Abstract
Objective:
In youth, a preoccupation with weight and desire to be thinner, or drive for thinness, might persist into adulthood, and predict reward-based compulsive eating and greater weight status.
Methods:
We enrolled 623 women from a prospective cohort study starting at 10 years old, and assessed up to 20 years later. Drive for thinness was measured five times during adolescence. In adulthood (mean age = 39.5), we measured drive for thinness, reward-based eating drive and body mass index (BMI).
Results:
Structural equation modeling found cumulative adolescent drive for thinness predicted higher scores for both adult drive for thinness and reward-based eating drive. Youth drive for thinness was not directly associated with adult BMI but rather indirectly through adult drive for thinness. Reward-based eating drive was not associated with adult BMI.
Conclusion:
Drive for thinness during the critical developmental years may exert long-term effects on adulthood eating behaviors tied to greater weight gain, potentially reflecting an important early target of intervention.
Keywords: adolescents, eating behaviors, disordered eating, body mass index
Introduction
In our modern food environment, a drive to restrict eating may be necessary to avoid weight gain, but excessive thoughts and emotions around dieting and weight gain can have unintended consequences. A strong drive to restrict eating and to lose weight may paradoxically result in weight gain among normal weight women (1). In survey and longitudinal cohort studies, self-reports of dieting and weight control are prospective predictors of weight gain, rather than loss, in adolescents and adults (1) (2) (3). For example, in adolescent females, both self-reported dieting status and dietary restraint were related to prospective risk of obesity (2). Dieting has also been prospectively positively associated with obesity in women (4), (5). In a review, Lowe and colleagues (1) found that self-reported weight loss dieting in the past year was related to prospective weight gain in 15 out of 20 studies.
A preoccupation with thinness, and negative emotions after eating certain foods, may lead to counterproductive dieting. This preoccupation is well measured by the concept and scale for “drive for thinness”. The drive for thinness scale, developed as part of the Eating Disorder Inventory (6), captures negative emotions, thoughts and preoccupation with weight, and extreme pursuit of thinness. Drive for thinness is associated with dieting behaviors (7) and is highly correlated with body dissatisfaction, independent of eating disorder or depression (8).
There are several pathways through which drive for thinness might lead to dieting and ultimately dysregulated eating behavior, such as reward-based eating drive, and in some cases, weight gain. Dieting is associated with impaired cognitive performance (9) (10) and negative effects on cognitive function (11). When attempting excessive cognitive restraint to chronically manage food intake, people’s attention is taxed and they can easily lose restraint and inadvertently increase intake (12). Chronic self-monitoring of food intake is a source of cognitive load, and in some but not all studies, this leads to less self-control over eating and other impulsive behaviors (13, 14) (15). Rigid, “all-or-none” dieting, restricting certain comfort foods, puts individuals at risk of disinhibited overeating when common dietary lapses occur (16), and leaves individuals vulnerable to overeating in response to emotions or external cues (17), (18), possibly due to the commonly found low prefrontal cortex / limbic balance under states of stress (19) (20).
Dieting can also serve as a chronic source of stress. In one study, restricting caloric intake using calorie counting in order to lose weight increased perceived stress and elevated activity of the hypothalamic-pituitary-adrenal axis as reflected by daily salivary cortisol (21). These experiences of stress may make one more vulnerable dysregulated eating, creating a cycle of unhealthy behaviors that promote weight gain (22).
Dieting, especially in the presence of stress, may increase the reinforcement value of food, leading to excessive drive to eat (23) (24). Reward-based eating, is conceptualized as common compulsive eating behavior, but one that drives overeating and obesity. Reward-based eating drive (RED) is measured by three issues-- feeling one cannot stop overeating, eating rapidly or mindlessly without perceiving fullness or satiation, and excessive thoughts of food and eating. RED is associated with eating hyperpalatable foods, food craving, weight gain and at extremes developing obesity (24), (25).
We hypothesize that psychological drive for thinness; which includes cognitive and behavioral measures indicative of constant dieting may drive reward-based eating drive and obesity. In fact, previous results from the longitudinal NHLBI Growth and Health Study (NGHS) (26) children found that drive for thinness was higher for black girls at age ten but associated with higher body mass index (BMI) for both white and black girls in cross-sectional analysis (7). Using data from NGHS, we found that the strongest predictors of BMI increase in girls from age 10 through 19 were family socio-economic position (income and parent education) and drive for thinness (27).
It is unclear if childhood drive for thinness might also have long term consequences –does it track through life, manifesting as a high drive for thinness in adulthood? Does it lead to both reward-based eating and adulthood obesity? Here we conducted a follow up of this cohort, allowing us to address these questions. The objective of this investigation was to determine the long-term consequences of adolescent drive for thinness in women who participated in NGHS as children, investigating adult eating behaviors and BMI approximately 30 years later. We asked: 1) Does adolescent drive for thinness predict adult drive for thinness and elevated reward-based eating? 2) Does adolescent drive for thinness predict higher adulthood BMI? If so, is it a direct relationship or does it work through adult drive for thinness or adult reward-based eating?
Methods
Study Sample
NGHS is a population-based cohort study of white and black girls recruited from two communities (Cincinnati, OH and Richmond, CA) and from families enrolled in a health maintenance organization in Washington DC. A total of 2,379 girls (1,213 Black and 1,166 White) who were 9 or 10 years old were recruited between 1987 and 1988 and assessed in 10 annual measurement points. The original objective of NGHS was to investigate racial differences in dietary intake, physical activity, family, and psychosocial factors associated with the development of obesity from pre-adolescence through maturation. NGHS also sought to examine effects of obesity on cardiovascular disease risk factors. NGHS procedures included a physical examination, anthropometric measurements, dietary information, physical activity, lipoprotein profiles, family socioeconomic status and psychosocial information. Extensive information on this study and sample are available elsewhere (26).
NGHS Follow-Up Study
We conducted the follow-up study from January 2016 to September 2019 with women from the Richmond, CA cohort (n=882) in the original NGHS study. We found that 29 years after enrollment into the study, there was still satisfactory recruitment and retention of this sample of women; 624 women (73.3% response rate) of 850 eligible participants (32 women were deceased, lost to follow-up after the initial year of the study, or institutionalize).
The analytic sample included 614 women (300 black, 314 white) with complete eating and BMI data (98.6%). Using baseline demographic information, we found that a higher percentage of participants were white, from two parent households, highest parental education, and highest income level, compared to eligible non-participants. There was no difference in mean baseline BMI between participants and non-participants. All procedures were approved by the Committee on Human Research of the University of California, Berkeley.
Dysregulated eating behaviors
We measured drive for thinness in both childhood and in adulthood and reward-based eating only in adulthood. The EDI was administered when the girls were ages 12, 14, 16, 18 and 19 years; therefore, adolescent drive for thinness was averaged across these timepoints. We found that the mean and median values did not change much across these timepoints, and at each timepoint the childhood drive for thinness measure was associated with adult BMI. Sample items are, “I think about dieting,” “I am terrified of gaining weight,” “If I gain a pound, I worry that I will keep gaining,” “I feel extremely guilty after overeating,” and “I am preoccupied with the desire to be thinner.” Respondents are asked to choose a value on a 6-point Likert-type scale from Never = 0 to Always = 5; for a range of 0–35. The drive for thinness scale has been found to have psychometric properties for adolescents similar to those of adults (28). Fabian and Thompson (29) found that among female adolescents age 10–15 years, drive for thinness significantly increased among postmenarcheal compared to premenarcheal females, and was significantly correlated with lower body esteem.
Drive for thinness was assessed again in the follow-up study at age 37–43 years. The internal reliability for the drive for thinness scale was good (Cronbach’s α = 0.86).
Reward-based eating drive was assessed only in the follow-up adult study. The Reward-based Eating Drive (24) is a 11-item scale that focuses on aspects of compulsive eating --feeling out of control when eating, lack of satiety, and preoccupation with thoughts of food and predicts weight gain. Higher scores on RED are correlated with food craving (25). The Cronbach’s alpha was 0.92 demonstrating excellent internal reliability.
Body mass index
During the original ten years of the study annual health assessments were conducted including measured height and weight occurred. In the follow-up study, all participants self-reported their weight and height on the baseline questionnaire. Participants received a home visit or visited the University of California, Berkeley to complete anthropometric measurements for those who lived within 60 miles of campus. A Tanita Professional digital scale and a Portable Adult/Infant Measuring Unit stadiometer from Perspective Enterprises was used for local participants. Participants who lived more than 60 miles from campus self-reported their weight measured on a scale and height measured using a paper copy of the QuickMedical Wall Growth Chart, which were mailed to the participant at home (30). Each weight was recorded in pounds to one decimal place and height was recorded in centimeters to one decimal place. The results comparing a measured weight and height at a home or clinic visit or with a professional Tanita scale and resulted in a near-perfect correlation for weight (ρ = 0.99), with a mean difference of 2.4 pounds, and an almost perfect correlation for BMI (ρ = 0.98), with a mean difference of 0.6 BMI units. BMI was based on measured weight and height for 503 participants (82%) and self-reported height and weight for 111 (18%) and calculated as kilograms divided by meters square (kg/m2).
Covariates
To avoid model over fitting and to limit covariate on the pathway, we limited the number of covariates included in the analytic model, using a priori assumptions and evidence from prior NGHS studies to guide our variable selection. Covariates for the final model included participant’s race (White or African American), baseline household income ($0–9,999, $10,000–19,999, $20,000–39,999, >$40,000), baseline household educational attainment (high school or less, some college, college or more) and baseline BMI when the participant was aged 9 or 10. A missing indicator was used to account for 20 girls with missing household income data.
Statistical Methods
We examined the trajectories of drive for thinness throughout adolescence. We first calculated the interquartile range at each time point. We then estimated the association between drive for thinness and BMI for each time point that it was measured to identify if there was a linear relationship across time or if there was a critical period during adolescent that had the greatest association with adult BMI. As correlations were relatively constant across time points, we concluded that a summary adolescent drive for thinness score would be most relevant in predicting adult BMI, rather than drive for thinness at any particular age.
Structural equation modeling was used to examine the relationships between the variables of interest. We fit four equations simultaneously for the outcomes of adolescent drive for thinness, adult drive for thinness, adult reward-based eating drive and adult BMI, using the data’s inherent temporality to predict variable paths (Figure 1).
Figure 1:
Conceptual model of adolescent drive for thinness and BMI in adulthood
For example, adolescent drive for thinness was predicted by baseline BMI, baseline household income and race. Adult drive for thinness and reward-based eating drive were both predicted by baseline BMI and adolescent drive for thinness. Adult BMI was predicted by all of the model covariates. Total, direct and indirect effects were estimated. Model fit was evaluated using the Comparative Fit Index (CFI) >0.90, root mean square error of approximation (RMSEA) <0.08 and standardized root mean squared residual (SRMR) <0.05 (31). We report both unstandardized (B) and standardized (β) estimates, and focus our interpretations on the unstandardized estimates.
For comparison, we also conducted a sensitivity analysis by omitting participants who met the criteria of being above the 95th percentile for age and sex at baseline (n=112, 18%) to establish that any effect of adolescent drive for thinness on adult BMI was not due to obesity at baseline. Baseline obesity was determined using age- and gender-specific cutpoints for child overweight and obesity from the Center for Disease Control Growth Charts (32). All statistical tests were two-sided and statistical significance considered at P<0.05. Statistical analyses were conducted using Stata/SE 14 (StataCorp, College Station, TX).
Results
Women were aged 37–43 at the time of the follow-up study. Table 1 shows the baseline characteristics and outcome variables. The average weight of the participants in the follow-up study was 190.0 pounds (SD = 55.6, range: 103–444). Calculated mean BMI was 31.8 (SD ± 9.4). Most women (79%) had children – on average, they had 2.3 (SD ± 1.2) children with mean age of 10.1 years (SD ± 5.7). The mean score for drive for thinness in the follow-up sample was 9.3 (SD ± 7.3). The mean score for RED was 0.77 (SD ± 0.77). Drive for Thinness and RED were correlated at ρ = 0.41.
Table 1:
Characteristics of the NHLBI Growth and Health Follow-Up Participants (n=614)
| n | % | |
|---|---|---|
|
| ||
| Baseline characteristics (ages 9–10 years) | ||
| Race | ||
| White | 314 | 51.1 |
| Black | 300 | 48.9 |
| Parental education | ||
| High school diploma or less | 131 | 21.3 |
| Any college | 286 | 46.7 |
| College graduate | 196 | 32.0 |
| Household income | ||
| $0–9,999 | 112 | 19.0 |
| $10,000–19,999 | 104 | 17.7 |
| $20,000–39,999 | 172 | 29.3 |
| ≥$40,000 | 200 | 34.0 |
| BMI (mean ± SD) | 18.8 ± 3.7 | |
| Follow-up characteristics (age 37–43 years) | ||
| BMI (mean ± SD) | 31.7 ± 9.1 | |
| ≥30 BMI | 311 | 50.3 |
| Reward-based Eating Drive (mean ± SD) | 0.77 (0.78) | |
| Drive for thinness (mean ± SD) | 9.3 (7.3) | |
During adolescence, the mean score for drive for thinness was 4.8 (SD ± 4.8), ranging from a minimum of 4.2 at age 15/16 to a peak of 4.9 at age 19/20 (Table 2).
Table 2:
Relation between adolescent drive for thinness and BMI in adulthood
| Drive for thinness score | Relation with BMI in adulthood* | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| N | Mean | Median | IQR | r | β | SE | P | |
|
| ||||||||
| Age 12–13 (Year 3) | 569 | 4.5 | 2.0 | 7.0 | 0.28 | 0.47 | 0.07 | 0.0001 |
| Age 14–15 (Year 5) | 540 | 4.2 | 2.0 | 6.0 | 0.22 | 0.37 | 0.07 | 0.0001 |
| Age 16–17 (Year 7) | 520 | 4.7 | 2.0 | 8.0 | 0.18 | 0.29 | 0.07 | 0.0001 |
| Age 18–19 (Year 9) | 564 | 4.4 | 2.0 | 7.0 | 0.19 | 0.31 | 0.07 | 0.0001 |
| Age 19–20 (Year 10) | 596 | 4.9 | 3.0 | 9.0 | 0.21 | 0.34 | 0.06 | 0.0001 |
| Adolescent average | 615 | 4.8 | 2.8 | 8.0 | 0.27 | 0.52 | 0.08 | 0.0001 |
Adjusted for race, baseline household income, baseline household education, and baseline BMI
Note: IQR=Inter-quartile range.
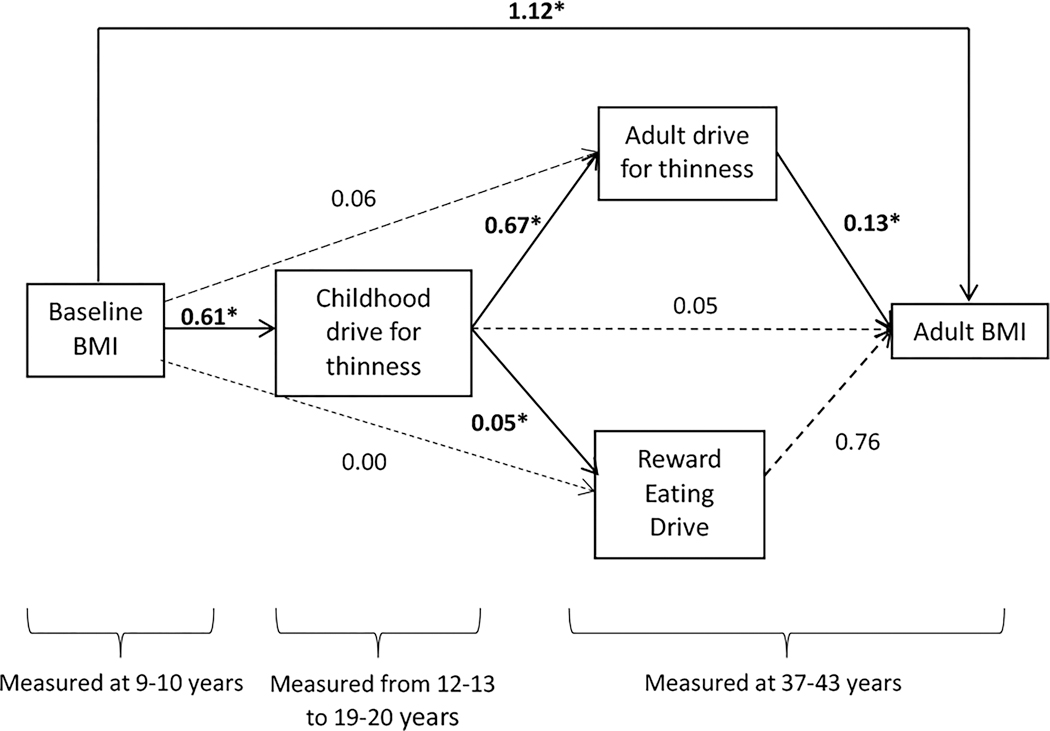
A significant association between drive for thinness and adult BMI was found starting at age 10 and remained significant until the end of adolescence, after adjusting for race, baseline household income, and baseline BMI. The cumulative (average) drive for thinness had the largest association with adult BMI (β = 0.52), compared to any single measurement in time, suggesting that increasing exposure may be the most relevant pathway to adult BMI. The proposed structural equation model fit the data well: CFI was 0.962; RMSEA was 0.10; and SRMR was 0.04 (Figure 2).
Figure 2:
Results of Structural Equation Modeling for the association between adolescent drive for thinness and BMI in adulthood.
Coefficients are unstandardized estimates (B). Solid lines represent paths significant at P<0.05. Dashed lines represent non-significant paths.
* p-value significant at < 0.05.
Table 3 shows both unstandardized and standardized regression coefficients from the full structural equation model. From the unstandardized model, adolescent drive for thinness was positively predicted by baseline child BMI (B=0.61, 95% CI 0.53, 0.70) independent of race and household income. Higher adolescent drive for thinness significantly predicted higher adult drive for thinness (B=0.67, 95% CI 0.54, 0.81) and adult reward-based eating drive (B=0.05, 95% CI 0.04, 0.07), and was only associated with adult BMI through adult drive for thinness (B=0.13, 95% CI 0.03, 0.22), controlling for race, maternal education, household income and baseline BMI.
Table 3:
Associations between averaged adolescent drive for thinness during adolescence and adult eating behavior and body mass index using structural equation modeling in the NHLBI Growth and Health Study (N=577)
| Unstandardized B | 95% CI | Standardized β | 95% CI | |
|---|---|---|---|---|
|
| ||||
| Adolescent drive for thinness | ||||
| Baseline BMI | 0.61* | 0.53, 0.70 | 0.50* | 0.44, 0.56 |
| Black race | -2.25* | -2.97, −1.53 | -0.24* | -0.31, −0.17 |
| Baseline household income - $10,000–19,999 | -1.27* | -2.36, −0.18 | -0.10* | -0.19, −0.02 |
| Baseline household income - $20,000–39,999 | -0.58 | -1.60, 0.43 | -0.06 | -0.16, 0.04 |
| Baseline household income - ≥$40,000 | -0.66 | -1.73, 0.40 | -0.07 | -0.18, 0.04 |
| Baseline household education – some college | -0.19 | -1.05, 0.67 | -0.02 | -0.11, 0.07 |
| Baseline household education –college or more | -0.14 | -1.13, −.84 | -0.01 | -0.11, 008 |
| Adulthood drive for thinness | ||||
| Baseline BMI | 0.06 | -0.10, 0.22 | 0.03 | -0.05, −0.11 |
| Adolescent drive for thinness | 0.67* | 0.54, 0.81 | 0.43* | 0.35, 0.51 |
| Reward-based eating drive | ||||
| Baseline BMI | 0.00 | -0.01, 0.02 | 0.02 | -0.07, 0.11 |
| Adolescent drive for thinness | 0.05* | 0.04, 0.07 | 0.32* | 0.23, 0.40 |
| Adulthood BMI | ||||
| Baseline BMI | 1.16* | 0.98, 1.34 | 0.48* | 0.41, 0.55 |
| Adolescent drive for thinness | 0.05 | -0.11, 0.21 | 0.02 | -0.06, 0.10 |
| Adulthood drive for thinness | 0.13* | 0.03, 0.22 | 0.10* | 0.03, 0.18 |
| Black race | 4.13* | 2.76, 5.51 | 0.22* | 0.15, 0.30 |
| Baseline household income - $10,000–19,999 | -0.88 | -2.86, 1.10 | -0.04 | -0.12, 0.05 |
| Baseline household income - $20,000–39,999 | -0.97 | -2.82, 0.88 | -0.05 | -0.14, 0.04 |
| Baseline household income - ≥$40,000 | -1.32 | -3.26, 0.62 | -0.07 | -0.17, 0.03 |
| Baseline household education – some college | -1.52 | -3.08, 0.04 | -0.08 | -0.17, 0.02 |
| Baseline household education –college or more | -1.95* | -3.74, −0.16 | -0.10* | -0.19, −0.01 |
| Reward-based Eating Drive | 0.76 | -0.09, 1.34 | 0.06 | -0.01, 0.14 |
P<0.05
LR test of model vs. saturated: chi(2) = 94.50, P<0.0001 for both models
Childhood BMI was the largest predictor of adulthood BMI, and worked both through direct means (B = 1.12, 95% CI = 0.98, 1.34), as well as indirect means, through drive for thinness. Childhood BMI was not directly associated with either adult drive for thinness or adult reward-based eating drive. The total effect of adolescent drive for thinness on adult BMI (β=0.17) was comprised of a small direct effect (β=0.05) and a larger indirect effect that was mediated through adult drive for thinness (β=0.13) (data not shown). The results did not differ in sensitivity analyses excluding women who were considered obese at baseline when they were 9 to 10 years old (n=112).
Discussion
Drive for thinness is a critical concept to understand as it is common and can start early in life (29). As we found in an earlier study, this was a predictor of weight gain during childhood, up to 19 years old, the last time they were followed during youth (27). Here we assess their eating behavior now in their 40’s. We found as we hypothesized that the cumulative drive for thinness during childhood leads to a continued strong of drive for thinness twenty years later, in adulthood as well as scoring higher on adulthood reward-based eating drive. Furthermore, adolescent drive for thinness, independent of childhood BMI, had a significant indirect effect on adult BMI that was mediated through adult drive for thinness (but not through reward-based eating drive). Drive for thinness is easy to assess and in important predictor of adult metabolic health. Over half of the participants in this sample have a BMI over 30, and thus high risk for current or future obesity related metabolic disease.
The results from this follow-up study also suggest that adolescent drive for thinness may be a major determinant of not only continued drive for thinness but also of reward driven compulsive eating— such as preoccupation with food, feeling unsatiated and out of control. Surprisingly, reward driven eating was not cross sectionally associated with adult BMI in this sample, whereas drive for thinness was. Perhaps the drive for thinness indicates behaviors that are more obesogenic over time. Drive for thinness may tap a more challenging set of behaviors that contribute to excess weight—highly restrictive eating, typically followed by over-eating (as measured by the item asking about “struggling with weight”) compared to the behaviors captured by reward-based eating drive, which does not include any dieting behavior.
Roughly half of this sample of midlife women met the BMI cut-off for obesity. Interventions are needed to help address unhealthy eating behaviors early in life, especially such constructs as drive for thinness that captures desire to diet to help women manage weight and reduce risk of weight related chronic diseases. Such interventions may need to start before puberty and continue throughout adolescence, given that we saw consistent relationships between drive for thinness and BMI across childhood to adolescence and cumulative drive for thinness was related to outcomes at age ~40.
Drive for thinness is a potential target for early intervention because it is an important predictor of a variety of eating disorders as well as weight gain (33). Cognitive behavioral therapy has been used to address drive for thinness among young adults who score high on internalized weight bias (33). The implications of this study are also important to parents who can play a role in helping children develop a balanced or healthy restraint – not too high or low—early in life. Parental behaviors likely shape eating and dietary behaviors. For example, parents setting limits on and restricting young girls at age five from snacking has been associated with higher scores on eating in the absence of hunger and BMI at age seven compared to setting limits but not restricting or no limit setting (34). However, permitting child self-serve portions at meal time may need to be coupled with guidance and rules, especially among young children with higher BMI (35). Interventions are also needed to help mothers manage weight and eating related thoughts, emotions and behaviors because these maternal behaviors can increase child restrained eating behaviors (36).
These findings should be taken in light of the limitations to this study. There was a larger percentage of those who participated among eligible cohort members from the California site that came from families of higher socioeconomic status compared to eligible non-participants. Therefore, this may bias the results away from or toward a stronger finding.
We are also aware that there are many studies that suggest dieting behavior is a strong predictor of weight gain, not drive for thinness per se (1). This study did not have a measure of dieting behavior so we were not able to compare the two. However, results suggest that drive for thinness in adolescence is by no means benign. Drive for thinness is shaped in during childhood, tracks through adulthood, and predicts level of greater weight status.
Another limitation is that we only studied females; however, dieting behaviors are much higher in girls than boys (37) (38). Dieting has also been associated with mental health, which was not part of the current analysis (39). Future research is needed to examine the extent to which these findings apply to boys, and identify appropriate interventions. Despite these weaknesses, our study had notable strengths, such as prospectively collecting information on drive-for-thinness multiple times throughout adolescents, measured weight and height, and the long-time frame of the cohort.
Conclusions
Adolescent drive for thinness in girls has a long shadow on adulthood health. It tracks throughout adulthood, it predicts compulsive eating behavior, and greater weight mass independent of childhood weight. Given the associations with obesity related diseases, drive for thinness is a serious early risk factor for early morbidity. Further understanding of these relationships may help to design obesity prevention programs to address drive for thinness in adolescents.
Study Importance.
- What is already known about this subject?
Dieting and weight control are associated with weight gain in the short term
Dieting has been found to be a source of stress
- What are the new findings in your manuscript?
Drive for thinness during critical developmental periods has long-term effects on adulthood eating behaviors
Drive for thinness throughout life leads to greater weight gain in midlife
- How might your results change the direction of research or the focus of clinical practice?
Preoccupation with thinness and negative emotions about eating may be an important predictor of metabolic health
Interventions are needed to help women manage negative thoughts and emotions about weight and eating
Acknowledgements
This study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development grant Race, stress and dysregulated eating: Maternal to child transmission of obesity [R01HD073568], the National Heart, Lung, and Blood Institute grant Neighborhood Environments and Intergenerational Transmission of Cardiovascular Health [R56HL141878], and the National Institute on Aging grants Early Life Adversity, Cumulative Life Stress, Race, and Cellular Aging in Midlife Women and Offspring [R56AG059677 & R01AG059677]. We thank the Nutrition Policy Institute who provided consultation and support with historical study data. Most of all, we thank our incredible study participants.
Author disclosures:
B Laraia, C Leung, AJ Tomiyama, L Ritchie, P Crawford, and E Epel, none of the authors have a conflict of interest with a funding source.
Footnotes
BL, LR, PC, and EE conceived and carried out the study design and data collection; BL & CL conducted the data analysis; BL, CL, JT and EE completed the data interpretation. All authors were involved in writing the paper and had final approval of the submitted and published versions.
References
- 1.Lowe MR, Doshi SD, Katterman SN, Feig EH. Dieting and restrained eating as prospective predictors of weight gain. Front Psychol. 2013;4. doi: ARTN 577 10.3389/fpsyg.2013.00577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stice E, Cameron RP, Killen JD, Hayward C, Taylor CB. Naturalistic weight-reduction efforts prospectively predict growth in relative weight and onset of obesity among female adolescents. J Consult Clin Psych. 1999;67(6):967–74. doi: Doi 10.1037/0022-006x.67.6.967. [DOI] [PubMed] [Google Scholar]
- 3.van Strien T, Herman CP, Verheijden MW. Dietary restraint and body mass change. A 3-year follow up study in a representative Dutch sample. Appetite. 2014;76:44–9. Epub 2014/02/01. doi: 10.1016/j.appet.2014.01.015. [DOI] [PubMed] [Google Scholar]
- 4.Hill AJ. Does dieting make you fat? Br J Nutr. 2004;92 Suppl 1:S15–8. Epub 2004/09/24. [DOI] [PubMed] [Google Scholar]
- 5.Haines J, Neumark-Sztainer D. Prevention of obesity and eating disorders: a consideration of shared risk factors. Health Educ Res. 2006;21(6):770–82. Epub 2006/09/12. doi: 10.1093/her/cyl094. [DOI] [PubMed] [Google Scholar]
- 6.Garner DM, Olmstead MP, Polivy J. Development and Validation of a Multidimensional Eating Disorder Inventory for Anorexia-Nervosa and Bulimia. Int J Eat Disorder. 1983;2(2):15–34. doi: Doi . [DOI] [Google Scholar]
- 7.Striegel-Moore RH, Schreiber GB, Pike KM, Wilfley DE, Rodin J. Drive for thinness in black and white preadolescent girls. Int J Eat Disord. 1995;18(1):59–69. Epub 1995/07/01. [DOI] [PubMed] [Google Scholar]
- 8.Wiederman MW, Pryor TL. Body dissatisfaction, bulimia, and depression among women: The mediating role of drive for thinness. Int J Eat Disorder. 2000;27(1):90–5. doi: Doi . [DOI] [PubMed] [Google Scholar]
- 9.Green MW, Rogers PJ, Elliman NA, Gatenby SJ. Impairment of cognitive performance associated with dieting and high levels of dietary restraint. Physiol Behav. 1994;55(3):447–52. Epub 1994/03/01. [DOI] [PubMed] [Google Scholar]
- 10.Green MW, Rogers PJ. Impaired cognitive functioning during spontaneous dieting. Psychol Med. 1995;25(5):1003–10. Epub 1995/09/01. [DOI] [PubMed] [Google Scholar]
- 11.Hart KE, Chiovari P. Inhibition of eating behavior: negative cognitive effects of dieting. J Clin Psychol. 1998;54(4):427–30. Epub 1998/06/12. [DOI] [PubMed] [Google Scholar]
- 12.Bellisle F, Dalix AM. Cognitive restraint can be offset by distraction, leading to increased meal intake in women. Am J Clin Nutr. 2001;74(2):197–200. [DOI] [PubMed] [Google Scholar]
- 13.Baumeister RF, Bratslavsky E, Muraven M, Tice DM. Ego depletion: Is the active self a limited resource? Journal of Personality and Social Psychology. 1998;74(5):1252–65. doi: Doi 10.1037//0022-3514.74.5.1252. [DOI] [PubMed] [Google Scholar]
- 14.Hagger MS, Panetta G, Leung CM, Wong GG, Wang JCK, Chan DKC, et al. Chronic Inhibition, Self-Control and Eating Behavior: Test of a ‘Resource Depletion’ Model. Plos One. 2013;8(10). doi: ARTN e76888 10.1371/journal.pone.0076888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ward A, Mann T. Don’t mind if I do: disinhibited eating under cognitive load. J Pers Soc Psychol. 2000;78(4):753–63. Epub 2000/05/04. doi: 10.1037//0022-3514.78.4.753. [DOI] [PubMed] [Google Scholar]
- 16.Westenhoefer J, Broeckmann P, Munch AK, Pudel V. Cognitive control of eating behaviour and the disinhibition effect. Appetite. 1994;23(1):27–41. Epub 1994/08/01. doi: 10.1006/appe.1994.1032. [DOI] [PubMed] [Google Scholar]
- 17.Gibson EL. Emotional influences on food choice: sensory, physiological and psychological pathways. Physiology & behavior. 2006;89(1):53–61. Epub 2006/03/21. doi: 10.1016/j.physbeh.2006.01.024. [DOI] [PubMed] [Google Scholar]
- 18.Greeno CG, Wing RR. Stress-induced eating. Psychol Bull. 1994;115(3):444–64. Epub 1994/05/01. doi: 10.1037/0033-2909.115.3.444. [DOI] [PubMed] [Google Scholar]
- 19.Epel EE, Tomiyama AJ, & Dallman MF. Stress and reward neural networks, eating, and obesity. . In: Gold KDBMS, editor. Handbook of Food and Addiction. Oxford: Oxford University Press; 2012. [Google Scholar]
- 20.Arnsten AF. Stress signalling pathways that impair prefrontal cortex structure and function. Nat Rev Neurosci. 2009;10(6):410–22. Epub 2009/05/21. doi: 10.1038/nrn2648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tomiyama AJ, Mann T, Vinas D, Hunger JM, Dejager J, Taylor SE. Low calorie dieting increases cortisol. Psychosom Med. 2010;72(4):357–64. Epub 2010/04/07. doi: 10.1097/PSY.0b013e3181d9523c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tomiyama AJ. Stress and Obesity. Annu Rev Psychol. 2019;70:703–18. Epub 2018/06/22. doi: 10.1146/annurev-psych-010418-102936. [DOI] [PubMed] [Google Scholar]
- 23.Adam TC, Epel ES. Stress, eating and the reward system. Physiology & behavior. 2007;91(4):449–58. Epub 2007/06/05. doi: 10.1016/j.physbeh.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 24.Epel ES, Tomiyama AJ, Mason AE, Laraia BA, Hartman W, Ready K, et al. The reward-based eating drive scale: a self-report index of reward-based eating. PLoS One. 2014;9(6):e101350. Epub 2014/07/01. doi: 10.1371/journal.pone.0101350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mason AE, Epel ES, Aschbacher K, Lustig RH, Acree M, Kristeller J, et al. Reduced reward-driven eating accounts for the impact of a mindfulness-based diet and exercise intervention on weight loss: Data from the SHINE randomized controlled trial. Appetite. 2016;100:86–93. Epub 2016/02/13. doi: 10.1016/j.appet.2016.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Obesity and cardiovascular disease risk factors in black and white girls: the NHLBI Growth and Health Study. Am J Public Health. 1992;82(12):1613–20. Epub 1992/12/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rehkopf DH, Laraia BA, Segal M, Braithwaite D, Epel E. The relative importance of predictors of body mass index change, overweight and obesity in adolescent girls. Int J Pediatr Obes. 2011;6(2–2):e233–42. Epub 2011/01/20. doi: 10.3109/17477166.2010.545410. [DOI] [PubMed] [Google Scholar]
- 28.Williams RL, Schaefer CA, Shisslak CM, Gronwaldt VH, Comerci GD. Eating Attitudes and Behaviors in Adolescent Women - Discrimination of Normals, Dieters, and Suspected Bulimics Using the Eating Attitudes Test and Eating Disorder Inventory. Int J Eat Disorder. 1986;5(5):879–94. doi: Doi . [DOI] [Google Scholar]
- 29.Fabian LJ, Thompson JK. Body-Image and Eating Disturbance in Young Females. International Journal of Eating Disorders. 1989;8(1):63–74. doi: Doi . [DOI] [Google Scholar]
- 30.Wardle J, Carnell S, Haworth CM, Plomin R. Evidence for a strong genetic influence on childhood adiposity despite the force of the obesogenic environment. Am J Clin Nutr. 2008;87(2):398–404. Epub 2008/02/09. [DOI] [PubMed] [Google Scholar]
- 31.Hooper D, Coughlan J, Mullen M. Evaluating Model Fit: A Synthesis of the Structural Equation Modelling Literature. 7th European Conference on Research Methodology for Business and Management Studies. 2008:195–200. [Google Scholar]
- 32.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000. CDC Growth Charts for the United States: methods and development. Vital Health Stat 11. 2002(246):1–190. Epub 2002/06/05. [PubMed] [Google Scholar]
- 33.Marshall RD, Latner JD, Masuda A. Internalized Weight Bias and Disordered Eating: The Mediating Role of Body Image Avoidance and Drive for Thinness. Front Psychol. 2019;10:2999. Epub 2020/02/11. doi: 10.3389/fpsyg.2019.02999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rollins BY, Loken E, Savage JS, Birch LL. Maternal controlling feeding practices and girls’ inhibitory control interact to predict changes in BMI and eating in the absence of hunger from 5 to 7 y. Am J Clin Nutr. 2014;99(2):249–57. doi: 10.3945/ajcn.113.063545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Savage JS, Haisfield L, Fisher JO, Marini M, Birch LL. Do children eat less at meals when allowed to serve themselves? Am J Clin Nutr. 2012;96(1):36–43. doi: 10.3945/ajcn.112.035261. [DOI] [PubMed] [Google Scholar]
- 36.Francis LA, Birch LL. Maternal influences on daughters’ restrained eating behavior. Health Psychol. 2005;24(6):548–54. Epub 2005/11/17. doi: 10.1037/0278-6133.24.6.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.French SA, Story M, Downes B, Resnick MD, Blum RW. Frequent dieting among adolescents: psychosocial and health behavior correlates. Am J Public Health. 1995;85(5):695–701. Epub 1995/05/01. doi: 10.2105/ajph.85.5.695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Neumark-Sztainer D, Paxton SJ, Hannan PJ, Haines J, Story M. Does body satisfaction matter? Five-year longitudinal associations between body satisfaction and health behaviors in adolescent females and males. J Adolesc Health. 2006;39(2):244–51. Epub 2006/07/22. doi: 10.1016/j.jadohealth.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 39.Crow S, Eisenberg ME, Story M, Neumark-Sztainer D. Psychosocial and behavioral correlates of dieting among overweight and non-overweight adolescents. J Adolesc Health. 2006;38(5):569–74. Epub 2006/04/26. doi: 10.1016/j.jadohealth.2005.05.019. [DOI] [PubMed] [Google Scholar]