Abstract
Objectives: The aim of the present investigation was to evaluate the possible anxiolytic effect of jasmine aromatherapy in pediatric dental procedures.
Materials and Methods: A parallel randomized single-blinded placebo-controlled clinical trial was designed and conducted from February 19 until April 19, 2020, on children aged 7 to 12 years-old requiring class 1 restorative treatment of primary or permanent tooth with infiltration anesthesia. Interventions were defined as 15 minutes of aromatherapy using 2mL of jasmine extract for the intervention group, and with water for the control group. Outcomes were defined as child’s anxiety and pain perception, measured by modified child dental anxiety scale (MCDAS), visual analogue scale (VAS) and changes of vital signs. After the patients received interventions based on their groups, their data was collected and analyzed. We used parametric tests and linear regression for outcome comparisons.
Results: 56 patients were randomized and allocated in two groups, 28 to each. The groups did not differ significantly regarding age, sex, heart rate and O2 saturation before, during, and after procedures. Based on multivariable regression, the intervention group showed a significantly reduced MCDAS (B (95% CI) =-2.11 (-4.09, -0.13), P=0.04) and VAS (B (95% CI) =-2.30 (-3.50, -1.10), P<0.001) scores.
Conclusion: Jasmine aromatherapy showed to be effective in reducing children’s anxiety and pain perception during dental procedures and therefore, can be suggested as a cheap and practical complementary method in dental practice.
Key Words: Jasmine Oil, Aromatherapy, Anxiety, Pain Perception, Pediatric Dentistry, Randomized Controlled Trial
Introduction
Dental anxiety/fear is a common problem among the children and adolescents across the globe (1). Managing this problem in a harmless cost-beneficial way has been among the aims of many previous studies. The suggested methods range from behavioral methods, e.g., communication, distraction etc., to musictherapy (2-4). Among which has also been aromatherapy, which is the inhalation of certain aromatic compounds, mostly extracted from plants. While its exact mechanistic effects understudied (5), the effects of aromatherapy with essential oils has been studied in patients undergoing a wide range of stressful phenomena, such as labor (6), menopause (7), burns (8), postoperative recovery (9), even stroke (10) and laparoscopic cholecystectomy (11). Although still in infancy, aromatherapy is making its way into dentistry as well, particularly to deal with anxious children for whom visiting the dentist office may be considered a major stressful phenomenon. Children receiving aromatherapy with lavender and orange essential oils – either with inhalers, nebulizers, or diffusers – have shown lower salivary cortisol levels, while being less anxious and perceiving less pain when undergoing dental procedures (12-17). It is unclear, however, whether other essential oils could have the same effects as lavender and orange. To the best of our knowledge, no study has yet aimed to investigate the effect of aromatherapy with jasmine essence, as an anxiolytic method in pediatric dentistry. Therefore, we aimed to investigate the anxiolytic effect of jasmine aromatherapy as a complementary method in pediatric dentistry, to determine whether it could have similar effects with lavender and orange aromatherapy.
MATERIALS AND METHODS
Study Design and Participants
The CONSORT guidelines were followed in the conduct and reporting of the current investigation. The study was designed as a randomized parallel placebo-controlled trial with 1:1 allocation ratio. The inclusion criteria were predefined as: 1. Children aged 7 to 12 years-old; 2. Candidates for dental practice with previous record; 3. Children with Frankl + or ++ based on previous records and gathering information from parents and dentist observation and interaction with the patient; 4. A history of dentistry for a child to perform simple tasks such as fluoride therapy and fissure sealant and 5. Children in need of class 1 restorative treatment of primary or permanent tooth with infiltration anesthesia. Exclusion criteria included:
1. Patients with the first referral to dentistry;
2. Systemic/mental illness of the child in such a way that prevent the necessary cooperation during the work;
3. Any condition that may affect the sense of smell;
4. A history of anesthesia/allergies
5. Sensitivity to jasmine odor; and
6. Patients with spontaneous pain.
The participants were planned to be randomly selected from the patients referred to the pediatric clinic of Isfahan Dental School. This study was approved by the ethics committee of the Isfahan University of Medical Sciences (Ethical approval: IR.MUI.REC.1398.657) and was registered in the Iranian Registry of Clinical Trials (registration number: IRCT20200218046545N1). All procedures performed were in accordance with the ethical standards of the institutional and national research committee. A detailed information sheet with simple nontechnical language was provided, and parents/ guardians signed an informed consent.
Interventions and Outcomes
The intervention group were treated with jasmine flower aromatherapy. All of the children in the intervention group underwent aromatherapy for 15 minutes, with 2mL of jasmine flower extract, diffused in 50 mL of distilled water, and then diffused in in a waiting room of ten square meters using a candle diffuser. The control group underwent the same procedure, except that distilled water replaced jasmine flower extract in the diffuser. Both groups then underwent the routine procedures of a Class 1 restorative treatment, with administration of infiltration anesthesia using 1/8 milliliter of Lidocaine 2% with epinephrine 1/80000 (Daroopakhsh, Iran). A single pediatric dentist performed all the mentioned procedures in an average duration of approximately 20 minutes, which were uniformly referred to as “procedures” throughout the manuscript.
The outcomes were defined as follows:
1. Anxiety levels during dental procedures: Assessed using a translated version of the Modified Child Dental Anxiety Scale (MCDAS), an 8-item questionnaire where each item is rated on a five-point Likert scale (18). Anxiety was also evaluated through changes in vital signs, including heart rate and blood oxygen saturation, at three time points: immediately before local anesthesia, during injection, and 20 minutes after the procedure.
2. Pain severity during the dental procedure: Measured using a Visual Analogue Scale (VAS), ranging from "no pain" (zero) to "worst possible pain" (ten), where the child indicated the severity of their pain by pointing to the corresponding value. Vital signs were recorded using a digital monitoring device (Pulse Oximeter, Beurer PO80).
Sampling, Randomization, and Blinding
The sampling was carried out in a simple manner, by randomly assessing for eligibility, the referred children to the Isfahan Dental School, and including them in the study after obtaining a form of consent from their parents. As this was the first study assessing the anxiolytic effect of jasmine aromatherapy, the target sample size was set to be 50 patients in total. Aiming to account for possible dropouts, 60 participants were considered to be adequate to be included in the study. After collecting data regarding the general demographics of the patients, the patients were randomly allocated into intervention or control group, using the SPSS v.24 for macOS software (simple randomization). The enrollment of patients, generation of the random allocation, and assignment of interventions were carried out by three separate investigators.
As the intervention involved aromatherapy, it was not possible to blind the care providers and investigators, as they could easily guess the allocation results by smelling. However, the children were blind to and unaware of the study aims and protocol and therefore, allocations.
Statistical Analyses
The SPSS software version 24 for MacOS (IBM Inc., USA) was used for the statistical analyses. Pearson Chi-square and independent samples t-test were used to compare the results between intervention and control groups. One-step univariate and multivariable linear regression models were used to estimate the effect size and precision of outcomes. Variables “age”, “sex”, and “study group” were entered into the models. Statistical significance was considered at 95% level (P<0.05).
Results
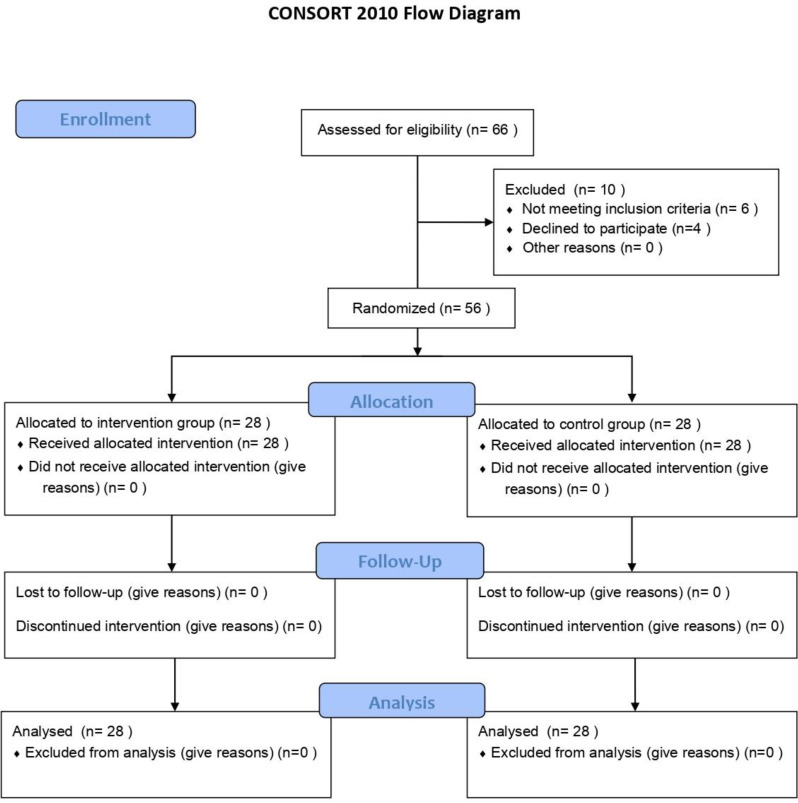
Participants were assessed and enrolled from February 19, 2020 until April 19, 2020. The flow and recruitment details of the participant can be interpreted from the CONSORT flow diagram as demonstrated in Figure 1.
Fig 1.
Allocation flow diagram
The baseline characteristics along with the measured outcomes regarding the children in each group is shown in Table 1. No harms or unintended effects were observed in either of the group.
Table 1.
General demographics and outcomes of all participants (N=28 in both groups)
| Intervention | Control | P | ||
|---|---|---|---|---|
| Mean age±standard deviation | 8.11±1.31 | 8.54±1.67 | 0.29* | |
| Gender | Female | 16 | 15 | 0.79** |
| Male | 12 | 13 | ||
| Mean O2 saturation±standard deviation | Before procedure | 95.54±1.53 | 95.68±1.28 | 0.71* |
| During procedure | 95.71±2.24 | 96.36±1.77 | 0.24* | |
| After procedure | 94.64±1.93 | 95.32±1.94 | 0.19* | |
| Mean heart rate±standard deviation | Before procedure | 98.46±13.49 | 101.14±12.87 | 0.45* |
| During procedure | 101.86±9.93 | 106±10.49 | 0.13* | |
| After procedure | 98.79±11.76 | 99.28±8.68 | 0.86* | |
| Mean MCDAS score±standard deviation | 9.86±3.5 | 11.89±3.69 | 0.04* | |
| Mean VAS score±standard deviation | 0.79±1.57 | 3.07±2.73 | <0.001* |
MCDAS: modified child dental anxiety scale; VAS: visual analogue scale.
Independent samples t-test
Pearson Chi-square
Children in the intervention and control groups did not demonstrate significant difference regarding age, sex, O2 saturation and heart rate before, during, and after dental procedures. The mean MCDAS and VAS scores were significantly lower in the intervention group, confirming the anxiolytic effect of jasmine aromatherapy.
Univariate and multivariable linear regression models showed that being in the intervention group significantly decreased both MCDAS and VAS scores, but showed no significant correlation between age/sex with either MCDAS or VAS scores (Table 2)
Table 2.
Results of univariate and multivariate linear regression
| Outcome | Variables | Univariate | Multivariable | ||
|---|---|---|---|---|---|
| B (95% CI) | P | B (95% CI) | P | ||
| MCDAS score | Age | -0.03 (-0.70, 0.64) | 0.93 | -0.13 (-0.80, 0.53) | 0.69 |
| Sex (ref: female) | -0.42 (-2.44, 1.59) | 0.67 | -0.50 (-2.47, 1.47) | 0.61 | |
| Study group (ref: control) | -2.04 (-3.96, -0.11) | 0.04 | -2.11 (-4.09, -0.13) | 0.04 | |
| VAS score | Age | 0.15 (-0.29, 0.61) | 0.49 | 0.04 (-0.36, 0.45) | 0.83 |
| Gender (ref: female) | -0.88 (-2.22, 0.45) | 0.19 | -0.97 (-2.16, 0.23) | 0.11 | |
| Study group (ref: control) | -2.29 (-3.48, -1.09) | <0.001 | -2.30 (-3.50, -1.10) | <0.001 | |
B: unstandardized beta; CI: confidence interval; ref: reference; MCDAS: modified child dental anxiety scale; VAS: visual analogue scale
Discussion
The results of this study indicate that aromatherapy with jasmine is effective in reducing anxiety and pain perception in pediatric patients. This is the first study to investigate the anxiolytic effect of jasmine aromatherapy in practice, which shows similar effects with recent studies on lavender and orange aromatherapy (14,16,17,19). Still, more investigation is required to determine which of these aromatherapies are more effective.
In several trials across the globe, lavender aromatherapy was proved effective in reducing anxiety and pain perception among children. These trials used different subjective and objective methods of outcome measurement e.g., salivary cortisol levels and face rating scale (FRS) (14), face image scale (FIS), Face, Legs, Activity, Cry, Consolability (FLACC) and Wong-Baker pain rating scale (WBS) (16), State Trait Anxiety Indicator (STAI-6) and Modified Dental Anxiety Scale (MDAS) (19), all of which showed a significant decrease of stress and pain perception in patients on lavender aromatherapy. The evidence regarding jasmine aromatherapy is however, limited to the present study.
Overall, despite being a relatively simple subject, very few studies aimed to evaluate the beneficial effects of aromatherapy as a complementary practice. This may stem in the fact that a lot of practitioners either prejudge these kinds of practices to be ineffective and based on superstitious beliefs, or consider their effects to be too obvious and not worth studying. However, this guard can be broken by taking an evidence-based approach in studying the effects of these cheap and (most probably) harmless complementary therapies, including aromatherapy with jasmine.
Furthermore, this anxiolytic effect may stem in specific substances within aromatic materials, or it simply can be a psychological response to their aromas. Future studies can focus on the underlying mechanisms and possible involved compounds which cause this anxiolytic effect.
Regardless of the underlying mechanism, aromatherapy with jasmine flower extract can be suggested as a cheap and practical complementary method to reduce children’s anxiety and pain perception, lessening the harmful stresses they experience and also assisting the clinicians in their practices.
Some limitations account to this study. Most important of all, the unblindness of the care providers and investigators, which may have introduced a possible bias into the results. Furthermore, limited number of participants and the subjective natures of outcome measurements are among the limitations of this study. Also, the results may not be generalizable to all children, as only the cooperative ones with Frankl +/++ were included in this study.
CONCLUSION
Jasmine aromatherapy has been shown to effectively reduce anxiety and pain perception in children during dental procedures, making it a cost-effective and practical complementary method that can be recommended for use in dental practices.
ACKNOWLEDGMENTS
None declared.
Notes:
Cite this article as: Jafarzadeh Samani M, Ziaei S, Monjezi N, Fazaeli R, Sedaghat N, Panahi H.et al. Anxiolytic Effect of Jasmine Aromatherapy in Pediatric Dental Procedures: A Single-Blinded Randomized Placebo-Controlled Trial Front Dent. 2024:21:39.
CONFLICT OF INTEREST STATEMENT
None declared.
References
- 1.Cianetti S, Lombardo G, Lupatelli E, Pagano S, Abraha I, Montedori A, Caruso S, Gatto R, De Giorgio S, Salvato R. Dental fear/anxiety among children and adolescents. A systematic review. Eur J Paediatr Dent. 2017 Jun;18(2):121–130. doi: 10.23804/ejpd.2017.18.02.07. [DOI] [PubMed] [Google Scholar]
- 2.Armfield JM, Heaton LJ. Management of fear and anxiety in the dental clinic: a review. Aust Dent J. 2013 Dec;58(4):390–407. doi: 10.1111/adj.12118. quiz 531. [DOI] [PubMed] [Google Scholar]
- 3.Cai H, Xi P, Zhong L, Chen J, Liang X. Efficacy of aromatherapy on dental anxiety: A systematic review of randomised and quasi-randomised controlled trials. Oral Dis. 2021 May;27(4):829–847. doi: 10.1111/odi.13346. [DOI] [PubMed] [Google Scholar]
- 4.Packyanathan JS, Lakshmanan R, Jayashri P. Effect of music therapy on anxiety levels on patient undergoing dental extractions. J Family Med Prim Care. 2019 Dec 10;8(12):3854–3860. doi: 10.4103/jfmpc.jfmpc_789_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Soares GABE, Bhattacharya T, Chakrabarti T, Tagde P, Cavalu S. Exploring Pharmacological Mechanisms of Essential Oils on the Central Nervous System. Plants (Basel) 2021 Dec 22;11(1):21. doi: 10.3390/plants11010021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ghiasi A, Bagheri L, Haseli A. A Systematic Review on the Anxiolytic Effect of Aromatherapy during the First Stage of Labor. J Caring Sci. 2019 Mar 1;8(1):51–60. doi: 10.15171/jcs.2019.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mehrnoush V, Darsareh F, Roozbeh N, Ziraeie A. Efficacy of the Complementary and Alternative Therapies for the Management of Psychological Symptoms of Menopause: A Systematic Review of Randomized Controlled Trials. J Menopausal Med. 2021 Dec;27(3):115–131. doi: 10.6118/jmm.21022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Froutan R, Tavousi SH, Sedaghat A, Sadeghnia HR, Layegh M, Mazlom SR. The Effect of Inhalation Aromatherapy on Sedation Level, Analgesic Dosage, and Bispectral Index Values during Donor Site Dressing in Patients with Burns: A Randomized Clinical Trial. Adv Skin Wound Care. 2022 Jan 1;35(1):1–9. doi: 10.1097/01.ASW.0000801544.79621.24. [DOI] [PubMed] [Google Scholar]
- 9.Marsh E, Millette D, Wolfe A. Complementary Intervention in Postoperative Care: Aromatherapy's Role in Decreasing Postoperative Nausea and Vomiting. J Holist Nurs. 2022 Dec;40(4):351–358. doi: 10.1177/08980101211065555. [DOI] [PubMed] [Google Scholar]
- 10.Contrada M, Cerasa A, Tonin P, Bagetta G, Scuteri D. Aromatherapy in Stroke Patients: Is it Time to Begin? Front Behav Neurosci. 2021 Dec 8;15:749353. doi: 10.3389/fnbeh.2021.749353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee J, Hur MH. The Effects of Aroma Essential Oil Inhalation on Stress, Pain, and Sleep Quality in Laparoscopic Cholecystectomy Patients: A Randomized Controlled Trial. Asian Nurs Res (Korean Soc Nurs Sci). 2022 Feb;16(1):1–8. doi: 10.1016/j.anr.2021.11.002. [DOI] [PubMed] [Google Scholar]
- 12.Nirmala K, Kamatham R. Effect of Aromatherapy on Dental Anxiety and Pain in Children Undergoing Local Anesthetic Administrations: A Randomized Clinical Trial. J Caring Sci. 2021 Aug 23;10(3):111–120. doi: 10.34172/jcs.2021.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jadhav GR, Mittal P. Evaluation of aromatherapy on success rate of inferior alveolar nerve block in teeth with irreversible pulpitis: a prospective randomized clinical trial. Quintessence Int. 2020;51(10):864–870. doi: 10.3290/j.qi.a45172. [DOI] [PubMed] [Google Scholar]
- 14.Ghaderi F, Solhjou N. The effects of lavender aromatherapy on stress and pain perception in children during dental treatment: A randomized clinical trial. Complement Ther Clin Pract. 2020 Aug;40:101182. doi: 10.1016/j.ctcp.2020.101182. [DOI] [PubMed] [Google Scholar]
- 15.Benli M, Olson J, Huck O, Özcan M. A novel treatment modality for myogenous temporomandibular disorders using aromatherapy massage with lavender oil: A randomized controlled clinical trial. Cranio. 2023 Jan;41(1):48–58. doi: 10.1080/08869634.2020.1819067. [DOI] [PubMed] [Google Scholar]
- 16.Arslan I, Aydinoglu S, Karan NB. Can lavender oil inhalation help to overcome dental anxiety and pain in children? A randomized clinical trial. Eur J Pediatr. 2020 Jun;179(6):985–992. doi: 10.1007/s00431-020-03595-7. [DOI] [PubMed] [Google Scholar]
- 17.Jafarzadeh M, Arman S, Pour FF. Effect of aromatherapy with orange essential oil on salivary cortisol and pulse rate in children during dental treatment: A randomized controlled clinical trial. Adv Biomed Res. 2013 Mar;2:10. doi: 10.4103/2277-9175.107968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Howard KE, Freeman R. Reliability and validity of a faces version of the Modified Child Dental Anxiety Scale. Int J Paediatr Dent. 2007 Jul;17(4):281–8. doi: 10.1111/j.1365-263X.2007.00830.x. [DOI] [PubMed] [Google Scholar]
- 19.Kritsidima M, Newton T, Asimakopoulou K. The effects of lavender scent on dental patient anxiety levels: a cluster randomised-controlled trial. Community Dent Oral Epidemiol. 2010 Feb;38(1):83–7. doi: 10.1111/j.1600-0528.2009.00511.x. [DOI] [PubMed] [Google Scholar]