Both in everyday life and extraordinary situations such as wars and natural disasters, humans are at risk of zoonotic diseases. These diseases originate in animals but can be transmitted to humans. Whether endemic or newly emerging, bacterial zoonotic diseases can significantly threaten public health, individual livelihoods, national economies, and food security.1, 2 Infectious diseases originating from wildlife have always been a particular risk for human epidemics, particularly when first transmitted between the species. Because the human immune system does not have an established defense against the disease at this point, it can spread rapidly. Direct or indirect contact between humans and animals and their bodily fluids is necessary for interspecies transmission. While humans have coexisted with domestic and wild animals for thousands of years, various anthropogenic factors have recently intensified the animal-human interface, increasing our interactions with animals and the risk of disease transmission between them.3
The risk of zoonotic diseases is higher in densely populated areas, among displaced groups such as immigrant refugees, when there are changes in social structures or human behaviors, in overcrowded and unhygienic camps and housing, and in regions with poor or deteriorating health infrastructures. Zoonotic diseases, such as brucellosis, rabies, human immunodeficiency virus, and the recently emerged severe acute respiratory syndrome coronavirus 2 can lead to large-scale epidemics and pandemics that spread exponentially as they are transmitted from person to person.4
Natural disasters can lead to infectious disease outbreaks, including zoonotic diseases. This occurs when they cause significant population displacement and exacerbate risk factors for disease transmission such as increased vulnerability to existing pathogens, changes in the environment, and changes in human living conditions. Disease outbreaks following disasters such as floods, tsunamis, earthquakes, tropical cyclones, hurricanes, typhoons, and tornadoes have included diarrheal diseases, acute respiratory infections, malaria, leptospirosis, measles, dengue fever, viral hepatitis, typhoid fever, meningitis, tetanus, and cutaneous mucormycosis. The increase in the spread of infectious diseases and increased risk of epidemics after natural disasters is primarily attributable to the longer-term, less immediate effects of the disaster. The downstream impacts that mediate the relationship between natural disasters and zoonotic disease outbreaks include displaced populations (both internally displaced and refugees), environmental changes, proliferation of disease vectors (rodents, mosquitoes), increases in vector breeding grounds, increased human exposure to disease vectors, unplanned settlements and overcrowded housing, unclean water, poor sanitation conditions and personal hygiene, malnutrition, low levels of immunity to vaccine-preventable diseases or inadequate vaccination coverage, and limited access to healthcare. Changes in human living conditions, the pathogen ecosystem, and the environment are known as the epidemiological triad (agent, host, environment) as they facilitate the emergence and transmission of infectious diseases.5 Table 1 lists notable outbreaks of zoonotic diseases associated with wars and natural disasters.6
Table 1.
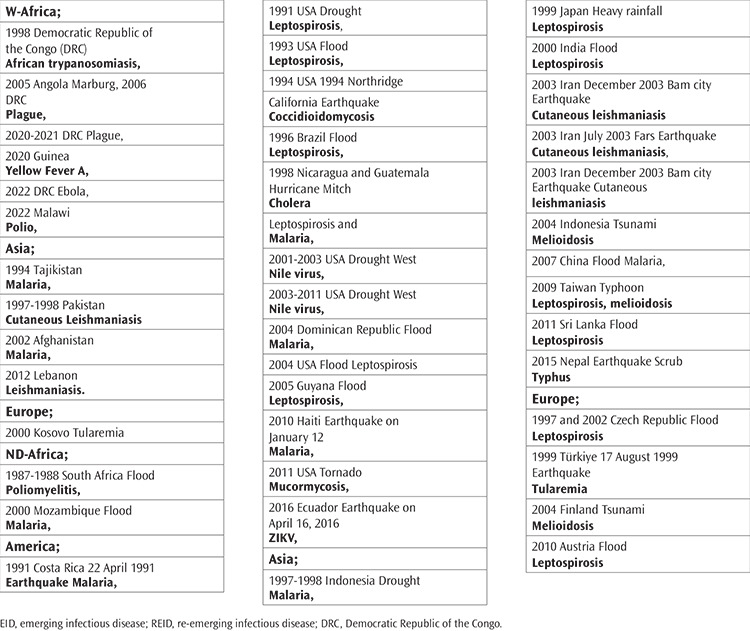
Selected EIDs/REIDs Outbreaks Associated with Wars (W) and Natural Disasters (ND), Year Continent/Region, Emerging Infectious Diseases/Re-Emerging Infectious Diseases (EID/REID) respectively.6
The One Health approach brings together experts from various fields to work synergistically to optimize health internationally, nationally, regionally, and within every human community. The application of this approach to the reduction and prevention of zoonotic disease outbreaks among humans has brought together the knowledge, expertise, and practical skills of professionals from a wide range of fields, including human and veterinary medicine, epidemiology, ecology, and environmental science. Detecting and reporting disease outbreaks early is essential and interventions must be implemented immediately to prevent further spread. The One Health approach aims to understand disease origins, transmission dynamics, and prevention strategies. It also develops strategies for the prevention, control, and treatment of zoonotic diseases. These include the promotion and execution of animal vaccination programs, controlling disease vectors, improving hygiene practices within human communities, and improving biosecurity measures in livestock production.7 Clinical studies of COVID-19 have shown that vaccines are highly effective in preventing symptomatic diseases and reducing disease transmission, mortality rates, and related hospital and intensive care admission rates.8 In addition, the One Health approach recognizes that the environment conditions and the health of ecosystems are vital considerations in the prevention of diseases. Experts working within the One Health paradigm have studied the effects of environmental factors such as deforestation, climate change, and biodiversity loss on the emergence of diseases. Protecting natural habitats and promoting sustainable practices can help reduce disease risks.7 Increasing awareness, more rapid identification of outbreaks, public health information campaigns, education, research, and a multidisciplinary approach coordination by national health departments are all necessary factors in disease control and epidemic prevention. This is an issue that directly concerns national populations and economies and the implementation of the above measures should be prioritized to ensure effective management of disease outbreaks and minimize their long-term effects. The longer an epidemic continues, the more difficult it becomes to meet healthcare needs, particularly in low- and middle-income countries with large populations. Epidemics are a considerable drain on fiscal and medical resources and workforce loss can further impede economic recovery. Therefore, this issue needs to be addressed in detail by the World Health Organization and governments.9
When wars and natural disasters occur, human nutritional resources often become sparse. Those in affected areas may find themselves living in crowded, unsuitable conditions with inadequate hygiene. Following such events, emergency action plans must be created and implemented by governments and relevant stakeholders. While these should focus on meeting the survival needs of those affected, the prevention of zoonotic disease outbreaks and epidemics must also be incorporated into these plans. Meeting some of these survival needs will contribute somewhat to disease prevention through access to clean water, shelter, and healthy food. Nevertheless, it is vital that additional measures are taken to reduce the risk of disease as the detrimental effects of epidemics following closely on the heels of another national crisis are much higher as financial resources and healthcare are already stretched to their limit. Prevention is more easily implemented than treatment and minimization of the speed and extent of disease dissemination.
Footnotes
Conflict of Interest: No conflict of interest was declared by the author
References
- 1.Arredondo-Rivera M, Barois Z, Monti GE, Steketee J, Daburon A. Bridging Food Systems and One Health: A key to preventing future pandemics? One Health. 2024;18:100727. doi: 10.1016/j.onehlt.2024.100727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang T, Nickerson R, Zhang W. The impacts of animal agriculture on One Health-Bacterial zoonosis, antimicrobial resistance, and beyond. One Health. 2024;18:100748. doi: 10.1016/j.onehlt.2024.100748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Magouras I, Brookes VJ, Jori F, Martin A, Pfeiffer DU, Dürr S. Emerging Zoonotic Diseases: Should We Rethink the Animal-Human Interface? Front Vet Sci. 2020;7:582743. doi: 10.3389/fvets.2020.582743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oakley R, Hedrich N, Walker A. Status of zoonotic disease research in refugees, asylum seekers and internally displaced people, globally: A scoping review of forty clinically important zoonotic pathogens. PLoS Negl Trop Dis. 2024;18(5):e0012164. doi: 10.1371/journal.pntd.0012164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kouadio IK, Aljunid S, Kamigaki T, Hammad K, Oshitani H. Infectious diseases following natural disasters: prevention and control measures. Expert Rev Anti Infect Ther. 2012;10(1):95–104. doi: 10.1586/eri.11.155. [DOI] [PubMed] [Google Scholar]
- 6.Topluoglu S, Taylan-Ozkan A, Alp E. Impact of wars and natural disasters on emerging and re-emerging infectious diseases. Front Public Health. 2023;11:1215929. doi: 10.3389/fpubh.2023.1215929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adnyana IM, Utomo B, Eljatin DS, Sudaryati NL. One Health approach and zoonotic diseases in Indonesia: Urgency of implementation and challenges. Narra J. 2023;3(3):e257. doi: 10.52225/narra.v3i3.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gül F, Kasapoğlu US, Sabaz MS. The Impact of CoronaVac Vaccination on 28-day Mortality Rate of Critically Ill Patients with COVID-19 in Türkiye. Balkan Med J. 2023;40(6):435–444. doi: 10.4274/balkanmedj.galenos.2023.2023-6-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nune A, Iyengar KP, Barman B, Manzo C. Post-COVID-19 Condition and İts Recognition in Low- and Middle-income Countries: Working Notes from the United Kingdom Experience. Balkan Med J. 2022;39(4):303–304. doi: 10.4274/balkanmedj.galenos.2022.2022-5-102. [DOI] [PMC free article] [PubMed] [Google Scholar]


