Abstract
BACKGROUND
Meniscus extrusion occurs in most elderly individuals and most patients after meniscus allograft transplantation. The risk factors and correlative factors of meniscus extrusion have been extensively studied. However, for using tendon autograft for meniscus reconstruction, both graft type and surgical method are different from those in previous studies on meniscus extrusion.
AIM
To identify predictive factors for coronal and sagittal graft extrusion length after using tendon autograft for medial meniscus reconstruction.
METHODS
Ten patients who underwent medial meniscus reconstruction with tendon autograft were selected for this retrospective observational study. The graft extrusions and potential factors were measured and correlation and regression analyses were performed to analyze their relationships.
RESULTS
The medial graft extrusion correlated with the preoperative bilateral hip-knee-ankle angle difference, preoperative Kellgren-Lawrence grade, preoperative relative joint space width, and preoperative bilateral medial edge incline angle difference. The anterior graft correlated with the anterior tunnel edge distance at 1 week after operation. The posterior graft extrusion correlated with the preoperative bilateral hip-knee-ankle angle difference, preoperative relative joint space width, and posterior tunnel edge distance at 1 week after operation. The mean graft extrusion correlated with the preoperative bilateral hip-knee-ankle angle difference and preoperative relative joint space width. The preoperative joint space width and anterior and posterior tunnel edge distance at 1 week can be used to predict the medial, anterior, posterior, and mean graft extrusion length.
CONCLUSION
The preoperative joint space width and tunnel position can be used to predict the coronal and sagittal graft extrusion length after using tendon autograft for medial meniscus reconstruction.
Keywords: Meniscus, Extrusion, Reconstruction, Autograft, Graft
Core Tip: Meniscus extrusion in the natural meniscus and meniscus allograft transplantation have been extensively studied but there are no studies on meniscus extrusion after using tendon for meniscus reconstruction. This study found that the preoperative joint space width and tunnel position at 1 week after operation could be used to predict the coronal and sagittal graft extrusion length at 1 week and 8 mo after using tendon autograft for medial meniscus reconstruction. This knowledge offers information for patient selection and surgical points of using tendon autograft for meniscus reconstruction.
INTRODUCTION
After subtotal or total meniscectomy, the onset and progression of osteoarthritis are hard to avoid because of the absence of the meniscus[1]. To delay the process of degeneration of the articular cartilage and restore the function of the meniscus, materials for meniscal replacement, including meniscus allografts and tendon autografts, have been used[2].
Meniscus extrusion occurs in more than 70% of the elderly individuals, and it is considered a risk factor for osteoarthritis[3,4]. The risk factors of natural meniscus extrusion may include female sex, meniscal tear, and higher baseline value of extrusion[5]. Similarly, graft extrusions occur in half or even most meniscus allografts after meniscus allograft transplantation although the relationship between graft extrusion and clinical outcome remains unknown[6]. Studies found that incorrect bone block position, relatively large meniscus allograft, and large osteophyte in peripheral tibial plateau could contribute to graft extrusion[7-9]. For using tendon autograft for meniscus reconstruction, both the graft and surgical method are different from those used for meniscus allograft transplantation[2]. To our knowledge, there are no studies on graft extrusion after using tendon for meniscus reconstruction, thus the potential risk factors of graft extrusion are unclear.
The aim of this study was to explore the potential predictive factors for coronal and sagittal graft extrusion after using tendon autograft for medial meniscus reconstruction. It was hypothesized that factors that are pre-existing and can directly influence the force of the graft can be used to predict the coronal and sagittal graft extrusion length.
MATERIALS AND METHODS
Patients
This retrospective observational study was approved by the Ethics Committee of Dalian University Affiliated Xinhua Hospital (document number: 2024-43-02). Ten patients who underwent medial meniscus reconstruction with tendon autograft between July 2021 and February 2023 were selected for the analysis. The inclusion criteria were medial meniscus reconstruction with tendon autograft, a preoperative anteroposterior knee radiograph, a preoperative anteroposterior lower limb radiograph, a preoperative lateral tibia radiograph, and postoperative magnetic resonance imaging (MRI) images of the knee at 1 week and 8 mo. The exclusion criteria were integrity, resolution, contrast, or position of the bone, bone tunnel, or tendon graft in a radiograph or on MRI images that did not meet the standard required for the accurate measurement in the study. Meniscus reconstructions were performed in selected patients. Indications included meniscus deficiency, pain, and < 50 years of age. Contraindications included irreparable chondral injury, malalignment, ligamentous laxity, arthrofibrosis, or active infection.
MR VB17A (Siemens) with a magnetic field strength of 1.5T was used to acquire proton-density weighted turbo spin-echo fat-suppressed coronal and sagittal MRI images and proton-density weighted BLADE fat-suppressed axial MRI images. CXDI NE 213014 (Canon) was used to acquire radiographs.
Surgical technique
All surgeries were performed by a senior surgeon. The tendon autograft was harvested and threaded. The anatomic anterior and posterior meniscus root tunnels for medial meniscus reconstruction were drilled. Subtotal or total meniscectomy was carried out. The corresponding part of the joint capsule or remnant meniscus was debrided to obtain a bleeding surface. The prepared tendon was pulled into the tibial tunnels and sutured to the joint capsule or meniscus remnant. The tension of the tendon was adjusted and the threads were fixed.
Evaluation of MRI images and radiographs
The x and y coordinates of the anchor points for the measurement were accurate to at least 1 pixel. The blind method was used for the evaluation.
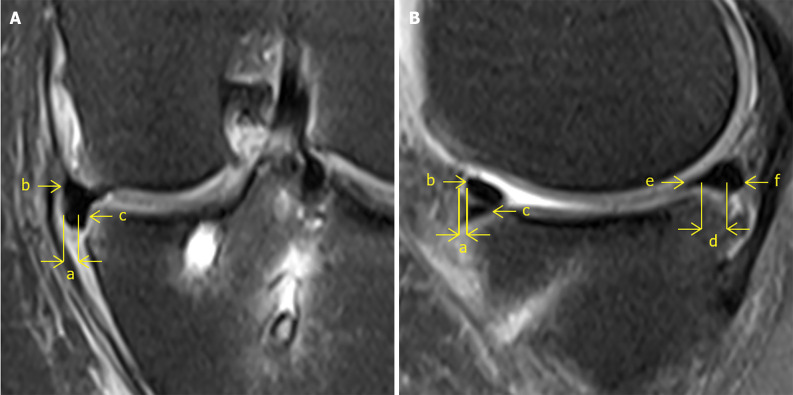
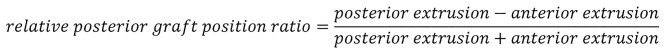
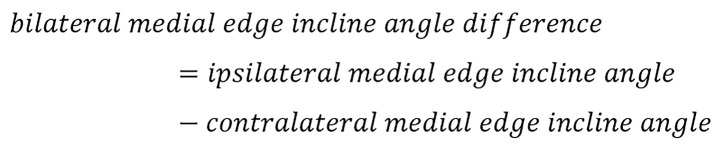
The slices where the joint space width was the narrowest on postoperative coronal and sagittal knee MRI images were used to measure the medial extrusion and anterior and posterior extrusion (Figure 1). The absolute value of the degree of graft extrusion was measured as the horizontal distance from the most peripheral aspect of the graft to the edge of the tibia. The mean extrusion was calculated as the arithmetic mean of the medial, anterior, and posterior extrusion. The relative posterior graft position ratio was calculated by dividing the value of subtracting the anterior extrusion from the posterior extrusion by the value of adding the posterior anterior extrusion and the anterior extrusion.
Figure 1.
The absolute value of the degree of graft extrusion, measured as the horizontal distance from the most peripheral aspect of the graft to the edge of the tibia measured on the slice that the medial joint space is the narrowest on coronal and sagittal knee magnetic resonance imaging. A: Medial extrusion. a: The absolute value of medial extrusion; b: Meniscus remnant; c: Tendon graft; B: Anterior and posterior extrusiona. a: The absolute value of anterior extrusion; b: Tendon graft; c: Meniscus remnant; d: The absolute value of posterior extrusion; e: Tendon graft; f: Meniscus remnant.
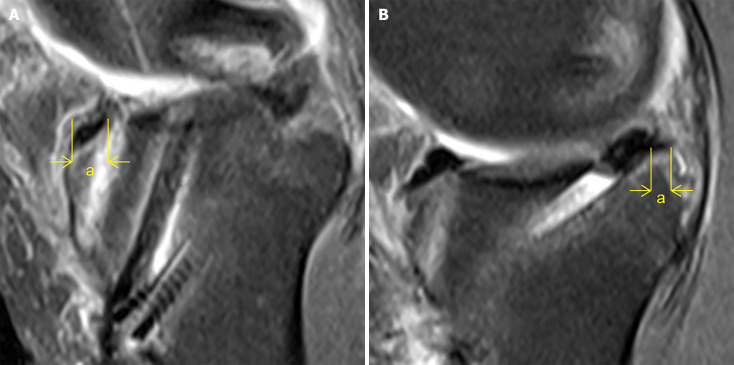
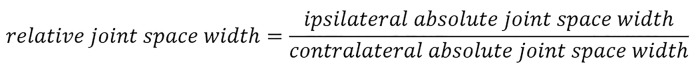
The slices where the anterior and posterior meniscus root tunnel entrances were the widest on the sagittal knee MRI images at 1 week after operation were used to measure the anterior and posterior tunnel edge distance, respectively (Figure 2). The tunnel edge distance was measured as the horizontal distance from the intraarticular tunnel entrance to the edge of the tibia.
Figure 2.
Tunnel edge distance, measured as the horizontal distance from the intraarticular tunnel entrance to the edge of the tibia measured on the slice where the tunnel entrance is the widest on sagittal knee magnetic resonance imaging. A: Anterior tunnel edge distance (indicated by the letter “a”); B: Posterior tunnel edge distance (indicated by the letter “a”).
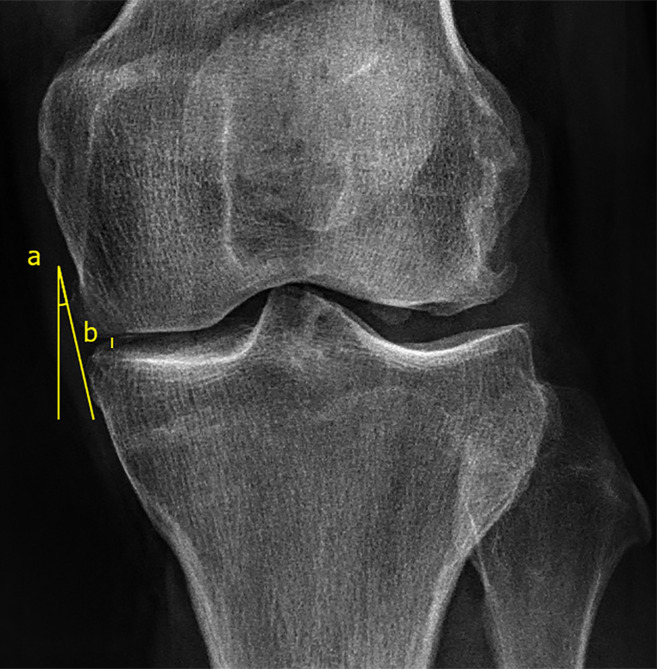
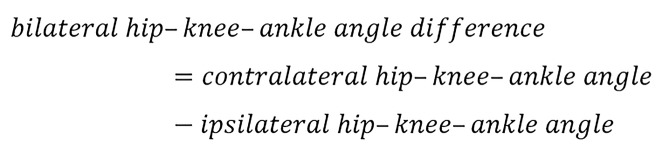
The preoperative anteroposterior knee radiograph was used to measure the medial edge incline angle and absolute joint space width and assess the Kellgren-Lawrence grade (Figure 3). The medial edge incline angle was measured as the degree of the incline angle formed by the common tangent to the medial edge of the femur and tibia and the vertical line. If the medial edge of the femur was medial to that of the tibia, the value was determined as positive and vice versa. The bilateral medial edge incline angle difference was calculated by subtracting the contralateral medial edge incline angle from the ipsilateral medial edge incline angle.
Figure 3.
Medial edge incline angle and medial joint space measured on anteroposterior knee radiograph. a: Medial edge incline angle, measured as the degree of the incline angle formed by the common tangent to the medial edge of the femur and tibia and the vertical line; b: Medial joint space, measured as the length of the vertical line segment from the medial edge of the tibia plateau to the femoral condyle.
The absolute joint space width was measured as the length of the vertical line segment from the medial edge of the tibial plateau to the femoral condyle. The relative joint space width was calculated by dividing the ipsilateral absolute joint space width by the contralateral absolute joint space width.
The preoperative anteroposterior lower limb radiograph was used to measure the hip-knee-ankle angle, which was measured as the degree of the medial angle formed by the line from the hip center to the knee center and the line from the knee center to the ankle center. The center of the femoral head was regarded as the hip center. The center of the bases of the tibial spines was regarded as the knee center. The center of the talus was regarded as the ankle center. The bilateral hip-knee-ankle angle difference was calculated by subtracting the ipsilateral hip-knee-ankle angle from the contralateral hip-knee-ankle angle.
The preoperative lateral tibia radiograph was used to measure the medial posterior tibial slope, which was measured as the degree of the posterior inferior angle formed by the line from the anterior edge to the posterior edge of the medial tibia plateau and the long axis of the tibia.
Statistical analysis
GraphPad Prism 9 was used for all statistical analyses. For the description of the demographics, the mean and standard deviation were calculated for measurement data and the number of each portion was calculated for enumeration and ranked data. The correlations between the graft extrusions and the potential factors, between the sagittal graft extrusions and the tunnel edge distances, and between the relative posterior graft position ratio and the preoperative medial posterior tibial slope were computed. Two patients were excluded from the correlation analysis between the relative posterior graft position ratio and the preoperative medial posterior tibial slope because of the additional anterior closing wedge high tibial osteotomy. The factors that are preexisting and can directly influence the force of the graft were selected for the regressions. The regressions between the graft extrusions and the potential factors were computed by simple linear regression and least squares multiple linear regression to explore good predictive models for the medial, anterior, posterior, and mean extrusions. If the P value of the analysis of variance ≤ 0.05, the R squared value ≥ 0.6, and the variance inflation factor of the multicollinearity ≤ 5, the model was regarded as a good predictive model for graft extrusion.
RESULTS
Demographics
The medial, anterior, posterior, and mean extrusion of the tendon grafts at 1 week after operation were 1.00 ± 1.90, -3.42 ± 2.34, 0.13 ± 2.90, and -0.76 ± 2.05 mm, respectively. The medial, anterior, posterior, and mean extrusions of the tendon grafts at 8 mo after operation were 1.73 ± 2.38, 2.90 ± 2.39, 0.07 ± 2.72, and 0.49 ± 0.76 mm, respectively (Table 1).
Table 1.
Demographics
|
Variable
|
Description
|
| Age (year) | 36.10 ± 4.98 |
| Gender, male/female | 6/4 |
| Body mass index | 28.30 ± 4.80 |
| Preoperative medial posterior tibial slope (°) | 14.42 ± 2.39 |
| Preoperative Kellgren-Lawrence grade, grade 0/grade 1/grade 2/grade 3 | 2/3/2/3 |
| Preoperative hip-knee-ankle angle (°) | 175.40 ± 3.86 |
| Preoperative bilateral hip-knee-ankle angle difference (°) | 2.13 ± 3.00 |
| Preoperative absolute joint space width (mm) | 3.09 ± 0.77 |
| Preoperative relative joint space width | 0.68 ± 0.12 |
| Preoperative medial edge incline angle (°) | 6.68 ± 9.68 |
| Preoperative bilateral medial edge incline angle difference (°) | 4.88 ± 7.87 |
| Anterior tunnel edge distance (mm) | 5.93 ± 3.42 |
| Posterior tunnel edge distance (mm) | 11.23 ± 6.15 |
| 1 wk after operation | |
| Medial extrusion (mm) | 1.00 ± 1.90 |
| Anterior extrusion (mm) | -3.46 ± 2.29 |
| Posterior extrusion (mm) | 0.13 ± 2.90 |
| Mean extrusion (mm) | -0.76 ± 2.05 |
| Relative posterior graft position ratio | -0.08 ± 1.09 |
| 8 mo after operation | |
| Medial extrusion (mm) | 1.73 ± 2.38 |
| Anterior extrusion (mm) | -2.90 ± 2.39 |
| Posterior extrusion (mm) | 1.38 ± 4.43 |
| Mean extrusion (mm) | 0.07 ± 2.72 |
| Relative posterior graft position ratio | 0.49 ± 0.76 |
Measurement data are given as the mean ± SD. Enumeration and ranked data are given as numbers of each portion.
Correlations between graft extrusions and potential factors
The medial extrusion at 1 week after operation correlated with the preoperative Kellgren-Lawrence grade, preoperative bilateral hip-knee-ankle angle difference, preoperative absolute joint space width, preoperative relative joint space width, preoperative bilateral medial edge incline angle difference, anterior extrusion, and posterior extrusion. The medial extrusion at 8 mo after operation correlated with the preoperative Kellgren-Lawrence grade, preoperative hip-knee-ankle angle, preoperative bilateral hip-knee-ankle angle difference, preoperative relative joint space width, preoperative bilateral medial edge incline angle difference, and posterior extrusion (Table 2). The anterior extrusion at 1 week after operation correlated with the medial extrusion and anterior tunnel edge distance. The anterior extrusion at 8 mo after operation correlated with the anterior tunnel edge distance (Tables 2 and 3). The posterior extrusion at 1 week after operation correlated with the preoperative bilateral hip–knee–ankle angle difference, preoperative absolute joint space width, preoperative relative joint space width, preoperative bilateral medial edge incline angle difference, medial extrusion, and posterior tunnel edge distance. The posterior extrusion at 8 mo after operation correlated with the preoperative bilateral hip–knee–ankle angle difference, preoperative relative joint space width, medial extrusion, and posterior tunnel edge distance (Tables 2 and 3). The mean extrusion at 1 week after operation correlated with the preoperative bilateral hip-knee-ankle angle difference, preoperative relative joint space width, medial extrusion, anterior extrusion, and posterior extrusion. The mean extrusion at 8 mo after operation correlated with the preoperative bilateral hip-knee-ankle angle difference, preoperative relative joint space width, medial extrusion, and posterior extrusion. The relative posterior graft position ratio at 1 week after operation correlated with the preoperative medial posterior tibial slope (Table 4).
Table 2.
Correlations between graft extrusions and potential factors
|
Medial extrusion
|
Anterior extrusion
|
Posterior extrusion
|
Mean extrusion
|
|||||
|
Pearson r
|
P value
|
Pearson r
|
P value
|
Pearson r
|
P value
|
Pearson r
|
P value
|
|
| 1 wk after operation | ||||||||
| Preoperative medial posterior tibial slope | 0.259 | 0.575 | 0.375 | 0.360 | 0.381 | 0.399 | 0.362 | 0.425 |
| Preoperative Kellgren-Lawrence grade | 0.646 | 0.044a | 0.125 | 0.732 | 0.543 | 0.105 | 0.488 | 0.152 |
| Preoperative hip-knee-ankle angle | -0.580 | 0.079 | -0.127 | 0.727 | -0.625 | 0.053 | -0.518 | 0.125 |
| Preoperative bilateral hip-knee-ankle angle difference | 0.736 | 0.015a | 0.272 | 0.448 | 0.725 | 0.018a | 0.661 | 0.038a |
| Preoperative absolute joint space width | -0.672 | 0.034a | -0.218 | 0.545 | -0.668 | 0.035a | -0.591 | 0.072 |
| Preoperative relative joint space width | -0.934 | 0.000a | -0.575 | 0.082 | -0.795 | 0.006a | -0.873 | 0.001a |
| Preoperative medial edge incline angle | 0.332 | 0.349 | -0.006 | 0.987 | 0.455 | 0.186 | 0.311 | 0.382 |
| Preoperative bilateral medial edge incline angle difference | 0.678 | 0.031a | 0.133 | 0.713 | 0.756 | 0.011a | 0.604 | 0.064 |
| Medial extrusion | 0.711 | 0.021a | 0.733 | 0.016a | 0.914 | 0.000a | ||
| Anterior extrusion | 0.711 | 0.021a | 0.480 | 0.160 | 0.818 | 0.004a | ||
| Posterior extrusion | 0.733 | 0.016a | 0.480 | 0.160 | 0.872 | 0.001a | ||
| 8 mo after operation | ||||||||
| Preoperative medial posterior tibial slope | 0.643 | 0.357 | -0.265 | 0.735 | 0.469 | 0.531 | 0.415 | 0.585 |
| Preoperative Kellgren-Lawrence grade | 0.832 | 0.040a | 0.142 | 0.789 | 0.575 | 0.233 | 0.596 | 0.212 |
| Preoperative hip-knee-ankle angle | -0.890 | 0.018a | -0.142 | 0.789 | -0.799 | 0.056 | -0.735 | 0.096 |
| Preoperative bilateral hip-knee-ankle angle difference | 0.962 | 0.002a | 0.398 | 0.434 | 0.867 | 0.025a | 0.868 | 0.025a |
| Preoperative absolute joint space width | -0.723 | 0.105 | -0.208 | 0.692 | -0.675 | 0.142 | -0.638 | 0.173 |
| Preoperative relative joint space width | -0.940 | 0.005a | -0.266 | 0.610 | -0.887 | 0.018a | -0.834 | 0.039a |
| Preoperative medial edge incline angle | 0.509 | 0.302 | -0.398 | 0.434 | 0.229 | 0.662 | 0.156 | 0.767 |
| Preoperative bilateral medial edge incline angle difference | 0.848 | 0.033a | -0.052 | 0.921 | 0.625 | 0.185 | 0.571 | 0.236 |
| Medial extrusion | 0.324 | 0.531 | 0.844 | 0.035a | 0.854 | 0.031a | ||
| Anterior extrusion | 0.324 | 0.531 | 0.614 | 0.194 | 0.721 | 0.106 | ||
| Posterior extrusion | 0.844 | 0.035a | 0.614 | 0.194 | 0.985 | 0.000a | ||
P value ≤ 0.05.
Table 3.
Correlations between sagittal graft extrusions and tunnel edge distances
|
Anterior extrusion
|
Posterior extrusion
|
|||
|
Pearson r
|
P value
|
Pearson r
|
P value
|
|
| 1 wk after operation | ||||
| Anterior tunnel edge distance | -0.753 | 0.012a | -0.151 | 0.676 |
| Posterior tunnel edge distance | -0.349 | 0.323 | -0.658 | 0.039a |
| 8 mo after operation | ||||
| Anterior tunnel edge distance | -0.910 | 0.012a | -0.634 | 0.177 |
| Posterior tunnel edge distance | -0.728 | 0.101 | -0.942 | 0.005a |
P value ≤ 0.05.
Table 4.
Correlations between relative posterior graft position ratio and preoperative medial posterior tibial slope
|
Relative posterior graft position ratio
|
||
|
Pearson r
|
P value
|
|
| 1 wk after operation | ||
| Preoperative medial posterior tibial slope | 0.800 | 0.031a |
| 8 mo after operation | ||
| Preoperative medial posterior tibial slope | 0.147 | 0.854 |
P value ≤ 0.05.
Two patients were excluded from the analysis because of the additional anterior closing wedge high tibial osteotomy.
Regressions between graft extrusions and potential factors
The preoperative relative joint space width could be used to predict the medial and mean extrusion length at 1 week and 8 mo after operation. The anterior tunnel edge distance at 1 week after operation could be used to predict the anterior extrusion length at 1 week and 8 mo after operation. The preoperative relative joint space and the posterior tunnel edge distance could be used to predict the posterior extrusion length at 1 week and 8 mo after operation (Table 5).
Table 5.
Regressions between graft extrusions and potential factors
|
y
|
Standardized
|
Equation
|
P value
|
R
2
|
|||
|
Regression
|
x1
|
x1
|
x1
|
||||
|
Preoperative relative joint space width
|
Anterior tunnel edge distance
|
Posterior tunnel edge distance
|
|||||
| 1 wk after operation | |||||||
| Medial extrusion | Yes | y = -14.6x1 + 68.9 | 0.000 | 0.000 | 0.873 | ||
| No | y = -0.0604x1 + 0.737 | ||||||
| Anterior extrusion | Yes | y = -9.755x2 + 5.77 | 0.006 | 0.006 | 0.632 | ||
| No | y = -1.185x2 + 1.831 | ||||||
| Posterior extrusion | Yes | y = -0.6192x1 - 0.3481x3 + 86.65 | 0.009 | 0.024 | 0.132 | 0.741 | |
| No | y = -14.75x1 - 0.1744x3 + 12.07 | ||||||
| Mean extrusion | Yes | y = -12.6x1 + 44.6 | 0.001 | 0.001 | 0.763 | ||
| No | y = -0.0523x1 + 0.63 | ||||||
| 8 mo after operation | |||||||
| Medial extrusion | Yes | y = -15.13x1 + 88.34 | 0.005 | 0.005 | 0.884 | ||
| No | y = -0.04563x1 + 0.7183 | ||||||
| Anterior extrusion | Yes | y = -16.80x2 - 6.641 | 0.012 | 0.012 | 0.827 | ||
| No | y = -0.9522x2 + 2.994 | ||||||
| Posterior extrusion | Yes | y = -0.3597x1 - 0.6639x3 + 99.15 | 0.016 | 0.232 | 0.078 | 0.936 | |
| No | y = -14.09x1 - 0.5704x3 + 17.02 | ||||||
| Mean extrusion | Yes | y = -11.74x1 + 62.93 | 0.039 | 0.039 | 0.696 | ||
| No | y = -0.0354x1 + 0.6417 | ||||||
DISCUSSION
The most important finding of the study was that the preoperative joint space width and tunnel position at 1 week after operation could be used to predict the coronal and sagittal graft extrusion length at 1 week and 8 mo after using tendon autograft for medial meniscus reconstruction. The hypothesis of the study was confirmed. Additionally, the medial, anterior, posterior, or mean extrusion at 1 week or 8 mo correlated with the preoperative Kellgren-Lawrence grade; preoperative hip-knee-ankle angle or bilateral hip-knee-ankle angle difference; preoperative absolute or relative joint space width; preoperative bilateral medial edge incline angle difference; or anterior or posterior tunnel edge distance at 1 week after operation. This knowledge offers information for patient selection and surgical points of using tendon autograft for meniscus reconstruction.
The joint space width reflects the ability of joint space to accommodate the meniscus because of the direct contacts between the meniscus and femoral condyle and tibial plateau. A study compared the preoperative absolute and relative joint space width between patients with graft extrusion (≥ 3 mm) and graft nonextrusion (< 3 mm) at 1 year after meniscal allograft transplantation. The study found no difference in joint space width between patients with graft extrusion and those with graft nonextrusion[10]. However, this study found that the preoperative joint space width can be used to predict medial, posterior, and mean graft extrusion at 1 week and 8 mo after operation. There are several possible reasons for this difference. First, the tendon autograft is softer than the meniscus allograft and it is therefore more susceptible to the contact area of femoral condyle and tibial plateau. In a study using semitendinosus tendon for meniscus reconstruction in rabbits, the tendon autografts might need 6 weeks to generate as many chondrocytes as the natural meniscus. For the hardness, the time might be 24 weeks[11]. Considering that the life cycle of rabbits is shorter than that of humans, it may take more time for tendon autograft in humans to construct the mechanical structure like the natural meniscus so as to achieve adequate hardness and avoid extrusion under the pressure of the femoral condyle and tibial plateau. In this study, the observation that general extrusion at 8 mo after operation was greater than that at 1 week after operation also demonstrated that enough time is needed for the tendon to be remodeled into the meniscus. Second, the joint space width was measured as the length of the vertical line segment from the medial edge of the tibial plateau to the femoral condyle in this study in order to ensure that the measure position was close to the graft midbody, since the measurement method of joint space width varied across studies. Third, that study did not differentiate the medial meniscus and lateral meniscus in study design, while our study concentrated on the medial meniscus.
The position of the meniscus root may affect meniscus extrusion because of the action and reaction force between adjacent tissues. The ratio of the distance between the edge of the lateral tibial plateau and the center of the bone bridge to the tibial plateau length and the distance between the interspinal groove and the middle of the bone bridge were demonstrated to correlate with the coronal extrusion after lateral meniscus transplantation[12]. Similarly, the axial trough angle, the angle between the long axis of the bone trough and the line perpendicular to the common tangent to the medial and lateral posterior tibial condylar cortexes on axial MRI images, was demonstrated to correlate with the coronal extrusion after lateral meniscus transplantation[13,14]. For medial meniscus transplantation, the distance between the anterior bone plug and the line perpendicular to the common tangent to the medial and lateral posterior tibial condylar cortexes and passing through the posterior cruciate ligament on axial MRI images was found to be associated with the coronal extrusion[15]. All these studies found that the closer the meniscus root is to the ipsilateral edge of the tibial plateau, the greater the likelihood that the coronal extrusion will occur. However, when it comes to using tendon for meniscus reconstruction, the intraarticular length of the tendon graft can be adjusted after the bone tunnels are drilled, hence the tunnel position hardly affects the magnitude but rather the direction of the force on the graft. Therefore, the relationship between the coronal tunnel position and the coronal graft extrusion was not investigated in this study. In addition, a study assessed the ratio of the anteroposterior distance between the tunnel center and the anatomic center to the anteroposterior length of the tibia at 1 week after medial meniscus posterior root pullout repair and posterior meniscus extrusion at 3 mo after operation, and no correlation was found[16]. However, the present study found that the tunnel edge distance, measured as the anteroposterior distance from the intraarticular tunnel entrance to the edge of the tibia, can be used to predict anterior and posterior graft extrusion at 1 week and 8 mo after operation. The possible reason for this difference is that the tendon autograft is softer than the meniscus allograft and its sagittal extrusion is therefore more susceptible to its sagittal tunnel position.
The hip-knee-ankle angle, the reflection of lower limb alignment, may influence meniscus extrusion because it determines the distribution of the load between medial and lateral knee joint. A study evaluated the hip–knee–ankle angle and coronal extrusion of the medial meniscus within 3 mo from the first consultation in those suspected of having knee disease or injury. A correlation between the hip-knee-ankle angle and meniscus extrusion was demonstrated[17]. Similarly, this study found that the preoperative bilateral hip-knee-ankle angle difference correlated with the medial, posterior, and mean graft extrusions at 1 week and 8 mo after operation. At first glance, the hip-knee-ankle angle is also a good factor to be chosen for the predictive model for graft extrusion in this study, since it correlates with the extrusion of both the natural meniscus and tendon graft. However, considering that the joint space can more directly influence the force of the graft, the hip-knee-ankle was not chosen.
The medial edge incline angle, measured as the degree of the incline angle formed by the common tangent to the medial edge of the femur and tibia and the vertical line, was used to reflect the relationship between the medial femoral condyle and the medial tibial plateau in the mediolateral direction. To our knowledge, there are no studies on this relationship in the field of meniscus extrusion. This study found that the preoperative bilateral medial edge incline angle difference correlated with the medial and posterior graft extrusion at 1 week and the medial graft extrusion at 8 mo after operation. Because the function that medial meniscus restricts lateral tibial translation, which is equal to medial femoral translation, implies that medial femoral condyle exerts a force toward the medial side on the medial meniscus, medial femoral translation may contribute to medial graft extrusion[18]. Since the posterior graft extrusion was measured on the slice that the joint space width was the narrowest of the sagittal knee on MRI images, the medial femoral translation made the corresponding tibial plateau at the relative medial portion of the medial tibial plateau. In this condition, the anteroposterior length of the tibial plateau might decrease, and the posterior graft extrusion might increase. As a result, the medial femoral translation might contribute to the posterior graft extrusion.
Kellgren-Lawrence grade has been extensively used to assess knee arthrosis according to bone morphology. Kellgren-Lawrence grade was found to correlate with the coronal extrusion of the medial meniscus in both early knee osteoarthritis and medial meniscus posterior horn tear[19,20]. Two studies analyzed the preoperative Kellgren-Lawrence grade and the coronal extrusion of the lateral meniscus at 1 year following meniscus allograft transplantation. One failed to find an association between them[21]. The other found that among the knees with grades 0, 1, and 2, the meniscus extrusion was more likely to occur in the knees with grade 1 compared with those with grade 0[14]. In this study, the preoperative Kellgren-Lawrence grade correlated with the medial graft extrusion at 1 week and 8 mo after operation. Since the tendon autograft is softer than the meniscus allograft and Kellgren-Lawrence grade involves joint space, which determined the degree of graft extrusion in this study, tendon autograft may be more susceptible to bone morphology than meniscus allograft.
The posterior tibial slope can influence the force on the femoral condyle and meniscus. A study found that the knees with a posterior tibial slope of 15° exerted greater force on the medial meniscus posterior roots with the joints loaded in compression compared with those with a posterior tibial slope of 10°[22]. Similarly, this study found that the preoperative posterior tibial slope correlated with the relative posterior graft position ratio at 1 week after operation.
There may be a relationship among medial, anterior, and posterior extrusions of the meniscus since they are adjacent tissues. However, a study found no correlation between the medial, anterior, and posterior extrusions of the medial meniscus on immediate postoperative MRI images after meniscus allograft transplantation[23]. Nevertheless, this study found that the medial extrusion correlated with the posterior extrusion at 1 week and 8 mo after operation. In addition, the medial extrusion correlated with the anterior extrusion at 1 week after operation. Interestingly, the correlation between the medial extrusion and posterior extrusion was stronger than that between the medial extrusion and anterior extrusion. Similarly, the most important risk factor for the medial and posterior extrusions was the preoperative joint space width while the most important risk factor for the anterior extrusion was the anterior tunnel edge distance in this study. The anatomical characteristic of the medial meniscus that anterior root attachment is anterior to the center of the anterior horn and posterior root attachment is anterior to the center of the posterior horn helps to explain these findings. In theory, the characteristic determines that radially inward tension and radially outward compression on the anterior horn are weaker than those on the posterior horn, which has been confirmed in a previous study[24]. In theory, the characteristic also determines that the influence of the position of anterior root attachment on anterior extrusion is stronger than that of posterior root attachment on posterior extrusion since the resistance of the femoral condyle is weaker.
This study had several strengths. First, the longitudinal study in which the images used to measure almost all the correlative factors were acquired ahead of the images used to measure the graft extrusions was helpful to explore the causal link while most studies on meniscus extrusion were cross-sectional. Second, this study not only found that many factors correlated with the coronal and sagittal graft extrusion, but also proposed models with good fitness that can be used to predict the medial, anterior, posterior, and mean extrusion length since no studies on graft extrusion after using tendon autograft for meniscus reconstruction could be found. Third, to our knowledge, the sample size was the largest among clinical studies on using tendon autograft for meniscus reconstruction since other studies included no more than several patients.
This study had several limitations. First, the sample size was small, which might contribute to random errors. Second, the respective slices where the joint space width was the narrowest on coronal and sagittal knee MRI images were used to measure the medial extrusion and anterior and posterior extrusions, respectively. The method that using graft extrusion measured on a particular slice to represent graft extrusion might contribute to systematic errors. Third, there might be some correlative factors or risk factors for graft extrusion that this study neglected.
CONCLUSION
The preoperative joint space width and tunnel position can be used to predict the coronal and sagittal graft extrusion length after using tendon autograft for medial meniscus reconstruction. This knowledge offers information for patient selection and surgical points of using tendon autograft for meniscus reconstruction.
Footnotes
Institutional review board statement: This study was reviewed and approved by the Ethics Committee of Dalian University Affiliated Xinhua Hospital (document number: 2024-43-02).
Informed consent statement: Patients were not required to give informed consent to the study because the analysis used anonymous clinical data that were obtained after each patient agreed to treatment by written consent.
Conflict-of-interest statement: All the authors report no relevant conflicts of interest for this article.
STROBE statement: The authors have read the STROBE Statement-checklist of items-and the manuscript was prepared and revised according to the STROBE Statement-checklist of items.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade C
Novelty: Grade B
Creativity or Innovation: Grade B
Scientific Significance: Grade B
P-Reviewer: Gao Y S-Editor: Qu XL L-Editor: Wang TQ P-Editor: Yu HG
Contributor Information
Tian-Wang Zhu, Department of Sports Medicine, Dalian University Affiliated Xinhua Hospital, Dalian 116021, Liaoning Province, China.
Xian-Xiang Xiang, Department of Sports Medicine, Dalian University Affiliated Xinhua Hospital, Dalian 116021, Liaoning Province, China.
Chun-Hui Li, Department of Sports Medicine, Dalian University Affiliated Xinhua Hospital, Dalian 116021, Liaoning Province, China.
Rui-Xin Li, Department of Sports Medicine, Dalian University Affiliated Xinhua Hospital, Dalian 116021, Liaoning Province, China. m-cc@163.com.
Nan Zhang, Department of Spine Surgery, Dalian University Affiliated Xinhua Hospital, Dalian 116021, Liaoning Province, China.
Data sharing statement
No additional data are available.
References
- 1.Papalia R, Del Buono A, Osti L, Denaro V, Maffulli N. Meniscectomy as a risk factor for knee osteoarthritis: a systematic review. Br Med Bull. 2011;99:89–106. doi: 10.1093/bmb/ldq043. [DOI] [PubMed] [Google Scholar]
- 2.Goble EM, Verdonk R, Kohn D. Arthroscopic and open surgical techniques for meniscus replacement--meniscal allograft transplantation and tendon autograft transplantation. Scand J Med Sci Sports. 1999;9:168–176. doi: 10.1111/j.1600-0838.1999.tb00449.x. [DOI] [PubMed] [Google Scholar]
- 3.Kaneko H, Ishijima M, Aoki T, Negishi Y, Liu L, Arita H, Momoeda M, Arepati A, Ji X, Someya Y, Tamura Y, Watada Y, Kawamori R, Kaneko K. Prevalence of medial meniscus extrusion in elderly persons -the bunkyo health study. Osteoarthritis Cartilage. 2020;28:S295. [Google Scholar]
- 4.Emmanuel K, Quinn E, Niu J, Guermazi A, Roemer F, Wirth W, Eckstein F, Felson D. Quantitative measures of meniscus extrusion predict incident radiographic knee osteoarthritis--data from the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2016;24:262–269. doi: 10.1016/j.joca.2015.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang F, Kumm J, Svensson F, Turkiewicz A, Frobell R, Englund M. Risk factors for meniscal body extrusion on MRI in subjects free of radiographic knee osteoarthritis: longitudinal data from the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2016;24:801–806. doi: 10.1016/j.joca.2015.12.003. [DOI] [PubMed] [Google Scholar]
- 6.Lee DH. Incidence and Extent of Graft Extrusion following Meniscus Allograft Transplantation. Biomed Res Int. 2018;2018:5251910. doi: 10.1155/2018/5251910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee SY, Yoon J, Cho YS, Son RC, Kim SK, Ahn SH, Lee HK. Various factors contribute to graft extrusion in lateral meniscus allograft transplantation. Knee Surg Sports Traumatol Arthrosc. 2017;25:374–382. doi: 10.1007/s00167-015-3882-3. [DOI] [PubMed] [Google Scholar]
- 8.Jang SH, Kim JG, Ha JG, Shim JC. Reducing the size of the meniscal allograft decreases the percentage of extrusion after meniscal allograft transplantation. Arthroscopy. 2011;27:914–922. doi: 10.1016/j.arthro.2011.02.017. [DOI] [PubMed] [Google Scholar]
- 9.Jeon B, Kim JM, Kim JM, Lee CR, Kim KA, Bin SI. An osteophyte in the tibial plateau is a risk factor for allograft extrusion after meniscus allograft transplantation. Am J Sports Med. 2015;43:1215–1221. doi: 10.1177/0363546515570462. [DOI] [PubMed] [Google Scholar]
- 10.Lee SM, Bin SI, Kim JM, Lee BS, Lee CR, Son DW, Park JG. Long-term Outcomes of Meniscal Allograft Transplantation With and Without Extrusion: Mean 12.3-Year Follow-up Study. Am J Sports Med. 2019;47:815–821. doi: 10.1177/0363546518825251. [DOI] [PubMed] [Google Scholar]
- 11.Li C, Hu X, Meng Q, Zhang X, Zhu J, Dai L, Cheng J, Zhong M, Shi W, Ren B, Zhang J, Fu X, Duan X, Ao Y. The potential of using semitendinosus tendon as autograft in rabbit meniscus reconstruction. Sci Rep. 2017;7:7033. doi: 10.1038/s41598-017-07166-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choi NH, Yoo SY, Victoroff BN. Position of the bony bridge of lateral meniscal transplants can affect meniscal extrusion. Am J Sports Med. 2011;39:1955–1959. doi: 10.1177/0363546511407614. [DOI] [PubMed] [Google Scholar]
- 13.Lee DH, Kim JM, Lee BS, Kim KA, Bin SI. Greater axial trough obliquity increases the risk of graft extrusion in lateral meniscus allograft transplantation. Am J Sports Med. 2012;40:1597–1605. doi: 10.1177/0363546512447932. [DOI] [PubMed] [Google Scholar]
- 14.Ahn JH, Kang HW, Yang TY, Lee JY. Multivariate Analysis of Risk Factors of Graft Extrusion After Lateral Meniscus Allograft Transplantation. Arthroscopy. 2016;32:1337–1345. doi: 10.1016/j.arthro.2015.12.050. [DOI] [PubMed] [Google Scholar]
- 15.Yoon KH, Lee HW, Park SY, Kim JS, Park JY. Centralized anterior bone plug results in less graft extrusion in patients undergoing medial meniscus allograft transplantation following anterior cruciate ligament reconstruction. Knee. 2020;27:884–890. doi: 10.1016/j.knee.2020.02.014. [DOI] [PubMed] [Google Scholar]
- 16.Kamatsuki Y, Furumatsu T, Hiranaka T, Okazaki Y, Okazaki Y, Kodama Y, Hino T, Masuda S, Miyazawa S, Ozaki T. Placement of an anatomic tibial tunnel significantly improves the medial meniscus posterior extrusion at 90° of knee flexion following medial meniscus posterior root pullout repair. Knee Surg Sports Traumatol Arthrosc. 2021;29:1025–1034. doi: 10.1007/s00167-020-06070-w. [DOI] [PubMed] [Google Scholar]
- 17.Goto N, Okazaki K, Akiyama T, Akasaki Y, Mizu-Uchi H, Hamai S, Nakamura S, Nakashima Y. Alignment factors affecting the medial meniscus extrusion increases the risk of osteoarthritis development. Knee Surg Sports Traumatol Arthrosc. 2019;27:2617–2623. doi: 10.1007/s00167-018-5286-7. [DOI] [PubMed] [Google Scholar]
- 18.Zhang Y, Huang W, Yao Z, Ma L, Lin Z, Wang S, Huang H. Anterior Cruciate Ligament Injuries Alter the Kinematics of Knees With or Without Meniscal Deficiency. Am J Sports Med. 2016;44:3132–3139. doi: 10.1177/0363546516658026. [DOI] [PubMed] [Google Scholar]
- 19.Sekiya I, Katano H, Guermazi A, Miura Y, Okanouchi N, Tomita M, Masumoto J, Kitazume Y, Koga H, Ozeki N. Association of AI-determined Kellgren-Lawrence grade with medial meniscus extrusion and cartilage thickness by AI-based 3D MRI analysis in early knee osteoarthritis. Sci Rep. 2023;13:20093. doi: 10.1038/s41598-023-46953-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee DH, Lee BS, Kim JM, Yang KS, Cha EJ, Park JH, Bin SI. Predictors of degenerative medial meniscus extrusion: radial component and knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2011;19:222–229. doi: 10.1007/s00167-010-1274-2. [DOI] [PubMed] [Google Scholar]
- 21.Lee BS, Kim JM, Kim JM, Kim KA, Bin SI. Patient-related risk factors for the extrusion of lateral meniscal allograft transplants. Arthroscopy. 2015;31:699–706. doi: 10.1016/j.arthro.2014.10.016. [DOI] [PubMed] [Google Scholar]
- 22.Melugin HP, Brown JR, Hollenbeck JFM, Fossum BW, Whalen RJ, Ganokroj P, Provencher CMT. Increased Posterior Tibial Slope Increases Force on the Posterior Medial Meniscus Root. Am J Sports Med. 2023;51:3197–3203. doi: 10.1177/03635465231195841. [DOI] [PubMed] [Google Scholar]
- 23.Lee DH, Lee CR, Jeon JH, Kim KA, Bin SI. Graft extrusion in both the coronal and sagittal planes is greater after medial compared with lateral meniscus allograft transplantation but is unrelated to early clinical outcomes. Am J Sports Med. 2015;43:213–219. doi: 10.1177/0363546514555699. [DOI] [PubMed] [Google Scholar]
- 24.Walker PS, Arno S, Bell C, Salvadore G, Borukhov I, Oh C. Function of the medial meniscus in force transmission and stability. J Biomech. 2015;48:1383–1388. doi: 10.1016/j.jbiomech.2015.02.055. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No additional data are available.