Abstract
BACKGROUND
Artificial intelligence (AI) is a branch of computer science that allows machines to analyze large datasets, learn from patterns, and perform tasks that would otherwise require human intelligence and supervision. It is an emerging tool in pediatric orthopedic surgery, with various promising applications. An evaluation of the current awareness and perceptions among pediatric orthopedic surgeons is necessary to facilitate AI utilization and highlight possible areas of concern.
AIM
To assess the awareness and perceptions of AI among pediatric orthopedic surgeons.
METHODS
This cross-sectional observational study was conducted using a structured questionnaire designed using QuestionPro online survey software to collect quantitative and qualitative data. One hundred and twenty-eight pediatric orthopedic surgeons affiliated with two groups: Pediatric Orthopedic Chapter of Saudi Orthopedics Association and Middle East Pediatric Orthopedic Society in Gulf Cooperation Council Countries were surveyed.
RESULTS
The pediatric orthopedic surgeons surveyed had a low level of familiarity with AI, with more than 60% of respondents rating themselves as being slightly familiar or not at all familiar. The most positively rated aspect of AI applications for pediatric orthopedic surgery was their ability to save time and enhance productivity, with 61.97% agreeing or strongly agreeing, and only 4.23% disagreeing or strongly disagreeing. Our participants also placed a high priority on patient privacy and data security, with over 90% rating them as quite important or highly important. Additional bivariate analyses suggested that physicians with a higher awareness of AI also have a more positive perception.
CONCLUSION
Our study highlights a lack of familiarity among pediatric orthopedic surgeons towards AI, and suggests a need for enhanced education and regulatory frameworks to ensure the safe adoption of AI.
Keywords: Artificial intelligence, Pediatric orthopedics, Surgeon awareness, Data security, Patient privacy, Healthcare technology, Medical education, Orthopedic surgery
Core Tip: This study highlights the significant gap in pediatric orthopedic surgeons’ familiarity with artificial intelligence (AI), and shows the need for improved AI education in healthcare. Our results also indicate a high willingness to adopt AI tools, and a positive attitude towards its integration into practice. Moreover, our findings emphasize the importance of patient data security, and point to the need for regulatory oversight over the integration of AI so that it can be implemented safely.
INTRODUCTION
Artificial intelligence (AI) is a branch of computer science that allows machines to analyze large datasets, learn from patterns, and perform tasks that would otherwise require human intelligence and supervision[1,2]. Worldwide, many countries are investing in and utilizing AI in healthcare, including the United States, Canada, China, and several European countries[3-6]. For example, the Chinese State Council released a guideline on the development of AI, and indicated that extensive application of AI will advance the level of precision in medical services and relieve obstacles in healthcare distribution[6].
In the middle east, Gulf countries such as Saudi Arabia, Qatar, and the United Arab Emirates have also emerged as leaders in the development of AI regulations and applications in healthcare[7,8]. These nations have made significant investments in AI, leading to their high rankings in global AI indices[7,8]. Institutions such as the United Arab Emirates’s ministry of state for AI, Qatar’s center for AI at Hamad Bin Khalifa University, and Saudi Arabia’s Saudi Data and AI Authority (SDAIA) aim to guide AI’s integration into various sectors, including healthcare[7,8].
In Saudi Arabia specifically, the field of AI has made considerable progress in recent years, partly due to government programs and initiatives[9]. AI is increasingly being used to transform healthcare, aligned with the goals of Saudi’s vision 2030 which aims to position the country among the global leaders in healthcare[9]. The strategies employed include developing the country’s digital healthcare and expanding AI capabilities[8,10]. The SDAIA, established in August 2019 by a Royal Decree, aims to drive the utilization of AI to help achieve the goals of vision 2030[8]. Studies have shown that AI is becoming more integrated into Saudi healthcare, with a 2022 study by Mirza et al[11] reporting that 7% of Saudi radiology residents regularly use AI, and another study revealing that 25% of dental professionals in the country utilize AI software or applications[12].
Furthermore, the adoption and application of AI in the various fields of medicine are growing[1]. For instance, AI has shown success in effectively aiding endoscopic polyp detection, identifying skin malignancies, and aiding in the diagnosis of diabetic retinopathy[2,13,14]. AI also has the potential to improve decision-making in difficult situations[15]. For example, clinical decision support systems (CDSS) are software applications that operate by matching patient characteristics with the clinical knowledge database. The system then generates individualized assessments and recommendations to aid the clinician in complex decision-making[16].
Pediatric orthopedics, a subspecialty of orthopedics, has the potential to greatly benefit from the application of AI. The nature of the field, which deals with the growing and developing bones of children, is quite different from adult orthopedics and general medicine and faces unique challenges[17]. Pediatric orthopedics specialize in treating disorders of the musculoskeletal system in children and teenagers including a wide range of conditions such as growth disorders, congenital disorders, cancers of the skeletal and muscular systems, and various other diseases[18-20]. About half of all children will experience a fracture at some point in their youth[18,21], with an approximate incidence of 133.1 fractures per 10000 children annually[18,22]. These fractures represent a significant cause of long-term disability in children and occur in 55% of those who have suffered physical abuse[23]. Additionally, emergency physicians may miss about 11% of acute pediatric fractures compared to specialist pediatric radiologists[20]. This discrepancy may be due to the different stages of bone maturation and diverse patterns of injury such as bowing fracture, metaphyseal injuries, and torus fractures[18,19]. According to Sharaf[17], pediatric orthopedics can benefit from AI in supporting and personalizing disease diagnosis, optimizing surgeries, and guiding rehabilitation. For instance, AI tools, such as BoneView (Gleamer, Paris, France) the first clinical AI application, have been developed to aid in diagnosing fractures and detecting effusion, dislocations, and focal bone lesions in both adult and pediatric patients[17,24]. This software employs advanced algorithms to identify lesions on X-rays, visually highlighting areas of interest. Notably, BoneView has demonstrated a 30% reduction in undetected fractures and a 15% decrease in radiograph reading time, marking a substantial advancement over conventional imaging techniques[17,24]. Another innovation in the field is the OrthoNext digital platform (Orthofix Medical Inc., Lewisville, TX, United States) which was recently approved by the United States Food and Drug Administration for preoperative surgical planning in pediatric orthopedics[25]. Other AI applications in pediatric orthopedics, such as bone age assessment, early tumor detection using convolutional neural networks, machine learning, and robot-assisted surgery, are contributing to advancements in the field[17,25-27].
Despite the significant benefits of AI in healthcare, its adoption by the medical community, including pediatric orthopedic surgeons, faces significant challenges. Studies have shown that there is limited awareness and education among physicians regarding the capabilities and applications of AI in their field[28,29]. Many medical professionals are not familiar with the details of AI, its algorithms, or how it can be integrated into their practice[28,29]. According to a recent article[30], the lack of awareness and transparency surrounding AI applications is a major ethical issue that leads to a lack of trust in AI. Trust could increase confidence in AI tools, and understanding the technology, its potential benefits, and its limitations is crucial for building this trust. However, apprehension regarding AI-generated recommendations may delay its adoption[30]. Another challenge is the integration of AI tools into the existing clinical workflow, as any disruption to established routines may cause resistance[31]. Furthermore, concerns about data security and patient privacy can be a significant barrier to the adoption of AI technologies[31]. A study involving 501 pharmacy professionals from the Middle East and North Africa revealed that 58.9% of participants were worried about patient data privacy and cybersecurity threats, and 67% believed there is a lack of legal regulation[32]. These findings underscore the necessity for ethical guidelines and regulatory frameworks to address these concerns and build trust in AI technologies.
Therefore, given the important role of AI in pediatric orthopedics, in addition to the rapid progression of AI in medicine, it is crucial to assess the perspectives and opinions of physicians and surgeons. Understanding their key thoughts and concerns could facilitate and promote a smoother transition to AI utilization. This study focused on assessing the views of pediatric orthopedics on AI in general rather than for specific tools, as this broader understanding may assist in identifying overarching concerns and barriers to AI adoption, rather than specific-use cases. According to an article by Wang et al[33], without the involvement of users in the design and evaluation processes, it is nearly impossible to successfully implement and apply AI-CDSS in the clinical context. Several studies have assessed the attitudes and perspectives of physicians from different specialties regarding AI[28,29,34]. A study by Oh et al[28] reported that 62% of Korean physicians surveyed agreed that AI offers an advantage of quickly obtaining clinically relevant data. Another study[34] assessing Turkish orthopedic surgeons found that less than half were familiar with AI. A recent article[29] surveying Sudanese orthopedic surgeons reported an overall lack of knowledge on the basic concepts of AI. Furthermore, medico-legal issues appear to be a recurring theme in the discussion surrounding AI[28,29]. Nonetheless, several authors have noted that research assessing the perspective of physicians on AI remains scarce[35-37]. However, to the best of our knowledge, this is this first study to assess the opinions and perceptions of pediatric orthopedic surgeons regarding the various aspects of AI.
The primary objective of this study was to assess the awareness and perceptions of AI among pediatric orthopedic surgeons. Furthermore, we assessed the importance of various barriers to AI adoption, along with surgeons’ interest in learning more about AI and their outlook on its future applications.
MATERIALS AND METHODS
Study design
This cross-sectional observational study was carried out using a structured questionnaire designed using QuestionPro online survey software (https://www.questionpro.com) to collect quantitative and qualitative data from pediatric orthopedic surgeons. The study design was chosen to effectively capture a snapshot of the current awareness, perceptions, and attitudes of a large sample of pediatric orthopedic surgeons regarding AI. This design also enables the identification of patterns and correlations in attitudes towards AI without the need for long-term follow-up[38].
Participants
The study population consisted of pediatric orthopedic surgeons who met the following eligibility criteria: (1) Actively practicing in one of the Gulf Cooperation Council countries; (2) Affiliated with either the Pediatric Orthopedic Chapter of the Saudi Orthopedics Association or the Middle East Pediatric Orthopedic Society; and (3) Specialized training in pediatric orthopedics. The participants represented a diverse group of professionals with various backgrounds, levels of experience, and practice settings, ensuring a broad perspective on the topics being studied. Surgeons were invited to participate in the survey and were given a defined period of 4 weeks to complete it.
Variables
The main domains in the study were demographics, familiarity with AI, perceptions of AI, willingness to adopt AI, factors affecting decision-making, and future outlook on AI. The demographic factors collected were age, years of experience, main hospital affiliation, region of practice, and place of fellowship. Questions regarding the other domains were mainly collected using 5-point Likert scales to measure respondents’ perspectives. The survey concluded with the following open-ended question: “Please provide any thoughts or comments on the role of AI in pediatric orthopedic surgery. You may include any additional insights, concerns, or suggestions related to its implementation.” This question was designed to provide participants the opportunity to share further insights or perspectives that might not have been captured through closed-ended questions.
Measurement
The questionnaire was developed by reviewing the existing literature for relevant challenges and perspectives regarding AI adoption in healthcare and in pediatric orthopedics specifically, using both closed-ended questions and an open-ended question to capture a range of information and opinions from the study sample.
The questionnaire was pilot tested with three experts in pediatric orthopedics and adjusted based on their feedback, which was incorporated to enhance the questionnaire’s content and face validity. As this study relies on self-reported data, information bias, particularly recall and observer bias, may have arisen. To mitigate this, we carefully designed the survey with clear, structured questions. Additionally, anonymity was ensured to encourage honest and accurate responses. Regarding the open-ended question, the authors independently reviewed the responses to identify key themes and patterns. These themes were then discussed collectively to categorize the repeating themes into the overall analysis to provide a deeper understanding of the participants’ perspectives on AI in pediatric orthopedics.
Study size
A specialized social media group, which currently consists of 128 pediatric orthopedic surgeons from the two aforementioned groups, was used to estimate the population size and therefore calculate the required sample size. Using the formula denoted by Cross and Daniel[39], taking into account a 95% confidence interval and 8% margin of error, the study required 69 participants to adequately represent the population. Participant selection was conducted through convenient sampling, with emphasis placed on the availability of their contact details. The abovementioned group was used to distribute the survey electronically.
Statistical analysis
Data from closed-ended questions were analyzed using statistical product and service solutions statistics version 22 (International Business Machines Corporation, Armonk, NY, United States), employing basic descriptive statistics and inferential statistics as appropriate.
Descriptive statistics summarized the sample’s demographic traits. Answers to questions based on the 5-point Likert scale were presented using tables and bar graphs that displayed the surgeons’ familiarity with AI, perceptions of AI, willingness to adopt AI, factors affecting decision-making, and future outlook on AI. Results to the open-ended question were analyzed and summarized by the authors.
For the inferential statistics, the Likert scales under each domain were combined to give a total domain score for each respondent. The Kruskal-Wallis H test was used to evaluate significant associations between demographic variables and the surgeon’s future outlook using the following study domains: familiarity; perception; willingness; and factors affecting decision-making.
For all tests, the level of significance was set at P ≤ 0.05. The results are presented as the median and interquartile range of each domain for all demographic variables. Further bivariate correlation between study domains was preformed using Spearman’s rank correlation coefficient.
Ethical approval for this study was obtained from the institutional review board of Imam Abdulrahman Bin Faisal University (No. IRB-UGS-2023-01-530; Dammam, Saudi Arabia). Participants were informed of the study’s purpose, methodology, requirements, and duration before enrollment. It was explained that participation is voluntary, and participants can withdraw at any time. By voluntarily participating, informed consent was implied. No identifiers were collected, and the anonymity and confidentiality of participants were strictly maintained, with results presented in aggregate form.
RESULTS
A total of 128 pediatric orthopedic surgeons affiliated with two groups the Pediatric Orthopedic Chapter of Saudi Orthopedics Association and Middle East Pediatric Orthopedic Society in Gulf Cooperation Council Countries were contacted using a specialized social media group from December 2023 through February 2024. Seventy-one surgeons completed the survey, all of whom were included in the final analyses.
Demographics
Most respondents in the study were under 40-year-old (47%), followed closely by those aged 40 to 60 (45%). Most pediatric orthopedic surgeons included in the study had less than 10 years of experience (58%), whereas only 13% had more than 20 years of experience. The largest portion of respondents was affiliated with Ministry of Health hospitals (37%). Most of the participants were from the central region of Saudi Arabia (41%), whereas only 7% were practicing surgeons outside Saudi Arabia. The highest number of respondents completed their fellowship in Saudi Arabia (44%), followed by North America (32%) (Table 1).
Table 1.
Participants’ demographic characteristics, n (%)
|
Variables
|
Subcategory
|
Frequency (n = 71)
|
| Age in years | < 40 | 33 (46.5) |
| 40-60 | 32 (45.1) | |
| > 60 | 6 (8.5) | |
| Experience as a pediatric orthopedic surgeon in years | < 10 | 41 (57.8) |
| 11-20 | 21 (29.6) | |
| > 20 | 9 (12.7) | |
| Main hospital affiliation | University | 15 (21.1) |
| 1Military | 14 (19.7) | |
| Ministry of health | 26 (36.6) | |
| Specialist or medical city | 11 (15.5) | |
| Private | 5 (7.0) | |
| Region of practice | Central | 29 (40.9) |
| Northern | 2 (2.8) | |
| Southern | 9 (12.7) | |
| Eastern | 13 (18.3) | |
| Western | 13 (18.3) | |
| 2Outside Saudi Arabia | 5 (7.0) | |
| Place of fellowship | Saudi Arabia | 31 (43.7) |
| Northern America (Canada and United States) | 23 (32.4) | |
| Europe | 11 (15.5) | |
| 3Others | 6 (8.5) |
Military, Security forces, National guard.
Bahrain, Kuwait (1), Oman (3), Qatar (1), Egypt (1).
Other places of fellowship include Eastern Asia (2), while others were not specified.
Survey responses
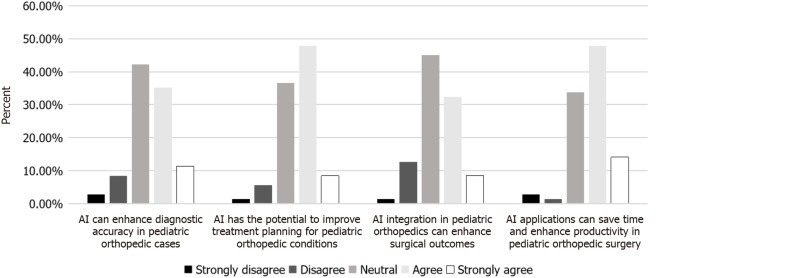
Participant responses to the survey questions are shown in Table 2 and Table 3. Regarding the perceptions of pediatric orthopedic surgeons towards AI, almost 50% of the respondents agreed or strongly agreed that AI can enhance diagnostic accuracy in pediatric orthopedic cases. Similarly, more than 56% of them agreed or strongly agreed that AI has the potential to improve treatment planning for pediatric orthopedic conditions (Figure 1 and Table 2).
Table 2.
Participants’ questionnaire responses, n (%)
|
Topical category
|
Response categories and data
|
||||
| Perceptions towards AI | Strongly disagree | Disagree | Neutral | Agree | Strongly agree |
| AI can enhance diagnostic accuracy in pediatric orthopedic cases | 2 (2.8) | 6 (8.5) | 30 (42.3) | 25 (35.2) | 8 (11.3) |
| AI has the potential to improve treatment planning for pediatric orthopedic conditions | 1 (1.4) | 4 (5.6) | 26 (36.6) | 34 (47.9) | 6 (8.5) |
| AI integration in pediatric orthopedics can enhance surgical outcomes | 1 (1.4) | 9 (12.7) | 32 (45.1) | 23 (32.4) | 6 (8.5) |
| AI applications can save time and enhance productivity in pediatric orthopedic surgery | 2 (2.8) | 1 (1.4) | 24 (33.8) | 34 (47.9) | 10 (14.1) |
| Familiarity with AI | Not at all familiar | Slightly familiar | Moderately familiar | Very familiar | Extremely familiar |
| How familiar are you with AI in medicine? | 18 (25.4) | 26 (36.6) | 24 (33.8) | 2 (2.8) | 1 (1.4) |
| Willingness to adopt AI tools | Very unwilling | Somewhat unwilling | Neutral | Somewhat willing | Very willing |
| How willing are you to adopt AI-based tools or systems in your clinical practice, if they are proven to be safe and effective? | 0 (0) | 0 (0) | 9 (12.7) | 30 (42.3) | 32 (45.1) |
| Factors affecting decision making | Not important at all | Slightly important | Moderately important | Quite important | Highly important |
| Evidence-based research supporting AI in pediatric orthopedics | 0 (0) | 4 (5.6) | 13 (18.3) | 19 (26.8) | 35 (49.3) |
| Trust in the accuracy of AI-driven diagnostics | 1 (1.4) | 6 (8.5) | 12 (16.9) | 21 (29.6) | 31 (43.7) |
| Support and training provided for AI utilization | 1 (1.4) | 0 (0) | 13 (18.3) | 18 (25.4) | 39 (54.9) |
| Protection of patient privacy and data security with AI implementation | 1 (1.4) | 2 (2.8) | 4 (5.6) | 16 (22.5) | 48 (67.6) |
| Ease of integration of AI systems into current practice | 0 (0.0) | 2 (2.8) | 13 (18.3) | 22 (31.0) | 34 (47.9) |
| Interest in learning about AI | Very uninterested | Somewhat uninterested | Neutral | Somewhat interested | Very interested |
| How interested are you in learning more about AI and how to apply them in your clinical practice? | 0 (0) | 3 (4.2) | 8 (11.3) | 24 (33.8) | 36 (50.7) |
AI: Artificial intelligence.
Table 3.
Participants’ questionnaire responses continued, n (%)
|
Topical category
|
Response categories and data
|
| 1Which of the following AI tools have you encountered? | |
| AI speech-to-text tools (e.g., mobius conveyor, the nuance dragon ambient experience, augmedix) | 23 (32.4) |
| Image analysis tools (e.g., nuance’s precision imaging network, zebra medical vision) | 16 (22.5) |
| AI clinical decision support tools (e.g., Sepsis Watch, ChatGPT 35/4) | 14 (19.7) |
| Surgical support tools (e.g., Da Vinci surgical system, ActivSight system) | 10 (14.1) |
| None of the above | 34 (47.9) |
| Would you recommend a tested and proven AI tool in pediatric orthopedic surgery to other clinicians? | |
| Yes | 64 (91.4) |
| No | 6 (8.6) |
| What role do you think AI will play in pediatric orthopedic surgery over the next 5 to 10 years? | |
| It will not have a significant impact | 2 (2.8) |
| It will be used in a limited capacity | 31 (43.7) |
| It will become a fundamental part of the field | 23 (32.4) |
| Uncertain | 15 (21.1) |
Participants can choose one, more than one, or not at all.
AI: Artificial intelligence.
Figure 1.
Perceptions towards artificial intelligence. Nearly 50% of respondents agree or strongly agree that artificial intelligence (AI) can enhance diagnostic accuracy in pediatric orthopedics, while over 56% believe it can improve treatment planning. Additionally, 41% agree that AI integration can enhance surgical outcomes. The most positively rated aspect was AI’s ability to save time and boost productivity, with 62% in agreement. AI: Artificial intelligence.
Regarding participant answers to whether AI integration in pediatric orthopedics can enhance surgical outcomes, 41% agreed or strongly agreed with that statement. Finally, the most positively rated aspect of AI applications for pediatric orthopedic surgery was found to be the perception of its ability to save time and enhance productivity, with 62% agreeing or strongly agreeing with that statement. Regarding surgeons’ familiarity with AI tools, most of the respondents were slightly familiar with AI in medicine (37%), followed by 34% who were moderately familiar (Table 2).
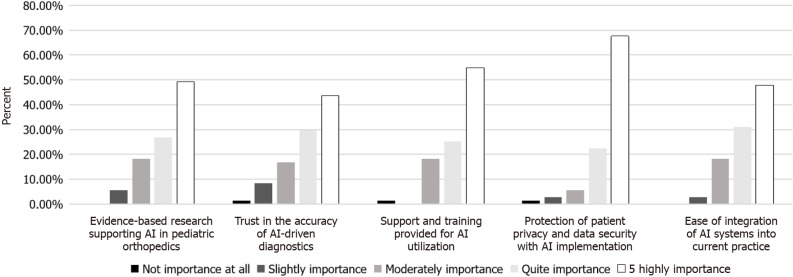
Almost half of the respondents considered evidence-based research supporting AI in pediatric orthopedics to be highly important, followed by 27% who rated it as quite important. Similarly, trust in the accuracy of AI-driven diagnostics was highly important for 44% and quite important for 30% of the participants. Support and training provided for AI utilization were also rated as highly important by more than half of the respondents, and 25% rated it as quite important (Figure 2).
Figure 2.
Factors affecting decision-making. Almost half of the respondents rated evidence-based research on artificial intelligence (AI) in pediatric orthopedics as highly important, with 27% considering it quite important. Trust in the accuracy of AI-driven diagnostics was highly important for 44% and quite important for 30%. Over half of the respondents found support and training for AI utilization highly important, with 25% rating it as quite important. The top priority was patient privacy and data security, with 68% rating it as highly important and 23% as quite important. Lastly, 48% viewed ease of AI integration into current practice as highly important, with 31% considering it quite important.
Protection of patient privacy and data security with AI implementation was the most highly rated priority for the surgeons, as 68% rated it as highly important and 23% as quite important. Finally, ease of integration of AI systems into current practice was highly important for 48% and quite important for 31% of the participants (Figure 2).
Most of the respondents were very willing to adopt AI-based tools or systems (45%), followed by 42% who were somewhat willing (Table 2). In addition, almost all of the respondents agreed that they would recommend a tested and proven AI-tool to their peers (91%) (Table 3). Furthermore, more than half of the respondents were very interested in learning about AI and its application in clinical practice, followed by 34% who were somewhat interested (Table 3). Overall, our results indicated a high level of willingness to adopt AI-based tools or systems and a strong tendency to recommend them to their peers.
The most common AI tool that the surgeons encountered was AI speech-to-text tools (e.g., Mobius Conveyor, The Nuance Dragon Ambient eXperience, Augmedix), which are being utilized by 32% of the respondents in the study. Overall, the pediatric orthopedic surgeons surveyed have limited exposure to AI tools in their field (Table 3).
Regarding the expected role of AI in pediatric orthopedic surgery in the next 5 years to 10 years, the majority (44%) believed that it will be used in a limited capacity, followed by 32% who believed it will become a fundamental part of the field. A small proportion of the participants (3%) believed it will not have a significant impact. Overall, the pediatric orthopedic surgeons had a high level of interest in learning about AI and its application in clinical practice and a moderate to high expectation of its role in their field in the near future (Table 3).
Subgroup analysis
Only one demographic variable appeared to be significantly related to the surgeon’s familiarity with AI, namely, the physician’s years of experience (Kruskal-Wallis H test = 7.037; P = 0.030). Participants with 11 years to 20 years of experience had significantly higher familiarity scores compared to physicians with more than 20 years of experience (Table 4).
Table 4.
Factors related to the domains in the study
|
Variables
|
Subcategory
|
Familiarity
|
Perception
|
Willingness
|
Decision-making
|
||||
|
Median (IQR)
|
4
P value
|
Median (IQR)
|
4
P value
|
Median (IQR)
|
4
P value
|
Median (IQR)
|
4
P value
|
||
| Age in years | < 40 | 2.0 (1) | 1.722 (0.423) | 19.0 (5) | 1.723 (0.422) | 5.0 (1) | 0.619 (0.734) | 23.0 (7) | 0.030 (0.985) |
| 40-60 | 2.0 (2) | 18.5 (5) | 5.0 (1) | 22.5 (5) | |||||
| > 60 | 1.5 (2) | 16.0 (5) | 5.0 (2) | 21.0 (7) | |||||
| Experience in years | < 10 | 2.0 (1) | 7.326 (0.026)a | 18.0 (4) | 7.037 (0.030)a | 5.0 (1) | 1.409 (0.494) | 23.0 (6) | 0.287 (0.866) |
| 11-20 | 3.0 (1) | 20.0 (5) | 5.0 (1) | 22.0 (5) | |||||
| > 20 | 1.0 (2) | 15.0 (5) | 5.0 (2) | 21.0 (8) | |||||
| Hospital affiliation | University | 3.0 (2) | 1.575 (0.813) | 18.0 (6) | 6.079 (0.193) | 6.0 (1) | 1.141 (0.888) | 22.0 (6) | 1.744 (0.783) |
| 1Military | 2.0 (1) | 19.5 (3) | 5.0 (1) | 24.0 (6) | |||||
| Ministry of Health | 2.0 (2) | 18.5 (4) | 5.0 (1) | 23.0 (6) | |||||
| 2Specialist | 2.0 (1) | 17.0 (3) | 5.0 (1) | 21.0 (9) | |||||
| Private | 2.0 (2) | 15.0 (4) | 5.0 (1) | 19.0 (6) | |||||
| Region | Central region | 3.0 (1) | 9.019 (0.108) | 19.0 (6) | 3.464 (0.629) | 5.0 (1) | 6.033 (0.303) | 24.0 (6) | 8.445 (0.133) |
| Northern | 2.5 (0) | 18.5 (0) | 6.0 (0) | 24.5 (0) | |||||
| Southern | 1.0 (2) | 17.0 (4) | 5.0 (2) | 22.0 (6) | |||||
| Eastern | 2.0 (2) | 20.0 (6) | 6.0 (2) | 22.0 (5) | |||||
| Western | 2.0 (1) | 17.0 (6) | 5.0 (2) | 19.0 (10) | |||||
| Gulf countries | 2.0 (1) | 17.0 (3) | 5.0 (1) | 21.0 (5) | |||||
| Fellowship | Saudi Arabia | 2.0 (2) | 1.055 (0.788) | 17.0 (6) | 1.063 (0.786) | 5.0 (1) | 2.053 (0.561) | 24.0 (6) | 5.545 (0.136) |
| 3Northern America | 2.0 (1) | 19.0 (5) | 5.0 (1) | 21.0 (6) | |||||
| Europe | 2.0 (2) | 20.0 (6) | 6.0 (1) | 22.0 (5) | |||||
| Others | 1.5 (2) | 17.5 (4) | 5.5 (1) | 20.0 (8) | |||||
| Future outlook | Significant impact | 1.5 (0) | 2.219 (0.528) | 13.0 (0) | 9.985 (0.019)a | 4.5 (0) | 1.452 (0.693) | 17.0 (0) | 5.572 (0.134) |
| Limited capacity | 2.0 (1) | 17.0 (6) | 5.0 (1) | 23.0 (8) | |||||
| Fundamental part | 2.0 (1) | 20.0 (4) | 6.0 (1) | 21.0 (5) | |||||
| Uncertain | 2.0 (2) | 17.0 (6) | 5.0 (1) | 25.0 (5) | |||||
Military hospital (military, security forces, national guard).
Specialist hospital or medical city.
Northern America (Canada and United States).
Kruskal-Wallis H test.
P < 0.05.
IQR: Interquartile range.
The participants perception towards AI was also significantly related to their years of experience (Kruskal-Wallis H test = 7.037; P = 0.030) and future outlook on AI (Kruskal-Wallis H test = 9.985; P = 0.019). Participants with 11 years to 20 years of experience had significantly higher scores of perceptions toward AI compared to those with more than 20 years of experience. Furthermore, surgeons who viewed the future of AI in their field as a fundamental part of the field had a more optimistic perception of AI, with a median score of 20. Finally, none of the tested variables appeared to influence surgeons’ willingness to adopt AI tools or impact their perception of factors affecting decision-making (Table 4).
Bivariate correlation analysis of the study domains revealed several significant relationships (Table 5). Familiarity and Perception were strongly correlated (r = 0.568; P < 0.001). Willingness to adopt AI was moderately correlated with both Familiarity (r = 0.262; P = 0.027) and Perception (r = 0.560; P < 0.001). Decision-making showed a positive correlation with Familiarity (r = 0.269; P = 0.023), Perception (r = 0.456; P < 0.001), and Willingness (r = 0.430; P < 0.001).
Table 5.
Bivariate correlation among study domains
|
Domain
|
Familiarity
|
Perception
|
Willingness
|
Decision-making
|
| Familiarity | 1.000 (0) | 0.568 (< 0.001) | 0.262 (0.027) | 0.269 (0.023) |
| Perception | 0.568 (< 0.001) | 1.000 (0) | 0.560 (< 0.001) | 0.456 (< 0.001) |
| Willingness | 0.262 (0.027) | 0.560 (< 0.001) | 1.000 (0) | 0.430 (< 0.001) |
| Decision-making | 0.269 (0.023) | 0.356 (< 0.001) | 0.430 (< 0.001) | 1.000 (0) |
Open-ended responses
The open-ended responses suggest that overall, the pediatric orthopedic surgeons in our study are cautious but hold an optimistic view of the future of AI in the specialty. The need for more education and understanding was highlighted. The specific use cases mentioned were AI’s potential to improve workflow in administrative tasks, and its possible role in Graf diagnosis and limp deformity correction. Finally, there is a clear need for more workshops and education about AI, as well as recognition of the need for caution due to AI’s current limitations.
DISCUSSION
Our investigation highlights several key findings: (1) There is a lack of familiarity among pediatric orthopedic surgeons towards AI; (2) Despite this, pediatric orthopedic surgeons have a positive perception of AI’s potential benefits; (3) Pediatric orthopedic surgeons consider ethical considerations, such as protection of patient privacy, to be highly important for the adoption of AI systems; and (4) Pediatric orthopedic surgeons tend to believe that AI will have a significant impact on the future of the specialty.
Currently, AI is rapidly progressing in many medical and surgical fields, especially in specialties such as pathology, radiology, and cardiology[40,41]. However, the field of pediatric orthopedics has also seen numerous AI developments such as for bone age assessment, assisting in disease diagnosis, optimizing surgeries, and personalizing rehabilitation[17,25-27]. As these tools are being developed, it is important to assess the views and expertise of the physicians to address major concerns and ultimately improve patient care[33]. To the best of our knowledge, this is the first study to evaluate pediatric orthopedic surgeons’ opinions and perceptions of various aspects of AI.
This study found that more than 60% of pediatric orthopedic surgeons have little to no familiarity with AI in medicine (Table 2). This finding is in accordance with studies that have observed similar trends among orthopedic surgeons in different regions[29,34]. A recent study showed that approximately 34% of Turkish orthopedic surgeons are familiar with AI[34]. Another study of Sudanese orthopedic surgeons reported an overall lack of knowledge on the basic concepts of AI[29]. Generally, existing literature points to a lack of understanding of AI in numerous healthcare specialties[29,34,42-44]. A study surveying staff employed by the national health service foundation trust, including physicians, nurses, managers, and employees, found that the majority of healthcare workers had a limited understanding of AI and were worried about possible issues that could arise from its widespread use[43]. These findings collectively point to a significant deficiency in understanding AI within the healthcare sector, indicating a pressing need for intensified educational efforts to bridge this gap.
By contrast, our study revealed a strong inclination among pediatric orthopedic surgeons to adopt AI-based tools and systems, with more than 90% expressing readiness to recommend such tools to their peers (Table 3). This positive attitude is in agreement with a study by Kamal et al[29], who reported that the majority of orthopedic surgeons are willing to integrate AI into their practice, as well as other studies that showed similar results[34,44]. This suggests a promising trajectory for the incorporation of AI into surgical practice.
In terms of perceptions, our findings suggest an overall positive outlook among pediatric orthopedic surgeons regarding AI’s potential benefits, particularly in enhancing diagnostic accuracy and treatment planning (Table 2). Notably, the aspect of AI applications most favorably received was their ability to save time and enhance productivity (Table 2). This finding aligns with previous research by Oh et al[28], who found that approximately 62% of Korean physicians surveyed agreed that AI offers an advantage of quickly obtaining clinically relevant data. Interestingly, we found that familiarity with AI correlated with a more positive attitude among pediatric orthopedic surgeons (Table 5), in accordance with existing literature suggesting that enhancing AI education could play a crucial role in developing trust towards AI integration in healthcare[30,40,45]. For instance, a recent article studying aspiring orthopedic surgeons found that AI literacy was significantly correlated with a more positive sentiment towards AI[40].
An intriguing observation from our study was the correlation between years of experience and attitudes towards AI. Surgeons with 10 years to 20 years of experience exhibited significantly greater familiarity with and a more positive attitude towards AI compared to their less or more experienced counterparts (Table 4). Interestingly, a study of Sudanese orthopedic surgeons by Kamal et al[29] also reported that those with 11 years to 20 years of practice and with more knowledge on AI had a significantly positive attitude towards the utilization of AI. This suggests that practitioners with this level of experience may be more receptive to AI integration, possibly due to higher exposure to technological advancements. However, this also suggests the need for targeted training programs to ensure widespread adoption of AI across all experience levels.
Moreover, participants in our study placed particularly high importance on patient privacy and data security when considering the adoption of AI. Protection of patient privacy and data security with AI implementation was the most highly rated priority for the surgeons in our survey, with more than 90% of pediatric orthopedic surgeons rating it as highly important or quite important (Table 2). This findings aligns with existing literature[32,43]. A study of healthcare staff found that over 80% of participants believed that there are major privacy concerns associated with the use of AI in healthcare[43]. Another study of pharmacy professionals from the Middle East and North Africa found that 58.9% of participants were concerned about patient data privacy and cybersecurity threats, while 67% felt there was insufficient legal regulation[32]. This emphasizes the ethical considerations surrounding AI implementation in healthcare and highlights the need for robust regulatory frameworks to safeguard patient information[29,43,44,46]. To overcome the dilemma of maintaining patient privacy and data security while adopting AI in healthcare, several strategies can be employed. According to Yadav et al[47], implementing robust legal frameworks such as the general data protection regulation and the health insurance portability and accountability act ensures that patient information is managed securely and with consent, whereas national policies such as India’s digital personal data protection bill (2023) provide specific guidelines for safeguarding personal data. Privacy-preserving AI techniques, including federated learning, differential privacy, and cryptographic methods, offer ways to protect data during AI model training and analysis[47,48]. Finally, educating healthcare professionals about data privacy, security practices, and ethical considerations ensures adherence to best practices and enhances the responsible use of AI in healthcare[47,48].
Regarding future expectations, our results on the anticipated role of AI in the next 5 years to 10 years show a cautious yet optimistic outlook. Most surgeons foresee a limited but significant impact of AI, and less than 3% believe it will have no significant influence (Table 3). A study assessing orthopedic surgeons from Turkey found that 80% of participants identified AI as most practical for extremity reconstruction[34]. Additionally, 68.7% noted that AI is most needed for fracture classification in pelvic injuries[34]. This gradual integration aligns with existing literature, which suggests a focused application of AI in specific areas such as extremity reconstruction and fracture classification, paving the way for more personalized and efficient patient care[17,34]. Overall, AI technologies are showing promise in improving various outcomes, including the length of hospital stays, associated costs, and functional recovery, thereby enhancing both patient management and resource allocation[49].
As aforementioned, our findings highlight a significant gap in pediatric orthopedic surgeons’ familiarity with AI (Table 2). Despite this gap, there is a high willingness among surgeons to adopt AI tools, accompanied by a positive attitude towards its integration into practice (Table 2), suggesting that the perceived lack of familiarity with AI is not due to a lack of willingness or interest, but rather the complexity and rapid evolution of the technology. This finding is further supported by a study by Şahin and Berk[34], who reported that more than 80% of orthopedic surgeons plan to learn about AI in in the near future. This may indicate a need for governments, healthcare institutions, and educational bodies to close this knowledge gap through targeted education and training programs. By focusing on pediatric orthopedic surgeons within the Gulf region, this research contributes insights that can guide future AI adoption strategies in pediatric orthopedics, particularly in the Middle East, which is heavily investing in developing AI applications and guidelines[7-10].
Limitations
Despite the valuable insights, this study had limitations. The focus on pediatric orthopedic surgeons in Gulf Cooperation Council countries limits the generalizability of the findings, as this region is heavily investing in AI development[7,9]. Thus, the findings may not reflect the views of surgeons in regions with different levels of AI adoption. Future research should assess the views of pediatric orthopedic surgeons in other countries that are heavily investing in AI, including the United States, Canada, European countries, and China, as well as developing countries. Additionally, reliance on self-reported data may introduce bias. Information bias, particularly recall and observer bias, may have arisen from the reliance on self-reported data, which may have introduced inaccuracies in responses. To mitigate this, we carefully designed the survey with clear, structured questions. Moreover, anonymity was ensured to encourage honest and accurate responses. Our study provides a snapshot of current attitudes toward AI, and the rapidly evolving nature of AI technology suggests that these findings may need reassessment as AI continues to develop. Future research could improve reliability by incorporating objective measures and validated instruments.
CONCLUSION
Our results showed a general low familiarity with AI among pediatric orthopedic surgeons. However, they also showed an overall positive attitude and high willingness to learn about and use AI in the future. Our study contributes to the growing body of evidence that pediatric orthopedic surgeons are open to the integration of AI into their field, recognizing its potential benefits while also acknowledging the need for vigorous evidence and ethical considerations. We suggest that comprehensive educational programs be developed and offered that explore AI in healthcare and address common concerns. We recommend continued surveillance of the opinions and concerns of all healthcare staff, patients, and other stakeholders to successfully implement and apply AI in clinical contexts.
ACKNOWLEDGEMENTS
The authors sincerely thank all of the pediatric orthopedic surgeons who participated in our survey for their valuable time and insights.
Footnotes
Institutional review board statement: Ethical approval for this study was obtained from the Institutional Review Board at Imam Abdulrahman Bin Faisal University, No. IRB-UGS-2023-01-530.
Informed consent statement: Participants were informed about the study’s purpose, methods, and voluntary nature, with the option to withdraw at any time. By voluntarily participating, informed consent was implied. No identifiers were collected, and the anonymity and confidentiality of participants were strictly maintained.
Conflict-of-interest statement: The authors declare that they have no conflict of interest.
STROBE statement: The authors have read the STROBE Statement—a checklist of items, and the manuscript was prepared and revised according to the STROBE Statement-a checklist of items.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country of origin: Saudi Arabia
Peer-review report’s classification
Scientific Quality: Grade C
Novelty: Grade C
Creativity or Innovation: Grade C
Scientific Significance: Grade B
P-Reviewer: Bouhouita-Guermech S S-Editor: Fan M L-Editor: A P-Editor: Yuan YY
Contributor Information
Ammar K Alomran, Department of Orthopedic, College of Medicine, Imam Abdulrahman Bin Faisal University, Dammam 31441, Eastern, Saudi Arabia.
Mohammed F Alomar, College of Medicine, Imam Abdulrahman Bin Faisal University, Dammam 31441, Eastern, Saudi Arabia. aomran@iau.edu.sa.
Ali A Akhdher, College of Medicine, Imam Abdulrahman Bin Faisal University, Dammam 31441, Eastern, Saudi Arabia.
Ali R Al Qanber, College of Medicine, Imam Abdulrahman Bin Faisal University, Dammam 31441, Eastern, Saudi Arabia.
Ahmad K Albik, College of Medicine, Imam Abdulrahman Bin Faisal University, Dammam 31441, Eastern, Saudi Arabia.
Arwa Alumran, Department of Health Information Management and Technology, Imam Abdulrahman Bin Faisal University, Dammam 34212, Eastern, Saudi Arabia.
Ahmed H Abdulwahab, College of Medicine, Imam Abdulrahman Bin Faisal University, Dammam 31441, Eastern, Saudi Arabia.
Data sharing statement
Raw data and materials are available upon reasonable request to the Corresponding Author.
References
- 1.Sadat-ali M. Concept of Artificial Intelligence (AI) and Its Use in Orthopaedic Practice: Applications and Pitfalls: A Narrative Review. Open J Orthop. 2024;14:32–40. [Google Scholar]
- 2.Wadhwa V, Alagappan M, Gonzalez A, Gupta K, Brown JRG, Cohen J, Sawhney M, Pleskow D, Berzin TM. Physician sentiment toward artificial intelligence (AI) in colonoscopic practice: a survey of US gastroenterologists. Endosc Int Open. 2020;8:E1379–E1384. doi: 10.1055/a-1223-1926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Syed W, Basil A Al-Rawi M. Assessment of Awareness, Perceptions, and Opinions towards Artificial Intelligence among Healthcare Students in Riyadh, Saudi Arabia. Medicina (Kaunas) 2023;59 doi: 10.3390/medicina59050828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kermany DS, Goldbaum M, Cai W, Valentim CCS, Liang H, Baxter SL, McKeown A, Yang G, Wu X, Yan F, Dong J, Prasadha MK, Pei J, Ting MYL, Zhu J, Li C, Hewett S, Dong J, Ziyar I, Shi A, Zhang R, Zheng L, Hou R, Shi W, Fu X, Duan Y, Huu VAN, Wen C, Zhang ED, Zhang CL, Li O, Wang X, Singer MA, Sun X, Xu J, Tafreshi A, Lewis MA, Xia H, Zhang K. Identifying Medical Diagnoses and Treatable Diseases by Image-Based Deep Learning. Cell. 2018;172:1122–1131.e9. doi: 10.1016/j.cell.2018.02.010. [DOI] [PubMed] [Google Scholar]
- 5.Tang A, Tam R, Cadrin-Chênevert A, Guest W, Chong J, Barfett J, Chepelev L, Cairns R, Mitchell JR, Cicero MD, Poudrette MG, Jaremko JL, Reinhold C, Gallix B, Gray B, Geis R Canadian Association of Radiologists (CAR) Artificial Intelligence Working Group. Canadian Association of Radiologists White Paper on Artificial Intelligence in Radiology. Can Assoc Radiol J. 2018;69:120–135. doi: 10.1016/j.carj.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 6.Li R, Yang Y, Wu S, Huang K, Chen W, Liu Y, Lin H. Using artificial intelligence to improve medical services in China. Ann Transl Med. 2020;8:711. doi: 10.21037/atm.2019.11.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Solaiman B, Cohen IG, editors . Research Handbook on Health, AI and the Law. 2024 . [Google Scholar]
- 8.Memish ZA, Altuwaijri MM, Almoeen AH, Enani SM. The Saudi Data & Artificial Intelligence Authority (SDAIA) Vision: Leading the Kingdom's Journey toward Global Leadership. J Epidemiol Glob Health. 2021;11:140–142. doi: 10.2991/jegh.k.210405.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Albinsaad LS, Alkhawajah AA, Abuageelah BM, Alkhalaf RA, Alfaifi MH, Oberi IA, Alnajjad AI, Albalawi IA, Alessa MY, Khan A. The Saudi Community View of the Use of Artificial Intelligence in Health Care. Ann Afr Med. 2024;23:343–351. doi: 10.4103/aam.aam_192_23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hassounah M, Raheel H, Alhefzi M. Digital Response During the COVID-19 Pandemic in Saudi Arabia. J Med Internet Res. 2020;22:e19338. doi: 10.2196/19338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mirza AA, Wazgar OM, Almaghrabi AA, Ghandour RM, Alenizi SA, Mirza AA, Alraddadi KS, Al-Adwani FH, Alsakkaf MA, Aljuaid SM. The Use of Artificial Intelligence in Medical Imaging: A Nationwide Pilot Survey of Trainees in Saudi Arabia. Clin Pract. 2022;12:852–866. doi: 10.3390/clinpract12060090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aboalshamat KT. Perception and Utilization of Artificial Intelligence (AI) among Dental Professionals in Saudi Arabia. Open Dent J. 2022;16 [Google Scholar]
- 13.Esteva A, Kuprel B, Novoa RA, Ko J, Swetter SM, Blau HM, Thrun S. Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017;542:115–118. doi: 10.1038/nature21056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ting DSW, Cheung CY, Lim G, Tan GSW, Quang ND, Gan A, Hamzah H, Garcia-Franco R, San Yeo IY, Lee SY, Wong EYM, Sabanayagam C, Baskaran M, Ibrahim F, Tan NC, Finkelstein EA, Lamoureux EL, Wong IY, Bressler NM, Sivaprasad S, Varma R, Jonas JB, He MG, Cheng CY, Cheung GCM, Aung T, Hsu W, Lee ML, Wong TY. Development and Validation of a Deep Learning System for Diabetic Retinopathy and Related Eye Diseases Using Retinal Images From Multiethnic Populations With Diabetes. JAMA. 2017;318:2211–2223. doi: 10.1001/jama.2017.18152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haleem A, Javaid M, Khan IH. Current status and applications of Artificial Intelligence (AI) in medical field: An overview. Curr Med Res Pract. 2019;9:231–237. [Google Scholar]
- 16.Sutton RT, Pincock D, Baumgart DC, Sadowski DC, Fedorak RN, Kroeker KI. An overview of clinical decision support systems: benefits, risks, and strategies for success. NPJ Digit Med. 2020;3:17. doi: 10.1038/s41746-020-0221-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sharaf Y, Taha B, Sayyad Y. Application of Artificial Intelligence in Pediatric Orthopaedic. SVOA Orthopaedics. 2023;3:1–6. [Google Scholar]
- 18.Al-rumaih MH, Al-ahmari MS, Kishta W. The role of artificial intelligence (AI) in paediatric orthopaedic surgery. J Orthop Rep. 2025;4:100416. [Google Scholar]
- 19.Taves J, Skitch S, Valani R. Determining the clinical significance of errors in pediatric radiograph interpretation between emergency physicians and radiologists. CJEM. 2018;20:420–424. doi: 10.1017/cem.2017.34. [DOI] [PubMed] [Google Scholar]
- 20.Al-Sani F, Prasad S, Panwar J, Stimec J, Khosroawshahi A, Mizzi T, Camp M, Colaco K, Kramer A, Boutis K. Adverse Events from Emergency Physician Pediatric Extremity Radiograph Interpretations: A Prospective Cohort Study. Acad Emerg Med. 2020;27:128–138. doi: 10.1111/acem.13884. [DOI] [PubMed] [Google Scholar]
- 21.Wolfe JA, Wolfe H, Banaag A, Tintle S, Perez Koehlmoos T. Early Pediatric Fractures in a Universally Insured Population within the United States. BMC Pediatr. 2019;19:343. doi: 10.1186/s12887-019-1725-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Segal D, Slevin O, Aliev E, Borisov O, Khateeb B, Faour A, Palmanovich E, Brin YS, Weigl D. Trends in the seasonal variation of paediatric fractures. J Child Orthop. 2018;12:614–621. doi: 10.1302/1863-2548.12.180114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Larsen AV, Mundbjerg E, Lauritsen JM, Faergemann C. Development of the annual incidence rate of fracture in children 1980-2018: a population-based study of 32,375 fractures. Acta Orthop. 2020;91:593–597. doi: 10.1080/17453674.2020.1772555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Renal Interventions. Artificial intelligence software BoneView helps radiologists and emergency physicians detect and localise fractures. [cited October 08, 2024]. Available from: https://interventionalnews.com/boneview-ai-detect-fractures/
- 25.Wang Y, Fan M, Zaman Q, Zheng P. Application progress and potential of digital medicine in pediatric orthopedics. Digit Med. 2021;7:4. [Google Scholar]
- 26.Daldrup-Link H. Artificial intelligence applications for pediatric oncology imaging. Pediatr Radiol. 2019;49:1384–1390. doi: 10.1007/s00247-019-04360-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Offiah AC. Current and emerging artificial intelligence applications for pediatric musculoskeletal radiology. Pediatr Radiol. 2022;52:2149–2158. doi: 10.1007/s00247-021-05130-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oh S, Kim JH, Choi SW, Lee HJ, Hong J, Kwon SH. Physician Confidence in Artificial Intelligence: An Online Mobile Survey. J Med Internet Res. 2019;21:e12422. doi: 10.2196/12422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kamal AH, Zakaria OM, Majzoub RA, Nasir EWF. Artificial intelligence in orthopedics: A qualitative exploration of the surgeon perspective. Medicine (Baltimore) 2023;102:e34071. doi: 10.1097/MD.0000000000034071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nickel PJ. Trust in medical artificial intelligence: a discretionary account. Ethics Inf Technol. 2022;24:7. [Google Scholar]
- 31.Char DS, Shah NH, Magnus D. Implementing Machine Learning in Health Care - Addressing Ethical Challenges. N Engl J Med. 2018;378:981–983. doi: 10.1056/NEJMp1714229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hasan HE, Jaber D, Khabour OF, Alzoubi KH. Ethical considerations and concerns in the implementation of AI in pharmacy practice: a cross-sectional study. BMC Med Ethics. 2024;25:55. doi: 10.1186/s12910-024-01062-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang L, Zhang Z, Wang D, Cao W, Zhou X, Zhang P, Liu J, Fan X, Tian F. Human-centered design and evaluation of AI-empowered clinical decision support systems: a systematic review. Front Comput Sci. 2023;5:1187299. [Google Scholar]
- 34.Şahin E, Berk H. Orthopedic surgeons’ attitudes and expectations toward artificial intelligence: A national survey study. J Surg Med. 2023;7:151–155. [Google Scholar]
- 35.Scott IA, Carter SM, Coiera E. Exploring stakeholder attitudes towards AI in clinical practice. BMJ Health Care Inform. 2021;28 doi: 10.1136/bmjhci-2021-100450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.He J, Baxter SL, Xu J, Xu J, Zhou X, Zhang K. The practical implementation of artificial intelligence technologies in medicine. Nat Med. 2019;25:30–36. doi: 10.1038/s41591-018-0307-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pedro AR, Dias MB, Laranjo L, Cunha AS, Cordeiro JV. Artificial intelligence in medicine: A comprehensive survey of medical doctor's perspectives in Portugal. PLoS One. 2023;18:e0290613. doi: 10.1371/journal.pone.0290613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Capili B. Cross-Sectional Studies. Am J Nurs. 2021;121:59–62. doi: 10.1097/01.NAJ.0000794280.73744.fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Daniel WW, Cross CL. Biostatistics: A Foundation for Analysis in the Health Sciences. 11th edition. John Wiley & Sons, 2018. [Google Scholar]
- 40.Pawelczyk J, Kraus M, Eckl L, Nehrer S, Aurich M, Izadpanah K, Siebenlist S, Rupp MC. Attitude of aspiring orthopaedic surgeons towards artificial intelligence: a multinational cross-sectional survey study. Arch Orthop Trauma Surg. 2024;144:3541–3552. doi: 10.1007/s00402-024-05408-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Benjamens S, Dhunnoo P, Meskó B. The state of artificial intelligence-based FDA-approved medical devices and algorithms: an online database. NPJ Digit Med. 2020;3:118. doi: 10.1038/s41746-020-00324-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bisdas S, Topriceanu CC, Zakrzewska Z, Irimia AV, Shakallis L, Subhash J, Casapu MM, Leon-Rojas J, Pinto Dos Santos D, Andrews DM, Zeicu C, Bouhuwaish AM, Lestari AN, Abu-Ismail L, Sadiq AS, Khamees A, Mohammed KMG, Williams E, Omran AI, Ismail DYA, Ebrahim EH. Artificial Intelligence in Medicine: A Multinational Multi-Center Survey on the Medical and Dental Students' Perception. Front Public Health. 2021;9:795284. doi: 10.3389/fpubh.2021.795284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Castagno S, Khalifa M. Perceptions of Artificial Intelligence Among Healthcare Staff: A Qualitative Survey Study. Front Artif Intell. 2020;3:578983. doi: 10.3389/frai.2020.578983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.De Simone B, Abu-Zidan FM, Gumbs AA, Chouillard E, Di Saverio S, Sartelli M, Coccolini F, Ansaloni L, Collins T, Kluger Y, Moore EE, Litvin A, Leppaniemi A, Mascagni P, Milone L, Piccoli M, Abu-Hilal M, Sugrue M, Biffl WL, Catena F. Knowledge, attitude, and practice of artificial intelligence in emergency and trauma surgery, the ARIES project: an international web-based survey. World J Emerg Surg. 2022;17:10. doi: 10.1186/s13017-022-00413-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gong B, Nugent JP, Guest W, Parker W, Chang PJ, Khosa F, Nicolaou S. Influence of Artificial Intelligence on Canadian Medical Students' Preference for Radiology Specialty: ANational Survey Study. Acad Radiol. 2019;26:566–577. doi: 10.1016/j.acra.2018.10.007. [DOI] [PubMed] [Google Scholar]
- 46.Sarwar S, Dent A, Faust K, Richer M, Djuric U, Van Ommeren R, Diamandis P. Physician perspectives on integration of artificial intelligence into diagnostic pathology. NPJ Digit Med. 2019;2:28. doi: 10.1038/s41746-019-0106-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yadav N, Pandey S, Gupta A, Dudani P, Gupta S, Rangarajan K. Data Privacy in Healthcare: In the Era of Artificial Intelligence. Indian Dermatol Online J. 2023;14:788–792. doi: 10.4103/idoj.idoj_543_23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Murdoch B. Privacy and artificial intelligence: challenges for protecting health information in a new era. BMC Med Ethics. 2021;22:122. doi: 10.1186/s12910-021-00687-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lisacek-Kiosoglous AB, Powling AS, Fontalis A, Gabr A, Mazomenos E, Haddad FS. Artificial intelligence in orthopaedic surgery. Bone Joint Res. 2023;12:447–454. doi: 10.1302/2046-3758.127.BJR-2023-0111.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Raw data and materials are available upon reasonable request to the Corresponding Author.