Sir,
Mucinoses can be nonspecific skin findings of lupus erythematosus (LE) as per Gilliam’s classification.[1] Usual presentations of primary mucinosis are that of skin-colored papules and plaques over the trunk and extremities.[2] Rarely, it can present as patchy alopecia quite different from classical lupus lesions over the scalp. We describe a case with mucinous lupus alopecia and papulonodular mucinosis as the sole clinical presentation in a case of systemic LE.
A 19-year-old male presented with multiple asymptomatic patches of hair loss over the scalp and a few slow-growing papules and nodules over upper limbs and face for 1 year. He had symptoms suggestive of Raynauds and arthralgias of small and large joints for the same duration. Since the last 6 months, he started to have generalized malaise and recurrent low-grade fever. There was no history of photosensitivity, muscle weakness, oral ulcers, or malar rash. He was evaluated for fever, but no definite infective focus could be found. There were five nonscarring alopecia patches over the parietal and occipital scalp [Figure 1a]. The lesions were flat without any infiltration, pigmentary alteration, or follicular plugging over the surface. Ill-defined skin-colored to erythematous soft to firm, nontender papules and plaques were present over bilateral arms, elbows, forearms [Figure 1b and c], along with a single skin-colored nodule over forehead. Dermoscopy of the alopecia showed multiple white dots and curved and coiled tiny hairs without any evidence of scarring [Figure 1d]. His systemic features were suggestive of a connective tissue disease, but skin lesions were not fitting into the classical cutaneous features of any of the disorders. For the scalp lesions, the possibility of alopecia areata was kept.
Figure 1.
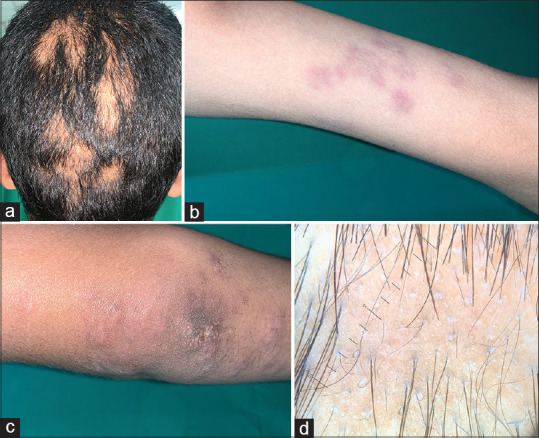
Multiple patches of nonscarring alopecia over parietooccipital scalp, (a) erythematous papules and plaques over arm (b), skin-colored to erythematous papules over the elbow and forearm (c), dermoscopy of patches over scalp showing white dots (black arrow), coiled hairs (red arrow) and curved hairs (blue arrow) (Heine Delta 20T, ×10) (d)
Investigations revealed leukopenia (total leukocyte count: 2300/mm3), thrombocytopenia (platelet count: 70,000/mm3), and anemia (hemoglobin: 9.2 g/dl). Direct Coombs test was positive. Urine examination showed albuminuria (urine albumin:creatinine ratio-573.63 microgram/mg). Both antinuclear antibody (183 units/dl) and ds DNA (402 units/dl) were positive. The clinical features and investigations were suggestive of systemic LE according to Systemic Lupus International Collaborating Clinics (SLICC) criteria,[3] but the skin lesions were difficult to explain. Biopsy from the scalp showed prominent mucin deposition in superficial and deep dermis perivascular and interstitial locations. There was no significant perifollicular infiltrate and no interface change [Figure 2a and b]. The papule over the arm and forehead showed a similarly normal epidermis, no interface change, or dermal infiltrate [Figure 2c] but prominent mucin deposition in a similar manner to that of the scalp [Figure 2d]. With clinicopathological correlation, the final diagnosis of mucinous lupus alopecia with papulonodular mucinosis associated with systemic lupus erythematosus (SLE) was made.
Figure 2.
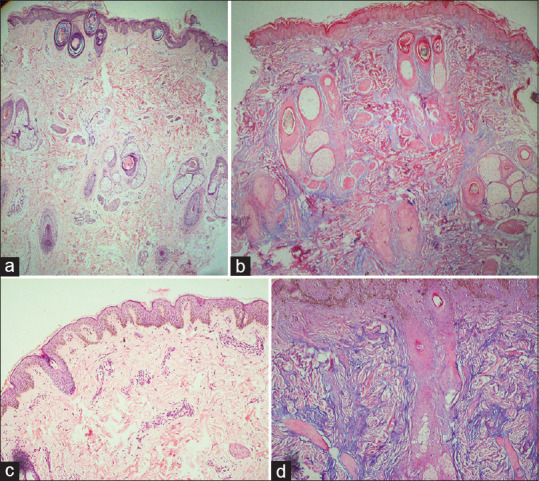
Biopsy from scalp showing miniaturized hair follicle and absence of significant infiltrate (H and E, ×100) (a) and special stain highlighted deposition of excess mucin in interstitial and peri-follicular location (Alcian blue and PAS, ×200) (b). Normal epidermis and lack of significant infiltrate in skin biopsy from the skin nodule (H and E, ×40) (c), moderate interstitial and perifollicular mucin deposition on special stain (Alcian blue and PAS, ×200) (d). PAS – Periodic acid–Schiff
He was treated with tablet of hydroxychloroquine 200 mg along with 30-mg prednisolone once daily. Prednisolone dose was tapered to 10 mg every month after his cytopenia recovered completely. After 3 months, there was a partial resolution of plaques and partial regrowth of hairs over the scalp.
Systemic LE has been associated with various types of alopecia both scarring and nonscarring. The most common of these is telogen effluvium often associated with lupus hairs. Localized hair loss could be due to discoid lupus-related scarring alopecia or alopecia areata as a nonspecific lesion of LE.[4] Mucinosis can be a rare cause of alopecia in LE patients.[5] Mucinosis per se has been described in LE in both primary and secondary forms. Secondary mucinosis is more common and present histologically in typical cutaneous lesions of lupus with classical histopathological features. Primary forms are characterized by only the deposition of mucin in the dermis without significant inflammation.[2] There are various forms of mucinosis described such as papulonodular mucinosis, reticular erythematous mucinosis,[6] and periorbital mucinosis.[7] Alopecia could be a very rare presentation in such setting. Our patient had both papulonodular mucinosis and mucionous alopecia. Papulonodular mucinosis (PNM) being the most common among the primary subset and typically presents more often in males either preceding at the same time or following the diagnosis of SLE.[2] They are commonly associated with arthritis and renal involvement and were present in our case too. As clinical manifestations can be nonspecific, diagnosis is made primarily on histopathology. Mucin deposition throughout the dermis in the absence of interface changes is characteristic. Dermal infiltrate could be variable. Direct immunofluorescence may demonstrate linear or granular deposits of immunoglobulin and/or complement protein. Various underlying pathogenetic factors such as cytokines, immunoglobulins, and androgens leading to increased accumulation of sulfated glycosaminoglycans had been postulated.[2] Treatment modalities such as corticosteroids and hydroxychloroquine have been used, but PNM particularly scalp lesions are less responsive to treatment and might fluctuate with disease severity. Our patient is a unique case presented with papulonodular mucinosis and mucinous nonscarring alopecia patches mimicking as alopecia areata.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Gilliam JN, Sontheimer RD. Skin manifestations of SLE. Clin Rheum Dis. 1982;8:207–18. [PubMed] [Google Scholar]
- 2.Kanda N, Tsuchida T, Watanabe T, Tamaki K. Cutaneous lupus mucinosis: A review of our cases and the possible pathogenesis. J Cutan Pathol. 1997;24:553–8. doi: 10.1111/j.1600-0560.1997.tb01459.x. [DOI] [PubMed] [Google Scholar]
- 3.Petri M, Orbai AM, Alarcón GS, Gordon C, Merrill JT, Fortin PR, et al. Derivation and validation of the systemic lupus international collaborating clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum. 2012;64:2677–86. doi: 10.1002/art.34473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Concha JS, Werth VP. Alopecias in lupus erythematosus. Lupus Sci Med. 2018;5:e000291. doi: 10.1136/lupus-2018-000291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee WS, Chung J, Ahn SK. Mucinous lupus alopecia associated with papulonodular mucinosis as a new manifestation of lupus erythematosus. Int J Dermatol. 1996;35:72–3. doi: 10.1111/j.1365-4362.1996.tb01624.x. [DOI] [PubMed] [Google Scholar]
- 6.Thareja S, Paghdal K, Lien MH, Fenske NA. Reticular erythematous mucinosis – A review. Int J Dermatol. 2012;51:903–9. doi: 10.1111/j.1365-4632.2011.05292.x. [DOI] [PubMed] [Google Scholar]
- 7.Morales-Burgos A, Sánchez JL, Gonzalez-Chávez J, Vega J, Justiniano H. Periorbital mucinosis: A variant of cutaneous lupus erythematosus? J Am Acad Dermatol. 2010;62:667–71. doi: 10.1016/j.jaad.2009.05.043. [DOI] [PubMed] [Google Scholar]


