Abstract
Background
South Sudanese have experienced prolonged exposure to conflict and displacement regionally and globally, with studies in different settings yielding vastly inconsistent rates of trauma-associated mental disorders. This systematic review and meta-analysis aimed to synthesize the methodological approach and quality, trauma exposure, risk and protective factors, and aggregate available data on the prevalence of trauma-associated mental disorders among South Sudanese in different settings to gain better understanding of the impact of war trauma in this population.
Methods
Guided by the new (2020) Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) statement, we conducted a systematic review and meta-analysis of all studies published from 1981 to 2021. The main inclusion criteria were as follows: studies published in English, present prevalence rates on anxiety, depression, and/or posttraumatic stress disorder (PTSD), and number of traumatic events, and have a sample size of 30 or more. We calculated pooled prevalence, 95% confidence intervals, and I2 statistic to test heterogeneity between studies in MedCalc statistical software.
Results
We reviewed a total of nine reports from eight unique studies with total of 6138 participants. All studies were cross-sectional in design with six designated as low quality and two as moderate quality. South Sudanese experienced on average nine war-related traumatic events. Consequently, the overall pooled rates of trauma-associated mental disorders are high: anxiety = 25.2% (95% CI: 14.0, 38.5); depression = 24.2% (8.4, 45.0); and PTSD = 34.0% (29.0, 39.1). Overall prevalence of PTSD was 40% in both preflight and flight settings; however, aggregate rate of just 14% was recorded in resettlement settings. Risk factors include female gender, advanced age, severity, and recency of traumatic events, and cultural adjustment difficulties. Protective factors include urban residency, social support, religion, higher annual household income, household possessions, and history of migration.
Conclusions
This systematic review and meta-analysis reveals that prolonged exposure to war trauma has negatively impacted the psychological wellbeing of South Sudanese in refugee camps and those still in their homeland. However, the prevalence appears to be lower among those resettled in developed countries.
Keywords: PTSD, Depression, Anxiety, War trauma, Refugees, South Sudanese
Background
War has severe direct and indirect effects on human health and development (Betancourt & Khan, 2008), which leads to immense suffering of mass populations. Beyond the obvious loss of life and destruction of property, war leads to devastating mental health consequences which may last for generations (Betancourt et al., 2020). The most common psychiatric disorders that result from war trauma include anxiety, depression, and posttraumatic stress disorder (PTSD) (Kanter, 2008; Lindert et al., 2018; Murthy & Lakshminarayana, 2006; Steel et al., 2002; Tol et al., 2011). Consistently, studies of refugees and post-conflict populations have found high prevalence rates of trauma-associated mental disorders ranging from 3 to 88% for PTSD, 12 to 85% for depression, and 25 to 81% for anxiety (Abu Suhaiban et al., 2019; Bogic et al., 2015; Johnson & Thompson, 2008; Lindert et al., 2018; Morina et al., 2018; Nesterko et al., 2019; Slewa-Younan et al., 2015).
In sub-Saharan Africa that has been affected by increasing number of conflicts, with just 12 conflicts in 1989 and a record-setting 25 state-based conflicts in 2019 (Palik et al., 2020), mental disorders are a serious public health threat in this region. One of the sub-Saharan Africa countries adversely affected by conflict is South Sudan, which has been in perpetual conflict for the last seven decades (Atari & McKague, 2015). During the prolonged period of conflict, which continue to this day, South Sudanese have been exposed to many atrocities including, rape, abduction of women and children, beheadings, looting and burning of livestock, and mass killings disproportionately targeting civilians (Jok, 2015). During the second Sudanese civil war from 1983 to 2005 alone, an estimated 2.5 million South Sudanese died and over 5.5 million were displaced from their homes (Collins, 2008). Moreover, in the most recent conflict that began in December 2013, it is estimated that over 400,000 people have been killed and approximately 4.5 million people, 41% of the country’s 11 million citizens, have been forcibly displaced to refugee camps in neighboring countries or internally displaced persons (IDP) camps (Sullivan, 2018).
In addition to the traumatic events that they faced during the civil wars, South Sudanese also faced significant challenges under displacement in refugee camps such as insecurity, gender-based violence, overcrowding, poor housing, and scarcity of food (Bashir, 2018; Chkam, 2016). Moreover, masses of South Sudanese refugees who had settled in refugee camps in Ethiopia had to flee back into South Sudan when the government that had supported them was overthrown in 1991 (Tutlam, 2013). Many people, including unaccompanied minors famously known as the “lost boys of South Sudan” perished during the flight back to a country still at war and the survivors had to make grueling journeys through hostile territories to reach refugee camps in Kenya where some were then processed for resettlement in the west (Geltman et al., 2005). Many would end up residing in the camp for three decades and continue to live there to this day. Even upon resettlement in the west, additional acculturative stressors and other potential traumas such as community violence, racism, and discrimination, which contribute to psychological distress, have been a part of the refugee experience (Betancourt et al., 2017; Ellis et al., 2008; Schweitzer et al., 2006).
While a number of studies have been conducted to assess the mental health impact of conflict among South Sudanese in different settings, these studies have yielded vastly inconsistent findings in terms of the prevalence of trauma-associated mental disorders. There are a number of potential factors for these observed inconsistencies including study design and quality issues, type of instruments used, and settings. Therefore, there is need to synthesize all available evidence to understand the source of these discrepancies and the overall extent of trauma-associated mental disorders and their associated risk and protective factors in this highly traumatized population and how rates of trauma-associated disorders may differ across different settings. This systematic review and meta-analysis, modeled after phases of refugee experience described by Lustig et al. (2004), that is, preflight, flight, and resettlement settings had the following objectives: (1) identify common measures used to assess trauma-associated mental disorders and synthesize methodological approaches and quality of mental health studies conducted among South Sudanese; (2) explore the extent of preflight trauma exposure and compute the average number of traumatic events experienced by South Sudanese participants reported in these studies; (3) aggregate overall prevalence of trauma-associated disorders; (4) compute pooled prevalence of trauma-associated disorders in different settings; and (5) summarize risk and protective factors for the different trauma-associated disorders in different settings.
Methods
We conducted a systematic review and meta-analysis of all studies on the mental health of South Sudanese. This review was guided by the new 2020 Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) statement (Page et al., 2021); a flow chart of how articles included in the review were identified and selected is presented in Fig. 1.
Fig. 1.
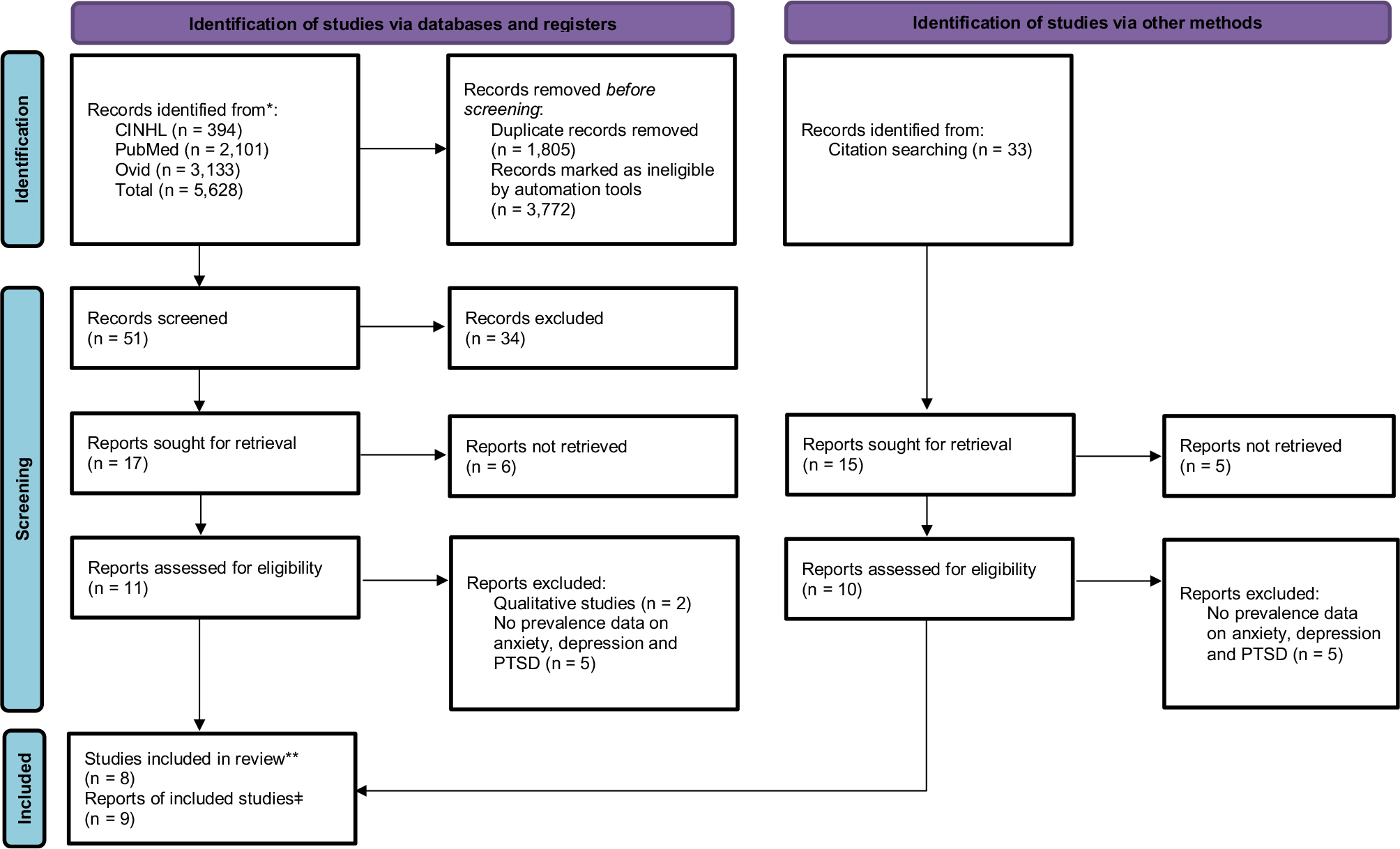
PRISMA flow chart outlining search process for selection of studies and reports included in this systematic review and meta-analysis. *Records identified from different databases using a combination of terms; **one study had two articles; ǂone article included data from two populations from two different settings. From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. https://doi.org/10.1136/bmj.n71. For more information, visit: http://www.prisma-statement.org/
Inclusion and Exclusion Criteria
The main criteria for inclusion in the review was that studies had to: (1) be quantitative in design; (2) present rates or prevalence of the most common trauma-associated mental disorders (anxiety, depression, and PTSD); (3) have data on the number of traumatic events experienced by participants; (4) assess risk and protective factors for development of trauma-associated mental disorders; (5) have a minimum sample size of 30 to maximize the number of published studies assessing these trauma-associated disorders in this population; and (6) be published in the English language. Multiple publications from the same study population were included if they presented additional information addressing the objectives under consideration (e.g., number of traumatic events and risk and protective factors). To assess the magnitude of trauma-associated mental disorders in different settings, we included studies conducted in South Sudan/southern Sudan (preflight setting); refugee camps or settlements (flight setting); and countries of resettlement (resettlement setting). We excluded qualitative studies because they were outside the scope of this review and would have required different methodological approach for analysis (Bogic et al., 2015). Additionally, we excluded non-English studies and those focusing on children under the age of 18 due to their differences from adults in responses to trauma (Ahmad et al., 2000); however, if a study included both adults and children such as the one by Peltzer et al. (1999), only data from adults were included in the review.
Information Source and Search Strategy
A literature search was conducted between June and October 2021 on the following search engines covering the period between 1981 and 2021: Google Scholar, Ovid, PsychInfo, PubMed, and CINAHL. In conducting the search, first, “South Sudan” was entered into the search box of CINAHL, Ovid, and PubMed to pull all research articles that contain “South Sudan” in their titles or key words. All these articles were then pulled into EndNote library for screening. A second round of search was conducted in the same data bases applying different combination of search terms, with the term “South Sudan” as a constant, to find additional articles that might have been missed if they did not contain “South Sudan” in their titles: South Sudan, refugees, trauma, war trauma, mental disorders, PTSD, anxiety, and depression. All these articles were then uploaded to EndNote library yielding a total of 5628 articles. After removing all duplicates, the titles of the remaining 3772 articles were screened by the first author. After this review, only 51 articles were deemed appropriate for further screening after which 17 were designated for full text retrieval. Through review of references and internet search on Google Scholar, we identified additional 33 articles, of which 15 were selected for full text retrieval.
After full screening of the final list of 32 articles, the full text of 21 articles was independently reviewed by two authors (NTT and JJC). After excluding articles that did not contain prevalence data on outcomes of interest, nine (9) articles from eight (8) unique studies met full inclusion criteria and were included in the review. A summary of these articles is presented in Table 1.
Table 1.
Summary of the studies reviewed
| Author/year | Setting | Population type | Sampling | Sample size | Age category | Instruments | Findings | Conclusions |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Ayazi et al. (2012) * | Bahr-el-Ghazal, South Sudan | Community | Multistage random cluster | 1200 | Adults | GHQ-28, HTQ, MINI | PTSD = 37.6%; depression = 15.9%; PTSD-depression = 9.5% | Risk factors for PTSD-depression similar to PTSD only but different from depression only |
| Ayazi et al. (2014) * | Bahr-el-Ghazal, South Sudan | Community | Multistage random cluster | 1200 | Adults | GHQ-28, HTQ, MINI | GAD-only = 7.1%; PD-only = 4.6%; PTSD-only = 25.5%; any anxiety disorder = 26% | Exposure to traumatic events and socioeconomic disadvantage associated with having one or more anxiety diagnosis |
| Fox and Willis (2009) | Nebraska, USA | South Sudanese refugees | Convenience sample | 31 | Adults | HSCL-25, HTQ | Traumatic events = 8.6; PTSD = 3%; Anxiety = 9%; Depression = 12% | Although the Sudanese suffered trauma resulting from their refugee experience, the prevalence rate for PTSD was lower than expected |
| Karunakara et al. (2004) | South Sudan and Uganda (West Nile Region) | Ugandan and Sudanese nationals; Sudanese refugees in Uganda | Multistage sampling | 3323 | Adults | PDS | PTSD in: Sudanese nationals = 48%; Sudanese refugees = 46%; Ugandan nationals = 18% | The symptoms of PTSD in war-affected Sudanese populations can be partly explained by traumatic events exposure |
| Ng et al. (2017) | South Sudan after the 2013 conflict | Community sample | Non-random sample | 1525 | Adults | HTQ-R | PTSD = 40.7; average number of traumatic events =7.6 | People with PTSD may prioritize ending violence through reconciliation; people exposed to more trauma want to see punitive measures. Study showed trauma-associated disorders still high after independence, perhaps as a result of retraumatization from the latest round of conflict |
| Peltzer (1999) | Refugee camp in Uganda | South Sudanese refugees, ex-soldiers | Convenience sample | 323 | Adults (n = 267), children (n = 56) | HTQ, HSCL-25, PTSD Questionnaire for Children | Depressive scale median score = 74.6 in ex-soldiers; 20% PTSD in children; 32% PTSD in adults | High rates of trauma and psychosocial problems were found among Sudanese refugees in Uganda |
| Roberts et al. (2009) | Juba, South Sudan | Community | Multistage random cluster | 1242 | Adults | HTQ, HSCL-25 | Depression = 50%; PTSD = 36%; trauma = 22% experienced ≥ 8 events | There is high prevalence of mental distress in the population in Juba town |
| Tutlam et al. (2020) | Nebraska and Tennessee, USA | Community | Convenience sample | 76 | Adult women | HTQ, HSCH-25 | Current anxiety = 39.5% Current depression = 28.9% Current PTSD = 26.3% Past anxiety = 26.3% Past depression = 21.1% Past PTSD = 15.8% Lifetime anxiety = 40.8% Lifetime depression = 31.6% Lifetime PTSD = 28.9% |
The study identified high level of war trauma among South Sudanese Dinka and Nuer women during the long civil war in South Sudan. As a result, the rates of trauma-associated disorders in the study sample were high |
| Schweitzer et al. (2006) | Southeast Queensland, Australia | Sudanese refugees | Snowball sampling | 63 | Adults | HTQ, HSCL-37, PMLD | Mean traumatic events = 5.6; MDD = 16%; PTSD = 13% | Refugees in Australia may constitute a particularly vulnerable group in terms of mental health outcomes. Culturally specific sequelae in terms of social isolation and acculturation may be particularly problematic for these migrants |
CHQ Child Health Questionnaire, DSI Daily Stress Inventory, GHQ-28 General Health Questionnaire, HTQ Harvard Trauma Questionnaire, HSCL-25 Hopkins Symptoms Checklist-25, HSCL-37 Hopkins Symptoms Checklist-37, IS Interview schedule for functional factors of social support, LCIACDS Levonn Cartoon-based Interview for Assessing Children’s Daily Distress Symptoms, MDD Major Depressive Disorder, MINI MINI International Neuropsychiatric Interview, PDS Posttraumatic Stress Diagnostic Scale, PTSD Posttraumatic Stress Disorder, RCQ WHO Reporting Questionnaire for Children, WC Ways of Coping Instrument, WGSSD Washington Group Short Measurement Set on Disability, YSR Youth Self Report
Articles from the same study but providing different outcomes of interest
Same population as study by Karunakara but included because this had additional data on risk factors
Statistical Analysis
Data extraction was performed by the first author (NTT) and reviewed by the third author (WB) For the systematic review, we extracted data on year of the study, sampling strategy, sample size, population, type, instruments utilized, number of traumatic events experienced, type and prevalence of traumatic events experienced, and risk and protective factors. Additionally, we extracted data required for assessment of the quality of the studies including sample information, comparison group, exposure/outcome measurement, follow-up, distorting influences, and data reporting (Table 2) and synthesized these applying the adapted version (Betancourt et al., 2013) of the Systematic Assessment of Quality in Observational Research (SAQOR) system originally developed by Ross et al. (2011) for assessing research quality in psychiatric research. Based on this, we rated the quality of the studies reviewed as high, moderate, low, or very low (see Table 2). We then conducted meta-analysis in MedCalc statistical software, version 18.6 (MedCalc, 2018) to compute prevalence rates and 95% confidence intervals, test for the degree of statistical heterogeneity between the studies, and generate forest plots. To compute prevalence rates, we extracted the raw numbers of the participants meeting diagnostic criteria for the primary outcomes of interest (anxiety, depression, and PTSD) and the total number of participants in the study and entered these data into MedCalc statistical software. For two of the studies reviewed (Fox & Willis, 2009; Karunakara et al., 2004), only proportions of those meeting criteria for mental disorders were reported. In these two cases, the proportion and total N were used to compute the number of people meeting criteria for mental disorders of interest that we then entered as raw values into MedCalc. We first generated prevalence rates and 95% confidence intervals for each of the trauma-associated disorders and, where possible, we also computed pooled prevalence rates for each of the three trauma-associated disorders (anxiety, depression, and PTSD) for the three different settings separately. Where there was only one study for which data were available on a specific mental disorder, we used the value for that study for the prevalence rates and computed 95% confidence intervals calculated in MedCalc. We used the I2 (inconsistency) statistic, which is automatically generated by MedCalc, to measure the degree of statistical heterogeneity between the studies. For this meta-analysis, we report the random effects value because of the known variability of the settings, and measurement instruments. To compute setting-specific and the overall average number of traumatic events experienced by the participants, we added the number of traumatic events from each study and divided them by the number of studies that had data available for this variable in each setting or overall. As this was a review of existing scientific literature, approval of an Institutional Review Board (IRB) was not required.
Table 2.
Rating of Systematic Assessment of Quality in Observational Research (SAQOR)*
| SAQOR Domains | |||||||||||||
| Sample | comparison group | Exposure/outcome measurement | |||||||||||
| Representative | Source | Method | Power Calculation | Inclusion Criteria | Summary | Inclusion | Identifiable | Source | Matched or randomized | Statistical control | Summary | Exposure | |
|
| |||||||||||||
| Ng et al. (2017) | Y | Y | Y | N | N | A | N/A | N/A | N/A | N/A | N/A | N/A | Y |
| Ayazi et al. (2014) | Y | Y | Y | N | N | A | N/A | N/A | N/A | N/A | N/A | N/A | Y |
| Roberts et al. (2009) | Y | Y | Y | Y | N | A | N/A | N/A | N/A | N/A | N/A | N/A | Y |
| Karunakara et al. (2004) | Y | Y | Y | Y | N | A | N/A | N/A | N/A | N/A | N/A | N/A | Y |
| Peltzer (1999) | N | Y | Y | N | N | I | N/A | N/A | N/A | N/A | N/A | N/A | Y |
| Fox and Willis (2010) | N | Y | Y | N | N | I | N/A | N/A | N/A | N/A | N/A | N/A | Y |
| Tutlam et al. (2020) | N | Y | Y | N | Y | A | N/A | N/A | N/A | N/A | N/A | N/A | Y |
| Schweitzer et al. (2006) | N | Y | Y | N | N | I | N/A | N/A | N/A | N/A | N/A | N/A | Y |
| Totals | 5 | 9 | 9 | 2 | 0 | 6 | 0 | 0 | 0 | 0 | 0 | 0 | 9 |
|
| |||||||||||||
| SAQOR Domains |
|||||||||||||
| Exposure/outcome measurement |
Follow-up | Distorting influences | Data reporting | Quality | |||||||||
| Outcome | Summary | Number lost | Reason for loss | Summary | Gender | Intervention | Stigma | Summary | Missing data | Clarity accuracy | Summary | ||
|
| |||||||||||||
| Ng et al. (2017) | N | I | N/A | N/A | N/A | Y | N | N | I | Y | Y | A | Moderate |
| Ayazi et al. (2014) | N | I | N/A | N/A | N/A | Y | N | N | I | Y | Y | A | Moderate |
| Roberts et al. (2009) | N | I | N/A | N/A | N/A | Y | N | N | I | N | Y | I | Low |
| Karunakara et al. (2004) | N | I | N/A | N/A | N/A | Y | N | N | I | N | Y | I | Low |
| Peltzer (1999) | N | I | N/A | N/A | N/A | N | N | N | I | N | Y | I | Low |
| Fox and Willis (2010) | N | I | N/A | N/A | N/A | N | Y | N | I | N | N | I | Low |
| Tutlam et al. (2020) | N | I | N/A | N/A | N/A | N | N | N | I | N | Y | I | Low |
| Schweitzer et al. (2006) | N | I | N/A | N/A | N/A | Y | N | N | I | N | Y | I | Low |
| Totals | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 9 | 3 | 3 Moderate 6 Low |
Adapted from Betancourt et al. (2013)
Results
Approximately 43% of the eligible studies that were reviewed in full met inclusion criteria and were included in the systematic review and meta-analysis (Fig. 1). Studies included in the systematic review and meta-analysis were published between 1999 and 2020, with four of them conducted in preflight settings, two were conducted in flight settings, and three were conducted in resettlement settings. These studies generally targeted adults, including males and females residing in these different settings; only two studies included both adults and children, but the children were excluded from analysis.
Measures, Study Design, Validation, and Overall Quality of Studies Reviewed
Seven of the eight (7/8) unique studies included in the review utilized the Harvard Trauma Questionnaire (HTQ) (Mollica et al., 1992) to assess PTSD. The HTQ is a self-report instrument that elicits information about 40 different traumatic events experienced by individuals and 40 different symptoms of PTSD. Of note, the first 16 items of this instrument are based on the DSM-IV criteria. The Posttraumatic Stress Diagnostic Scale (PDS) (Foa et al., 1997) was used to assess PTSD in one of the studies. This is a self-report measure that consists of 49 items. It measures the severity of PTSD symptoms in four different categories of ratings: 0 means no rating, 1–10 = mild, 11–20 = moderate, 21–35 = moderate to severe, and anything above 36 is considered severe. These ratings produce a symptom severity score ranging from 0 to 51. The most common instrument used for assessment of depression and anxiety was the Hopkins Symptom Checklist-25 (HSCL-25) (Mollica et al., 1987) with four studies utilizing it for assessing depression and anxiety. The HSCL-25 is also a self-report instrument made up of 25 items: 10 items measure anxiety symptoms and 15 measure depression symptoms. The study by Ayazi and colleagues employed the MINI International Neuropsychiatric Interview (MINI) (Sheehan et al., 1998) to assess depression and anxiety. This is a standardized psychiatric interview, which often serves as a gold standard for assessing psychiatric disorders. All of the studies included were cross-sectional in design; four of the unique studies employed multistage random cluster sampling while the remaining four used convenience or snowball sampling methods. Of all the studies reviewed, four utilized instruments translated to six local languages (Classic Arabic, Juba Arabic, Bari, Dinka, Nuer, and Shiluk); three studies relied on in vivo translation of the English version of instruments to Arabic, Nuer, and Dinka languages, while one study did not have any information on whether the instruments were translated to local languages or not. Crucially, although some of the studies used instruments translated a priori, none of the studies used instruments validated or developed specifically for local cultural contexts. In terms of the overall quality of the studies, two studies met designation of moderate quality, while the other six were determined to be low quality (Table 2).
The Extent of Preflight Setting Trauma Exposure Among South Sudanese
Overall, there was very high prevalence of war-related trauma exposure among South Sudanese. The lifetime prevalence of each of the different traumatic events experienced by South Sudanese is presented in Table 3. Notably, looking at the type of traumatic events participants were exposed to, some traumatic events were more common than others. For example, traumatic events, such as lack of food or water, loss of property, forced separation from family members and isolation, and murder or unnatural death of family member or friends, were common among South Sudanese participants, with prevalence as high as 94%. On the other hand, traumatic events such as rape and forced prostitution or sexual slavery were on the lower end of the spectrum, with prevalence ranging from 1 to 11%. Considering the number of traumatic events experienced by individuals, Roberts et al. (2009) reported that of the 1242 participants in their study, more than 92% had experienced one or more of the 16 trauma events listed on the questionnaire and about 23% experienced eight or more traumatic events. Similarly, Schweitzer et al. (2006) reported that 54% of their study sample reported experiencing approximately six traumatic events based on the original version of the HTQ, which consists of 16 traumatic events (Mollica et al., 1992). A more recent study by Ayazi et al. (2014) reported 15 traumatic events during the war versus just 2.5 traumatic events after the war in their study sample. The two studies conducted in the USA with data on traumatic events (Fox & Willis, 2009; Tutlam et al., 2020) found that a group of South Sudanese refugees living in Nebraska and Tennessee, on average, had been exposed to 9.2 traumatic events, which is similar to results from studies of South Sudanese refugees in Uganda and southern Sudan (Karunakara et al., 2004). The average number of traumatic events based on all the studies reviewed was nine; examples of these traumatic events can be found in Table 3.
Table 3.
Level of trauma exposure among South Sudanese
| Type of war trauma | Prevalence range | |
|---|---|---|
| 1 | Lack of food or water | 61–91% |
| 2 | Unnatural death of family or friend | 18–81% |
| 3 | Combat situation | 12–51% |
| 4 | Murder of family or friend | 16–68% |
| 5 | Witness of death of family member | 41–63% |
| 6 | Very ill without access to medical care | 16–62% |
| 7 | Lack of housing or shelter | 39–57% |
| 8 | Being close to death | 30–51% |
| 9 | Forced separation from family members | 26–91% |
| 10 | Serious injury | 7–26% |
| 11 | Tortured or beaten | 14–31% |
| 12 | Forced isolation from others | 6–94% |
| 13 | Murder of stranger or strangers | 18–19% |
| 14 | Forced to accept thoughts against will/brainwashing | 2–16% |
| 15 | Imprisonment | 6–27% |
| 16 | Being lost, abducted or kidnapped | 8–48% |
| 17 | Rape or sexual abuse | 2–11% |
| 18 | Forced prostitution or sexual slavery | 1–8% |
| 19 | Harassment by armed personnel | 16–26% |
| 20 | Loss of property | 57–94% |
| 21 | Witnessed rape of a woman | 9–33% |
| 22 | Had a child abducted* | 18% |
| 23 | Had a family member disappear* | 41% |
| 24 | Any other situation that was very frightening or you felt your life was in danger* | 91% |
Based on responses from one study that asked this question
Overall Pooled Prevalence of Trauma-Associated Disorders Among All South Sudanese
All the studies reviewed assessed the prevalence of PTSD in their study samples. As presented in Fig. 2, based on a combined total sample of 6138 from all settings, the pooled prevalence of likely PTSD is 34.0% (95% CI: 29.0, 39.1) (I2 = 92.8% (88.6, 95.5)). Only five of the studies reviewed assessed depression among participants, yielding a total sample of 2614. Among these participants, the pooled prevalence for likely depression is 24.2% (8.4, 45.0) (I2 = 98.9% (98.4, 99.2)) (Fig. 3). Only three studies, with a combined sample size of 416, investigated the prevalence of anxiety disorder. Among these participants, the pooled rate of likely anxiety is 25.2% (14.0, 38.5) (I2 = 84.1% (52.4, 94.7)) (Fig. 4).
Fig. 2.
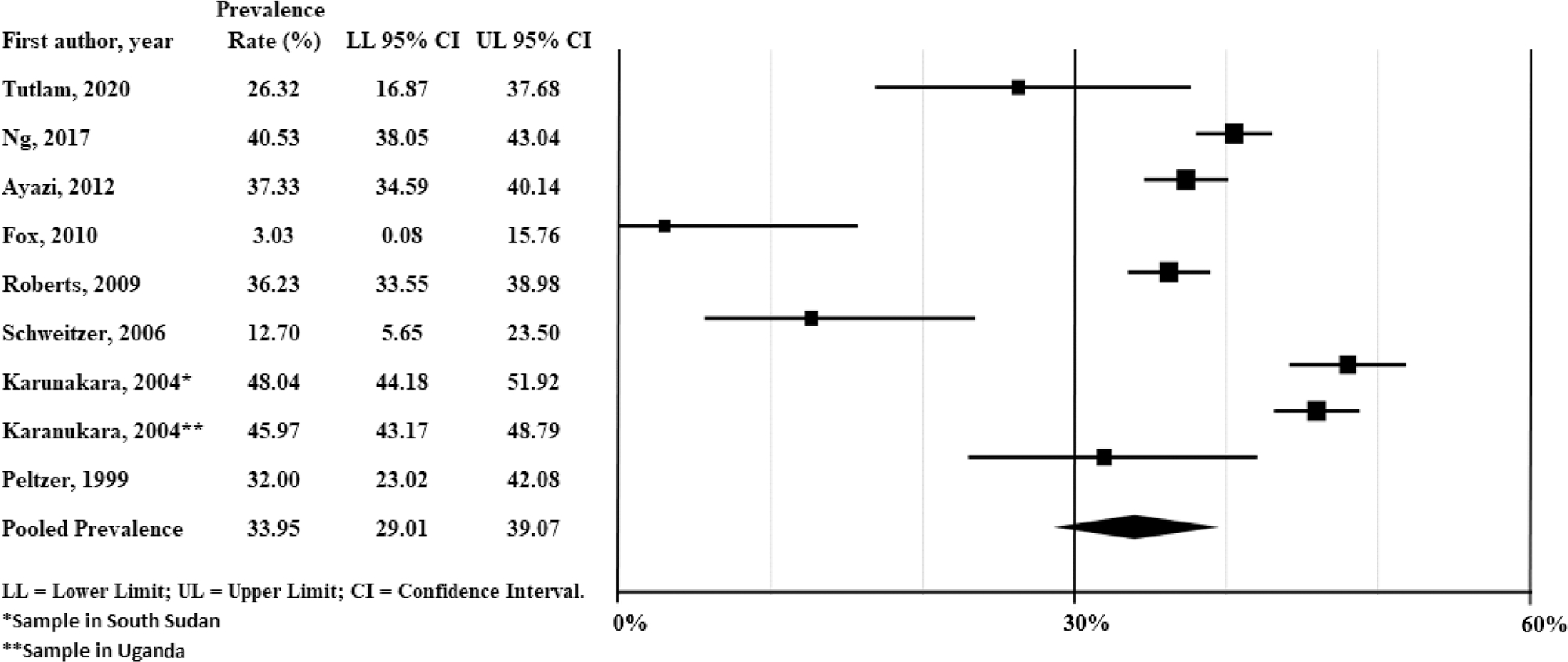
Forest plot of prevalence rates of post traumatic stress disorder (PTSD) across all South Sudanese studies reviewed (N = 6138)
Fig. 3.
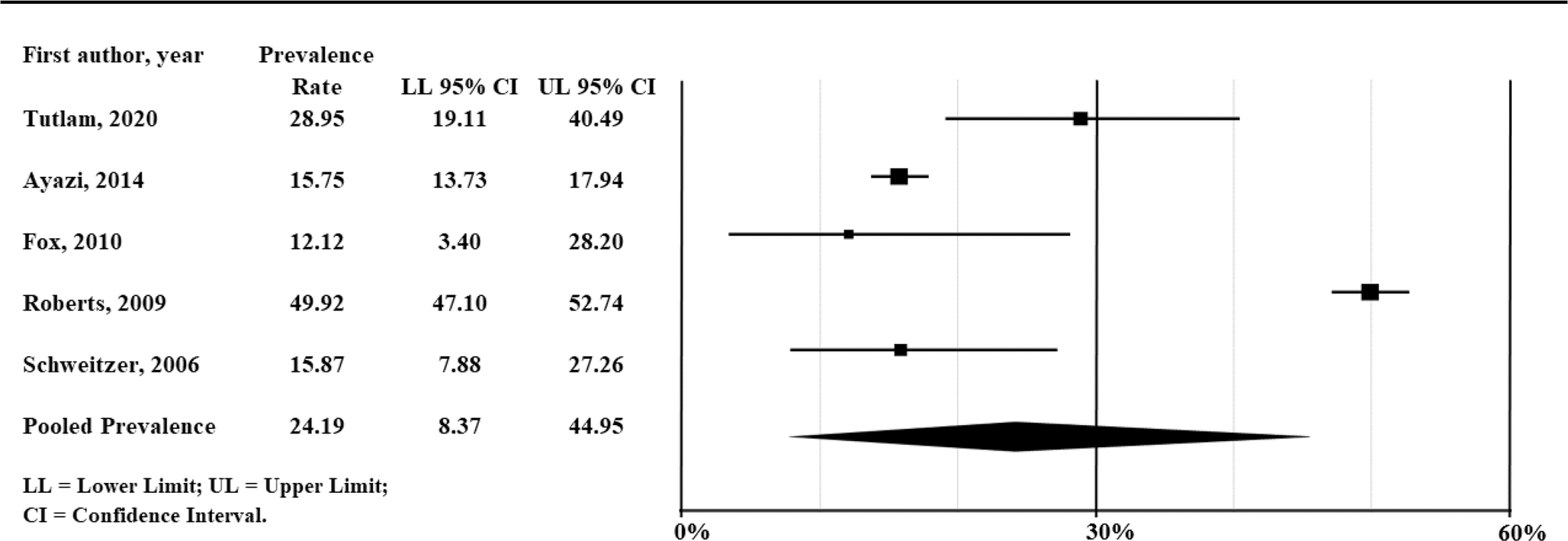
Forest plot of prevalence rates of depression across all South Sudanese studies reviewed (N = 2614)
Fig. 4.
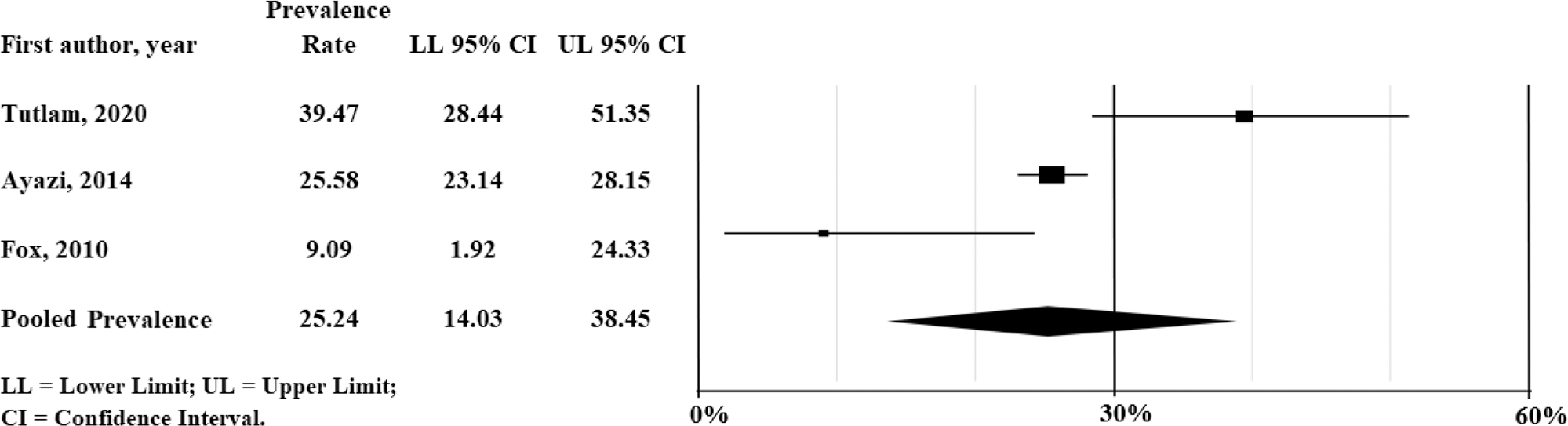
Forest plot of prevalence rates of anxiety across all South Sudanese studies reviewed (N = 416)
Prevalence of Trauma-Associated Mental Disorders Among South Sudanese in Different Settings
Studies Among South Sudanese in South Sudan/Southern Sudan (Preflight Setting)
The prevalence of trauma-associated disorders occurring in different settings is presented in Table 4. The prevalence of PTSD in these studies ranged from 36 to 48%. In the studies conducted among South Sudanese in South Sudan or Southern Sudan, based on a combined sample of 4626 participants, the pooled prevalence of likely PTSD is 40.4% (95% CI: 36.0, 44.8). There was a great deal of heterogeneity in these studies (I2 = 89.4%; 95% CI: 75.8, 95.4). Only two of the studies assessed depression prevalence and found 16% and 50% prevalence. The pooled prevalence of likely depression based on these two studies is 31.6% (95% CI: 5.1, 67.6). The sole study that reported data on anxiety found 26% meeting criteria for standard clinical thresholds (95% CI: 23.2, 28.2) (Ayazi et al., 2014).
Table 4.
Prevalence of various trauma-associated disorders and traumatic events
| Author/year | PTSD |
Depression |
Anxiety |
Average number of traumatic events | |||
|---|---|---|---|---|---|---|---|
| N | % (95% CI) | N | % (95% CI) | N | % (95% CI) | ||
|
| |||||||
| Studies among South Sudanese in South Sudan/southern Sudan preflight setting) | |||||||
| Ng et al. (2017) | 618/1525 | 40.55 (38.05, 43.04) | - | - | - | - | 7.6 |
| Ayazi et al. (2012) | 448/1200 | 37.33 (34.59, 40.14 | 189/1200 | 15.75 (13.73, 17.94) | 15.1 | ||
| Ayazi et al. (2014) * | - | - | - | - | 307/1200 | 25.58 (23.13, 28.15) | |
| Roberts et al. (2009) | 450/1242 | 36.23 (33.55, 38.98) | 620/1242 | 49.92 (47.10, 52.74) | - | - | - |
| Karunakara et al. (2004) | 319/664 | 48.04 (44.18, 51.92) | - | - | - | - | 7.0 |
| Integrative score | 1835/4626 | 40.36 (35.99, 44.81) | 809/2442 | 31.56 (5.11, 67.59) | 307/1200 | 25.58 (23.15, 28.15) | 9.9 |
| a (inconsistency) | - | 89.44 (75.75, 95.40) | - | 99.71 (66.54, 99.82) | |||
| Studies among South Sudanese in refugee camps (flight setting) | |||||||
| Karunakara et al. (2004) | 570/1240 | 45.97 (43.17, 48.79) | - | - | - | - | 9.8 |
| Peltzer (1999) | 32/100 | 32.0 (23.02, 42.08) | - | - | - | - | - |
| Integrative score | 602/1340 | 39.75 (26.78, 53.9) | - | - | - | - | 9.8 |
| a (inconsistency) | - | 86.71 (47.49, 96.64) | |||||
| Studies among South Sudanese in developed countries (resettlement setting) | |||||||
| Fox and Willis (2010) | 1/33 | 3.03 (0.08, 15.76) | 4/33 | 12.12 (3.40, 28.20) | 3/33 | 9.01 (1.92, 24.33) | 8.5 |
| Tutlam et al. (2020) | 20/76 | 26.32 (16.87, 36.67) | 22/76 | 28.9 (18.5, 39.4) | 30/76 | 39.47 (28.44, 51.35) | 9.7 |
| Schweitzer et al. (2006) | 8/63 | 12.70 (5.65, 23.50) | 10/63 | 15.87 (7.88, 27.26) | - | - | 5.6 |
| Integrative score | 29/169 | 13.98 (4.05, 28.55) | 36/172 | 15.26 (8.79, 23.63) ** | 33/99 | 23.75 (2.59, 57.10) | 7.1 |
| a (inconsistency) | - | 82.18 (45.11, 94.21) | 0.00 (0.00, 0.00) | 91.58 (70.57, 97.59) a | |||
Ayazi et al. published this second paper from the same population as the previous paper, but was included because it provides prevalence for anxiety
Value for fixed effect recorded due to very low heterogeneity value (I.2 = 0.00%)
for the two studies that assessed anxiety in the USA
Studies Among South Sudanese in Refugee Camps (Flight Setting)
Based on two studies conducted among South Sudanese in flight settings such as refugee camps, the prevalence of trauma-associated mental disorders was equally high. For example, one study among 100 adults from South Sudan in a refugee camp in Uganda found likely PTSD prevalence of 32% (Peltzer, 1999). The other study by Karunakara et al. (2004) found 46% likely PTSD prevalence among 1240 South Sudanese refugees in Uganda. The pooled prevalence of PTSD for this setting is 39.8 (26.8, 53.9). Although these two studies were conducted in the same general area and just a few years apart, there was high degree of variability between them (I2 = 86.7 (47.5, 96.6)). Neither of these studies assessed depression or anxiety prevalence (Table 4).
Studies Among South Sudanese Residing in Countries of Resettlement (Resettlement Setting)
There were only three studies conducted among South Sudanese adults resettled in developed countries (Australia and North America) that met our inclusion criteria. Two of the studies were conducted in the USA. The first study by Fox and Willis (2009) found the rate of likely PTSD among a group of South Sudanese (N = 33) in Nebraska to be just 3% (0.1, 15.8). The second study by Tutlam et al. (2020) among a sample of 76 South Sudanese women resettled in Nebraska and Tennessee found likely PTSD rate of 26.3% (16.9, 36.7). An additional study was conducted in Australia by Schweitzer and colleagues and found likely PTSD rate of 13% among 63 South Sudanese. The pooled rate of likely PTSD among South Sudanese resettled in the west, based on a total sample of 172, is 14% (4.1, 28.6). The pooled prevalence for likely depression in these studies is 15.3% (8.8, 23.6). Only the two studies conducted in the USA assessed anxiety, and based on these two studies, the pooled rate of those meeting standard diagnostic criteria for anxiety is 23.8% (2.6, 57.1) (Table 4).
Risk and Protective Factors Among South Sudanese in Different Settings
Studies Among South Sudanese in South Sudan/Southern Sudan (Preflight Setting Factors)
In the studies that assessed the risk factors for development of the various trauma-associated disorders, among participants in South Sudan/southern Sudan during or after the war, degree and recency of war trauma were significant risk factors (Ayazi et al., 2012; Karunakara et al., 2004; Peltzer, 1999; Roberts et al., 2009). Specifically, people who were exposed to ≥ 8 lifetime traumatic events had almost two and half to three fold likelihood of exhibiting likely PTSD diagnosis, and more than twice as likely to have clinical levels of depression (Ayazi et al., 2012; Roberts et al., 2009). Similarly, the recency of the trauma exposure increased the likelihood of PTSD, with exposure to ≥ 4 recent trauma events increasing the likelihood of PTSD and depression almost three fold and two fold, respectively (Roberts et al., 2009). This study also found that both older and recent trauma were risk factors for developing an anxiety disorder. Moreover, these studies have observed a clear dose–response relationship between level of trauma exposure and prevalence as well as severity of PTSD symptoms (Ayazi et al., 2012; Karunakara et al., 2004; Roberts et al., 2009).
Another significant risk factor for development of PTSD or depression is female gender (Ayazi et al., 2012; Karunakara et al., 2004; Roberts et al., 2009). When the prevalence was stratified by gender, women exhibited higher levels of likely PTSD compared to men (43% vs. 30%) and even higher levels of likely depression (59% vs. 41%) (Roberts et al., 2009). In this study, Roberts et al. (2009) found that women had double the risk of developing PTSD 2.4 (95% CI: 1.9, 2.9) and greater odds of having depression. Other factors include advanced age, having witnessed violent events ever or in the past year or trauma exposure (Karunakara et al., 2004; Roberts et al., 2009); urban residency, being a returnee from the refugee camps after the war, severe socioeconomic disadvantage among those in South Sudan (Ayazi et al., 2012); forceful displacement more than once, and being no longer married (divorced/separated), experiencing ill health without medical care, and being injured (Roberts et al., 2009). Similarly, of the studies that assessed protective factors, Roberts et al. (2009) identified urban residency as a factor protective against depression in a sample of South Sudanese in the capital city, Juba.
Studies Among South Sudanese in Refugee Camps (Flight Setting Factors)
Karunakara et al. (2004) assessed risk and protective factors among South Sudanese refugees in northern Uganda and some drawn from those still residing in South Sudan. They found age, gender, and witnessing traumatic events to be risk factors for developing PTSD, similar to other studies in southern Sudan. The same study found the protective factors included having some education (aOR = 0.6; 0.4, 0.9), having a salaried job (aOR = 0.4; 0.2, 0.8), having household possessions (aOR = 0.8; 0.7, 0.9), and having a history of forced migration from their homeland (aOR = 0.6; 0.5, 0.9).
Studies Among South Sudanese Resettled in Developed Countries (Resettlement Setting Factors)
Refugee populations that have been resettled in developed countries tend to have different challenges compared to those in refugee camps or native country. The sole study in Australia that met our inclusion criteria by Schweitzer et al. (2006) found post-migration stressors such as concerns about not being with family, employment difficulties, and cultural adjustment difficulties, to be important risk factors for development of mental disorders. This study also found factors such as religion, social support from family and South Sudanese community, and governmental support to be protective against development of psychiatric disorders (Schweitzer et al., 2006). The two studies in the USA (Fox & Willis, 2009; Tutlam et al., 2020) found that factors such as low education level, being over 35 years of age, and having teeth removed in childhood increased likelihood of trauma-associated mental disorders among participants. The study by Fox and Willis (2010) found that restoration of teeth removed during childhood notably reduced trauma-associated mental disorders among a group of 33 South Sudanese participants resettled in Nebraska. Similarly, Tutlam et al. (2020) found being divorced or separated and having high annual household income as protective factors against trauma-associated mental disorders.
Discussion
This systematic review and meta-analysis examined the prevalence of trauma-associated mental disorders and their associated risk and protective factors and found high levels of exposure to trauma among South Sudanese during the Second Sudanese Civil War (1983–2005) and beyond. The average number of traumatic events (nine) across the different South Sudanese studies is consistent with findings of other studies in the region. Specifically, similar to findings of studies of other African refugees, we found an average number of traumatic events experienced by participants ranging from eight to fourteen across the different studies and settings (Barbieri et al., 2019; Lambert & Alhassoon, 2015; Onyut et al., 2009). Previous studies have found that the risk of mental disorders such as anxiety, depression, and PTSD increases with increasing number of traumatic events experienced (Do et al., 2019). Indeed, as demonstrated by previous studies (Kolassa et al., 2010; Neuner et al., 2004; Pfeiffer & Elbert, 2011; Scholte et al., 2004; Steel et al., 2009), the South Sudanese refugee studies also showed a dose–response relationship between the number of traumatic events and likelihood of developing PTSD. Neuner et al. (2004) showed that as number of traumatic events increased, PTSD prevalence increased proportionally, with 100% of those reporting 28 or more traumatic events being positive for PTSD symptomology. However, they also demonstrated a j-shaped relationship between the number of traumatic events and PTSD severity. There is not a simple cumulative effect; the effect accelerates as number of traumatic events increase.
The high level of traumatization from conflict-related traumatic events has resulted in high overall prevalence of trauma-associated mental disorders among South Sudanese. There were, however, significant disparities in prevalence rates for participants studied in settings of preflight, flight, or resettlement. Despite some studies indicating that the prevalence of trauma-associated disorders may be particularly higher among those in refugee camps (Jaranson et al., 2004), this review found comparable rates of war trauma both in conflict-affected South Sudan (preflight setting) and in the refugee camps (flight setting). These findings are supported by the ADAPT model which posits that disruption of the core psychological pillars negatively affects the psychological wellbeing of the war-affected population (Silove, 2013). Namely, disruption of the pillar of safety/security eventually leads to negative psychological impact that is manifested as PTSD, anxiety, and depression in the population. This theory is supported by evidence from a systematic review of studies from ten sub-Saharan Africa (SSA) counties conducted by Ng et al. (2017), which found very high prevalence of likely PTSD (30%) in countries affected by conflict, compared to a rate of just 8% in regions not affected by conflict.
On the other hand, based on this systematic review and meta-analysis, South Sudanese resettled in developed countries appear to have significantly lower prevalence rates than their counterparts in refugee camps or in their native land, with pooled prevalence rates of 14% for likely PTSD, 15% for likely depression, and 24% for likely anxiety. A plausible explanation for the low finding may be related to the notion of posttraumatic growth. This is the idea that people who have experienced trauma or tragedy undergo a positive psychological change (Calhoun & Tedeschi, 1999). Studies have found that women tend to have more post traumatic growth compared to men (Tedeschi & Calhoun, 1996) and the fact that women constitute the vast majority of the participants in these studies may support this proposition.
Additionally, these low rates would seem to lend credence to the theory that suggests effects of trauma diminish with time following resettlement in developed countries (Tran et al., 2007). However, this theory is not consistently supported by evidence as the study by Fox and Willis (2009) with the lowest rate of likely PTSD (3%) was conducted when the participants had been in the USA for only about 4 years on average, while in the study with the relatively higher rate by Tutlam et al. (2020), from a relatively larger community sample, the participants had lived in the USA for an average of 16 years.
Moreover, although these studies found low rates of likely PTSD among those resettled in the west, when Fox and Willis (2009) reviewed individual symptoms in their sample, they found high rates of PTSD symptoms, such as avoidance (67%), recurrent thoughts of most traumatic event (60%), recurring nightmares (58%), and feeling on guard (55%), indicating a high level of distress. Therefore, the findings of low overall prevalence in these studies are somewhat surprising and inconsistent with previous studies of other resettled refugee populations that suggest the effects of trauma persist for decades or even a lifetime. For example, a study among resettled refugees in the Netherlands found that the prevalence of PTSD was unchanged over the course of 7 years (Lamkaddem et al., 2014) and another study of Cambodian refugees found very high current (within past 12 months) prevalence of PTSD (62%) and depression (51%) 20 years after resettlement in the USA (Marshall et al., 2005). Similarly, Holocaust survivors have been found to have high levels of PTSD and other psychotic disorders more than half a century after exposure to their trauma (Barak & Szor, 2000).
This review has found wide variability in the prevalence of the different trauma-associated mental disorders, and even the prevalence of traumatic events. An important factor that may be contributing to wide variabilities in results of the studies included in the review is sampling problems and lack of robust study designs. In particular, studies included in this review employed different sampling strategies of varying qualities ranging from convenience and snowball sampling to multistage random cluster sampling. More important, there were no comparison groups or longitudinal studies and all the studies reviewed are cross-sectional and are vulnerable to selection bias inherent in this design. This is particularly important given that many of the studies did not employ random sampling methodology in participant selection. Indeed, when we applied the Systematic Assessment of Quality in Observational Research (SAQOR) system criteria (Ross et al., 2011) for assessing the research quality of the studies reviewed, only two of the eight unique studies met criteria for moderate overall quality while the other six were of low quality. Taken together, these factors may partly explain the high heterogeneity ranging from I2 = 82% to 91%.
Another crucial issue to consider vis-à-vis these vastly varying results is validity of the measures used to assess these trauma-associated disorders. Specifically, the diagnostic thresholds utilized for these studies have not received gold standard validation in this specific population. This is a critical procedure that requires careful step by step methodology to develop and validate context specific measures (Betancourt et al., 2012; Ng et al., 2014; Scorza et al., 2013). This is particularly important as concerns are often raised that instruments developed using Western definitions of anxiety, depression, and PTSD are inappropriately applied to new cultures and contexts where such disorders are seen as foreign (Summerfield, 1999). Although experts acknowledge that psychiatric disorders such as PTSD are valid universal reactions to traumatic experience (Kienzler, 2008), there are ethnic and cultural differences in how symptoms of psychiatric disorders are conceptualized and described (Kirmayer & Bhugra, 2009), which must be taken into consideration in these analyses.
A related issue concerns the use of different cutoff values for diagnosis of disorders. Even studies that use the same version of the instrument can result in different prevalence rates if they use different scoring cutoff points. For example, studies that utilize the revised HTQ and apply a cutoff point of ≥ 2.0 for PTSD diagnosis instead of the ≥ 2.5 cutoff value that is regularly cited in the literature can have higher PTSD prevalence. Simply applying the same cutoff value of ≥ 2.5, which was established in an Indochinese population, is problematic because this cutoff value is not necessarily the same for all populations. For example, the cutoff value in a primary healthcare setting for Bosnian refugees was found to be 2.03 (Mollica, 2004). In the absence of population-specific cutoff values, the developers of the HTQ recommend using cutoff value of ≥ 2.0 (Mollica, 2004).
Moreover, the use of different instruments may lead to wide variations. For example, studies that use the Harvard Trauma Questionnaire (HTQ) instead of Posttraumatic Stress Diagnostic Scale (PDS) might find different figures because while the HTQ determines PTSD diagnosis based on the first 16 items of the DSM-IV which measure just three of the criteria (psychological arousal, avoidance and numbing, and re-experiencing traumatic events), the PDS uses all criteria (A to F) (Foa et al., 1997; Mollica, 2004). On that score, when we grouped the prevalence rates by the two main types of measures employed to assess PTSD (HTQ vs. PDS), we observed that the PDS tended to yield higher prevalence than the HTQ. However, the prevalence rates based on the HTQ were highly unstable, ranging from 3 to 36%. Interestingly, when the prevalence rates were stratified by gender both the PDS and HTQ yielded nearly identical prevalence rates for males and females. Moreover, even in cases where the same instrument is used, changes made to the instruments over time make comparison cumbersome. For example, in the case of the HTQ, whereas the original version contained only sixteen traumatic events (Mollica et al., 1992), the revised version includes 40 different events (Mollica et al., 2004). Similarly, while there were only 30 trauma symptoms in the original version, there are now 40 symptoms in the revised version. These variations may lead to different results. An appropriate approach may be to compare results of studies using similar instruments; however, the dearth of studies in this population at this time precludes this option.
In addition to using different instruments, the use of different interpreters with varying levels of English proficiency and knowledge about mental health could potentially lead to different findings as the interpreters may not be conveying the same information during interviews. It is therefore imperative that the instruments are translated and cross culturally validated following proper protocols before use in communities whose primary language is not English. This should not be mere word for word translation but also based on careful qualitative inquiry to incorporate local understandings of mental health difficulty as expressed in that culture and context (Betancourt et al., 2009, 2012; Mollica, 2004).
It is also plausible that this wide variability in prevalence rates may be due in part to different experiences in different refugee camps (Johnson & Thompson, 2008). These could include factors such as the size of the refugee camp, how many people are housed there, its proximity to the border, level of security in the camp, nature of interaction with host community, refugee policies of the host government, whether hostile or cordial, availability of basic needs such as proper shelter, adequacy of food supplies, and local government policies toward the refugee population. If certain important factors are not considered in the study design and accounted for in the analysis, one may potentially introduce residual confounding.
To improve our knowledge about the underlying reasons for the wide variability in findings, particularly regarding prevalence of symptoms and traumatic events in the different studies, future studies should pay greater attention to important measures such as period of time under consideration, whether it is past month, past year, or lifetime. This must be made explicit to both participants and all research team members conducting interviews. In addition, greater attention should be paid to cultural norms and understanding about certain conditions and how they are defined or understood in the groups under study (Betancourt et al., 2009). Moreover, it is important to pay attention to some of the cultural aspects that contribute to disparities in risk and prevalence of trauma effects by gender. It is also important to have population-specific measures for assessment of traumatic events as war experiences will vary from setting to setting. For instance, in the HTQ, which was developed and validated using Indochinese population, some of the traumatic events such as people being “forced to find and bury bodies,” or being “forced to desecrate or destroy the bodies or graves of deceased persons,” did not necessarily occur in the South Sudanese context. On the other hand, some traumatic events such as cattle raiding, mass rape, and castrations, which are designed to inflict specific type of fear and pain on the population, are not captured by this instrument. It is evident that while there are certain universal aspects to conflicts that are captured by the most commonly used instruments, there are other population- or conflict-specific factors that could be missed by use of instruments designed or validated in other populations. Therefore, it is also important for a research team to learn as much about the target population as possible before embarking on a research project and to ensure strong local collaborations as well as mechanisms for community review and input (Betancourt et al., 2009; Ng et al., 2014; Scorza et al., 2013).
The risk factors found in the South Sudanese studies reviewed are similar to findings of previous studies of other war-affected populations (Ai et al., 2002; Eytan et al., 2004; Johnson & Thompson, 2008). For example, the strongest risk factor for development of PTSD included recent exposure to four or more trauma events post-conflict lifetime exposure to ≥ 8 traumatic events, low level of education, older age (≥ 35 years), and female gender. The finding that female gender is a strong risk factor finds particular resonance in the context of the conflict between northern Sudan and southern Sudan (North–South conflict), where gender-based violence was used as a deliberate military strategy, women experienced specific and painful trauma (Jok, 2015).
Similarly, that having never attended school was the strongest risk factor for depression and moderate socioeconomic disadvantage and rural residency were the strongest risk factors for anxiety among women and men respectively was not surprising. It is possible that because these findings were seen in post-conflict South Sudan, economic factors became more salient issues and having no education versus having education, even very little education, is determinative of one’s economic station, in a country where the majority are illiterate. That rural residency was the strongest predictor of anxiety for men made a great deal of sense because although relative peace had returned to most urban population centers, many rural areas still experience some degree of instability to this day.
In terms of protective factors, one of the studies among South Sudanese in northern Uganda and those in Southern Sudan by Karunakara et al. (2004) found that high level of education, having a salaried job, having household possessions, and, paradoxically, history of migration were protective factors against trauma-associated mental disorders. Roberts et al. (2009) identified urban residency as a factor protective against depression in a sample of South Sudanese in the capital city, Juba. Studies of South Sudanese in resettlement settings identified several important protective factors including religion, social support from family and South Sudanese community, higher annual household income, and governmental support (Schweitzer et al., 2006; Tutlam et al., 2020). An interesting finding by one of the studies conducted among resettled South Sudanese in the USA was that PTSD symptoms improved following dental restoration of teeth that had been removed when they were young, as part of cultural practices in South Sudan (Fox & Willis, 2010). This underscores the complex nature of how some situational and cultural factors may be influencing the mental health of South Sudanese refugees besides the well-known trauma triggering events resulting from war; therefore, cultural context is an important factor to consider in understanding mental disorders for those still in their homeland as well as those who have migrated to foreign settings.
Strengths and Limitations
This systematic review and meta-analysis is not without limitations. First, the paucity of studies on this highly traumatized population that the review is attempting to highlight means that fewer studies were available for systematic review and meta-analysis in the different settings. Having fewer studies may have contributed to the very high heterogeneity in the meta-analysis. Moreover, not all the studies assessed the three most common trauma-associated psychiatric disorders (anxiety, depression, and PTSD); therefore, we were unable to compute pooled prevalence rates of all the three conditions of interest in the different settings. Additionally, we were unable to conduct meta-analysis on the risk and protective factors for development of these trauma-associated disorders because there were no consistent set of risk and protective factors assessed across the studies included in the review. This study has some important strengths. To the best of our knowledge, it is the first study to synthesize the methodological approach and quality, trauma exposure, risk and protective factors, and aggregate prevalence of trauma-associated disorders in different settings in the South Sudanese population, which has been exposed to perpetual conflict. This systematic review and meta-analysis is an important contribution to the scientific literature given the dearth of studies assessing the impact of their prolonged exposure to conflict and the fact that many South Sudanese are still living in refugee camps, including some who have lived there for more than three decades, and many are scattered all over the world in search of refuge. The ability to compute prevalence rates for PTSD in different settings in particular is noteworthy.
Implication for Practice
These data suggest notable decline in symptoms from exposure to trauma among those in resettlement settings despite the population being exposed to a new set of stressors such as acculturation difficulties, discrimination, and isolation. Identifying important factors that may be responsible for this improvement of symptoms over time can inform design of interventions and policies that may be useful for others in similar situations. A related point is that this review has highlighted the paucity of studies in this population; therefore, more studies are needed to build a stronger evidence base to guide practice and policy development.
Conclusions
The prolonged exposure to war trauma has negatively impacted psychological wellbeing of South Sudanese, with particularly high prevalence of trauma-associated disorders among those still in refugee camps and in South Sudan. However, the prevalence of trauma-associated disorders appears to be relatively lower among those resettled in developed countries despite having experienced similar number and type of traumatic events as their peers still in preflight and flight settings. This warrants further investigation to delineate the factors that may be contributing to lower prevalence of trauma-associated disorders in this population to guide intervention development and policy recommendations for practice.
Funding
The review was part of the first author’s work as a postdoctoral trainee in the LEAD Global Training Program (T37).
Footnotes
Competing Interests The authors declare no competing interests.
Ethics Approval and Consent to Participate Not applicable.
Consent for Publication Not applicable.
Availability of Data and Materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
- Abu Suhaiban H, Grasser LR, & Javanbakht A (2019). Mental Health of Refugees and Torture Survivors: A Critical Review of Prevalence, Predictors, and Integrated Care. International Journal of Environmental Research and Public Health, 16(13). 10.3390/ijerph16132309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmad A, Sofi M, Sundelin-Wahlsten V, & Von Knorring A-L (2000). Posttraumatic stress disorder in children after the military operation “Anfal” in Iraqi Kurdistan. European Child & Adolescent Psychiatry, 9(4), 235–243. [DOI] [PubMed] [Google Scholar]
- Ai AL, Peterson C, & Ubelhor D (2002). War-related trauma and symptoms of posttraumatic stress disorder among adult Kosovar refugees. Journal of Traumatic Stress, 15(2), 157–160. [DOI] [PubMed] [Google Scholar]
- Atari DO, & McKague K (2015). South Sudan: Stakeholders’ views of technical and vocational education and training and a framework for action. Journal of Vocational Education & Training, 67(2), 169–186. [Google Scholar]
- Ayazi T, Lien L, Eide A, Swartz L, & Hauff E (2014). Association between exposure to traumatic events and anxiety disorders in a post-conflict setting: a cross-sectional community study in South Sudan. BMC Psychiatry, 14(6). Artn 6. 10.1186/1471-244x-14-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayazi T, Lien L, Eide AH, Ruom MM, & Hauff E (2012). What are the risk factors for the comorbidity of posttraumatic stress disorder and depression in a war-affected population? A cross-sectional community study in South Sudan. BMC Psychiatry, 12, 175. 10.1186/1471-244x-12-175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barak Y, & Szor H (2000). Lifelong posttraumatic stress disorder: Evidence from aging Holocaust survivors. Dialogues in Clinical Neuroscience, 2(1), 57–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbieri A, Visco-Comandini F, Alunni Fegatelli D, Schepisi C, Russo V, Calò F, Dessì A, Cannella G, & Stellacci A (2019). Complex trauma, PTSD and complex PTSD in African refugees. European Journal of Psychotraumatology, 10(1), 1700621. 10.1080/20008198.2019.1700621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashir UKM (2018). Challenges Facing Somali Women Refugees In Dadaab Refugee Camp, 1991–2016 University of Nairobi; ]. [Google Scholar]
- Betancourt TS, Bass J, Borisova I, Neugebauer R, Speelman L, Onyango G, & Bolton P (2009). Assessing local instrument reliability and validity: A field-based example from northern Uganda. Social Psychiatry and Psychiatric Epidemiology, 44(8), 685–692. 10.1007/s00127-008-0475-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt TS, Borisova I, Williams TP, Meyers-Ohki SE, Rubin-Smith JE, Annan J, & Kohrt BA (2013). Psychosocial adjustment and mental health in former child soldiers–systematic review of the literature and recommendations for future research. Journal of Child Psychology and Psychiatry, 54(1), 17–36. 10.1111/j.1469-7610.2012.02620.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt TS, & Khan KT (2008). The mental health of children affected by armed conflict: Protective processes and pathways to resilience. International Review of Psychiatry, 20(3), 317–328. 10.1080/09540260802090363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt TS, Newnham EA, Birman D, Lee R, Ellis BH, & Layne CM (2017). Comparing Trauma Exposure, Mental Health Needs, and Service Utilization Across Clinical Samples of Refugee, Immigrant, and U.S.-Origin Children. Journal of Traumatic Stress, 30(3), 209–218. 10.1002/jts.22186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt TS, Scorza P, Meyers-Ohki S, Mushashi C, Kayiteshonga Y, Binagwaho A, Stulac S, & Beardslee WR (2012). Validating the Center for Epidemiological Studies Depression Scale for Children in Rwanda. Journal of the American Academy of Child and Adolescent Psychiatry, 51(12), 1284–1292. 10.1016/j.jaac.2012.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt TS, Thomson DL, Brennan RT, Antonaccio CM, Gilman SE, & VanderWeele TJ (2020). Stigma and Acceptance of Sierra Leone’s Child Soldiers: A Prospective Longitudinal Study of Adult Mental Health and Social Functioning. Journal of the American Academy of Child and Adolescent Psychiatry, 59(6), 715–726. 10.1016/j.jaac.2019.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogic M, Njoku A, & Priebe S (2015). Long-term mental health of war-refugees: A systematic literature review. BMC International Health and Human Rights, 15, 29. 10.1186/s12914-015-0064-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calhoun LG, & Tedeschi RG (1999). Facilitating posttraumatic growth: A clinician’s guide. Routledge. [Google Scholar]
- Chkam H (2016). Aid and the perpetuation of refugee camps: The case of Dadaab in Kenya 1991–2011. Refugee Survey Quarterly, 35(2), 79–97. [Google Scholar]
- Collins RO (2008). A History of Modern Sudan. Cambridge University Press. [Google Scholar]
- Do TTH, Correa-Velez I, & Dunne MP (2019). Trauma exposure and mental health problems among adults in Central Vietnam: a randomized cross-sectional survey. Frontiers in Psychiatry, 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis BH, MacDonald HZ, Lincoln AK, & Cabral HJ (2008). Mental health of Somali adolescent refugees: The role of trauma, stress, and perceived discrimination. Journal of Consulting and Clinical Psychology, 76(2), 184. [DOI] [PubMed] [Google Scholar]
- Eytan A, Gex-Fabry M, Toscani L, Deroo L, Loutan L, & Bovier PA (2004). Determinants of postconflict symptoms in Albanian Kosovars. The Journal of Nervous and Mental Disease, 192(10), 664–671. [DOI] [PubMed] [Google Scholar]
- Foa EB, Cashman L, Jaycox L, & Perry K (1997). The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychological Assessment, 9(4), 445. [Google Scholar]
- Fox S, & Willis M (2009). Initiatory Mental Health Assessments for Dinka and Nuer Refugees from Sudan. Journal of Immigrant and Refugee Studies, 7(2), 159–179. 10.1080/15562940902935621 [DOI] [Google Scholar]
- Fox S, & Willis M (2010). Dental restorations for dinka and nuer refugees: A confluence of culture and healing. Transcultural Psychiatry, 47(3), 452–472. 10.1177/1363461510374559 [DOI] [PubMed] [Google Scholar]
- Geltman PL, Grant-Knight W, Mehta SD, Lloyd-Travaglini C, Lustig S, Landgraf JM, & Wise PH (2005). The “lost boys of Sudan”: Functional and behavioral health of unaccompanied refugee minors resettled in the United States. Archives of Pediatrics & Adolescent Medicine, 159(6), 585–591. [DOI] [PubMed] [Google Scholar]
- Jaranson JM, Butcher J, Halcon L, Johnson DR, Robertson C, Savik K, Spring M, & Westermeyer J (2004). Somali and Oromo refugees: Correlates of torture and trauma history. American Journal of Public Health, 94(4), 591–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson H, & Thompson A (2008). The development and maintenance of post-traumatic stress disorder (PTSD) in civilian adult survivors of war trauma and torture: A review. Clinical Psychology Review, 28(1), 36–47. [DOI] [PubMed] [Google Scholar]
- Jok JM (2015). Sudan: Race, religion, and violence. Oneworld Publications. [Google Scholar]
- Kanter ED (2008). The impact of war on mental health. In Levy BS & Sidel VW (Eds.), War and Public Health (pp. 51–68). Oxford University Press. [Google Scholar]
- Karunakara UK, Neuner F, Schauer M, Singh K, Hill K, Elbert T, & Burnha G (2004). Traumatic events and symptoms of post-traumatic stress disorder amongst Sudanese nationals, refugees and Ugandans in the West Nile. African Health Sciences, 4(2), 83–93. [PMC free article] [PubMed] [Google Scholar]
- Kienzler H (2008). Debating war-trauma and post-traumatic stress disorder (PTSD) in an interdisciplinary arena. Social Science and Medicine, 67(2), 218–227. 10.1016/j.socscimed.2008.03.030 [DOI] [PubMed] [Google Scholar]
- Kirmayer LJ, & Bhugra D (2009). Culture and mental illness: social context and explanatory models. Psychiatric diagnosis: patterns and prospects. New York (NY): John Wiley & Sons, Ltd, 29–37. [Google Scholar]
- Kolassa IT, Kolassa S, Ertl V, Papassotiropoulos A, & De Quervain DJ (2010). The risk of posttraumatic stress disorder after trauma depends on traumatic load and the catechol-o-methyltransferase Val(158)Met polymorphism. Biological Psychiatry, 67(4), 304–308. 10.1016/j.biopsych.2009.10.009 [DOI] [PubMed] [Google Scholar]
- Lambert JE, & Alhassoon OM (2015). Trauma-focused therapy for refugees: Meta-analytic findings. Journal of Counseling Psychology, 62(1), 28–37. 10.1037/cou0000048 [DOI] [PubMed] [Google Scholar]
- Lamkaddem M, Stronks K, Deville WD, Olff M, Gerritsen AA, & Essink-Bot ML (2014). Course of post-traumatic stress disorder and health care utilisation among resettled refugees in the Netherlands. BioMed Central Psychiatry, 14, 90. 10.1186/1471-244x-14-90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindert J, von Ehrenstein OS, Wehrwein A, Brähler E, & Schäfer I (2018). Anxiety, Depression and Posttraumatic Stress Disorder in Refugees - A Systematic Review. Psychotherapie, Psychosomatik, Medizinische Psychologie, 68(1), 22–29. 10.1055/s-0043-103344. (Angst, Depressionen und posttraumatische Belastungsstörungen bei Flüchtlingen – eine Bestandsaufnahme.) [DOI] [PubMed] [Google Scholar]
- Lustig SL, Kia-Keating M, Knight WG, Geltman P, Ellis H, Kinzie JD, Keane T, & Saxe GN (2004). Review of child and adolescent refugee mental health. Journal of the American Academy of Child and Adolescent Psychiatry, 43(1), 24–36. 10.1097/00004583-200401000-00012 [DOI] [PubMed] [Google Scholar]
- Marshall GN, Schell TL, Elliott MN, Berthold SM, & Chun CA (2005). Mental health of Cambodian refugees 2 decades after resettlement in the United States. Journal of the American Medical Association, 294(5), 571–579. 10.1001/jama.294.5.571 [DOI] [PubMed] [Google Scholar]
- MedCalc. (2018). MedCalc statistical software (Version 18.6) [Computer software].
- Mollica RF (2004). Measuring trauma, measuring torture: Instructions and guidance on the utilization of the Harvard Program in Refugee Trauma’s versions of The Hopkins Symptom Checklist-25 (HSCL-25) & The Harvard Trauma Questionnaire (HTQ). Harvard Program in Refugee Trauma. [Google Scholar]
- Mollica RF, Caspi-Yavin Y, Bollini P, Truong T, Tor S, & Lavelle J (1992). The Harvard Trauma Questionnaire: Validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in Indochinese refugees. The Journal of Nervous and Mental Disease, 180(2), 111–116. [PubMed] [Google Scholar]
- Mollica RF, McDonald L, Massagli M, & Silove DM (2004). Measuring trauma, measuring torture: Instructions and guidance on the utilization of the Harvard Program in Refugee Trauma’s versions of The Hopkins Symptom Checklist-25 (HSCL-25) & The Harvard Trauma Questionnaire (HTQ). Harvard University. [Google Scholar]
- Mollica RF, Wyshak G, de Marneffe D, Khuon F, & Lavelle J (1987). Indochinese versions of the Hopkins Symptom Checklist-25: A screening instrument for the psychiatric care of refugees. American Journal of Psychiatry, 144(4), 497–500. [DOI] [PubMed] [Google Scholar]
- Morina N, Akhtar A, Barth J, & Schnyder U (2018). Psychiatric Disorders in Refugees and Internally Displaced Persons After Forced Displacement: A Systematic Review. Front Psychiatry, 9, 433. 10.3389/fpsyt.2018.0433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murthy RS, & Lakshminarayana R (2006). Mental health consequences of war: A brief review of research findings. World Psychiatry, 5(1), 25–30. [PMC free article] [PubMed] [Google Scholar]
- Nesterko Y, Jäckle D, Friedrich M, Holzapfel L, & Glaesmer H (2019). Prevalence of post-traumatic stress disorder, depression and somatisation in recently arrived refugees in Germany: An epidemiological study. Epidemiol Psychiatr Sci, 29, e40. 10.1017/s2045796019000325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuner F, Schauer M, Karunakara U, Klaschik C, Robert C, & Elbert T (2004). Psychological trauma and evidence for enhanced vulnerability for posttraumatic stress disorder through previous trauma among West Nile refugees. BioMed Central Psychiatry, 4, 34. 10.1186/1471-244X-4-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng LC, Kanyanganzi F, Munyanah M, Mushashi C, & Betancourt TS (2014). Developing and validating the Youth Conduct Problems Scale-Rwanda: A mixed methods approach. PLoS ONE, 9(6), e100549. 10.1371/journal.pone.0100549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng LC, Lopez B, Pritchard M, & Deng D (2017). Posttraumatic stress disorder, trauma, and reconciliation in South Sudan. Social Psychiatry and Psychiatric Epidemiology, 52(6), 705–714. 10.1007/s00127-017-1376-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onyut LP, Neuner F, Ertl V, Schauer E, Odenwald M, & Elbert T (2009). Trauma, poverty and mental health among Somali and Rwandese refugees living in an African refugee settlement - an epidemiological study. Conflict and Health, 3, 6. 10.1186/1752-1505-3-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, & Brennan SE (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. International Journal of Surgery, 88, 105906. [DOI] [PubMed] [Google Scholar]
- Palik J, Rustad SA, & Methi F (2020). Conflict Trends in Africa, 1989–2019. PRIO Paper, 1946–2019. [Google Scholar]
- Peltzer K (1999). Trauma and mental health problems of Sudanese refugees in Uganda. Central African Journal of Medicine, 45(5), 110–114. [DOI] [PubMed] [Google Scholar]
- Pfeiffer A, & Elbert T (2011). PTSD, depression and anxiety among former abductees in Northern Uganda. Confl Health, 5(1), 14. 10.1186/1752-1505-5-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts B, Damundu EY, Lomoro O, & Sondorp E (2009). Post-conflict mental health needs: A cross-sectional survey of trauma, depression and associated factors in Juba. Southern Sudan. Biomed Central Psychiatry, 9, 7. 10.1186/1471-244X-9-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross LE, Grigoriadis S, Mamisashvili L, Koren G, Steiner M, Dennis CL, Cheung A, & Mousmanis P (2011). Quality assessment of observational studies in psychiatry: An example from perinatal psychiatric research. International Journal of Methods in Psychiatric Research, 20(4), 224–234. 10.1002/mpr.356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholte WF, Olff M, Ventevogel P, de Vries G-J, Jansveld E, Cardozo BL, & Crawford CAG (2004). Mental health symptoms following war and repression in eastern Afghanistan. JAMA, 292(5), 585–593. [DOI] [PubMed] [Google Scholar]
- Schweitzer R, Melville F, Steel Z, & Lacherez P (2006). Trauma, post-migration living difficulties, and social support as predictors of psychological adjustment in resettled Sudanese refugees. Australian and New Zealand Journal of Psychiatry, 40(2), 179–187. 10.1080/j.1440-1614.2006.01766.x [DOI] [PubMed] [Google Scholar]
- Scorza P, Stevenson A, Canino G, Mushashi C, Kanyanganzi F, Munyanah M, & Betancourt T (2013). Validation of the “World Health Organization Disability Assessment Schedule for children, WHODAS-Child” in Rwanda. PLoS ONE, 8(3), e57725. 10.1371/journal.pone.0057725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, & Dunbar GC (1998). The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59, 22–33. [PubMed] [Google Scholar]
- Silove D (2013). The ADAPT model: A conceptual framework for mental health and psychosocial programming in post conflict settings. Intervention, 11(3), 237–248. [Google Scholar]
- Slewa-Younan S, Uribe Guajardo MG, Heriseanu A, & Hasan T (2015). A Systematic Review of Post-traumatic Stress Disorder and Depression Amongst Iraqi Refugees Located in Western Countries. Journal of Immigrant and Minority Health, 17(4), 1231–1239. 10.1007/s10903-014-0046-3 [DOI] [PubMed] [Google Scholar]
- Steel Z, Chey T, Silove D, Marnane C, Bryant RA, & van Ommeren M (2009). Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: A systematic review and meta-analysis. JAMA, 302(5), 537–549. 10.1001/jama.2009.1132 [DOI] [PubMed] [Google Scholar]
- Steel Z, Silove D, Phan T, & Bauman A (2002). Long-term effect of psychological trauma on the mental health of Vietnamese refugees resettled in Australia: A population-based study. The Lancet, 360(9339), 1056–1062. 10.1016/s0140-6736(02)11142-1 [DOI] [PubMed] [Google Scholar]
- Sullivan DP (2018). Didplaced Nation: The Dangerous Implications of Rushed Returns in South Sudan. R. International. https://static1.squaespace.com/static/506c8ea1e4b01d9450dd53f5/t/5c016929575d1ff2db20dd62/1543596335696/South+Sudan+Report+-+November+2018+-+1137+11.30.pdf [Google Scholar]
- Summerfield D (1999). A critique of seven assumptions behind psychological trauma programmes in war-affected areas. Social Science & Medicine, 48(10), 1449–1462. [DOI] [PubMed] [Google Scholar]
- Tedeschi RG, & Calhoun LG (1996). The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress, 9(3), 455–471. [DOI] [PubMed] [Google Scholar]
- Tol WA, Barbui C, Galappatti A, Silove D, Betancourt TS, Souza R, Golaz A, & van Ommeren M (2011). Mental health and psychosocial support in humanitarian settings: Linking practice and research. Lancet, 378(9802), 1581–1591. 10.1016/s0140-6736(11)61094-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran TV, Manalo V, & Nguyen VT (2007). Nonlinear relationship between length of residence and depression in a community-based sample of Vietnamese Americans. International Journal of Social Psychiatry, 53(1), 85–94. [DOI] [PubMed] [Google Scholar]
- Tutlam NT (2013). Liberating South Sudan One Patient at a Time: The Life of Dr. Xlibris Corporation. [Google Scholar]
- Tutlam NT, Flick LH, Xian H, Matsuo H, Glowinski A, & Tutdeal N (2020). Trauma-Associated Psychiatric Disorders Among South Sudanese Dinka and Nuer Women Resettled in the USA. Global Social Welfare. 10.1007/s40609-020-00171-7 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.


