Dear Sir,
Pediatric patients may present with physiologically difficult airway due to variations in anatomy, which might be exaggerated in the presence of a cleft palate.[1] The role of supraglottic airway devices (SADs) has been established in managing such cases as a conduit for endotracheal tube (ETT) and as a rescue device.
Here we describe the use of Blockbuster® (BB) laryngeal mask airway (LMA) as a primary airway device in a pediatric patient with congenital heart disease and cleft palate undergoing laparoscopic hernia repair. A 5-year-old male child of weight 18 kg and a known case of patent ductus arteriosus (with left-to-right shunt, moderate tricuspid regurgitation, bicuspid aortic valve, and moderate pulmonary arterial hypertension: right ventricular systolic pressure – 47 mmHg) with a defect of 1.5 × 2 cm in the hard palate presented for laparoscopic hernia repair [Figure 1a]. He had a history of recurrent chest infections, but was asymptomatic at the time of presentation. All other systemic examinations and investigations were normal.
Figure 1.
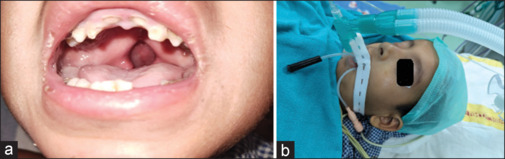
(a) Child with cleft palate; (b) LMA BB in place. BB = Blockbuster®, LMA = laryngeal mask airway
After parental consent was taken and the nil per oral status was confirmed, patient was given intravenous (IV) midazolam 0.75 mg for premedication and shifted to operating theater. After attaching standard monitors, IV induction was performed with fentanyl 40 μg, titrated dose of propofol, and atracurium 10 mg for muscle relaxation. Subsequently, BB LMA (size 2) was inserted, positioning the cuff in the midline against the tongue [Figure 1b]. Upon cuff inflation, a gastric tube was advanced through designated access channel. Adequate ventilation was achieved in a pressure control mode – airway pressures of 14 cm H2O, tidal volume of 140 ml, and positive end-expiratory pressure of 5 with minimal leak. Caudal block ensured perioperative analgesia, and anesthesia was maintained with sevoflurane and atracurium boluses. Intraoperative period was uneventful, and the LMA was removed once the child was fully awake.
An ETT may be the preferred airway management, but has practical challenges like difficult laryngoscopy, intubation leading to increased attempts, bleeding, edema, and hemodynamic response in a cleft palate patient.[2] Among LMAs, we chose BB because of its unique features, like a short airway tube with an angulation of over 95°, which aligns well with the oropharyngeal curve. This facilitates easier insertion of ETT, resulting in a higher success rate.[3] This is useful, especially for emergency airway scenarios which may arise even in the middle of surgery. Various trials have established higher oropharyngeal leak pressure with this device compared to other SADs.[4] This is due to an additional dorsal cuff of BB LMA, which enhances the seal pressure in the oropharyngeal region during positive pressure ventilation.
Though LMA has been included in the “difficult to ventilate” algorithm, the use of newer SADs needs a special mention for their use as a primary device in pediatric patients with airway anomalies. A previous study has used flexible LMA in cleft palate repair surgery.[5] This report is the first description of the use of BB LMA as a primary device in difficult airways. Further studies might validate its use.
Consent
Consent for publication has been taken from the patient.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Sen J, Sen B. Airway management: A comparative study in cleft lip and palate repair surgery in children. Anesth Essays Res. 2014;8:36–40. doi: 10.4103/0259-1162.128905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gunawardana RH. Difficult laryngoscopy in cleft lip and palate surgery. Br J Anaesth. 1996;76:757–9. doi: 10.1093/bja/76.6.757. [DOI] [PubMed] [Google Scholar]
- 3.Endigeri A, Ganeshnavar A, Varaprasad B, Shivanand YH, Ayyangouda B. Comparison of success rate of BlockBuster®versus Fastrach®LMA as conduit for blind endotracheal intubation: A prospective randomised trial. Indian J Anaesth. 2019;63:988–94. doi: 10.4103/ija.IJA_396_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gaur Y, Jaju R, Paliwal N, Choudhary U, Bihani P, Janweja S. Comparison of clinical performance of Ambu® AuraGain™ and BlockBuster® in anaesthetised preschool children-A randomised controlled trial. Indian J Anaesth. 2023;67:420–5. doi: 10.4103/ija.ija_286_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kundra P, Supraja N, Agrawal K, Ravishankar M. Flexible laryngeal mask airway for cleft palate surgery in children: A randomized clinical trial on efficacy and safety. Cleft Palate Craniofac J. 2009;46:368–73. doi: 10.1597/08-009.1. [DOI] [PubMed] [Google Scholar]


