failure to include all primary health facilities in the referral information system.
“The referral information system makes the process longer. There are only 1-2 administrative staff, sometimes unavailable. The fastest response from the hospital is 10-15 minutes, but it can also take up to 4 hours. We get scolded if we take patients to the hospital without inputting data into the information system. We argue that emergency patients cannot wait that long… they could get worse and die.” (Participant 1)
“We live in the mountains, and it is difficult to get an internet signal. The referral information system requires a stable internet connection. Just inputting data can take 15 minutes or more; therefore, we contact the hospital by phone. Although we still input data into the referral information system afterward, it is a requirement for patient documents that are participants in the national health insurance.” (Participant 10)
Close relationships with obstetricians or hospital staff were reported to expedite the referral process. Rejections were rare when the sender informed the hospital that approval had been received from an obstetrician. The handover process was also faster because the staff asked fewer questions and immediately began providing treatment.
“If we already know and call the obstetrician at the hospital, the patient will not be rejected. As the senders, we are also not scolded, and the patient receives prompt treatment. Everything becomes easier if we call the obstetrician directly.” (Participant 4)
External environmental factors were also reported to slow patient transfers, particularly damaged road conditions that extended travel time. Many rural areas experienced varying degrees of road damage, and transportation infrastructure development lacked even distribution.
“Almost every part of the road has holes ranging from small to large and deep. The government has not repaired the roads for a long time. Accidents are prone to happen during the rainy season.” (Participant 3)
“The area here is mountainous, and not all roads are in good condition. In rural areas, residents go down the mountains using motorbikes with wheels wrapped in chains. However, people here help each other when someone needs to be taken to the health center or hospital, such as carrying patients together to roads that can be accessed by cars or lending their cars for free. We usually reach the hospital in about 1-2 hours.” (Participant 5)
Theme 4: Patient Admission to the Hospital
The sending health facilities were responsible for safely delivering women to the hospital, after which the responsibility shifted to the receiving health facilities. This process should not take long, as the next treatment steps fall under the jurisdiction of the receiving health facilities, including the availability of treatment rooms.
“I was once held up in the hospital emergency room for up to 3 hours and was not allowed to leave until the patient received confirmation of a treatment room. Even though the handover process had been completed, with referral letters and other documents provided and interviews conducted regarding the patient’s condition and treatment, I was asked to wait until a treatment room became available. If one was unavailable, I had to look for another hospital.” (Participant 12)
The findings indicated that the demeanor of the hospital emergency room staff, who were often unfriendly and tended to blame colleagues, instilled fear among staff accompanying the referrals. The staff felt harassed and unappreciated in front of patients and their families; however, they received support from patients by expressing empathy and not blaming the referral companion.
“I was blamed by the hospital emergency room staff regarding the care provided before the referral. Even though I had given the best care possible, it was still wrong. However, not all hospitals are like that; some do not place blame on the sender.” (Participant 8)
“The unfriendly attitude of the hospital staff made me afraid to accompany referred patients. I know they have extensive experience in emergency care, but they should understand our conditions in rural areas, where facilities and experience in handling obstetric emergencies are limited. We were once scolded in front of patients and their families, which made us feel embarrassed and disrespected as colleagues.” (Participant 9)
Discussion
Summary of the Findings
The results revealed that primary health facilities did not effectively implement the referral system due to significant challenges, including obtaining referral approval, providing pre-referral care, transferring patients to hospitals, and managing hospital admissions. These challenges were caused by various factors, including community influences (women, family, and community members), individual factors (confidence, care experience, and training), health system limitations (equipment, medications, staffing, guidelines, and policies), and environmental factors (transportation and telecommunications).
The first theme, referral consent, is influenced by women’s concerns about hospital care and delays from family members. Fears surrounding surgery, blood donations, and other medical procedures—such as the unfamiliarity of medical equipment, the stressful atmosphere of the operating room, pain from surgical wounds, and the complexities of wound care—contributed to delays in obtaining referral approval. These findings align with previous studies that highlighted the slow pace of women’s consent in the referral process due to perceptions of surgery or blood donation (Proos et al., 2020; Tabong et al., 2021). It is essential to provide information about hospital treatment processes to alleviate concerns about surgery, pain, lengthy healing processes, and disruptions to daily activities. Moreover, referral decisions are often contingent upon family approval, particularly from the husband (Shah et al., 2020). If the husband works out of town and faces communication difficulties in obtaining consent, there is often no delegation of authority to make decisions. Additionally, the husband may fear being blamed for not seeking permission from parents or consulting other family members. This observation corresponds with other studies indicating that social influences, such as cultural norms and family dynamics, frequently delay access to health services (Barua et al., 2022; Dempsey et al., 2021).
The lack of knowledge regarding the urgency of seeking immediate care and women’s limited autonomy in decision-making can be attributed to prevailing cultural norms and beliefs. Other studies support this, indicating that women often lack the autonomy to make healthcare decisions due to harmful cultural practices (Rajbanshi et al., 2021; Sialubanje et al., 2015). Therefore, it is vital to provide education during pregnancy to enhance women’s understanding, fostering a positive perception of the care process and preparing them to confront potential complications. Educating husbands, families, and the community about women’s autonomy, prenatal care, obstetric complications, and childbirth preparation is expected to promote positive health behaviors and prevent delays in seeking emergency care.
The second theme is pre-referral care, which aims to stabilize patients' conditions and ensure they remain stable during transit to the hospital. Health workers in primary health facilities must possess adequate skills in emergency management to save patients, supported by the availability of necessary equipment and medications. Competent healthcare professionals and sufficient material resources are crucial indicators for enhancing the quality of maternal health services and preventing maternal deaths (WHO, 2017).
The low confidence among midwives in providing emergency care, particularly for postpartum hemorrhage resulting from uterine atony and severe lacerations of the birth canal, contributes to this issue. In such cases, timely intervention is critical, as bleeding requires prompt action—ideally within two hours—to prevent postpartum women from experiencing shock or death (WHO, 2009). Village midwives often work without assistants, necessitating collaboration with families during emergencies to save patients' lives. While fellow midwives from nearby areas may be called upon for assistance, there is still a delay as they travel to the health facilities. This lack of confidence is often rooted in insufficient experience with emergency care and a failure to enhance knowledge through training or further education. Similar studies have shown that midwives in middle-income countries often lack knowledge of emergency management (Hobbs et al., 2019). Reports have indicated that staff shortages and inadequate training contribute to the inability to provide quality emergency obstetric care (Bewket et al., 2022).
According to authorities, other contributing factors include the absence of equipment, medications, and clear care guidelines. In practice, there is limited availability of magnesium sulfate for treating women with pre-eclampsia and size 16 or 18 cannulae (Abocath) for severe postpartum hemorrhage. These shortages arise from challenges in obtaining essential drugs and medical supplies from local pharmacies, coupled with a lack of supervision over expired drug inventories. These findings align with other studies that have reported inadequate equipment and medication as significant factors hindering timely and appropriate care for women (Mahmood et al., 2018; Mashamba & Ramavhoya, 2021; Mgawadere et al., 2017; Mohammed et al., 2020; Muthoni et al., 2021).
The third theme is the transfer to the hospital, which necessitates initial communication between the sending and receiving health facilities to ensure the availability of space, readiness of the emergency team, and access to equipment and medications. Various communication methods, including telephone calls, letters, and internet-based applications, can be utilized. In Indonesia, the government has established an integrated referral information system to facilitate communication between health facilities and expedite the referral process.
However, the results indicated that the referral information system often hinders the referral process due to the lengthy response times from hospitals. Delays are primarily caused by operators needing to consult with senior doctors, who sometimes do not provide immediate answers regarding the availability of treatment, operating, and ICU rooms, along with other necessities. As a result, senders frequently make telephone calls to refer patients, which complicates matters for hospitals, as using the referral information system is a requirement for national health insurance participants.
Other studies have also identified barriers to using this referral information system, including long response times, unstable internet connections, and limited staffing (Irianto et al., 2021; Legawati et al., 2024). Inadequate communication prior to referral has led to patient rejections at hospitals due to insufficient bed availability, lack of medical equipment, or the unpreparedness of the medical team. Such rejections often result in patients needing to visit two or three hospitals before finding one capable of accepting and providing treatment. Previous research has similarly reported that patient rejections at hospitals cause delays in referrals and worsen maternal outcomes, such as death during transit or upon arrival at the hospital (Alobo et al., 2021; Ayebare et al., 2021; Nabulo et al., 2023).
The fourth theme highlights the need for midwives to facilitate the admission of patients to the hospital through a lengthy and complicated handover process following successful transportation. Health workers accompanying referred patients may spend up to four hours solely on the handover process, waiting for patients to be transferred to a treatment room. This handover mechanism involves providing information about the patient’s condition previous treatment, and submitting relevant treatment documents. All necessary information should be documented in the referral letter at the sending health facility, allowing hospital staff to read and study it beforehand.
However, staff in the hospital emergency unit often ask numerous questions with an unfriendly attitude, tending to blame the sending health facilities. This behavior creates fear among those accompanying referrals. Previous research has reported that midwives are reluctant to accompany maternal referrals due to harassment from their colleagues. Instead of offering support and constructive feedback, staff often blame pre-referral care for being inappropriate or leading to misdiagnoses (Kanyesigye et al., 2022). Studies have indicated that unfriendly attitudes among hospital staff and attempts to interrogate midwives from sending health facilities contribute to disharmony in colleague relationships (Garti et al., 2023; Ximba et al., 2021).
Challenges in the admission process could be mitigated if there were clear guidelines on standardized and mutually agreed-upon referral and pre-referral care mechanisms. Other research has indicated that the lack of referral and care guidelines acts as a barrier to emergency care provision and contributes to delays in referrals (Ekawati et al., 2020; Ximba et al., 2021). One of the most distressing issues reported is patient rejection, which leads to searching for alternative hospitals and extends the referral time, whereas patients experiencing emergencies require prompt treatment to prevent fatalities. The primary reasons given by hospitals for rejecting patients include inadequate equipment and a shortage of treatment beds (Alobo et al., 2021; Banke-Thomas et al., 2020). If hospitals were to meet the infrastructure, equipment, and medication requirements according to their classification, such rejections would likely be minimized (USAID & Ministry of Health, 2019). Furthermore, these rejection incidents contradict existing laws that state, “Health service facilities owned by the Central Government, Regional Government, and the community are required to provide health services for people in emergency conditions to prioritize saving lives and preventing disability” (Government of Indonesia, 2009).
Determinants of the Obstetric Emergency Referral System
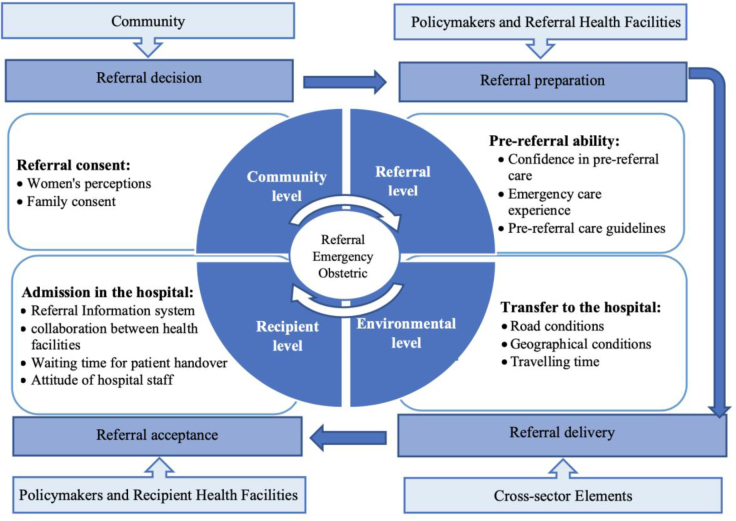
The results of this study revealed that health workers face challenges in implementing obstetric emergency referrals at multiple stages, including referral preparation, delivery, and acceptance. These challenges manifest at various levels—community, health facility, and environmental—which align with the theory of determinants for successful referrals in obstetric emergencies. This theory is the foundation for the obstetric emergency referral system, guided by the WHO's “referral system” framework (WHO, 2007, as cited in Hort et al., 2019). Each level includes numerous factors that contribute to the overall referral process (Figure 1).
Figure 1.
Determinants of the Obstetric Emergency Referral System [Developed by the authors, adapted from (WHO, 2007, as cited in Hort et al., 2019)]
The successful referral of obstetric emergencies must consider factors at each level, as an effective referral system is supported by five key components: sending health facilities, receiving health facilities, policymakers, the community, and cross-sector elements (Hort et al., 2019). Policymakers are responsible for designing policies, creating guidelines, allocating funds, supplying materials and competent human resources, establishing referral information systems, and facilitating cooperation among healthcare facilities. Participants in the referral process, specifically sending and receiving health facilities, must adhere to referral procedures, including referral preparation, delivery, and acceptance. Meanwhile, the community should actively engage in health-seeking behaviors by fostering a positive perception of health, encouraging timely referral agreement, and promoting community empowerment. Additionally, cross-sector elements are crucial in creating an environment that facilitates access to health services, such as transportation and telecommunications. In Indonesia, the referral system can benefit from considering factors at the individual, community, health facility, and environmental levels, as the active involvement of all components in the referral system is expected to reduce delays and prevent maternal deaths.
Strengths and Limitations
This study investigated the challenges faced by primary healthcare providers in conducting emergency obstetric referrals. It is the first research to comprehensively explore challenges ranging from referral preparation to patient admission, highlighting emergency care efforts at the forefront of the health system. However, a limitation of this study is that it is confined to the context of one province among the 38 provinces in Indonesia.
Implications of the Study
The findings of this study have direct implications for maternal health services in Indonesia, as rapid and appropriate obstetric emergency care is essential to preventing maternal deaths. Midwives, as primary health facility workers, act as gatekeepers to the health system, and the care they provide to women is crucial for saving lives. The challenges and inhibiting factors identified in this study require immediate attention from policymakers and service providers to avoid delays in referrals that negatively impact maternal health. To strengthen primary health services, there needs to be a focus on increasing the availability of competent human resources, adequate facilities, equipment, and medications. Furthermore, collaboration among health service facilities, advancements in information technology, and support from the community and other sectors are necessary to improve access to obstetric emergency services.
Conclusion
The results of this study indicate that the challenges faced by health workers in saving mothers are influenced by community, environmental, and health system factors. Issues such as unclear divisions of authority between health facilities, insufficient opportunities for health workers to enhance their competencies through training, an ineffective referral system, and a lack of cooperation between health facilities were identified as systemic factors. From a community perspective, the lack of educational initiatives during pregnancy to raise awareness about obstetric complications also affects referral consent. Environmental conditions, such as poor road conditions and lengthy travel times, further impact access to health facilities. Therefore, this study highlights the causes of high maternal mortality due to delayed referrals, providing a basis for the government to develop interventions that strengthen the maternal referral system in Indonesia.
Acknowledgment
The authors would like to thank the midwives at the Public Health Centers and Private Midwife Clinics who took the time to conduct interviews for this research. Next, we thank the provincial health department and district hospitals for granting permission for data collection.
Funding Statement
Funding None.
Declaration of Conflicting Interest
The authors declared no conflict of interest.
Authors’ Contributions
Novita Rudiyanti contributed to conceptualization, methodology, validation, and writing – original draft preparation, review and editing. Budi Utomo contributed to conceptualization, formal analysis, methodology, supervision, visualization, writing – review and editing. All authors approved the final version of the article to be published.
Authors’ Biographies
Novita Rudiyanti, S.ST, M.Kes, is a PhD student in public health at the Universitas Indonesia and a Lecturer at the Tanjung Karang Ministry of Health Polytechnic, Lampung, Indonesia.
Prof. dr. Budi Utomo, MPH., Ph.D, is a Professor in the Department of Biostatistics and Population, Faculty of Public Health, Universitas Indonesia, Depok, Indonesia.
Data Availability
The data collected and analyzed during this research is not publicly available but is available from the corresponding author upon reasonable request.
Declaration of Use of AI in Scientific Writing
None to declare.
References
- Adams, A. M., Ahmed, R., Ahmed, S., Yusuf, S. S., Islam, R., Zakaria Salam, R. M., & Panciera, R. (2020). Modelling improved efficiency in healthcare referral systems for the urban poor using a geo-referenced health facility data: the case of Sylhet City Corporation, Bangladesh. BMC Public Health, 20, 1476. 10.1186/s12889-020-09594-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alemayehu, M., Yakob, B., & Khuzwayo, N. (2022). Barriers and enablers to emergency obstetric and newborn care services use in Wolaita Zone, Southern Ethiopia: A qualitative case study. BMC Public Health, 22(1), 2087. 10.1186/s12889-022-14504-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alobo, G., Ochola, E., Bayo, P., Muhereza, A., Nahurira, V., & Byamugisha, J. (2021). Why women die after reaching the hospital: A qualitative critical incident analysis of the ‘third delay’in postconflict northern Uganda. BMJ Open, 11(3), e042909. 10.1136/bmjopen-2020-042909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ameyaw, E. K., Njue, C., Tran, N. T., & Dawson, A. (2020). Quality and women’s satisfaction with maternal referral practices in sub-Saharan African low and lower-middle income countries: A systematic review. BMC Pregnancy and Childbirth, 20, 682. 10.1186/s12884-020-03339-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anggondowati, T., Deviany, P. E., Latief, K., Adi, A. C., Nandiaty, F., Achadi, A., Kalter, H. D., Weaver, E. H., Rianty, T., & Ruby, M. (2022). Care-seeking and health insurance among pregnancy-related deaths: A population-based study in Jember District, East Java Province, Indonesia. PloS One, 17(3), e0257278. 10.1371/journal.pone.0257278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- ASEAN Secretariat . (2023). ASEAN Statistical Yearbook 2023. https://asean.org/book/asean-statistical-yearbook-2023/
- Ayebare, E., Ndeezi, G., Hjelmstedt, A., Nankunda, J., Tumwine, J. K., Hanson, C., & Jonas, W. (2021). Health care workers’ experiences of managing foetal distress and birth asphyxia at health facilities in Northern Uganda. Reproductive Health, 18, 29. 10.1186/s12978-021-01083-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banke-Thomas, A., Balogun, M., Wright, O., Ajayi, B., Abejirinde, I.-O. O., Olaniran, A., Giwa-Ayedun, R. O., Odusanya, B., & Afolabi, B. B. (2020). Reaching health facilities in situations of emergency: Qualitative study capturing experiences of pregnant women in Africa’s largest megacity. Reproductive Health, 17, 145. 10.1186/s12978-020-00996-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barua, M., Chowdhury, S., Saha, A., Mia, C., Sajow, S. H., & Sarker, M. (2022). Community-based referral transportation system for accessing emergency obstetric services in the Rohingya refugee camp during the COVID-19 pandemic in Bangladesh: Facilitators and barriers through beneficiaries’ and providers’ lens using a mixed-method design. Conflict and Health, 16(1), 51. 10.1186/s13031-022-00485-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bewket, T., Ensieh, F., Virginia, P., & Gayle, M. (2022). Barriers to effective management of primary postpartum haemorrhage following in-hospital births in northwest Ethiopia: Healthcare providers’ views using a qualitative approach. BMC Pregnancy and Childbirth, 22(1), 755. 10.1186/s12884-022-05071-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniels, A. A., & Abuosi, A. (2020). Improving emergency obstetric referral systems in low and middle income countries: A qualitative study in a tertiary health facility in Ghana. BMC Health Services Research, 20, 32. 10.1186/s12913-020-4886-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dempsey, A., Sripad, P., Sultana, K., Kirk, K., Hossain, S. M. I., & Warren, C. (2021). Pathways to service access for pre-eclampsia and eclampsia in rural Bangladesh: Exploring women’s care-seeking. PloS One, 16(2), e0245371. 10.1371/journal.pone.0245371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diba, F., Ichsan, I., Muhsin, M., Marthoenis, M., Sofyan, H., Andalas, M., Monfared, I., Richert, K., Kaplan, L., & Rogge, L. (2019). Healthcare providers’ perception of the referral system in maternal care facilities in Aceh, Indonesia: A cross-sectional study. BMJ Open, 9(12), e031484. 10.1136/bmjopen-2019-031484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doyle, L., McCabe, C., Keogh, B., Brady, A., & McCann, M. (2020). An overview of the qualitative descriptive design within nursing research. Journal of Research in Nursing, 25(5), 443-455. 10.1177/1744987119880234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dzomeku, V. M., Mensah, A. B. B., Nakua, E. K., Agbadi, P., Okyere, J., Kumah, A., Munukpa, J., Ofosu, A. A., Lockhart, N., & Lori, J. R. (2023). Perspectives of healthcare workers on the challenges with obstetric referrals in rural communities in Ghana: A descriptive phenomenology study. BMJ Open, 13(4), e066910. 10.1136/bmjopen-2022-066910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekawati, F. M., Emilia, O., Gunn, J., Licqurish, S., & Lau, P. (2020). The elephant in the room: An exploratory study of hypertensive disorders of pregnancy (HDP) management in Indonesian primary care settings. BMC Family Practice, 21(1), 242. 10.1186/s12875-020-01303-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garti, I., Gray, M., Bromley, A., & Tan, B. (2023). A socioecological description of the influencing factors to midwives’ management of preeclampsia in a Ghanaian tertiary hospital. PloS One, 18(9), e0291036. 10.1371/journal.pone.0291036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government of Indonesia . (2009). Legislative Regulations Number 44 of 2009 concerning Hospitals. Retrieved from https://peraturan.bpk.go.id/Details/38789/uu-no-44-tahun-2009
- Graneheim, U. H., & Lundman, B. (2004). Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Education Today, 24(2), 105-112. 10.1016/j.nedt.2003.10.001 [DOI] [PubMed] [Google Scholar]
- Hendarto, H., Dharmayanti, H. E., Winardi, B., Budi Prasetyo, B., Laksana, M. A. C., Yusuf, M., Pranadyan, R., Habibie, P. H., Trijanto, B., & Dewi, E. R. (2021). Suboptimal care on maternal near-miss cases: A study from a tertiary hospital in East Java, Indonesia. Journal of International Dental and Medical Research, 14(4), 1727-1735. [Google Scholar]
- Hobbs, A. J., Moller, A.-B., Kachikis, A., Carvajal-Aguirre, L., Say, L., & Chou, D. (2019). Scoping review to identify and map the health personnel considered skilled birth attendants in low-and-middle income countries from 2000–2015. PloS One, 14(2), e0211576. 10.1371/journal.pone.0211576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hort, K., Gilbert, K., Basnayaka, P., & Annear, P. L. (2019). Strategies to strengthen referral from primary care to secondary care in low- and middle-income countries (Vol. 6). New Delhi: World Health Organization Regional Office for South-East Asia. https://iris.who.int/bitstream/handle/10665/325734/9789290227090-eng.pdf?sequence=1&isAllowed=y [Google Scholar]
- Irianto, S. E., Djamil, A., & Aryono, A. C. (2021). Lessons learned of the implementation of an integrated referal system at the general hospital. Jurnal Peduli Masyarakat, 3(4), 527-542. [Google Scholar]
- Kanyesigye, H., Ngonzi, J., Mulogo, E., Fajardo, Y., & Kabakyenga, J. (2022). Health care workers’ experiences, challenges of obstetric referral processes and self-reported solutions in South Western Uganda: Mixed methods study. Risk Management and Healthcare Policy, 15, 1869-1886. 10.2147/RMHP.S377304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, H., Sefcik, J. S., & Bradway, C. (2017). Characteristics of qualitative descriptive studies: A systematic review. Research in Nursing & Health, 40(1), 23-42. 10.1002/nur.21768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lampung Provincial Health Office . (2024). Health Profile 2023 Lampung Provincial Health Office. Lampung: Lampung Provincial Health Office. [Google Scholar]
- Legawati, L., Utama, N. R., Purba, M. M., Yeyentimalla, Y., Aryani, V. D., & Nurfianto, S. (2024). The effectiveness of the Integrated Referral System (SISRUTE) on obstetrics and neonatal referral indicators at RSUD dr. Doris Sylvanus Palangka Raya. Formosa Journal of Science and Technology, 3(3), 491-498. 10.55927/fjst.v3i3.8617 [DOI] [Google Scholar]
- Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic inquiry. California: Sage Publications. [Google Scholar]
- Lubis, I. S., & Ganap, E. P. (2023). Utilization of Phyo Referral Score in assessing maternal referral quality in emergency cesarean section of maternal COVID-19 cases in Pekanbaru, Indonesia. Bali Medical Journal, 12(3), 3129-3134. 10.15562/bmj.v12i3.4700 [DOI] [Google Scholar]
- Mahmood, M. A., Hendarto, H., Laksana, M. A. C., Damayanti, H. E., Suhargono, M. H., Pranadyan, R., Santoso, K. H., Redjeki, K. S., Winard, B., & Prasetyo, B. (2021). Health system and quality of care factors contributing to maternal deaths in East Java, Indonesia. PloS One, 16(2), e0247911. 10.1371/journal.pone.0247911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahmood, M. A., Mufidah, I., Scroggs, S., Siddiqui, A. R., Raheel, H., Wibdarminto, K., Dirgantoro, B., Vercruyssen, J., & Wahabi, H. A. (2018). Root‐cause analysis of persistently high maternal mortality in a rural district of Indonesia: Role of clinical care quality and health services organizational factors. BioMed Research International, 2018(1), 3673265. 10.1155/2018/3673265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mashamba, E. K., & Ramavhoya, I. T. (2021). The stress of the midwife: Experiences of advanced midwives working in obstetric emergency units in Johannesburg, South Africa. African Journal of Reproductive Health, 25(5), 93-104. [DOI] [PubMed] [Google Scholar]
- Mengist, B., Semahegn, A., Yibabie, S., Amsalu, B., & Tura, A. K. (2024). Barriers to proper maternal referral system in selected health facilities in Eastern Ethiopia: A qualitative study. BMC Health Services Research, 24(1), 376. 10.1186/s12913-024-10825-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mgawadere, F., Unkels, R., Kazembe, A., & van den Broek, N. (2017). Factors associated with maternal mortality in Malawi: Application of the three delays model. BMC Pregnancy and Childbirth, 17, 219. 10.1186/s12884-017-1406-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health . (2012). Regulation of the Minister of Health of the Republic of Indonesia No. 1 of 2012 concerning Referral System for Individual Health Services. Retrieved from https://peraturan.bpk.go.id/Details/233396/permenkes-no-1-tahun-2012
- Ministry of Health . (2024). Indonesia Health Profile 2023. Ministry of Health of the Republic of Indonesia. https://kemkes.go.id/id/home [Google Scholar]
- Mohammed, M. m. M., El Gelany, S., Eladwy, A. R., Ali, E. I., Gadelrab, M. T., Ibrahim, E. M., Khalifa, E. M., Abdelhakium, A. K., Fares, H., & Yousef, A. M. (2020). A ten year analysis of maternal deaths in a tertiary hospital using the three delays model. BMC Pregnancy and Childbirth, 20, 585. 10.1186/s12884-020-03262-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mselle, L., Sirili, N., Anaeli, A., & Massawe, S. (2021). Understanding barriers to implementing referral procedures in the rural and semi-urban district hospitals in Tanzania: Experiences of healthcare providers working in maternity units. PloS One, 16(8), e0255475. 10.1371/journal.pone.0255475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthoni, D. M., Kabue, P. N., & Ambani, E. K. (2021). Factors that influence management of postpartum hemorrhage among midwives in a rural setting in Kenya. African Health Sciences, 21(1), 304-310. 10.4314/ahs.v21i1.39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nabulo, H., Gottfredsdottir, H., Joseph, N., & Kaye, D. K. (2023). Experiences of referral with an obstetric emergency: voices of women admitted at Mbarara Regional Referral Hospital, South Western Uganda. BMC Pregnancy and Childbirth, 23(1), 498. 10.1186/s12884-023-05795-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proos, R., Mathéron, H., Nunes, J. V., Falama, A., Kamal, P. S., Grobusch, M. P., & Van Den Akker, T. (2020). Perspectives of health workers on the referral of women with obstetric complications: A qualitative study in rural Sierra Leone. BMJ Open, 10(12), e041746. 10.1136/bmjopen-2020-041746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajbanshi, S., Norhayati, M. N., & Nik Hazlina, N. H. (2021). A qualitative study to explore the barriers for nonadherence to referral to hospital births by women with high-risk pregnancies in Nepal. International Journal of Environmental Research and Public Health, 18(11), 5801. 10.3390/ijerph18115801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rambu Ngana, F., & Eka Karyawati, A. (2021). Scenario modelling as planning evidence to improve access to emergency obstetric care in eastern Indonesia. PloS One, 16(6), e0251869. 10.1371/journal.pone.0251869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders, B., Sim, J., Kingstone, T., Baker, S., Waterfield, J., Bartlam, B., Burroughs, H., & Jinks, C. (2018). Saturation in qualitative research: Exploring its conceptualization and operationalization. Quality & Quantity, 52, 1893-1907. 10.1007/s11135-017-0574-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah, B., Krishnan, N., Kodish, S. R., Yenokyan, G., Fatema, K., Uddin, K. B., Rahman, A. K. M. F., & Razzak, J. (2020). Applying the Three Delays Model to understand emergency care seeking and delivery in rural Bangladesh: A qualitative study. BMJ Open, 10(12), e042690. 10.1136/bmjopen-2020-042690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sialubanje, C., Massar, K., van der Pijl, M. S. G., Kirch, E. M., Hamer, D. H., & Ruiter, R. A. C. (2015). Improving access to skilled facility-based delivery services: Women’s beliefs on facilitators and barriers to the utilisation of maternity waiting homes in rural Zambia. Reproductive Health, 12, 61. 10.1186/s12978-015-0051-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabong, P. T.-N., Kyilleh, J. M., & Amoah, W. W. (2021). Reasons for the utilization of the services of traditional birth attendants during childbirth: A qualitative study in Northern Ghana. Women's Health, 17, 17455065211002483. 10.1177/17455065211002483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thaddeus, S., & Maine, D. (1994). Too far to walk: Maternal mortality in context. Social Science & Medicine, 38(8), 1091-1110. 10.1016/0277-9536(94)90226-7 [DOI] [PubMed] [Google Scholar]
- Tong, A., Sainsbury, P., & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349-357. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- United Nations [UN] . (2015). Transforming our world: The 2030 agenda for sustainable development. https://sdgs.un.org/publications/transforming-our-world-2030-agenda-sustainable-development-17981
- USAID, & Ministry of Health . (2019). Every Mother and Newborn Counts Study - USAID Jalin Project https://pdf.usaid.gov/pdf_docs/PA00X87N.pdf
- WHO . (2009). Monitoring emergency obstetric care: A handbook. Geneva: World Health Organization. https://www.who.int/publications/i/item/9789241547734 [Google Scholar]
- WHO . (2017). The Network for Improving Quality of Care for Maternal, Newborn and Child Health meet on accountability for quality of care. World Health Organization. https://www.who.int/news/item/11-03-2019-the-network-for-improving-quality-of-care-for-maternal-newborn-and-child-health-meet-on-accountability-for-quality-of-care [Google Scholar]
- WHO . (2021). Ending Preventable Maternal Mortality (EPMM): A renewed focus for improving maternal and newborn health and well-being. https://www.who.int/publications/i/item/9789240040519
- Ximba, S. W., Baloyi, O. B., & Jarvis, M. A. (2021). Midwives’ perceived role in up referral of high-risk pregnancies in primary healthcare settings, eThekwini district, South Africa. Health SA Gesondheid, 26, a1546. 10.4102/hsag.v26i0.1546 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data collected and analyzed during this research is not publicly available but is available from the corresponding author upon reasonable request.