Abstract
Objectives: Despite the successful tobacco smoking cessation counseling (TSCC) efforts of dental professionals, Iranian primary care dentists have not fully utilized their potential for TSCC provision. Thus, this study assessed the TSCC practices and their associations with socio-professional attributes, knowledge, and attitude, and explored the TSCC barriers and their socio-professional determinants in a sample of Iranian primary care dentists.
Materials and Methods: This cross-sectional study was conducted at Comprehensive Healthcare Centers (CHCs) in Tehran Province, Iran from March to June 2019. All dentists practicing in these centers (n=190) completed self-administered questionnaires regarding TSCC-related knowledge, attitude, practice, and barriers. Simple and multiple linear regression and multiple logistic regression tests were used for statistical analyses.
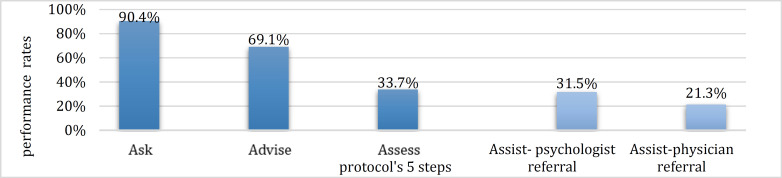
Results: The respondents (n=180, response rate=93%) were predominantly females (81.6%), recent graduates (69.6%), and non-cigarette smokers (90.2%), with a mean age of 34±9.98 years. Most performed 'Ask' (90.6%) and 'Advise' (69.1%), while a few were engaged in 'Assess' (33.7%) and fewer in 'Assist,' with 21.3% making physician referrals and 31.5% making psychologist referrals. Non-smokers (B=0.80, 95% CI: 0.19 to 1.40; P=0.01), and those with a more positive attitude (B=0.06, 95% CI: 0.04 to 0.08; P< 0.001) were more likely to provide TSCC. The main identified barriers included “absence of educational resources for patients”, “time constraints”, and “lack of patient cooperation.
Conclusion: Although the selected sample of Iranian primary care dentists performed “Ask” and “Advise” more frequently than their peers, their TSCC practice required further improvement through simplified guidelines, customized pathways, training, team work, and resource advocacy.
Key Words: Tobacco Use, Smoking, Smoking Cessation, Dentists, Primary Health Care, Iran
Introduction
Tobacco smoking is responsible for a significant number of avoidable fatalities globally, resulting in loss of more than eight million lives each year [1]. The majority of such deaths occur in low- and middle-income countries (LMICs), which account for about 80% of the global smoking population [1]. It is projected that 70% of the 10 million tobacco-related deaths expected by 2030 will occur in these nations [2]. Iran, a Middle Eastern LMIC, faces significant challenges due to tobacco smoking. The 14% smoking prevalence among the Iranian adults results in nearly 50,000 deaths annually and incurs costs exceeding 2 trillion Iranian Rials each year [3,4].
Tobacco smoking can cause a variety of oral complications [5]. It causes tooth and restoration discoloration, diminishes the sense of taste, and decelerates wound healing [6]. In addition, several studies have reported that smoking increases the mean Decayed, Missing, and Filled Teeth index by 1.2 points, doubles the risk of periodontal disease, raises the likelihood of tooth loss by 1.5 times, and elevates the risk of oral cancer by 7 to 10 times [6-8]. Nonetheless, smoking cessation can improve and even reverse most of these complications [6,9,10].
Although most smokers have the desire to quit, they may fail up to 30 times before quitting successfully, and only 3-5% quit without an external aid [10-12]. Quit rates are lower in LMICs where resources and infrastructure are lacking to combat tobacco use [13,14]. In such contexts, health professionals, given their credibility and influence on the community, can significantly contribute to smoking cessation efforts as advocates, leaders, and role models [10,15].
Global health organizations such as the World Health Organization (WHO) and the FDI World Dental Federation endorse tobacco smoking cessation counseling (TSCC) provided by dental professionals [6,9]. Dental professionals can achieve a remarkable 70% increase in long-term quit rates through TSCC due to their regular engagement with smokers, longer appointment periods with patients, and focusing only on the oral cavity, where early signs and symptoms of smoking appear [1,6,9,10,16].
Despite the endorsements and opportunities, only about 10-25% of dental professionals routinely provide TSCC [9,17]. A similar pattern of such a low engagement has been witnessed among Iranian senior dental students and private dentists [18-20]. However, limited data are available on TSSC practices of Iranian primary care dentists. This knowledge gap should be addressed since both the WHO and the FDI World Dental Federation identify primary care setting as the optimal setting for smoking cessation counseling [6,9]. Additionally, Iranian primary care services are valuable for smoking cessation research due to their extensive coverage and high patient load [21,22].
Therefore, the present study investigated the TSCC practices of Iranian primary care dentists in Tehran Province and assessed the relationship between such practices and socio-professional attributes, TSCC knowledge, and TSCC attitude. Furthermore, it explored the dentists’ barriers against TSCC provision as well as the socio-professional determinants of such barriers.
MATERIALS AND METHODS
This study followed the STROBE checklist [23].
Study design and ethical considerations:
The present cross-sectional study was conducted in Tehran Province, Iran between March and June 2019 after obtaining approval from the ethics committee of Tehran University of Medical Sciences (Ethics code: IR.TUMS.DENTISTRY.REC.1397.174). Prior to data collection, one investigator explained the study objectives to the participants and emphasized on voluntary participation, anonymity preservation, and data confidentiality. It was also stated that completing the questionnaire would mean giving an informed consent for participation in the study.
Setting:
Tehran Province was chosen as the study setting for three main reasons. First of all, it is Iran’s most populated province, with nearly 13 million residents [24], and home to the capital of Iran, Tehran. Also, it is a predominantly urban area, and Iranian urban primary care services claim to have close to 100% coverage in this province [22]. Additionally, urban primary care in Iran is delivered through Comprehensive Healthcare Centers (CHCs), each serving approximately 37,500 individuals [21]. All CHCs in Tehran Province were included in the sampling frame.
Study population:
Practicing dentists in all Tehran's CHCs were eligible for participation, and data were collected from all eligible participants using a census sampling method (n=190).
Research procedure:
Sessions were held with the CHC managers to explain the study objectives and design, and seek their collaboration. Following coordination, arrangements were made such that one of the investigators could attend the quarterly sessions of the CHC managers routinely held for Tehran Province’s CHC dentists to discuss the problems, find solutions, and exchange ideas. During these sessions, the investigator provided the dentists with explanations outlined in the study design and ethics section, distributed the questionnaires, offered necessary clarifications as the questionnaires were being completed, and collected the completed questionnaires.
Research tools:
A self-administered Persian questionnaire was developed and utilized for this study. The knowledge questions were adopted from previous studies [25,26]; while, the attitude, practice, and barrier questions were designed using previous studies and the United States Public Health Department guidelines [25-27]. The English translation of the questionnaire is provided as a supplementary file (Supplementary Material 1).
To assess the face validity of the questionnaire, a group of 10 dentists and a panel of experts (comprising of 6 community oral health professors and 1 epidemiology professor) were consulted to examine the response formats, phrasing, and readability. The panel was then asked to evaluate the questionnaire's content validity by rating the questions regarding relevance, simplicity, clarity, and necessity using a Likert scale ranging from 1 to 4. Following their feedback, revisions were made, resulting in a scale content validity index of 0.77. For reliability assessment, the questionnaire was administered among a subset of the original participants twice, with a two-week interval (these responses were excluded from the main statistical analysis). The agreement coefficient was calculated for each question, with values ranging from 60% to 97.5% for all questions.
The final questionnaire comprised of five sections on socio-professional attributes and TSCC-related knowledge, attitude, practice, and barriers.
Independent variables:
1. Socio-professional attributes included age (in years), gender (male, female), years since graduation, site of practice (city of Tehran, neighboring towns), years of practice at public dental centers, simultaneous private practice (yes, no), CHC employment status (on governmental service: a mandatory service for newly graduated Iranian health professionals [22], official employment, contractual employment, others), years of CHC practice (less than 6 months, less than 1 year, less than 18 months, less than 24 months, 2 to 5 years, 5 to 10 years, 10 to 15 years, 15 to 20 years, 20 to 25 years, 25 to 30 years), cigarette, hookah, and pipe smoking status (never smoked, used to smoke but quit, smoking once a month or less, smoking two or three times a month, smoking two or three times a week, smoking once a day or more), and presence of smoker(s) in the immediate family (yes, no).
2. The knowledge score was measured by 6 questions based on the 5As protocol (Ask, Advise, Assess, Assist, and Arrange) [27] with Likert scale responses ranging from strongly disagree (scored 1) to strongly agree (scored 5) and a total score of 6 to 30, according to the methodology of a previous study [25].
3. The attitude score was measured using 16 questions based on the 5As protocol, TSCC responsibilities, TSCC significance, training requirements, and dentists’ capabilities with Likert scale responses ranging from strongly disagree (scored 1) to strongly agree (scored 5) and a total score of 16 to 80, according to the methodology of a previous study [25].
Outcome variables:
The practice score was measured by 5 "yes or no" questions based on the 5As protocol [27], with a score of 2 for "yes", 1 for "no", and a total score of 5 to 10, according to the methodology of previous studies [25,26]. The questions addressed dentists' practice based on the 5As with a slight modification of not including a specific question on the “Arrange” item. This exclusion was due to the CHCs’ high workload, making it impractical for dentists to perform “Arrange” by personally scheduling follow-up appointments.
The barriers were assessed using 15 questions with Likert scale responses ranging from 1 (indicating no importance) to 5 (indicating extremely high importance). This variable was not scored according to the methodology of a previous study [18].
Statistical analysis:
Data were entered into IBM SPSS Statistics for Windows, version 24. Descriptive data were expressed as percentage, mean, standard deviation, and range. Based on the distribution of responses and in methodological alignment with previous studies [18, 28], socio-professional attributes were categorized as follows: “under 35” and "35 and above" for age, “less than 5 years”, and “5 years and above” for years since graduation, "less than 2 years" and "2 years and above” for history of public practice, and "contractual or on governmental service”, "official and others" for CHC employment status. Additionally, those who “never smoked” and “smoked and quit” were classified as non-smokers, and all others were classified as smokers. Also, “none”, “low”, and “moderate importance” responses to questions on barriers were grouped together as “low importance”, while “high” and “extremely high importance” responses were grouped together as “high importance” to be analyzed as categorical outcome variables and based on their distributions.
A simple linear regression assessed the relationship between practice score, socio-professional attributes, knowledge score, and attitude score to identify independent variables that were associated with outcome variables with P-values below 0.2. These variables were then included in a multiple linear regression model (forward method). A second similar regression model was developed (excluding knowledge and attitude scores) to assess the relationship between socio-professional attributes and practice score (the results of these two models were explained only in the text). Finally, multiple logistic regression (forward method) was applied to assess the relationship between TSCC barriers and socio-professional attributes. Significance was set at 0.05 for all tests.
Results
One-hundred and eighty CHC dentists completed the questionnaires, resulting in a response rate of 93%.
Socio-professional attributes:
The majority of the participating dentists were females (81.60%), with a mean age of 34±9.98 years. Of the participants, 69.6% had graduated less than 5 years ago, 71.8% were contractual and governmental service employees, and 66.47% had less than 2 years of public practice history. Most of the participants (90.2%) had never smoked cigarettes, and a small percentage (13.2%) had smoked tobacco i.e., either cigarette, hookah, or pipe (Table 1).
Table 1 .
Socio-professional attributes in a sample of Tehran primary care dentists (n=180)
| Variable | Number (%) |
|---|---|
| Sex Male Female |
32 (18.4%) 142 (81.6%) |
| Age Under 35 years 35 years and older |
122 (70.9%) 50 (29.1%) |
| Years since graduation Under 5 years 5 years and above |
112 (69.6%) 49 (30.4%) |
| Employment status Contractual/ governmental service Official and other |
125 (71.8%) 49 (28.2%) |
| History of public practice Under 2 years 2 years and above |
115 (66.5%) 58 (33.5%) |
| Site of practice City of Tehran Neighboring towns |
82 (47.4%) 91 (52.6%) |
TSCC practices:
The participants’ mean practice score was 7.46±1.35. As demonstrated in Figure 1, the majority of the participants performed “Ask” (90.4%) and “Advise” (69.1%), while only a little more than one-third (33.7%) engaged in “Assess”.
Fig. 1.
Smoking cessation counseling practices by a sample of Tehran primary care dentists (n=180)
As demonstrated in Table 2, non-smoking participants obtained higher practice scores than smokers [mean difference (MD)=-0.89, 95% CI: -1.33 to -0.40, P=0.001). Additionally, participants with higher attitude scores obtained higher practice scores (MD=0.06, 95% CI: 0.04 to 0.08, P<0.001), while those with higher knowledge scores obtained lower practice scores (MD=-0.11, 95% CI: -0.22 to 0.002, P=0.04).
Table 2 .
Influence of socio-professional attributes, tobacco smoking cessation counseling (TSCC), knowledge scores, and TSCC attitude scores on TSCC practice scores of a sample of Tehran primary care dentists (n=173a)
| Variables | Variable categories | Number | Mean practice scores (std.b) |
MDc of practice scoresd (95% CI) |
P- Value |
|---|---|---|---|---|---|
| Sex | Female | 141 | 7.49 (1.32) | 0.24 (0.28 to 0.76) |
0.37 |
| Male | 32 | 7.25 (1.50) | |||
| Age | Under 35 years | 121 | 7.40 (1.31) | 0.22 (-0.66 to 0.23) |
0.32 |
| 35 years and older | 50 | 7.62 (1.44) | |||
| Years since graduation |
< 5 years | 111 | 7.36 (1.33) | -0.28 (-0.72 to 0.16) |
0.20 |
| 5 and above | 56 | 7.64 (1.41) | |||
| Employment status | Contractual/ governmental service | 124 | 7.41 (1.34) | -0.12 (-0.57 to 0.33) |
0.60 |
| Official and others | 49 | 7.53 (1.42) | |||
| Public practice history |
Less than 2 years | 114 | 7.46 (1.37) | -0.17 (-0.41 to 0.45) |
0.94 |
| 2 years and above | 58 | 7.45 (1.31) | |||
| Site of practice | City of Tehran | 81 | 7.54 (1.38) | 0.19 (-0.23 to 0.60) |
0.39 |
| Neighboring towns | 91 | 7.36 (1.35) | |||
| Simultaneous private practice |
Yes | 57 | 7.42 (1.43) | -0.20 (-0.54 to 0.42) |
0.94 |
| No | 114 | 7.44 (1.33) | |||
| Tobacco smoking status |
Yes | 23 | 6.70 (0.97) | -0.89 (-1.33 to -0.40) |
0.001 |
| No | 150 | 7.56 (1.37) | |||
| Smoker(s) in immediate family |
Yes | 45 | 7.22 (1.28) | -0.32 (-0.78 to 0.15) |
0.18 |
| No | 126 | 7.54 (1.28) | |||
| Knowledge score | - | 178 | - | -0.11 (-0.22 to 0.002) |
0.04 |
| Attitude score | - | 178 | - | 0.06 (0.04 to 0.08) |
<0.001 |
Seven dentists did not respond to at least one question in this section;
standard deviation;
Mean difference;
Regression coefficient
Variables with P<0.2 (knowledge score, attitude score, years since graduation, presence of a smoker in the immediate family, and tobacco smoking status) were included in the first multiple linear regression model (forward method). Out of these, only the attitude score was found to be related to the practice score, as participants with higher attitude scores were more likely to achieve higher practice scores (B=0.06, 95% CI: 0.04 to 0.08; P<0.001). However, the differences in practice scores between the groups were negligible (less than 1.5%).
The second model of multiple linear regression (which excluded knowledge and attitude scores) revealed that only tobacco smoking status was associated with the practice score, with non-smokers being more likely to achieve higher practice scores (B=0.80, 95% CI: 0.19 to 1.40; P=0.01).
Barriers against TSCC:
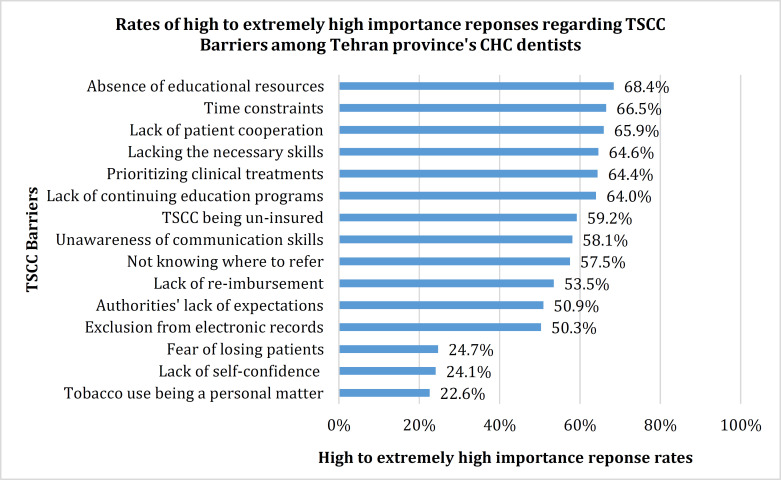
The participants perceived “absence of educational resources for patients (brochures or pamphlets)”, “time constraints”, and “lack of patient cooperation” as the most important barriers against TSCC; while deeming “tobacco smoking being a personal matter”, “lack of self-confidence”, and “fear of losing patients” as the least important ones (Fig 2).
Fig 2.
“High importance” responses to questions on barriers (n=180) by a sample of Tehran primary care dentists.
As illustrated in Table 3, considering the influence of socio-professional attributes on TSCC barriers, female dentists were more likely to consider "lack of reimbursement" as a substantial barrier compared to male dentists, and tobacco-smoking dentists were more likely to perceive this barrier as significant compared to their non-smoking counterparts (OR=0.34, 95% CI: 0.14 to 0.84, P=0.02 and OR=0.27, 95% CI: 0.09 to 0.83, P=0.02, respectively). Moreover, non-smoking dentists had an increased likelihood of struggling with “lack of confidence” than smoking dentists (OR=10.73, 95% CI: 1.43 to 85.68, P=0.02) and contractual and governmental service dentists had higher odds of considering "time constraints" as an important barrier compared to those with official/other employment status (OR=0.036, 95% CI: 0.18 to 0.73, P=0.005).
Table 3 .
Influence of socio-professional attributes on the barriers against tobacco smoking cessation counseling practices by a sample of Tehran primary care dentists (n=163a)
| Barrier | Socio-professional attributes |
Socio-professional attribute categories |
OR b (95% CI c) |
P- value |
|---|---|---|---|---|
| Tobacco use being personal |
Age | Under 35 years* | 2.53 (1.19 to 5.40) |
0.02 |
| 35 years and older | ||||
| Time constraints | Employment status | Contractual/governmental service* | 0.036 (0.18 to 0.73) |
0.005 |
| Official and others | ||||
| Lack of reimbursement |
Tobacco smoking status |
Yes* | 0.27 (0.09 to 0.83) |
0.02 |
| No | ||||
| Lack of reimbursement |
Sex | Female* | 0.34 (0.14 to 0.84) |
0.02 |
| Male | ||||
| Fear of losing patients |
Site of practice | City of Tehran* | 0.43 (0.21 to 0.89) |
0.02 |
| Neighboring towns | ||||
| Fear of losing patients |
Tobacco smoking status |
Yes* | 0.38 (0.15 to 1) |
0.05 |
| No | ||||
| Lack of continuing professional education |
Site of practice | City of Tehran* | 0.47 (0.24 to 0.90) |
0.02 |
| Neighboring towns | ||||
| TSCC being un- insured |
Simultaneous private practice |
Yes* | 2.70 (1.38 to 5.26) |
0.004 |
| No | ||||
| Authorities’ lack of expectations |
Public practice history |
Less than 2 years* | 2.66 (1.25 to 5.69) |
0.01 |
| 2 years and above | ||||
| Authorities’ lack of expectations |
Simultaneous private practice |
Yes* | 2.89 (1.36 to 6.12) |
0.006 |
| No | ||||
| TSCC electronic record excluded |
Sex | Female* | 0.26 (0.10 to 0.66) |
0.005 |
| Male | ||||
| TSCC electronic record excluded |
Site of practice | City of Tehran* | 0.31 (0.16 to 0.60) |
0.001 |
| Neighboring towns | ||||
| Lack of confidence | Tobacco smoking status |
Yes* | 10.73 (1.34 to 85.68) |
0.02 |
| No | ||||
| Lack of confidence | Smoker(s) in immediate family |
Yes* | 0.36 (0.16 to 0.80) |
0.01 |
| No |
Seventeen dentists did not respond to at least one question in this section;
Odds ratios;
confidence interval;
Reference categories
Discussion
The present study examined the TSCC practices of primary care dentists of Tehran Province, the socio-professional, knowledge, and attitude determinants of their practice, barriers in this regard, and the socio-professional determinants of the barriers. The results revealed that while the majority of Tehran primary care dentists performed "Ask" and "Advise", only about one-third engaged in "Assess" and "Assist". Positive attitudes towards TSCC and non-smoking status were significantly associated with greater TSCC implementation. Moreover, participants identified "absence of educational resources for patients," "time constraints," and "lack of patient cooperation" as significant barriers against TSCC. Contractual dentists and those on governmental service viewed "time constraints" as a more substantial barrier compared to their officially employed counterparts. Additionally, non-smoking dentists were more inclined to consider "lack of confidence" as a significant barrier compared to their smoking counterparts.
In alignment with previous studies [18-20,28-31], the participants of the present study demonstrated greater engagement in the initial steps of the 5As protocol, with less involvement in later steps. Their engagement was high in "Ask," moderate to high in "Advise," mid-range in "Assess," and moderate to low in "Assist," compared to engagement rates which ranged from 51% to 96% in American dental professionals, 26% to 84% in Kuwaiti dental professionals, and 4% to 74%, and 20% to 66% in two groups of Iranian dental professionals [18,20,29-31].
The association discovered between positive attitudes and superior TSCC practice was anticipated, as it has been frequently reported in previous studies [20,29,32]. These studies also indicated that the attitudinal factors relevant to effective TSCC include recognizing the importance and effectiveness of such practices, feeling knowledgeable and prepared to intervene, and willingness to intervene [20,29,32]. The present study participants might have exhibited superior TSCC practice due to their favorable attitude towards TSCC, which could have resulted in increased motivation, confidence, and dedication to patient care. Such positive attitudes may have contributed to the overall improvement in the quality of TSCC practice observed among the participants.
The literature was conflicting regarding the relationship between dentists' smoking status and their TSCC practices [33]. In agreement with the present study, non-smoking dentists in England and Saudi Arabia were more likely to provide TSCC [28,34]; whereas, no such associations were observed among periodontists in the United States or dentists in United Arab Emirates [31,35]. Participants who did not smoke in the present study probably exhibited better TSCC practices because they may strongly dislike smoking or have a clearer comprehension of the health risks of smoking.
"Absence of educational resources for patients" as the participants’ main barrier was an unexpected finding of the present study supported by some previous studies [18,36]. This barrier was potentially and particularly significant for the participants because they were mostly recent graduates with limited practice experience who probably felt uncomfortable discussing TSCC with patients and thus, relied heavily on external aids.
"Time constraints", the participants’ second most important barrier, is a common global challenge faced by dental professionals [18,28-31]. Interestingly, Australian oral health practitioners and primary prevention-focused oral healthcare providers, did not consider time limitations as a major TSCC obstacle [36], potentially because of their prevention-focused training and professional role description [37]. However, the participants of the present study were mostly inexperienced, lacked the necessary TSCC skills (reported as their fourth top barrier), and probably struggled with insufficient TSCC training similar to other Iranian dental professionals [18-20]; all these factors may contribute to time allocation challenges.
The participants’ third most important barrier, "lack of patient cooperation", is also a common worldwide challenge among dental professionals. Both the United States periodontists and Iranian private-practice dentists faced similar difficulties with "low patient acceptance," "patient resistance," and "patient disinterest" [18,31]. However, Kuwaiti dentists and Australian oral health practitioners did not deem patients’ resistance, non-compliance, or offense-taking as major barriers [30,36]. Similar to previous studies, where dentists often felt unsure and anxious about patients' reactions to TSCC due to their lack of confidence in providing such care and their subpar communication skills [33,38], the participants of the present study probably experienced a similar pattern that was also aggravated by their limited practice experience.
Contractual dentists and those on governmental service were more likely to consider "time constraints" as a significant barrier compared to their officially employed counterparts. This somewhat aligns with less experienced Indian dental practitioners struggling more with "lack of time" than their experienced counterparts [39]. Interestingly, however, experienced Saudi Arabian dentists were more likely to perceive "lack of time" as a substantial barrier than their inexperienced peers [28]. The predominance of recent graduates in contractual employment and governmental service may explain struggling with time management due to their inexperience in balancing clinical patient care and preventive care, resulting in longer consultations and task prioritization difficulties.
Non-smoking dentists were more likely to consider "lack of confidence" as a significant barrier compared to their smoking counterparts, a trend also observed among non-smoking Saudi Arabian dentists [28]. The non-smoking dentists’ lack of personal smoking experience may have caused them to feel they lack understanding and insight into the issue, thereby diminishing their confidence in their TSCC provision skills.
To enhance smoking cessation practices among Iranian primary care dentists, a comprehensive, multifaceted approach is required. Tailored executive pathways should be devised for different primary care settings, and the mandatory documentation of TSCC provision should be linked to recognition or financial compensation from primary care authorities. Simplified versions of the 5As protocol, such as Ask-Advise-Refer [33], should be integrated into Iranian TSCC guidelines to streamline the practice and facilitate progression. TSCC training should be offered based on smoking status, as the literature emphasizes on attitude cultivation among smoking dentists, and knowledge expansion among non-smoking dentists [34,40]. Smoking should be discouraged in the Iranian primary dental care setting through workshops, counseling, and peer support groups. Positive attitudes toward TSCC can be cultivated by establishing it early as a professional duty in dental schools, integrating it comprehensively in the undergraduate educational curricula, and regularly updating it in continuing education programs, with official recognition and celebration from Iranian primary care authorities.
Addressing TSCC barriers also requires a multifaceted approach. Iranian primary care authorities should allocate resources to developing patient-literacy educational content. Tailored training programs should focus on time management for less experienced dentists and building confidence in TSCC provision for non-smoking dentists. Practical training in dental schools and continuing education programs should emphasize on efficient 5As implementation within 3-5 minutes [9]. Mentorship programs should be established where experienced dentists guide colleagues in time management and confidence building. A team-based TSCC approach should involve other primary dental care staff, such as oral health technicians, dental hygienists, and dental assistants, to alleviate time pressures [22,31]. Additionally, Iranian primary care dentists should be informed that patients generally welcome and expect TSCC, alongside receiving communication skills training in dental schools and continuing education programs [33,38].
Strengths, limitations, and future directions:
The strengths of the present study included its underexplored population and setting, census sampling method, high response rate, scored and specifically-developed questionnaire, and assessment of TSCC barriers’ socio-professional determinants. It also had several limitations. The cross-sectional design, although suitable for study objectives, limited causal inference. The self-report measures, commonly utilized in the TSCC literature, may have introduced the bias of social desirability into the study. The sample skewed towards female recent graduates under the age of 35 years (which was the result of Iranian Ministry of Health’s dentist deployment arrangements in urban CHCs) might have affected the generalizability of the findings to all Iranian primary care dentists. Lastly, not investigating the participants’ performance of “Arrange” step of the 5As protocol may have reduced study comparability.
Future research could involve primary care dentists across other provinces of Iran as well as the primary care dentists of other LMICs, seek the opinions of other primary dental care team members and patients with regards to TSCC, collect qualitative data especially on dentists’ TSCC barriers, assess dentists’ TSCC practice in alternative ways such as electronically-documented referrals, and conduct interventions with adequate follow-ups to explore the impact of established executive routes on dentists’ TSCC practice.
CONCLUSION
The current study highlighted inadequate TSCC practice in a group of primary care dentists in Iran, demonstrating the correlation between non-smoking habits, favorable attitudes, and effective TSCC delivery, while also pointing out the main obstacles faced in providing TSCC. In order to support Iranian primary care dentists in their role as the key advocates for smoking cessation, it is suggested to introduce simplified local protocols, personalized action plans, and specialized training in both undergraduate and continuing education courses. Furthermore, promoting team-based strategies and securing essential resources could boost their efforts in helping patients to quit smoking.
ACKNOWLEDGMENTS
We would like to extend our gratitude to all those who took part in this study, specifically Dr. Ahmad Reza Shamshiri for his constructive feedback and help in data analysis.
Notes:
Cite this article as: Khami MR, Bastani P, Varmazyari S. Smoking Cessation Counseling: Practices, Determinants, and Barriers in a Sample of Iranian Primary Care Dentists. Front Dent. 2024:21:38.
FUNDING
The authors received partial financial support from Tehran University of Medical Sciences (TUMS) as a Master of Public Health (MPH) thesis grant.
CONFLICT OF INTEREST STATEMENT
None declared.
DATA AVAILABILITY STATEMENT
The datasets generated and analyzed during the current study are not publicly available due to TUMS data sharing policies. They can be made available by the corresponding author on reasonable request.
References
- 1.Fact sheet on tobacco use: World health organization. 2023. [Accessed August 7, 2024]. Available at: https://www.who.int/news-room/fact-sheets/detail/tobacco/
- 2.Jha P, Peto R. Global effects of smoking, of quitting, and of taxing tobacco. N Engl J Med. 2014 Jan;370(1):60–8. doi: 10.1056/NEJMra1308383. [DOI] [PubMed] [Google Scholar]
- 3.Country factsheet on Iran: Tobacco use atlas. 2024. [Accessed February 3, 2024]. Available at: https://tobaccoatlas.org/factsheets/iran-islamic-republic-of//
- 4.Abbasi-Kangevari M, Ghanbari A, Fattahi N, Malekpour M-R, Masinaei M, Ahmadi N, et al. Tobacco consumption patterns among Iranian adults: a national and sub-national update from the STEPS survey 2021. Sci Rep. 2023 Jun;13(1):10272. doi: 10.1038/s41598-023-37299-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.United States. Public Health Service. Office of the Surgeon General, United States. Office on Smoking. The health consequences of smoking: a report of the Surgeon General. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office of Smoking and Health. 2004.
- 6.Tobacco or oral health: An advocacy guide for oral health professionals: FDI World Dental Federation. [Accessed September 18, 2023]. Available at: https://fdiworldental.org/tobacco-or-oral-health-advocacy-guide-oral-health-professionals/
- 7.Warnakulasuriya S, Sutherland G, Scully C. Tobacco, oral cancer, and treatment of dependence. Oral Oncol. 2005 Mar;41(3):244–60. doi: 10.1016/j.oraloncology.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 8.Jiang X, Jiang X, Wang Y, Huang R. Correlation between tobacco smoking and dental caries: A systematic review and meta-analysis. Tob Induc Dis. 2019;17:34. doi: 10.18332/tid/106117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Monograph on tobacco cessation and oral health integration. World Health Organization; [Accessed February 3, 2024]. Available at: https://www.who.int/publications/i/item/9789241512671/ [Google Scholar]
- 10.Tobacco free inititative: role of health professionals. World Health Organization; [Accessed February 3, 2024]. Available at: https://www.who.int/publications/i/item/9241593202/ [Google Scholar]
- 11.Michael C, Lori D, Joanna EC, Susan JB, Peter S, Anne P, Robert S. Estimating the number of quit attempts it takes to quit smoking successfully in a longitudinal cohort of smokers. BMJ Open. 2016 Jun;6(6):e011045. doi: 10.1136/bmjopen-2016-011045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Martha A, Sotiria S, Eleni L, Vasiliki S, Kondylia K, Andromachi S, et al. Success rates are correlated mainly to completion of a smoking cessation program. Eur Respir J. 2016;48(suppl 60):PA4599. [Google Scholar]
- 13.Abdullah ASM, Husten CG. Promotion of smoking cessation in developing countries: a framework for urgent public health interventions. Thorax. 2004 Jul;59(7):623. doi: 10.1136/thx.2003.018820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nichter M. Introducing tobacco cessation in developing countries: an overview of Project Quit Tobacco International. Tob Control. 2006 Jun;15 Suppl 1(Suppl 1):i12–7. doi: 10.1136/tc.2005.014704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lando HA. Promoting Tobacco Cessation in Low- and Middle-Income Countries. J Smok Cessat. 2016 Jun;11(2):61–64. doi: 10.1017/jsc.2016.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carr AB, Ebbert J. Interventions for tobacco cessation in the dental setting. Cochrane Database Syst Rev. 2012;2012(6):Cd005084. doi: 10.1002/14651858.CD005084.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jannat-Khah DP, McNeely J, Pereyra MR, Parish C, Pollack HA, Ostroff J. Dentists' Self-Perceived Role in Offering Tobacco Cessation Services: Results From a Nationally Representative Survey, United States, 2010-2011. Preventing Chronic Disease. 2014;11:E196. doi: 10.5888/pcd11.140186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ebn Ahmady A, Khoshnevisan MH, Heidari N, Lando HA. Dentists' familiarity with tobacco cessation programs in dental settings in Iran. J Public Health Dent. 2011 Sep;71(4):271–7. doi: 10.1111/j.1752-7325.2011.00262.x. [DOI] [PubMed] [Google Scholar]
- 19.Ebn Ahmady A, Golmohammadi S, Ayremlou S, Khoshnevisan MH, Lando HA. Tobacco cessation practices of senior dental students in Iran. Int Dent J. 2011 Dec;61(6):302–6. doi: 10.1111/j.1875-595X.2011.00066.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Razavi SM, Zolfaghari B, Doost ME, Tahani B. Attitude and practices among dentists and senior dental students in iran toward tobacco cessation as an effort to prevent oral cancer. Asian Pac J Cancer Prev. 2015;16(1):333–8. doi: 10.7314/apjcp.2015.16.1.333. [DOI] [PubMed] [Google Scholar]
- 21.Gouya MM, Seif-Farahi K, Hemmati P. An overview of Iran's actions in response to the COVID-19 pandemic and in building health system resilience. Front Public Health. 2023 Feb;11:1073259. doi: 10.3389/fpubh.2023.1073259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khoshnevisan MH, Ghasemianpour M, Samadzadeh H, Baez RJ. Oral health status and healthcare system in I.R. Iran J Contem Med Sci. 2018;4(3):107–8. [Google Scholar]
- 23.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Br Med J. 2007;335(7624):806–8. doi: 10.1136/bmj.39335.541782.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Iran administrative division September 24, 2016. [Accessed March 29, 2024]. Available at: https://www.citypopulation.de/en/iran/admin//
- 25.Khami M, Ebn Ahmady A, Ahmadian M, Razghi S. Knowledge, attitude and skills of dental students of Tehran and Shahid Beheshti dental schools towards tobacco cessation counseling. J Dent Med. 2014 Sep 10;27(3):208–15. [Google Scholar]
- 26.Ahmadianghalehsorkh M, Khami M, Ahamdi A, Razeghi S, Yazdani R. Effectiveness of two interactive educational methods to teach tobacco cessation counseling for senior dental students. Eur J Dent. 2017 Jul;11:287–92. doi: 10.4103/ejd.ejd_352_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tobacco TC. A clinical practice guideline for treating tobacco use and dependence: 2008 update: a US public health service report. Am J Prev Med. 2008 Aug;35(2):158–76. doi: 10.1016/j.amepre.2008.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Halboub E, Jafer MA, Khormi HI, Kariri AA, Atiah SA, Lughbi SJ, et al. Attitudes and practices of tobacco cessation counseling among Saudi dental professionals: A nationwide cross-sectional survey. Niger J Clin Pract. 2022 Apr;25(4):502–8. doi: 10.4103/njcp.njcp_1784_21. [DOI] [PubMed] [Google Scholar]
- 29.Prakash P, Belek MG, Grimes B, Silverstein S, Meckstroth R, Heckman B, et al. Dentists' attitudes, behaviors, and barriers related to tobacco‐use cessation in the dental setting. J Pblic Health Dent. 2013 Mar;73(2):94–102. doi: 10.1111/j.1752-7325.2012.00347.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Khalaf M. Smoking cessation practices in Kuwaiti general dental clinics. Med Princ Pract. 2013 Sep;22(6):576–82. doi: 10.1159/000351560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Patel AM, Blanchard SB, Christen AG, Bandy RW, Romito LM. A survey of United States periodontists' knowledge, attitudes, and behaviors related to tobacco-cessation interventions. J Periodontol. 2011 Mar;82(3):367–76. doi: 10.1902/jop.2010.100405. [DOI] [PubMed] [Google Scholar]
- 32.Rajput S, Gadiyar A, Kumar A, Kamat A, Gaunkar R, Jain A. Tobacco cessation counseling: Are dentists doing enough? J Indian Assoc Public Health Dent. 2020 Jan;18(1):60–5. [Google Scholar]
- 33.Chan HL, Chan AKY, Chu CH, Tsang YC. Smoking cessation in dental setting: a narrative review on dental professionals' attitude, preparedness, practices and barriers. Front Oral Health. 2023 Sep;4:1266467. doi: 10.3389/froh.2023.1266467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.John J, Thomas D, Richards D. Smoking cessation interventions in the Oxford region: changes in dentists' attitudes and reported practices 1996–2001. Br Dent J. 2003 Sep;195(5):270–5. doi: 10.1038/sj.bdj.4810480. [DOI] [PubMed] [Google Scholar]
- 35.Bangera D, Takana M, Muttappallymyalil J. Tobacco cessation: attitude and practice of dentists in Northern United Arab Emirates. East Mediterr Health J. 2018 May;24(5):419–26. doi: 10.26719/2018.24.5.419. [DOI] [PubMed] [Google Scholar]
- 36.Ford P, Tran P, Keen B, Gartner C. Survey of Australian oral health practitioners and their smoking cessation practices. Aust Dent J. 2015 Mar;60(1):43–51. doi: 10.1111/adj.12270. [DOI] [PubMed] [Google Scholar]
- 37.Ford PJ, Farah CS. Oral health therapists: what is their role in Australian health care? Int J Dent Hyg. 2013 Feb;11(1):22–7. doi: 10.1111/j.1601-5037.2012.00564.x. [DOI] [PubMed] [Google Scholar]
- 38.Campbell HS, Sletten M, Petty T. Patient perceptions of tobacco cessation services in dental offices. J Am Dent Assoc. 1999 Feb;130(2):219–26. doi: 10.14219/jada.archive.1999.0171. [DOI] [PubMed] [Google Scholar]
- 39.Mehta A, Kaur G, Popli R, Khurana S. Tobacco use cessation efforts among private dental practitioners of Delhi, India. Dent 3000. 2020 Jul 23;8(1):11–23. [Google Scholar]
- 40.John JH, Yudkin P, Murphy M, Ziebland S, Fowler GH. Smoking cessation interventions for dental patients--attitudes and reported practices of dentists in the Oxford region. Br Dent J. 1997 Nov;183(10):359–64. doi: 10.1038/sj.bdj.4809511. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analyzed during the current study are not publicly available due to TUMS data sharing policies. They can be made available by the corresponding author on reasonable request.