Abstract
The current study focused on investigating the relationship between level and timing of physical activity and sleep quality and hygiene in healthy individuals. This cross-sectional study design recruited 175 participants (male: 98, 56%, female: 77, 44%, and BMI: 23.87 ± 3.92) aged between 18 and 65, 157 of whom were physically active and 18 of whom were physically inactive. The study recruited healthy participants from various sports facilities, fitness centers, and walking parks to ensure a diverse sample of physically active individuals in a metropolitan city. The study excluded people with sleep disorders, rheumatoid arthritis, heart or neurological problems, and those who had shift work. The study employed the Demographic Information Form, International Physical Activity Questionnaire (Short Form), Pittsburgh Sleep Quality Scale, and Sleep Hygiene Questionnaire. A one-way MANOVA was employed to compare sleep quality and hygiene in different physical activity levels. A second MANOVA compared sleep quality and hygiene in different physical activity timing, including only the minimally active and very active participants. One-way MANOVA showed a significant difference F (4, 171) = 7.532, Pillai’s trace = 0.161, partial eta squared = 0.081 between sleep quality and hygiene scores among inactive, minimally active, and very active participants. A post hoc analysis showed sleep quality was significantly better in minimal active (6.42 ± 2.55, p = 0.002, Cohen’s d = 0.867) and very active participants (5.99 ± 2.29, p < 0.001, Cohen’s d = 1.092) than inactive (8.61 ± 2.50) participants. Also, sleep hygiene was significantly better in minimal active (28.50 ± 6.74, p = 0.001, Cohen’s d = 0.867) and very active participants (29.52 ± 6.56, p < 0.001, Cohen’s d = 0.992) than inactive (36.05 ± 8.39) participants. The one-way MANOVA revealed no statistically significant differences in sleep quality and hygiene scores based on physical activity time. Our study showed that physically active individuals had significantly better sleep quality and hygiene scores, while there was no difference based on the timing of physical activity. Healthy individuals may be encouraged to participate in physical activity in the morning, afternoon, or evening to improve sleep parameters.
Supplementary information
The online version contains supplementary material available at 10.1186/s12889-024-20708-1.
Keywords: Physical activity, Sleep quality, Sleep hygiene, Time
Introduction
Sleep and physical activity are crucial for maintaining good health [1]. Insufficient sleep and low levels of physical activity can have detrimental effects on human health [2]. On the other hand, people who exercise regularly have better sleep and overall health [3]. Due to changes in lifestyle and behavior, individuals are particularly vulnerable to sleep deprivation and physical inactivity [4]. Getting less than the recommended amount of sleep [5] and physical activity [6] is independently associated with adverse health outcomes. Poor sleep is associated with insulin resistance [7], cardiovascular problems [8], immune system dysfunction [9], impaired brain function, and memory consolidation [10]. An inactive lifestyle is associated with various health issues, including insulin resistance, metabolic syndrome [11], obesity, high blood pressure [12], abdominal fat accumulation, poor health-related quality of life, pulmonary and cardiovascular problems [13], immune system problems, and sleep disorders such as insomnia and sleep apnea [14].
There is a bidirectional relationship between sleep and physical activity, meaning that physical activity affects sleep outcomes or vice versa [15]. There is evidence that low to moderate-intensity physical activity improves objective and subjective sleep parameters [16, 17], although some publications suggest otherwise [18]. Physical activity may enhance sleep outcomes by inducing stress psychophysiology and increasing sympathetic activity, heart rate, cortisol levels, and core body temperature [19, 20]. It has been proposed that physical activity during the daytime may enhance sleep quality by increasing perceived fatigue [18]. Furthermore, a restorative night’s sleep may facilitate increased physical activity the following day [21]. Another important issue between physical activity and sleep is the timing of physical activity [22]. Engaging in vigorous physical activity late at night can negatively affect sleep by increasing sleep onset latency (SOL) and decreasing non-rapid eye movement (NREM) sleep [23]. It was recommended to avoid vigorous exercise less than 3 h before bedtime to maintain sleep parameters [14]. Sleep quality is a parameter that refers to the extent to which an individual experiences a comfortable and restful sleep during the night, resulting in a refreshed state upon waking in the morning [24]. Sleep hygiene, a crucial aspect of sleep, focuses on preventing individual behaviors that disrupt or interfere with regular sleep patterns [25]. Sleep can be influenced by multiple factors, including diet [26], internet addiction [27], shift work [28], and more. This study will focus on the perception of sleep parameters regarding the perception of physical activity level and time perspective.
Contrary to current physical activity guidelines, there is growing evidence that the time of physical activity does not negatively affect sleep quality and hygiene [29–31]. In modern society, early morning or late evening exercise is often the most convenient for people’s schedules [32]. However, sleep hygiene guidelines [14] recommend avoiding vigorous exercise in the last 3 h before bedtime to avoid possible sleep disturbance. It is also recommended that morning exercise be encouraged because of its beneficial effects on objective or subjective sleep parameters [33]. On the other hand, two recent meta-analyses emphasize that late-night exercise is unlikely to affect subjective perceptions of sleep quality or objective characteristics of sleep architecture [23, 34]. Because of the controversy between sleep guidelines and recent evidence, there is still a need to establish clear associations between levels and times of physical activity and sleep parameters. The aim of this study was to ascertain whether there were differences in the perception of sleep quality and hygiene of participants according to the level and timing of their perception of physical activity. We hypothesized that physically active individuals would have better sleep quality and hygiene scores than inactive individuals. We also hypothesized that sleep quality or hygiene would not differ according to physical activity at different times of the day.
Methods
Study design
This is an observational study with a cross-sectional design.
Participants
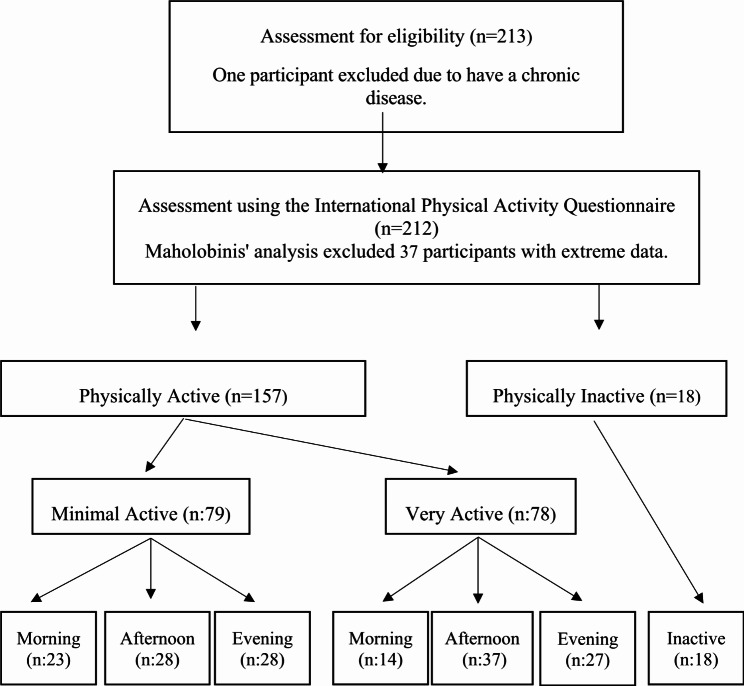
Our study employed healthy individuals aged between 18 and 65 in İstanbul, a metropolitan city in Türkiye. The study included 212 participants; 37 participants who were four or more Mahalanobis scores away from the central data were excluded, and the study was completed with 175 participants categorized as minimally active (n = 79), very active (n = 78), and inactive (n = 18) based on the International Physical Activity Questionnaire-Short Form (IPAQ-SF) scale (Fig. 1). Participants with sleep disorders, sleep apnea, recent healthcare visits for conditions such as rheumatoid arthritis, cardiology or neurology, shift work, and self-reported inability to do physical activity were excluded.
Fig. 1.
Flow diagram for study participants
The Non-Invasive Ethical Committee of Uskudar University obtained ethical approval for the research. The serial number of ethical approvals is 61351342/HAZİRAN/2021-65. All participants were informed of the study’s purpose and that their participation was voluntary. They were also informed that they could leave the study at any time. Written informed consent was obtained from all participants immediately before the forms were filled out.
Study design and procedure
Participants were invited face-to-face by the second author of the study at sports facilities, fitness centers, and walking parks between December 2021 and February 2022. We selected these centers to reach physically active participants. We collected data from paid and public physical activity venues to reach people from different socio-economic backgrounds.
The participants were divided into three groups according to their level of physical activity - very active, minimally active, and inactive - to compare sleep quality and hygiene. Furthermore, to evaluate the correlation between the timing of physical activity and sleep quality and sleep hygiene, the physically active participants (n = 157) were classified into three groups based on the time of their physical activity (morning: 06:01–12:00; afternoon: 12:01–18:00; evening: 18:01–24:00).
Data collection
The second author of the study provided the study questionnaires to the participants in printed format and requested that they be completed. The data were collected via self-administered questionnaires. This approach was selected to protect the participants’ privacy and facilitate the efficient collection of data. Participants filled out a demographic information form, the International Physical Activity Questionnaire [35], the Pittsburgh Sleep Quality Index (PSQI) [36], and the Sleep Hygiene Questionnaire [37].
The Demographic Information Form includes questions about age, educational background, marital status, employment status, regular physical activity, and the timing of that activity. The following question was asked to determine the participants’ physical activity time: “When do you typically engage in physical activity lasting more than 20 minutes during the day?”
The international physical activity questionnaire (short form) (IPAQ-SF)
The IPAQ-SF is the most widely used physical activity questionnaire that measures self-reported physical activity over the last 7 days [35]. The IPAQ-SF is reliable and valid for assessing physical activity in the Turkish population [38]. The questionnaire assesses activity levels through seven questions, with four levels of intensity: (1) vigorous-intensity activity like aerobics, (2) moderate-intensity activity like recreational cycling, (3) walking, and (4) sitting [39]. The IPAQ-SF is recommended for physical activity monitoring, although it shows a small correlation with objective activity measures [35]. A meta-analysis indicates a moderately high test-retest reliability (r = 0.74). The criterion validity (r = 0.41) and concurrent validity (r = 0.72) were both judged to be moderate [35]. The IPAQ-SF determines the duration of physical activity and provides a value for metabolic equivalents (METs). The walk value is calculated by multiplying the duration of the walk, the total number of days per week the individual engaged in that physical activity, and the constant value of 3.3. The value of moderate physical activity is calculated by multiplying the duration of the activity, the number of days, and the constant value of 4.0. Vigorous activity is calculated by multiplying the duration of the activity, the day, and the number 8.0. The IPAQ-SF is a tool that measures energy expenditure on a weekly basis, expressed in METS. It provides a continuous or categorical score that assesses an individual’s weekly physical activity (PA) level. The IPAQ-SF categorizes physical activity levels as inactive (less than 600 METS-1 min-1 week), minimally active (600–2999 METS-1 min-1 week), and very active (3000 METS-1 min-1 week or above) [40].
The pittsburgh sleep quality index (PSQI)
The PSQI is a self-administered questionnaire. It is designed to evaluate sleep quality in both clinical and nonclinical groups. The PSQI is a widely used generic measure in clinical and research settings to distinguish between ‘good’ and ‘poor’ sleepers [41]. The questionnaire evaluates an individual’s sleep patterns during the last month. The PSQI has demonstrated positive reliability and validity in the Turkish population [42]. The questionnaire comprises 19 questions, each scored on a scale of 0–3, and seven subheadings. These subheadings cover subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, use of sleeping pills, and daytime functioning. In scoring the scale, the items of each subheading are summed separately, resulting in a single subheading score. The score of each of the seven subitems can vary from 0 to 3, and the total PSQI score can range from 0 to 21. A score above five points indicates poor sleep quality [36].
Sleep hygiene index
The Sleep Hygiene Index (SHI) aims to evaluate sleep hygiene by asking about the frequency of movements during sleep [37]. Sleep hygiene involves adopting behaviors that promote sleep and avoiding those that disturb it [37]. This self-administered index evaluates environmental and behavioral factors that may contribute to insufficient sleep. The SHI was developed based on the diagnostic criteria for inadequate sleep hygiene in the International Classification of Sleep Disorders [37]. SHI showed sufficient validity and reliability in the Türkiye sample [43]. The scale comprises 13 items, each employing a five-point Likert scale format. In calculating the scale score, the responses to each item are summed, with the value of the possible response ranging from 13 to 65. An increase in the score indicates that the individual has poor sleep hygiene [44].
Statistical analyses
The results of this study were analyzed using the SPSS (Statistical Package for Social Sciences) 25 software program. The distribution of the variables was assessed using skewness and kurtosis coefficients, as well as visual investigation of histograms. If the values of skewness and kurtosis fall within the range of -1.50 to + 1.50, it is inferred that a normal distribution exists [45]. The Mahalanobis distance was also employed to analyze the interpoint distance in our multivariate data set. A Mahalanobis score of 4 points or above was excluded to ensure the homogeneity of the two dependent groups. Once the data had been normalized, the one-way multivariate analysis of variance (MANOVA) assumptions were tested by drawing a scatter matrix for each independent variable group and analyzing the variance-covariance matrices’ homogeneity, linearity, and multicollinearity (see Supplementary File 1 for details). The demographic data were presented as a frequency table, accompanied by a mean and standard deviations. The chi-square test was employed to analyze categorical variables, while the one-way ANOVA was used for continuous variables for demographics. The relationship between physical activity level, timing, sleep quality, and hygiene was evaluated using a MANOVA. As our data consisted of three groups, we performed a Bonferroni correction and considered p < 0.016 as significant. Effect sizes were calculated to indicate the strength of the difference in mean between groups for post hoc analyses, with d < 0.2, d = 0.2–0.5, d = 0.5–0.8, and d > 0.8 considered “trivial,” “small,” “moderate,” and “large,” respectively.
Results
Participants
The GPower program was utilized to calculate the sample size. For the primary outcome of PSQI, a MANOVA was conducted with a global test effect size of f = 0.0625, α = 0.05, and power of 1-β = 0.80, which required a minimum of 155 individuals. A subject population of 213 was involved in the study. One participant was excluded from the study because of their chronic illness, resulting in a final sample size of 212 individuals. The Mahalanobis distance values based on PSQI and SHI scores exceeding 4 were excluded from the final analysis, as their data was considered extreme value. Consequently, the remaining 175 participants were included in the final analysis. Seventy-eight participants were classified as very active (44%), 79 as minimally active (45%), and 18 as inactive (11%). For the analysis of physical activity timing, we excluded inactive participants and only included 157 physically active participants. Out of those who engaged in physical activity, 37 individuals were active in the morning (23%), 65 in the afternoon (41%), and 55 in the evening (35%).
We compared demographic variables in two groups as physical activity level and time. According to physical activity level, there were no significant differences in sex (p = 0.573), age (p = 0.948), marital status (p = 0.448), employment (p = 0.065), BMI (p = 0.101), and education level (p = 0.098). According to the time of physical activity, there were also no significant differences in sex (p = 0.627), age (p = 0.280), marital status (p = 0.569), employment (p = 0.054), BMI (p = 0.359), and education level (p = 0.220) (Table 1). Outlier descriptives were given in Supplementary File 1.
Table 1.
Demographic characteristics based on level and time of physical activity
| Physical Activity Level n: 175 |
Physical Activity Time n:157 |
|||||||
|---|---|---|---|---|---|---|---|---|
| 1 n (18) |
2 n (79) |
3 n (78) |
p | Morning n (37) |
Afternoon n (65) |
Evening n (55) |
p | |
| Sex | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||
| Male | 10 (55.6) | 41 (51.9) | 47 (60.3) | .573a | 23 (62.2) | 34 (52.3) | 31 (56.4) | .627a |
| Female | 8 (44.4) | 38 (48.1) | 31 (39.7) | 14 (37.8) | 31 (47.7) | 24 (43.6) | ||
| Age | ||||||||
| 18–25 | 11 (61.1) | 53 (67.1) | 49 (62.8) | .948a | 26 (70.3) | 46 (70.8) | 30 (54.5) | .280a |
| 26–45 | 4 (22.2) | 18 (22.8) | 18 (23.1) | 7 (18.9) | 11 (16.9) | 18 (32.7) | ||
| 46–65 | 3 (16.7) | 8 (10.1) | 11 (14.1) | 4 (10.8) | 8 (12.3) | 7 (12.7) | ||
| Marital Status | ||||||||
| Married | 2 (11.1) | 16 (20.3) | 19 (51.4) | .448a | 6 (16.2) | 15 (23.1) | 13 (23.6) | .569a |
| Single | 16 (88.9) | 63 (79.7) | 59 (75.6) | 31 (83.8) | 50 (76.9) | 42 (76.4) | ||
| Employment | ||||||||
| Yes | 7 (38.9) | 41 (51.9) | 51 (65.4) | .065a | 26 (70.3) | 31 (47.7) | 35 (63.6) | .054a |
| No | 11 (61.1) | 38 (48.1) | 27 (34.6) | 11 (29.7) | 34 (52.3) | 20 (36.4) | ||
| M ± SD | M ± SD | M ± SD | M ± SD | M ± SD | M ± SD | |||
| BMI (kg/m²) | 25.5 ± 5 | 23.2 ± 3.9 | 24.1 ± 3.4 | .101b | 22.8 ± 3.4 | 23.8 ± 3.8 | 24.0 ± 3.8 | .359b |
| Education (year) | 14.8 ± 1.7 | 15.7 ± 1.8 | 15.4 ± 1.9 | .098b | 15.8 ± 1.3 | 15.7 ± 1.5 | 15.3 ± 1.9 | .220b |
1: Inactive, 2: Minimal Active, 3: Very Active, a: Chi-Square, b: One Way ANOVA, BMI: Body mass index
A one-way MANOVA was performed to determine whether there was a difference between sleep quality and hygiene among different physical activity levels. There was a significant difference in sleep hygiene and quality based on physical activity level, F (4, 171) = 7.532, Pillai’s trace = 0.161, partial eta squared = 0.081 (Table 2).
Table 2.
Sleep quality and sleep hygiene based on physical activity level
| PSQI | Mean ± sd | Manova F | Manova p value (Pillai’s trace) | Manova eta2 | Univariate F | Univariate p value | Univariate eta2 |
|---|---|---|---|---|---|---|---|
| Inactive | 8.61 ± 2.50 | 7.532 | < 0.001 | 0.081 | 8.483 | < 0.001 | 0.090 |
|
Minimal Active |
6.42 ± 2.55 | ||||||
| Very Active | 5.99 ± 2.29 | ||||||
| SHI | Mean ± sd | Univariate F | Univariate p value | Univariate eta2 | |||
| Inactive | 36.05 ± 8.39 | 8.979 | < 0.001 | 0.095 | |||
|
Minimal Active |
28.50 ± 6.74 | ||||||
| Very Active | 29.52 ± 6.56 |
PSQI: pittsburgh sleep quality index, SHI: sleep hygiene index, Bonferroni-corrected p-value; *p < 0.016, **p < 0.0003
Univariate analyses showed sleep quality was significantly different (F (4, 171) = 8.483; p < 0.001; partial η2 = 0.09) based on physical activity level (Table 2). Post hoc Bonferroni analysis showed that minimally active (p = 0.002, d = 0.706) and very active (p < 0.001, d = 830) subjects had better outcomes with moderate and large effect sizes compared to inactive subjects. However, there is no significant difference between minimally active and very active individuals (p = 1.000) in sleep quality (Table 3).
Table 3.
Post Hoc Comparison of Sleep Quality and Sleep Hygiene based physical activity level
| Dependent Variable | (I) Groups by physical activity | (J) Groups by physical activity | Mean Difference (I-J) | Std. Error | p | Cohen’s d | 95% Confidence Interval for Difference | |
|---|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||||
| PSQI | inactive | minimal active | 2.19 | 0.63 | 0.002 | 0.867 | 0.65 | 3.73 |
| very active | 2.62 | 0.63 | < 0.001 | 1.092 | 1.08 | 4.17 | ||
| minimal active | inactive | -2.19 | 0.63 | 0.002 | 0.867 | -3.73 | -0.65 | |
| very active | 0.43 | 0.38 | 0.810 | - | -0.51 | 1.37 | ||
| SHI | inactive | minimal active | 7.54 | 1.78 | < 0.001 | 0.992 | 3.22 | 11.87 |
| very active | 6.52 | 1.79 | 0.001 | 0.867 | 2.20 | 10.85 | ||
| minimal active | inactive | -7.54 | 1.78 | < 0.001 | 0.992 | -11.87 | -3.22 | |
| very active | -1.01 | 1.09 | 1.000 | - | -3.66 | 1.62 | ||
PSQI: pittsburgh sleep quality index, SHI: sleep hygiene index
Univariate analyses also showed sleep hygiene was significantly different (F (4, 171) = 8.979; p < 0 0.001; partial η2 = 0.09) based on physical activity level (Table 2). Post hoc Bonferroni analysis showed that subjects who were minimally (p = 0.001, d = 0.928) and very active (p < 0.001, d = 1.151) had better sleep hygiene scores with a large effect size compared to inactive subjects. However, there is no significant difference between minimally active and very active individuals (p = 1.000) in sleep hygiene (Table 3).
A one-way MANOVA was conducted to determine whether there is a difference between physical activity timing and sleep quality and sleep hygiene. There was a non-significant difference in sleep quality and hygiene based on physical activity time: F (3, 153) = 0.989, Pillai’s trace = 0.413, and partial eta squared = 0.013 (Table 4).
Table 4.
Comparison of Sleep Quality and Sleep Hygiene according to physical activity time
| PSQI (n:157) |
Mean ± sd | Manova F | Manova p value (Pillai’s trace) | Manova eta2 | Univariate F | Univariate p value | Univariate eta2 |
|---|---|---|---|---|---|---|---|
| Morning | 6.41 ± 2.14 | 0.989 | 0.413 | 0.013 | 0.493 | 0.612 | 0.006 |
| Afternoon | 6.31 ± 2.59 | ||||||
| Evening | 5.95 ± 2.43 | ||||||
|
SHI (n:157) |
Mean ± sd | Univariate F | Univariate p value | Univariate eta2 | |||
| Morning | 27.91 ± 8.05 | 1.511 | 0.224 | 0.019 | |||
| Afternoon | 30.07 ± 5.64 | ||||||
| Evening | 28.49 ± 6.65 |
PSQI: pittsburgh sleep quality index, SHI: sleep hygiene index
Discussion
The study aimed to determine whether the perception of sleep quality and hygiene differed based on the perception of physical activity level and timing. The demographics of subgroups for physical activity level and timing were similar regarding sex, age, marital status, employment, BMI, and education. According to physical activity level, the minimally active and very active group had significantly better sleep quality and hygiene scores than the inactive group. However, based on physical activity timing, there were no differences in sleep quality and sleep hygiene scores for morning, afternoon, and evening groups.
Our main finding showed that physically active individuals have better sleep quality and sleep hygiene scores, to varying degrees, than those who are physically inactive. Consistent evidence shows that moderate-intensity physical activity positively affects various aspects of sleep quality [46, 47]. Sullivan et al. showed that physically active participants reported better sleep quality perception and duration [48]. Rayward et al. investigated the effect of a physical activity program on sleep quality, and they found significant improvements in sleep scores [49]. Physical activity can improve sleep quality through various mechanisms, including increased melatonin secretion, weight management, fatigue [50], and improved respiratory capacity. Sleep and physical activity can affect each other bidirectionally. Adequate sleep duration and continuity may positively impact physical activity the following day [18]. Physically active individuals experienced improved sleep quality, less time to fall asleep [44], and a rested awakening. Sleep hygiene combines environmental and behavioral factors to promote healthy sleep [25]. Education programs are typically implemented to enhance sleep hygiene. These programs include adjustments to routines, noise levels, temperature, sleeping surfaces, and lighting [51]. Our study showed that the perception of sleep hygiene was significantly better in people with minimal and very active levels. Several mechanisms can explain the positive effect of physical activity on sleep hygiene. Increasing the production of melatonin, a hormone that regulates the sleep-wake cycle, eases the transition to sleep [52]. Additionally, physical activity reduces stress, a typical obstacle to falling asleep and sleeping [53]. Furthermore, physical activity improves mood, resulting in improved engagement in physical activity and a positive feedback cycle [25]. Lastly, physical activity also helps to regulate body temperature, which is crucial for falling asleep [54]. Tseng ve ark.
We evaluated the relationship between timing of physical activity and sleep quality and sleep hygiene only in the minimally active and very active groups. The timing of physical activity is a factor that may potentially affect sleep due to circadian rhythm. The circadian rhythm is critical in modulating daytime rhythms of metabolism, sleep/wake cycles, feeding behavior, and hormone secretion [55]. However, our study showed that sleep quality and hygiene scores were similar across different times of physical activity. The literature is inconsistent regarding the relationship between physical activity timing and sleep. Seol et al. conducted a randomized controlled trial to investigate the effects of morning versus evening home-based low-intensity exercise on sleep parameters [56]. Their findings indicated that both groups experienced improvement; the evening group demonstrated greater benefit concerning sleep onset latency-D and sleep satisfaction than the morning group [56]. In the study by Seol et al. and our study, the PSQI scores of the evening group were similarly better than the morning group (0.36 and 0.46, respectively) [56]. Benloucif et al. demonstrated that a 2-week vigorous physical activity program benefits objective and subjective sleep parameters, regardless of whether it is performed in the morning or evening [57]. In their study, the mean PSQI score was approximately 1 point better than ours. This difference may be because Benloucif et al. applied for a structured exercise program [57]. In contrast, two studies demonstrated a correlation between engaging in physical activity in the morning [58] or at least four hours before bedtime [59] and enhanced sleep quality. However, this correlation was not observed in the evening group. Additionally, some publications suggest no relationship between the timing of physical activity and sleep quality [14]. Moderate physical activity is considered an effective non-pharmacological method to improve sleep parameters [16]. It can be argued that being physically active is a more important parameter for sleep parameters than physical activity time. Our results suggest that physical activity can be recommended in the morning, afternoon, or evening, consistent with the current literature [29]. Our results should be interpreted cautiously because our study did not include potential confounding variables for sleep and had a relatively small sample size.
Our study has several limitations. It used only subjective scales to assess sleep. It also did not assess diet, sleep-related behaviors, and healthy lifestyle habits, which are known to affect sleep. A limitation of our study is that the physical fitness parameters of the participants, such as endurance and respiratory capacity, were not measured. Other limitations include not accounting for potential confounding variables, the relatively small sample size, the wide age range, and the non-random sampling method.
Conclusion
The current study found that the perception of sleep quality and hygiene scores were significantly better among physically active individuals. However, there was no difference in the perception of sleep quality and hygiene scores between individuals who performed physical activity in the morning, afternoon, and evening. The level of physical activity is the critical parameter for improving sleep. Healthy individuals may be encouraged to engage in physical activity in the morning, afternoon, or evening. Future research should investigate whether comparable outcomes can be observed in individuals experiencing sleep difficulties.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
None.
Author contributions
T.A., E.A and A.O.O. conducted the research design, participated in collecting data, and drafted the manuscript. E.A. conceived the experiment. T.A. and A.O.O. analysed the results interpretation of the data and drafted the manuscript. All authors reviewed the manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sector.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The Non-Invasive Ethical Committee of Uskudar University obtained ethical approval of the research. The ethical approval’s serial number is 61351342/HAZIRAN 2021-65. All participants provided a signed informed consent form before enrolled the study. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kirov R, Brand S, Kolev V, Yordanova J. The sleeping brain and the neural basis of emotions. Behav Brain Sci. 2012;35:155–6. [DOI] [PubMed] [Google Scholar]
- 2.Janssen I, Campbell JE, Zahran S, Saunders TJ, Tomasone JR, Chaput J-P. Timing of physical activity within the 24-hour day and its influence on health: a systematic review. Health Promot Chronic Dis Prev Can. 2022;42:129–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kelley GA, Kelley KS. Exercise and sleep: a systematic review of previous meta-analyses. J Evid-Based Med. 2017;10:26–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Souza ALK, Santos LPD, Rech CR, Rodriguez-Añez CR, Alberico C, Borges LJ, et al. Barriers to physical activity among adults in primary healthcare units in the National Health System: a cross-sectional study in Brazil. Sao Paulo Med J Rev Paul Med. 2022;140:658–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Itani O, Jike M, Watanabe N, Kaneita Y. Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Med. 2017;32:246–56. [DOI] [PubMed] [Google Scholar]
- 6.Warburton DER, Bredin SSD. Reflections on physical activity and health: what should we recommend? Can J Cardiol. 2016;32:495–504. [DOI] [PubMed] [Google Scholar]
- 7.Gauthier P, Desir C, Plombas M, Joffray E, Benhamou P, Borel A. Impact of sleep and physical activity habits on real-life glycaemic variability in patients with type 2 diabetes. J Sleep Res. 2023;32:e13799. [DOI] [PubMed] [Google Scholar]
- 8.Khan MS, Aouad R. The effects of Insomnia and Sleep loss on Cardiovascular Disease. Sleep Med Clin. 2017;12:167–77. [DOI] [PubMed] [Google Scholar]
- 9.Irwin MR. Sleep and inflammation: partners in sickness and in health. Nat Rev Immunol. 2019;19:702–15. [DOI] [PubMed] [Google Scholar]
- 10.Hu X, Cheng LY, Chiu MH, Paller KA. Promoting memory consolidation during sleep: a meta-analysis of targeted memory reactivation. Psychol Bull. 2020;146:218–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marques KAP, Trindade CBB, Almeida MCV, Bento-Torres NVO. Pilates for rehabilitation in patients with multiple sclerosis: a systematic review of effects on cognition, health-related physical fitness, general symptoms and quality of life. J Bodyw Mov Ther. 2020;24:26–36. [DOI] [PubMed] [Google Scholar]
- 12.Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc. 2013;2:e004473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garcia L, Pearce M, Abbas A, Mok A, Strain T, Ali S, et al. Non-occupational physical activity and risk of cardiovascular disease, cancer and mortality outcomes: a dose-response meta-analysis of large prospective studies. Br J Sports Med. 2023;57:979–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee SH, Kim SJ, Bang JW, Lee JH. Relationship of the duration and timing of Exercise with Sleep Quality in Community-Dwelling adults. Sleep Med Res. 2018;9:83–91. [Google Scholar]
- 15.Best JR, Falck RS, Landry GJ, Liu-Ambrose T. Analysis of dynamic, bidirectional associations in older adult physical activity and sleep quality. J Sleep Res. 2019;28:e12769. [DOI] [PubMed] [Google Scholar]
- 16.Lai T-F, Liao Y, Lin C-Y, Huang W-C, Hsueh M-C, Chan D-C. Moderate-to-vigorous physical activity duration is more important than timing for physical function in older adults. Sci Rep. 2020;10:21344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang F, Boros S. The effect of physical activity on sleep quality: a systematic review. Eur J Physiother. 2021;23:11–8. [Google Scholar]
- 18.Mead MP, Baron K, Sorby M, Irish LA. Daily associations between Sleep and Physical Activity. Int J Behav Med. 2019;26:562–8. [DOI] [PubMed] [Google Scholar]
- 19.Bonato M, La Torre A, Saresella M, Marventano I, Merati G, Banfi G, et al. Effect of high-intensity interval training Versus Small-Sided games Training on Sleep and Salivary Cortisol Level. Int J Sports Physiol Perform. 2020;15:1237–44. [DOI] [PubMed] [Google Scholar]
- 20.Uchida S, Shioda K. Exercise effects on sleep physiology. Front Neurol. 2012;3:24606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dzierzewski JM, Buman MP, Giacobbi PR, Roberts BL, Aiken-Morgan AT, Marsiske M, et al. Exercise and sleep in community-dwelling older adults: evidence for a reciprocal relationship. J Sleep Res. 2014;23:61–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chennaoui M, Arnal PJ, Sauvet F, Léger D. Sleep and exercise: a reciprocal issue? Sleep Med Rev. 2015;20:59–72. [DOI] [PubMed] [Google Scholar]
- 23.Frimpong E, Mograss M, Zvionow T, Dang-Vu TT. The effects of evening high-intensity exercise on sleep in healthy adults: a systematic review and meta-analysis. Sleep Med Rev. 2021;60:101535. [DOI] [PubMed] [Google Scholar]
- 24.Hachenberger J, Li Y, Lemola S. Physical activity, sleep and affective wellbeing on the following day: an experience sampling study. J Sleep Res. 2023;32:e13723. [DOI] [PubMed] [Google Scholar]
- 25.Baranwal N, Yu PK, Siegel NS. Sleep physiology, pathophysiology, and sleep hygiene. Prog Cardiovasc Dis. 2023;77:59–69. [DOI] [PubMed] [Google Scholar]
- 26.Godos J, Grosso G, Castellano S, Galvano F, Caraci F, Ferri R. Association between diet and sleep quality: a systematic review. Sleep Med Rev. 2021;57:101430. [DOI] [PubMed] [Google Scholar]
- 27.Alonzo R, Hussain J, Stranges S, Anderson KK. Interplay between social media use, sleep quality, and mental health in youth: a systematic review. Sleep Med Rev. 2021;56:101414. [DOI] [PubMed] [Google Scholar]
- 28.Kang HM, Jeong DC, Suh B-K, Ahn MB. The impact of the Coronavirus Disease-2019 pandemic on childhood obesity and vitamin D status. J Korean Med Sci. 2021;36:e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goldberg M, Pairot De Fontenay B, Blache Y, Debarnot U. Effects of morning and evening physical exercise on subjective and objective sleep quality: an ecological study. J Sleep Res. 2024;33:e13996. [DOI] [PubMed] [Google Scholar]
- 30.Kline CE, Hillman CH, Bloodgood Sheppard B, Tennant B, Conroy DE, Macko RF, et al. Physical activity and sleep: an updated umbrella review of the 2018 Physical Activity Guidelines Advisory Committee report. Sleep Med Rev. 2021;58:101489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Martins LCG, Lopes MV, de O, Diniz CM, Guedes NG. The factors related to a sedentary lifestyle: a meta-analysis review. J Adv Nurs. 2021;77:1188–205. [DOI] [PubMed] [Google Scholar]
- 32.Cerin E, Leslie E, Sugiyama T, Owen N. Perceived barriers to leisure-time physical activity in adults: an ecological perspective. J Phys Act Health. 2010;7:451–9. [DOI] [PubMed] [Google Scholar]
- 33.American Sleep Association. Healthy Sleep Tips. 2022 [cited 2024 Aug 6]. https://sleepdoctor.com/sleep-hygiene/sleep-tips/
- 34.Stutz J, Eiholzer R, Spengler CM. Effects of Evening Exercise on Sleep in healthy participants: a systematic review and Meta-analysis. Sports Med Auckl NZ. 2019;49:269–87. [DOI] [PubMed] [Google Scholar]
- 35.Sember V, Meh K, Sorić M, Starc G, Rocha P, Jurak G. Validity and reliability of International Physical Activity questionnaires for adults across EU countries: systematic review and Meta Analysis. Int J Environ Res Public Health. 2020;17:7161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. [DOI] [PubMed] [Google Scholar]
- 37.Mastin DF, Bryson J, Corwyn R. Assessment of Sleep Hygiene using the Sleep Hygiene Index. J Behav Med. 2006;29:223–7. [DOI] [PubMed] [Google Scholar]
- 38.Saglam M, Arikan H, Savci S, Inal-Ince D, Bosnak-Guclu M, Karabulut E, et al. International Physical Activity Questionnaire: reliability and validity of the Turkish version. Percept Mot Skills. 2010;111:278–84. [DOI] [PubMed] [Google Scholar]
- 39.Bernard P, Savard J, Steindorf K, Sweegers M, Courneya K, Newton R et al. Effects and moderators of exercise on sleep in adults with cancer: Individual patient data and aggregated meta-analyses (2019). J Psychosom Res Httpsdoi Org101016j Jpsychores. 2019 [cited 2024 Jan 22]; https://www.academia.edu/download/95036397/Bernard_20et_20al_202019_20Exercise_20cancer_20sleep_20meta-nalysis_20IPD.pdf [DOI] [PubMed]
- 40.Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95. [DOI] [PubMed] [Google Scholar]
- 41.Mollayeva T, Thurairajah P, Burton K, Mollayeva S, Shapiro CM, Colantonio A. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: a systematic review and meta-analysis. Sleep Med Rev. 2016;25:52–73. [DOI] [PubMed] [Google Scholar]
- 42.Agargun M, Kara H, Anlar O. The validity and reliability of the Pittsburgh Sleep Quality Index. Turk Psikiyatri Derg. 1996;7:107–15. [Google Scholar]
- 43.Ozdemir PG, Boysan M, Selvi Y, Yildirim A, Yilmaz E. Psychometric properties of the Turkish version of the Sleep Hygiene Index in clinical and non-clinical samples. Compr Psychiatry. 2015;59:135–40. [DOI] [PubMed] [Google Scholar]
- 44.Passos GS, Poyares D, Santana MG, D’Aurea CVR, Youngstedt SD, Tufik S, et al. Effects of moderate aerobic exercise training on chronic primary insomnia. Sleep Med. 2011;12:1018–27. [DOI] [PubMed] [Google Scholar]
- 45.Asmundson GJ, Paluszek MM, Landry CA, Rachor GS, McKay D, Taylor S. Do pre-existing anxiety-related and mood disorders differentially impact COVID-19 stress responses and coping? J Anxiety Disord. 2020;74:102271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Solis-Navarro L, Masot O, Torres-Castro R, Otto-Yáñez M, Fernández-Jané C, Solà-Madurell M, et al. Effects on Sleep Quality of Physical Exercise Programs in older adults: a systematic review and Meta-analysis. Clocks Sleep. 2023;5:152–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vanderlinden J, Boen F, Van Uffelen JGZ. Effects of physical activity programs on sleep outcomes in older adults: a systematic review. Int J Behav Nutr Phys Act. 2020;17:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sullivan Bisson AN, Robinson SA, Lachman ME. Walk to a better night of sleep: testing the relationship between physical activity and sleep. Sleep Health. 2019;5:487–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rayward AT, Plotnikoff RC, Murawski B, Vandelanotte C, Brown WJ, Holliday EG, et al. Efficacy of an m-Health physical activity and sleep intervention to improve Sleep Quality in Middle-aged adults: the Refresh Study Randomized Controlled Trial. Ann Behav Med. 2020;54:470–83. [DOI] [PubMed] [Google Scholar]
- 50.Youngstedt SD, Perlis ML, O’Brien PM, Palmer CR, Smith MT, Orff HJ, et al. No association of sleep with total daily physical activity in normal sleepers. Physiol Behav. 2003;78:395–401. [DOI] [PubMed] [Google Scholar]
- 51.Dietrich SK, Francis-Jimenez CM, Knibbs MD, Umali IL, Truglio-Londrigan M. Effectiveness of sleep education programs to improve sleep hygiene and/or sleep quality in college students: a systematic review. JBI Database Syst Rev Implement Rep. 2016;14:108–34. [DOI] [PubMed] [Google Scholar]
- 52.Lewis P, Korf HW, Kuffer L, Groß JV, Erren TC. Exercise time cues (zeitgebers) for human circadian systems can foster health and improve performance: a systematic review. BMJ Open Sport Exerc Med. 2018;4:e000443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.De Nys L, Anderson K, Ofosu EF, Ryde GC, Connelly J, Whittaker AC. The effects of physical activity on cortisol and sleep: a systematic review and meta-analysis. Psychoneuroendocrinology. 2022;143:105843. [DOI] [PubMed] [Google Scholar]
- 54.Weinert D, Waterhouse J. The circadian rhythm of core temperature: effects of physical activity and aging. Physiol Behav. 2007;90:246–56. [DOI] [PubMed] [Google Scholar]
- 55.Westerterp-Plantenga MS. Sleep, circadian rhythm and body weight: parallel developments. Proc Nutr Soc. 2016;75:431–9. [DOI] [PubMed] [Google Scholar]
- 56.Seol J, Fujii Y, Inoue T, Kitano N, Tsunoda K, Okura T. Effects of Morning Versus Evening Home-based Exercise on subjective and objective sleep parameters in older adults: a Randomized Controlled Trial. J Geriatr Psychiatry Neurol. 2021;34:232–42. [DOI] [PubMed] [Google Scholar]
- 57.Benloucif S, Orbeta L, Ortiz R, Janssen I, Finkel SI, Bleiberg J, et al. Morning or evening activity improves neuropsychological performance and subjective sleep quality in older adults. Sleep. 2004;27:1542–51. [DOI] [PubMed] [Google Scholar]
- 58.Buman MP, Winkler EA, Kurka JM, Hekler EB, Baldwin CM, Owen N, et al. Reallocating time to sleep, sedentary behaviors, or active behaviors: associations with cardiovascular disease risk biomarkers, NHANES 2005–2006. Am J Epidemiol. 2014;179:323–34. [DOI] [PubMed] [Google Scholar]
- 59.Chen E, Viktorisson A, Danielsson A, Palstam A, Sunnerhagen KS. Levels of physical activity in acute stroke patients treated at a stroke unit: a prospective, observational study. J Rehabil Med. 2020;52:jrm00041. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.