Dear Editor,
Low back pain (LBP) is a heterogeneous disorder including patients with dominant nociceptive (e.g. myofascial low back pain), neuropathic (e.g. lumbar radiculopathy), and central sensitization pain.[1] LBP of myofascial origin is a chronic pain condition associated with the presence of multiple trigger points in a taut band of skeletal muscle, capable of activating muscle nociceptors. It is characterized by nociceptive pain, unlike LBP due to radiculopathy in which the pain is neuropathic. However, the two clinical conditions often overlap.
To date, therapy consists of the use of oral analgesic drugs, physiotherapy with myofascial manipulation, diet, and exercise but mainly infiltrative therapy.[2] In this article, we propose the use of a sacral ESP block[3,4] with double injection for the treatment of LBP.
We describe the case of a 40-year-old man suffering from chronic LBP with radicular irradiation to the sciatic nerve and reduction of range of motion. The MRI scan had shown a double disc protrusion of L4-L5 and L5-S1. The electromyography was negative.
The pain at rest was deemed to be at NRS 6 and the dynamic pain at NRS 7. The pain did not improve with the use of NSAIDs. We decided to perform a sacral ESP block at the S2 level, we explained the procedure to the patient and acquired informed consent. The patient was placed in prone decubitus and careful skin disinfection and sterile field packing were performed.
A low-frequency (2–5 MHz) curved ultrasound probe was initially positioned in the upper portion of the sacrum longitudinally to visualize the spinous process of L5 along the midline. From there, the probe was moved caudally to visualize the mid-sacral crest at S2 and then moved the probe laterally until the mid-sacral crest was visualized. An 80-mm echo-reflective needle was introduced in the plane initially craniocaudally [Figure 1]. After bone contact, after a negative aspiration test and hydrodissection, the mixture of 15 ml Ropivacaine 0.2% + Dexamethasone 4 mg was injected. During the injection, the needle was moved between the multifidus muscle and the sacral plane to facilitate the spread of the mixture, the disconnection of the muscle fascia, and the opening of the plane with ultrasound visualization of the same. At the end of this first injection at the same entry point, the needle was directed in the caudo-cranial direction with cranial spread of the mixture and allowing opening of the plane between the multifidus muscle and the laminae of L5-L4. It is recommended [Figure 2] that the needle tip be positioned upward and not toward the bone surface to promote anesthetic spread.
Figure 1.
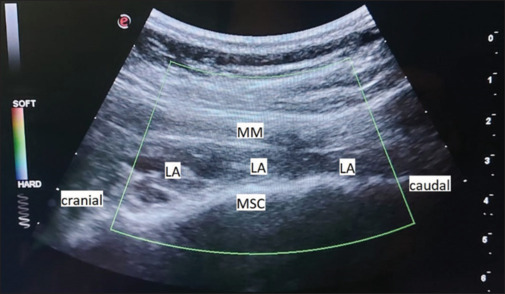
Spread of local anesthetic between the mid sacral crest and the fascia of the multifidus muscle. N: needle; MSC: Mid Sacral Crest; LA: local anesthetic; MM: multifidus muscle
Figure 2.
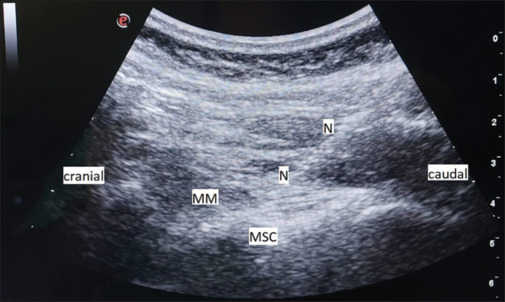
Caudo-cranial direction of the needle until contact with the mid sacral crest
These double injections allow for a better spread of the mixture both cranially and caudally.[5]
Our double injection technique, in the ESP sacral block, already described by Marrone et al.[6] in the setting of acute postoperative pain, may also be a very effective technique in chronic pain. A high-volume injection allowed for covering multiple dermatomes. The advantage of this double injection is the spread in a double craniocaudal direction involving the sacral and lumbar plexus nerve branches. In addition, the dynamic sacral esp block within the fascial compartment causes the rupture of the fibrous laciniae that form within the compartment itself and play a central role in the pathogenesis of these forms of chronic pain.
Therefore, the double injection would allow reaching the sacral and lumbar nerve branches in addition to an effect of the volume of anesthetic infiltrated on fascial trigger points that would allow a reduction in the stiffness of the muscle planes and improve the movement of the affected muscles and consequently the pain.
Further studies are needed.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Nijs J, Apeldoorn A, Hallegraeff H, Clark J, Smeets R, Malfliet A, et al. Low back pain: Guidelines for the clinical classification of predominant neuropathic, nociceptive, or central sensitization pain. Pain Physician. 2015;18:E333–46. [PubMed] [Google Scholar]
- 2.Chen Z, Wu J, Wang X, Wu J, Ren Z. The effects of myofascial release technique for patients with low back pain: A systematic review and meta-analysis. Complement Ther Med. 2021;59:102737. doi: 10.1016/j.ctim.2021.102737. doi: 10.1016/j.ctim.2021.102737. [DOI] [PubMed] [Google Scholar]
- 3.Fusco P, Stecco C, Petroni GM, Ciaschi W, Marinangeli F. ESP block and chronic pain: the dark side of the moon. Minerva Anestesiol. 2022;88:528–9. doi: 10.23736/S0375-9393.22.16282-6. [DOI] [PubMed] [Google Scholar]
- 4.Fusco P, Petroni GM, Nazzarro E, Ciaschi W, Meloncelli S, DE Sanctis F, et al. Low back pain: Is it time for erector spinae plane block? Minerva Anestesiol. 2024;90:210–11. doi: 10.23736/S0375-9393.23.17674-7. [DOI] [PubMed] [Google Scholar]
- 5.Fusco P, Nazzarro E, Petroni G, Stecco C, Ciaschi W, Marinangeli F. Fascial plane blocks and chronic pain: Another step towards the future. J Clin Anesth. 2023;84:111010. doi: 10.1016/j.jclinane.2022.111010. doi: 10.1016/j.jclinane.2022.111010. [DOI] [PubMed] [Google Scholar]
- 6.Marrone F, Paventi S, Tomei M, Failli S, Crecco S, Pullano C. Unilateral sacral erector spinae plane block for hip fracture surgery. Anaesth Rep. 2024;12:e12269. doi: 10.1002/anr3.12269. [DOI] [PMC free article] [PubMed] [Google Scholar]


