Abstract
Introduction Traumatic cervical spine injuries (CSIs) have an incidence of 1.7 to 8% among traumatic brain injury (TBI) patients and should be a pivotal part of its neurological examination. Prognosis of cervical spine insult in TBI depends on several epidemiological and clinical factors which need to be considered during the management of these injuries. This study aims to analyze the outcomes of patients with CSI and its associated predictors.
Materials and Methods A prospective observational study was conducted among 63 patients of traumatic CSI admitted at a tertiary care center of Lucknow, Uttar Pradesh, India. All patients underwent a clinical assessment using the American Spinal Injury Association, Functional Independence Measure (FIM), and Barthel Index scoring and grading at admission, 1, and 4 months, respectively. All patients at the facility underwent magnetic resonance imaging (MRI). Midsagittal T1- and T2-weighted sequences were used to measure the degree of spinal cord injury (SCI) impairment. Patients were followed for outcome assessment.
Results There was a significant difference in the median values of Barthel Index and mean values of FIM preoperatively and at 4 months' follow-up. There was a significant improvement in the neurological outcome of the patients after admission, at 1, and 4 months' follow-up. Out of the 30 patients who had improvement in the neurological outcome, majority (26) had edema present in less than equal to 2 segments and this was statistically significant. The overall FIM score was significantly higher among those with ≤ 2 segment edema as compared with those with > 2 segments.
Conclusion The study concludes that incomplete injury, edema on MRI imaging less than equal to 2 segments, and no listhesis are predictors of neurological and functional improvement in patients with traumatic cervical spinal injuries.
Keywords: anterior cervical corpectomy and fusion, American Spinal Injury Association, spinal cord injury, magnetic resonance imaging, anterior cervical discectomy and fusion, Functional Independence Measure, cervical spinal cord injury, computed tomography, factor influencing, recovery
Introduction
Traumatic cervical spine injuries (CSIs) result from falls, road traffic accidents, penetrating injuries or blunt trauma, and injuries related to sports and diving. 1 Globally, they contribute to almost half of all the spinal injuries and are emerging as a major cause of long-term disability because of the neurological impairment due to the magnitude of cervical spine insult and delay in its identification. 2 Patients with traumatic brain injury have a documented incidence of CSI that varies from 1.7 to 8% and hence should be a pivotal part of neurological examination in traumatic injuries. 3
Early identification and prompt treatment play a crucial role in the outcome of traumatic CSIs. These injuries require both surgical as well as conservative management. Conservative management mainly involves the use of a cervical collar or halo for neck stabilization. Surgical management is needed in cases of surgical decompression. 4 5 With the advent of advance emergency medical care, there has been a paradigm shift in the management of these injuries, moving away from conservative methods toward cord decompression, spine stabilization, early mobilization, and rehabilitation. 6 This results in early recovery of these patients with better functional and neurological outcome.
However, prognosis depends on several epidemiological and clinical factors which need to be considered during the management of these injuries. Factors like age, gender, mode or level of injury, extent of edema, etc. are crucial determinants of the outcome. 7 However, not much has been explored in this domain as the prevalence of isolated traumatic CSIs seem to be low when compared with other spinal injuries. But they can consequently cause adverse repercussions among the patients if robust action is not taken. Hence, this study aims to analyze the outcomes of patients with CSI and its associated predictors.
Materials and Methods
Study Design and Setting
This study was a prospective observational study that included all patients with cervical spinal injuries who presented at the emergency department within 1 week of the injury and underwent surgical management at the Department of Neurosurgery, King George's Medical University in Lucknow, Uttar Pradesh, India. The study received approval from the Institutional Ethics Committee [Number 128/Ethics/2020].
Study Participants
Patients who came within a week of their cervical spinal injuries spanning from C1 to C7 were included in this study. Exclusion criteria for the research included patients with significant autonomic disorders, such as systolic blood pressure less than 40, had correlated thoracolumbar and brain injuries, penetrating injuries, underwent conservative management, and arrival to the institution after 7 days following the injury.
Sample Size
For the purpose of sample size estimation, the study used was Srinivas et al. 8
Sample size formula used was n = ([ Z α /2 ] 2 * p (1– p ))/ d 2 , where Z α /2 is the critical value of the normal distribution at α/2 (for a confidence level of 95%, α = 0.05, and the critical value of 1.96), p is the proportion of patients with traumatic CSI and of American Spinal Injury Association (ASIA) grade D with significant neurological improvement (value 83.3%), and d is the margin of error for desired precision (10%). At 95% confidence interval, the required minimum sample size was 54 patients. Taking 10% loss to follow-up, the total sample size calculated was 59 patients. So a total of 63 patients were enrolled in the study.
Data Collection
After obtaining written informed consent from the patient or their guardian, all patients underwent a clinical assessment using the ASIA scoring and grading system. In addition to clinical characteristics, the study also considered demographic variables including age, gender, injury type, and chronology. All patients at the facility underwent magnetic resonance imaging (MRI). Midsagittal T1- and T2-weighted sequences were used to measure the degree of spinal cord injury (SCI) impairment. Based on the length of time of the traumatic incident and the MRI, the MRI results were divided into two groups: (1) contusion and (2) edema. The vertebral bodies and discs were used to segregate the midsagittal area of the MRI to objectively estimate the length of the lesion (edema/contusion). The SCI apart from routine axial, coronal, and sagittal T1 and T2 imaging, some special sequences are required depending on the clinical need like in T2-weighted image (T2WI) (gradient echo, susceptibility weighted imaging sequence are more sensitive for hemorrhage, while short tau inversion recovery are more sensitive to ligamentous injury).
In spinal cord swelling, sagittal T1WI focal cord enlargement is seen without signal changes, in spinal cord edema, changes like cord swelling with high T2 signal intensity is seen, and in spinal cord contusion, thick hyperintense T2 signal rim is seen around small central hypointense T1 signal with blooming on T2WI. 9
The adjacent disc was regarded as a third segment in addition to the upper and lower vertebral body segments. This led to the classification of edema as (1) 2 segments and (2) > 2 segments. The National Spinal Cord Injury Study II advised injecting methylprednisolone into patients who came within 8 hours of the injury ( n = 2). Based on the date of the operation after the accident, the patients were arbitrarily split into two groups: early (1 week) and late (> 1 week). A team of neurosurgeons from the department established the preoperative plan during the preoperative phase.
Surgery indicates if there was instability, dislocation, canal stenosis, and spinal cord compression. Anterior cervical discectomy/corpectomy has been the most used surgical procedure, which was described by Cloward and Robinson and Smith in 1958. This procedure is done under general anesthesia technique and the patient is positioned in a supine position. A longitudinal or vertical surgical incision was made medial to the sternocleidomastoid muscle at the targeted level of decompression, followed by superficial dissections through the fascia and platysma muscle, retraction of the tracheoesophageal complex medially and the sternocleidomastoid with the carotid sheath laterally. A deep dissection by splinting the longus colli muscles and anterior longitudinal ligament to expose the vertebral body was done. This was followed by decompression of the targeted level by removal of the affected disc level, fractured bone, and osteophytes. The bone graft was then applied followed by plate and screws. 10
An impartial supervising senior specialist recognized that surgical decompression was performed until the dura became visible, without any intervening disc or posterior longitudinal ligament. In the outpatient department, each of these patients received routine follow-up care. A change of one or more grades in the ASIA grade between the admission date and the 4-month follow-up was considered an improvement. The Functional Independence Measure (FIM) scale was used to evaluate functional grade at both the 4-month follow-up and admission.
Statistical Analysis
The data was evaluated using SPSS 24.0. The study data were presented in a descriptive summary including frequencies, percentages, graphs, means, and standard deviation. To assess statistical significance at the 5% level of significance, probability ( p ) was determined. The Kolmogorov–Smirnov test was used to determine the data's normality. The chi-square test was used to analyze categorical data. Continuous variables were calculated using the independent t -test. Paired t -test was used to compare FIM and Barthel Index at various follow-ups. ASIA grades were observed at various follow-ups using the Friedman test.
Results
Majority (26.9%) of the study participants were in the age group of 31 to 40 years. Maximum were males (88.9%). The most common mode of CSI was due to fall from height (46.03%). Most (25.4%) of the study participants presented to the hospital between 6 and 24 hours postinjury. More than half of the participants had incomplete injury. Note that 71.4% underwent operative management. Note that 22.2% had grade 1 listhesis, followed by 12.7, 19.0, 9.5, and 1.6% with grade 2, 3, 4, and 5 listhesis, respectively. Approximately 50.8% patients had edema in the MRI findings. The extent of edema was ≤ 2 segments in maximum (68.3%) patients. Only 6.3 and 17.5% patients had locked and parched facet, respectively ( Table 1 ).
Table 1. Baseline parameters of the study participants.
| Parameters | N = 63 | % | |
|---|---|---|---|
| Age (y) | Up to 20 | 3 | 4.76 |
| 21–30 | 22 | 34.9 | |
| 31–40 | 17 | 26.9 | |
| 41–50 | 15 | 23.8 | |
| 51–60 | 6 | 9.64 | |
| Gender | Male | 56 | 88.9 |
| Female | 7 | 11.1 | |
| Mode of injury | Fall from height | 29 | 46.03 |
| Road traffic accident (RTA) | 24 | 38.1 | |
| Hit by animal | 2 | 3.17 | |
| Assault | 3 | 4.76 | |
| Other | 5 | 7.94 | |
| Injury to hospital presentation time | Within 6 h | 4 | 6.34 |
| 6–24 h | 16 | 25.4 | |
| 24–48 h | 10 | 15.9 | |
| 48–72 h | 11 | 17.5 | |
| 72 h—1 wk | 7 | 14.3 | |
| > 1 wk | 13 | 20.6 | |
| Cervical immobilization used during transportation | Yes | 40 | 61.9 |
| No | 23 | 38.1 | |
| Type of injury | Complete | 28 | 44.4 |
| Incomplete | 34 | 54.0 | |
| Normal | 1 | 1.6 | |
| Level of injury | Upper (C2–C4) | 11 | 81 |
| Lower (C5–C7) | 51 | 19 | |
| Management | Operative | 45 | 71.4 |
| Conservative | 18 | 28.6 | |
| Listhesis | No listhesis | 22 | 34.9 |
| Grade 1 | 14 | 22.2 | |
| Grade 2 | 8 | 12.7 | |
| Grade 3 | 12 | 19.0 | |
| Grade 4 | 6 | 9.5 | |
| Grade 5 | 1 | 1.6 | |
| MRI finding | Normal | 7 | 11.1 |
| Edema | 32 | 50.8 | |
| Contusion | 24 | 38.1 | |
| Extent of edema | ≤ 2 segments | 43 | 68.3 |
| > 2 segments | 20 | 31.7 | |
| Locked facet/joint | Yes | 4 | 6.3 |
| No | 59 | 93.7 | |
| Parched facet/joint | Yes | 11 | 17.5 |
| No | 52 | 82.5 | |
Abbreviation: MRI, magnetic resonance imaging.
There was a significant difference in the median values of preoperative Barthel Index and at 4 months' follow-up ( Table 2 ).
Table 2. Functional outcome of the study participants.
| Functional outcome | Median (IQR) | 25th percentile | 75th percentile | p -Value a |
|---|---|---|---|---|
| Barthel Index preoperative | 5.0 (8) | 0 | 8 | 0.0001 |
| Barthel Index at 4 months' follow-up | 6.0 (10) | 0 | 10 |
Note: p -Value <0.05 are significant.
Abbreviation: IQR, interquartile range.
Wilcoxon sign rank test.
There was a significant difference in the mean values of FIM score preoperatively and 4 months' follow-up ( Table 3 ).
Table 3. Comparison of preoperative FIM and at 4 months' follow-up.
| FIM | Mean ± SD | 95% confidence interval | p -Value a | |
|---|---|---|---|---|
| Lower | Upper | |||
| Preoperative | 41.76 ± 27.16 | –18.58 | –6.98 | 0.0001 |
| 4 months' follow-up | 54.54 ± 41.90 | |||
Note: p -Value <0.05 are significant.
Abbreviations: FIM, Functional Independence Measure; SD, standard deviation.
Paired t -test.
There was a significant improvement in the neurological outcome of the patients after admission, at 1, and 4 months' follow-up. At admission, 28 patients were in grade A but at 4 months, only 14 patients were in grade A. Out of the 15, 11, and 8 patients in grade B, C, and D, only 2, 3, and 15 patients were in the same grades, respectively, at 4 months ( Table 4 ).
Table 4. Neurological outcome of the study participants.
| ASIA grade | A | B | C | D | E |
|---|---|---|---|---|---|
| At admission ( N = 63) | 28 (44.4) | 15 (23.8) | 11 (17.5) | 8 (12.7) | 1 (1.6) |
| 1 months' follow-up ( n = 50) a | 14 (28) | 12 (24) | 13 (26) | 10 (20) | 1 (2) |
| 4 months' follow-up ( n = 47) b | 12 (25.5) | 2 (4.3) | 3 (6.4) | 15 (31.9) | 8 (17.02) |
Abbreviations: ASIA, American Spinal Injury Association; LAMA, leave against medical advice.
Expired (11) and LAMA (2).
Expired (14) and LAMA (2).
At 4 months, 49.8% patients had neurological improvement, 27.9% had no improvement, and 22.3% had expired ( Fig. 1 ).
Fig. 1.
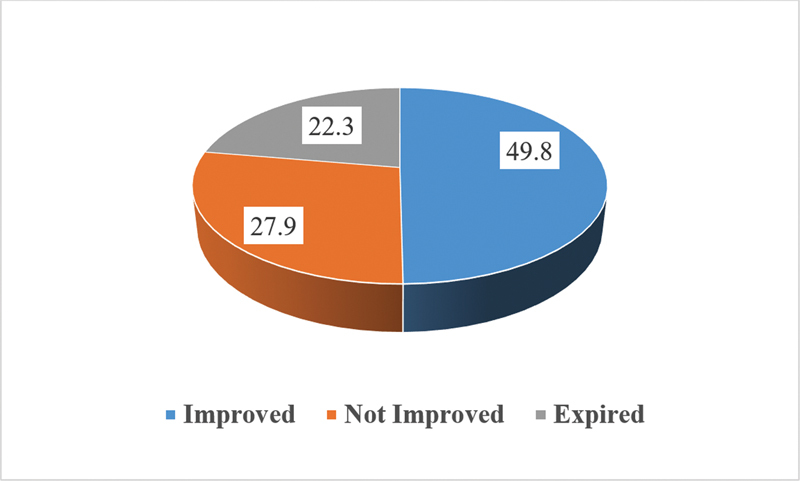
Neurological outcome at 4 months (American Spinal Injury Association [ASIA] grade).
Among the 30 patients who showed neurological improvement, 28 had incomplete injury, 26 had edema, 29 patients had extent of edema in less than equal to 2 segments, and 16 had no listhesis and all these were significantly associated with the neurological improvement ( Table 5 ).
Table 5. Predictors of neurological outcome among the study participants.
| ASIA grade at 4 months | |||||
|---|---|---|---|---|---|
| Parameters | Improved n = 30 (%) |
Not improved n = 17 (%) |
Expired n = 14 (%) |
p -Value | |
| Age (y) | 1–20 | 1 (3.3) | 1 (5.9) | 1 (7.1) | 0.393 |
| 21–30 | 9 (30) | 10 (58.8) | 2 (9.1) | ||
| 31–40 | 10 (33.3) | 2 (11.8) | 5 (35.7) | ||
| 41–50 | 6 (20) | 3 (17.6) | 4 (28.6) | ||
| 51–60 | 4 (13.3) | 1 (5.9) | 2 (14.3) | ||
| Sex | Male | 27 (90) | 16 (94.1) | 11 (78.6) | 0.377 a |
| Female | 3 (10) | 1 (5.9) | 3 (21.4) | ||
| Mode of injury | Fall from height | 11 (36.7) | 9 (52.9) | 9 (64.3) | 0.238 |
| Road traffic injury | 13 (43.3) | 7 (41.2) | 4 (28.6) | ||
| Hit by animal | 0 (0) | 1 (5.9) | 1 (7.1) | ||
| Assault | 2 (6.7) | 0 (0.0) | 0 (0) | ||
| Others | 4 (13.3) | 0 (0.0) | 0 (0) | ||
| Injury to hospital presentation time | Within 6 h | 2 (6.7) | 1 (5.9) | 1 (7.1) | 0.455 |
| 6–24 h | 19 (36.7) | 2 (11.8) | 3 (21.4) | ||
| 24–48 h | 2 (6.7) | 5 (29.4) | 4 (28.6) | ||
| 48–72 h | 6 (20) | 2 (11.8) | 3 (21.4) | ||
| > 72 h | 3 (10) | 4 (23.5) | 2 (14.3) | ||
| > 1 wk | 6 (20) | 3 (17.6) | 1 (7.1) | ||
| Mobilization | Yes | 19 (63.3) | 10 (58.8) | 11 (78.6) | 0.483 a |
| No | 11 (36.7) | 7 (41.2) | 3 (21.4) | ||
| Type of injury | Complete | 1 (3.3) | 12 (70.6) | 13 (92.9) | 0.0001 |
| Incomplete | 28 (93.3) | 5 (29.4) | 1 (7.1) | ||
| Normal | 1 (3.3) | 0 (0) | 0 (0) | ||
| Level of injury | Upper | 11 (36.7) | 16 (94.1) | 4 (28.6) | 0.026 a |
| Lower | 19 (63.3) | 1 (5.9) | 10 (71.4) | ||
| Management | Conservative | 17 (56.7) | 3 (17.6) | 10 (71.4) | 0.388 a |
| Operative | 13 (43.3) | 14 (82.4) | 4 (28.6) | ||
| MRI finding | None | 4 (13.3%) | 3 (17.6) | 0 (0.0%) | 0.0001 |
| Edema | 26 (86.7%) | 6 (35.3) | 0 (0.0%) | ||
| Contusion | 0 (0.0%) | 8 (47.1) | 14 (100.0) | ||
| Extent of edema | ≤ 2 segments | 29 (96.7%) | 9 (52.9) | 4 (28.6) | 0.0001 a |
| > 2 segments | 1 (3.3%) | 8 (47.1) | 10 (71.4) | ||
| Listhesis | No listhesis | 16 (53.3) | 4 (23.5) | 2 (14.3) | 0.0001 |
| Grade 1 | 10 (33.3) | 3 (17.6) | 1 (7.1) | ||
| Grade 2 | 3 (10) | 4 (23.5) | 0 (0) | ||
| Grade 3 | 1 (3.3) | 4 (23.5) | 6 (42.9) | ||
| Grade 4 | 0 (0) | 2 (11.8) | 4 (28.6) | ||
| Grade 5 | 0 (0) | 0 (0) | 1 (7.1) | ||
| Locked facet/joint | Yes | 3 (10) | 1 (5.9) | 0 | 0.802 |
| No | 27 (90) | 16 (94.1) | 14 (100) | ||
| Parched facet/joint | Yes | 2 (6.7) | 6 (35.3) | 2 (14.3) | 0.033 a |
| No | 28 (93.3) | 11 (64.7) | 12 (85.7) | ||
Abbreviation: MRI, magnetic resonance imaging.
Note: p < 0.05 is significant (bold).
Chi-square test, rest is Fischer's exact test.
The mean FIM score of patients with incomplete injury was significantly higher than those with complete injury. Those with lower level of injury had higher FIM score than the upper level of injury and this was statistically significant. Those with conservative management had higher FIM scores as compared with those with operative management, and this was significant. Those with edema had significantly higher FIM scores as compared with those with contusion. Those with extent of edema up to less than equal to 2 segments had higher FIM scores than those with ≥ 2 segments, and this was highly significant ( Table 6 ).
Table 6. Predictors of functional outcome among the study participants.
| FIM score at 4 months | |||||
|---|---|---|---|---|---|
| Parameters | Mean ± SD | 95% CI | p -Value | ||
| Lower | Upper | ||||
| Age (y) | 1–20 | 42.33 ± 51.033 | –84.44 | 169.11 | 0.665 a |
| 21–30 | 53.50 ± 37.011 | 37.09 | 69.91 | ||
| 31–40 | 54.71 ± 42.880 | 32.66 | 76.75 | ||
| 41–50 | 47.86 ± 43.661 | 22.65 | 73.07 | ||
| 51–60 | 76.00 ± 52.170 | 27.75 | 124.25 | ||
| Sex | Male | 56.45 ± 41.640 | 45.30 | 67.60 | 0.311 |
| Female | 39.29 ± 44.022 | –1.43 | 80.00 | ||
| Mode of injury | Fall from height | 43.90 ± 40.381 | 28.82 | 58.98 | 0.075 a |
| Road traffic injury | 63.38 ± 42.033 | 45.63 | 81.12 | ||
| Hit by animal | 11.00 ± 15.556 | –128.77 | 150.77 | ||
| Assault | 76.67 ± 50.964 | –49.94 | 203.27 | ||
| Others | 86.50 ± 16.823 | 59.73 | 113.27 | ||
| Injury to hospital presentation time | Within 6 h | 45.40 ± 52.046 | –19.22 | 110.02 | 0.237 a |
| 6–24 h | 70.25 ± 41.282 | 48.25 | 92.25 | ||
| 24–48 h | 31.36 ± 32.500 | 9.53 | 53.20 | ||
| 48–72 h | 52.18 ± 42.249 | 23.80 | 80.56 | ||
| > 72 h | 49.33 ± 42.790 | 16.44 | 82.22 | ||
| > 1 wk | 65.64 ± 41.752 | 37.59 | 93.69 | ||
| Mobilization | Yes | 53.35 ± 42.113 | 39.88 | 66.82 | 0.769 |
| No | 56.61 ± 42.375 | 38.28 | 74.93 | ||
| Type of Injury | Complete | 42.73 ± 38.983 | 31.02 | 54.45 | 0.0001 |
| Incomplete | 84.06 ± 34.304 | 67.00 | 101.11 | ||
| Level of Injury | Upper | 42.73 ± 38.983 | 31.02 | 54.45 | 0.0001 |
| Lower | 84.06 ± 34.304 | 67.00 | 101.11 | ||
| Management | Operative | 47.67 ± 38.888 | 35.98 | 59.35 | 0.038 |
| Conservative | 71.72 ± 45.274 | 49.21 | 94.24 | ||
| MRI findings | None | 88.71 ± 21.132 | 69.17 | 108.26 | 0.0001 a |
| Edema | 80.88 ± 27.392 | 71.00 | 90.75 | ||
| Contusion | 9.46 ± 12.755 | 4.07 | 14.84 | ||
| Extent of edema | ≤ 2 segments | 70.63 ± 38.033 | 58.92 | 82.33 | 0.0001 |
| > 2 segments | 19.95 ± 26.172 | 7.70 | 32.20 | ||
| Listhesis | Listhesis | 46.66 ± 40.429 | 33.90 | 59.42 | 0.125 a |
| Fracture | 69.36 ± 41.094 | 45.63 | 93.08 | ||
| Listhesis/fracture | 69.36 ± 41.094 | 45.63 | 93.08 | ||
Abbreviations: CI, confidence interval; FIM, Functional Independence Measure; MRI, magnetic resonance imaging; SD, standard deviation.
Note: p -value < 0.05 is significant (bold).
One-way analysis of variance test, rest all is independent t -test.
The overall FIM score and mean scores of self-care, sphincter control, locomotion, communication, and cognitive was higher among those with ≤ 2 segment edema as compared with those with > 2 segments. There was a highly significant association between overall FIM scores and all its components with the extent of edema ( Table 7 ).
Table 7. Association of Functional Independence Measure scores at 4 months with number of segments of injury.
| Functional Independence Measure scores | Mean | 95% CI of the difference | p -Value | ||
|---|---|---|---|---|---|
| ≤ 2 segment | > 2 segment | Lower | Upper | ||
| Overall FIM | 70.63 | 19.95 | 31.857 | 69.499 | 0.0001 |
| Self-care | 25.47 | 5.05 | 13.007 | 27.823 | 0.0001 |
| Sphincters | 6.35 | 1.30 | 2.791 | 7.307 | 0.0001 |
| Locomotion | 11.26 | 2.85 | 4.672 | 12.139 | 0.0001 |
| Communication | 11.47 | 5.45 | 3.175 | 8.855 | 0.0001 |
| Cognitive | 15.67 | 5.65 | 5.714 | 14.335 | 0.0001 |
Note: p -Value <0.05 are significant.
Abbreviation: FIM, Functional Independence Measure.
Out of the 30 patients who had improvement in the neurological outcome, majority (26) had edema present in less than equal to 2 segments and this was statistically significant ( Table 8 ).
Table 8. Association of extent of edema in the MRI with the neurological outcome.
| Extent of edema in MRI | Neurological outcome | p -Value | |||
|---|---|---|---|---|---|
| Improved n = 30 |
Not improved n = 17 |
Expired n = 14 |
|||
| No edema/contusion | ≤ 2 segment | 3 (75.0%) | 8 (72.7%) | 4 (28.6%) | 0.059 |
| > 2 segment | 1 (25.0%) | 3 (27.3%) | 10 (71.4%) | ||
| Edema present | < 2 segment | 26 (100.0%) | 1 (16.7%) | 0 (0) | 0.0001 |
| > 2 segment | 0 (0.0%) | 5 (83.3%) | 0 (0) | ||
Note: p -Value <0.05 are significant.
Abbreviation: MRI, magnetic resonance imaging.
Discussion
CSIs are a common cause of SCI and can lead to significant neurological and functional impairment. 11 12 Various factors determine the outcome of these injuries and need to be understood well for better prognosis and longevity of life of the sufferers. The following study has followed patients of traumatic CSI postmanagement to determine the neurological and functional outcome as well as assess its associated factors.
The neurological outcome assessed by ASIA grade improved significantly in our study from admission to 4 months' follow-up. This was in consensus with the study by Srinivas et al, who also observed improvement in the ASIA grade among almost half of the patients with cervical SCI. 8 Hitti et al in their study have explained that neurological recovery depends on nonmodifiable factors like sociodemographic information and underlying comorbidity and modifiable factors like timing of surgery, delay in stabilization, progressive edema, or ischemia, etc. and in few cases, the cause is iatrogenic where patients underwent reoperation. 13 Our study has also shown that the rate of improvement was least in ASIA grade A. This was in concordance with Vazquez et al who studied 173 traumatic cervical SCI patients and concluded that the rate of improvement was least in ASIA grade A patients, and none of them were functional. In contrast, incomplete injury patients had better recovery. 14
Significant predictors of neurological improvement in our study were type of injury, presence of edema on MRI, segments involved in injury ≤ 2, and grading of listhesis. Based on these variables, functional outcome (FIM score) was also highly significant. This finding was in concordance with the study by Srinivas et al, who found similar results with cervical injuries that were incomplete (grades C and D), lower cervical injuries (C5–C7), and those exhibiting edema in MRI experiencing greater improvements compared with the individuals with complete, upper cervical injuries (at or above C4), and contusion in the MRI. They also reported that patients with no abnormality on MRI improved to ASIA grade E irrespective of their neurological status at admission. 8 Hence, our study clearly depicts an association of MRI findings (absence of edema and number of segments involved) with the neurological outcome. Moreover, strong association was observed between presence of edema and number of segments involved with the neurological outcome. MRI is a gold standard imaging test for acute spinal trauma. Boldin et al studied the neurological recovery predictive value of MRI findings in 29 patients with acute cervical SCI and a median follow-up of 35 months. Length of edema was the only predictive measure of retaining SCI. Each millimeter increase in the length of edema entailed an increased rate of retaining a complete SCI ( p = 0.017). 15 The resolution of spinal cord edema after SCI with subsequent MRI examinations has been reported previously in the literature. 16 Martínez-Pérez et al found that edema larger than 36 mm was significantly ( p = 0.006) associated with a poor neurological outcome. 10 Hence, length of edema can serve as a proxy indicator of prognosis of traumatic CSIs. 17
Advancing age was associated with poor neurological and functional recovery in our study. It has been hypothesized that advancing age has a negative impact on neurological improvement, 18 19 as it reduces neural plasticity which deteriorates the neurologic recovery. 20 Similarly, other researchers have examined the impact of age and initial neurological status on ambulation recovery in patients with incomplete injuries. They concluded that patients classified as ASIA grade D had an excellent prognosis for achieving independent ambulation regardless of age. However, for patients classified as ASIA grade C, the likelihood of recovering ambulation was influenced by age, with a 42% improvement rate observed in individuals under the age of 50. 9 21 22 23
The following study has highlighted various determinants of neurological and functional outcome among patients with traumatic CSI which will play a key role in clinical decision making of a neurosurgeon. However, a small sample size limits the generalizability of the results, along with no uniformity in imaging and timing of surgery.
Conclusion
The study concludes that incomplete injury, edema on MRI imaging less than equal to 2 segments, and no listhesis are predictors of neurological and functional improvement in patients with traumatic cervical spinal injuries. Overall mean FIM score was higher in those who had less than 2 segments of edema on MRI, with no adverse outcome.
Funding Statement
Funding None.
Footnotes
Conflict of Interest None declared.
References
- 1.World Health Organization.Injuries and Violence: The FactsWorld health Organization.2014. Accessed September 30, 2020 at:https://www.who.int/violence_injury_prevention/media/news/2015/Injury_violence_facts_2014/en
- 2.Kumar R, Lim J, Mekary R A et al. Traumatic spinal injury: global epidemiology and worldwide volume. World Neurosurg. 2018;113:e345–e363. doi: 10.1016/j.wneu.2018.02.033. [DOI] [PubMed] [Google Scholar]
- 3.Leucht P, Fischer K, Muhr G, Mueller E J. Epidemiology of traumatic spine fractures. Injury. 2009;40:166–172. doi: 10.1016/j.injury.2008.06.040. [DOI] [PubMed] [Google Scholar]
- 4.Lomaz M B, Netto L A, Filho M S, Alves A P, De Tavares Canto F R. Epidemiological profile of patients with traumatic spinal fracture. Coluna/Columna. 2017;16:224–227. [Google Scholar]
- 5.Aleem I S, DeMarco D, Drew B et al. The burden of spine fractures in India: a prospective multicentre study. Global Spine J. 2017;7:325–333. doi: 10.1177/2192568217694362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh G, Prakash R, Bhatti V, Mahen A. Spinal cord injury in organizational setup-a hospital based descriptive study. J Mar Med Soc. 2019;21:46–50. [Google Scholar]
- 7.Birua G JS, Munda V S, Murmu N N. Epidemiology of spinal injury in north east India: a retrospective study. Asian J Neurosurg. 2018;13:1084–1086. doi: 10.4103/ajns.AJNS_196_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Srinivas B, Rajesh A, Purohit A. Factors affecting outcome of acute cervical spine injury: a prospective study. Asian J Neurosurg. 2017;12(03):416–423. doi: 10.4103/1793-5482.180942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Katzberg R W, Benedetti P F, Drake C M et al. Acute cervical spine injuries: prospective MR imaging assessment at a level 1 trauma centre. Radiology. 1999;213(01):203–212. doi: 10.1148/radiology.213.1.r99oc40203. [DOI] [PubMed] [Google Scholar]
- 10.Martínez-Pérez R, Cepeda S, Paredes I, Alen J F, Lagares A. MRI prognostication factors in the setting of cervical spinal cord injury secondary to trauma. World Neurosurg. 2017;101:623–632. doi: 10.1016/j.wneu.2017.02.034. [DOI] [PubMed] [Google Scholar]
- 11.Schousboe J T. Epidemiology of vertebral fractures. J Clin Densitom. 2016;19:8–22. doi: 10.1016/j.jocd.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 12.den Ouden L P, Smits A J, Stadhouder A, Feller R, Deunk J, Bloemers F W. Epidemiology of spinal fractures in a level one trauma center in the Netherlands: a 10 years review. Spine. 2019;44:732–739. doi: 10.1097/BRS.0000000000002923. [DOI] [PubMed] [Google Scholar]
- 13.Hitti F L, McShane B J, Yang A I et al. Predictors of neurological outcome following subaxial cervical spine trauma. Cureus. 2019;11(12):e6402. doi: 10.7759/cureus.6402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vazquez X M, Rodriguez M S, Peñaranda J M, Concheiro L, Barus J I. Determining prognosis after spinal cord injury. J Forensic Leg Med. 2008;15:20–23. doi: 10.1016/j.jflm.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 15.Boldin C, Raith J, Fankhauser F, Haunschmid C, Schwantzer G, Schweighofer F. Predicting neurologic recovery in cervical spinal cord injury with postoperative MR imaging. Spine. 2006;31(05):554–559. doi: 10.1097/01.brs.0000201274.59427.a4. [DOI] [PubMed] [Google Scholar]
- 16.Tarawneh A M, D'Aquino D, Hilis A, Eisa A, Quraishi N A. Can MRI findings predict the outcome of cervical spinal cord injury? A systematic review. Eur Spine J. 2020;29:2457–2464. doi: 10.1007/s00586-020-06511-7. [DOI] [PubMed] [Google Scholar]
- 17.Wenger M, Adam P J, Alarcón F, Markwalder T M. Traumatic cervical instability associated with cord oedema and temporary quadriparesis. Spinal Cord. 2003;41(09):521–526. doi: 10.1038/sj.sc.3101485. [DOI] [PubMed] [Google Scholar]
- 18.Singh R, Sharma S, Mittal R, Sharma A. Traumatic spinal cord injuries in Haryana: an epidemiological study. Indian J Community Med. 2003;13:184–186. [Google Scholar]
- 19.Grauer J N, Vaccaro A R, Lee J Y et al. The timing and influence of MRI on the management of patients with cervical facet dislocations remains highly variable: a survey of members of the spine trauma study group. J Spinal Disord Tech. 2009;22:96–99. doi: 10.1097/BSD.0b013e31816a9ebd. [DOI] [PubMed] [Google Scholar]
- 20.Hadley M N, Walters B C. The case for the future role of evidence-based medicine in the management of cervical spine injuries, with or without fractures. J Neurosurg Spine. 2019;31:457–463. doi: 10.3171/2019.6.SPINE19652. [DOI] [PubMed] [Google Scholar]
- 21.Gelb D E, Hadley M N, Aarabi B et al. Initial closed reduction of cervical spinal fracture-dislocation injuries. Neurosurgery. 2013;72:73–83. doi: 10.1227/NEU.0b013e318276ee02. [DOI] [PubMed] [Google Scholar]
- 22.Passias P G, Poorman G W, Segreto F A et al. Traumatic fractures of the cervical spine: analysis of changes in incidence, cause, concurrent injuries, and complications among 488,262 patients from 2005 to 2013. World Neurosurg. 2018;110:e427–e437. doi: 10.1016/j.wneu.2017.11.011. [DOI] [PubMed] [Google Scholar]
- 23.Jain M, Mohanty C R, Doki S K et al. Traumatic spine injuries in Eastern India: a retrospective observational study. Int J Crit Illn Inj Sci. 2021;11(02):79. doi: 10.4103/IJCIIS.IJCIIS_95_20. [DOI] [PMC free article] [PubMed] [Google Scholar]


