Abstract
Cytotoxic T lymphocytes (CTLs) are proposed to be critical for protection from intracellular pathogens such as Ebola virus. However, there have been no demonstrations that protection against Ebola virus is mediated by Ebola virus-specific CTLs. Here, we report that C57BL/6 mice vaccinated with Venezuelan equine encephalitis virus replicons encoding the Ebola virus nucleoprotein (NP) survived lethal challenge with Ebola virus. Vaccination induced both antibodies to the NP and a major histocompatibility complex class I-restricted CTL response to an 11-amino-acid sequence in the amino-terminal portion of the Ebola virus NP. Passive transfer of polyclonal NP-specific antiserum did not protect recipient mice. In contrast, adoptive transfer of CTLs specific for the Ebola virus NP protected unvaccinated mice from lethal Ebola virus challenge. The protective CTLs were CD8+, restricted to the Db class I molecule, and recognized an epitope within amino acids 43 to 53 (VYQVNNLEEIC) in the Ebola virus NP. The demonstration that CTLs can prevent lethal Ebola virus infection affects vaccine development in that protective cellular immune responses may be required for optimal protection from Ebola virus.
Ebola viruses are associated with outbreaks of highly lethal hemorrhagic fever in humans and nonhuman primates. The Ebola Zaire viruses responsible for outbreaks of human disease in 1976 and 1995 had case-fatality rates of greater than 80% (7, 21). The immune mechanisms necessary for protecting against Ebola virus infection are not clearly identified, and no vaccines or effective therapeutic treatments are currently available.
For vaccine development, it is critically important to identify protective immune responses and to ensure that the vaccine approaches adequately induce those responses. Several reports have evaluated various vaccine approaches and have tried to identify correlates of immunity for Ebola virus. Protection in animals has been demonstrated with candidate vaccines expressing the Ebola virus glycoprotein (GP) (4, 12, 13, 18, 22) or nucleoprotein (NP) (12, 18, 22). Standard enzyme-linked immunosorbent assays (ELISAs) have detected serum antibodies to the Ebola virus GP and NP after vaccination (4, 12, 13, 18, 22), although titers of virus-neutralizing antibodies in plaque reduction assays were either undetected (18, 22) or low (4, 12), and transfer of immune sera did not protect unvaccinated animals (12). The induction of cytotoxic-T-lymphocyte (CTL) responses to GP and NP was examined in only two of these studies (18, 22), with both reporting lysis of transformed cells expressing GP and only one reporting lysis of cells expressing NP (18). A third group vaccinated animals with liposome-encapsulated irradiated virus and identified a CTL epitope in the GP (16). However, because none of these studies evaluated the ability of the CTLs to protect against Ebola virus challenge, it is unknown whether these CTLs contributed to the protection observed in vaccinated animals. Therefore, although these studies suggest that both humoral and cellular immune mechanisms may function in vivo in protection, this has yet to be demonstrated.
The induction of both antibodies and CTLs to an Ebola virus protein makes it difficult to determine the relative contribution of each effector function in eliciting protective immunity. Protection elicited by polyclonal antisera to Ebola virus has been demonstrated but is inconsistent in different animal models for this disease (2, 6, 8). We recently identified monoclonal antibodies to the Ebola virus GP that are sufficient for protecting mice from a lethal Ebola virus challenge (20). However, protective responses elicited by viral antigens that are not present on the surface of the virion, such as the NP, are more likely to be due to CTLs. If CTLs are necessary to ensure protection from Ebola virus, the major histocompatibility complex (MHC) restriction of CTL responses and the limited number of CTL epitopes usually present in viral proteins (17) will make it more difficult to develop optimal vaccines for human use. This study was therefore initiated in order to identify the NP-specific immune response(s) mediating protection against Ebola virus.
MATERIALS AND METHODS
Vaccination and challenge of mice.
Specific-pathogen-free 6- to 8-week-old female C57BL/6 mice (National Cancer Institute, Frederick, Md.) were housed in cages equipped with microisolators and were provided food and water ad libitum. Research was conducted in compliance with the Animal Welfare Act and other Federal statutes and regulations relating to animals and experiments involving animals, and it adheres to principles stated in the Guide for the Care and Use of Laboratory Animals (10a). The facility where this research was conducted is fully accredited by the Association for Assessment and Accreditation of Laboratory Animal Care International. Animal experiments were performed a minimum of two times.
Groups of 10 mice per experiment were injected subcutaneously at the base of the neck with 2 × 106 focus-forming units of Venezuelan equine encephalitis (VEE) virus replicons encoding the Ebola virus NP protein (12, 13) or with a control replicon encoding Lassa virus N (14). For booster vaccinations, animals received identical injections at 1-month intervals. One month after the final booster injection, mice were transferred to a BSL-4 containment area and challenged by intraperitoneal (i.p.) inoculation of 10 PFU of mouse-adapted Ebola virus (3) (approximately 300 times the dose lethal for 50% of adult mice [LD50]). The mice were observed daily for at least 28 days, and morbidity and mortality were recorded.
To measure viral titers, four or five vaccinated mice were anesthetized and exsanguinated on day 5 after challenge, and the titers in serum were determined by plaque assay (10).
Antibody titers from mouse sera were determined by ELISA as described previously (20) with plates coated with sucrose-purified, irradiated Ebola Zaire 1995 virions. The end point of reactivity was defined as the last dilution with an absorbance at least 0.2 unit above that of control wells.
Transfer of cells and serum.
Donor sera were obtained from mice 28 days after the third inoculation with 2 × 106 focus-forming units of VEE virus replicons encoding either the Ebola virus NP or the control Lassa virus N. One milliliter of pooled donor serum was administered i.p. to unvaccinated C57BL/6 mice 24 h before i.p. challenge with 300 LD50s of mouse-adapted Ebola virus. For in vitro neutralization assays, twofold serial dilutions of pooled mouse sera (starting at a 1:10 dilution) were mixed with 100 PFU of mouse-adapted Ebola Zaire virus at 37°C for 1 h and used to infect Vero E6 cells (ATCC CRL 1586). Cells were overlaid with agarose (10), and a second overlay containing 5% neutral red was added 6 days later. Plaques were counted the next day and compared with control wells in which culture medium was added in the place of mouse sera.
For adoptive transfer experiments, mice were injected i.p. with 1 × 104 to 8 × 106 effector cells 4 hours before i.p. inoculation of 300 or 3,000 LD50s of mouse-adapted Ebola virus.
In vitro restimulation and chromium release assays.
In vitro restimulation of spleen cells and standard 4-h chromium release assays were performed essentially as described previously (5). Briefly, spleen cells were cultured in RPMI-EHAA medium supplemented with 10% heat-inactivated fetal bovine serum, 2 mM glutamine, 10 μg of gentamicin per ml, 5 mM HEPES, and 0.05 mM β-mercaptoethanol for 7 days in the presence of 10 μM Ebola virus NP peptide, 10 μM Lassa virus N peptide, or irradiated, allogeneic spleen cells from BALB/c mice. A 10% (vol/vol) solution of concanavalin A supernatant and 10 U of interleukin-2 (Beckton Dickinson) per ml was added to cultures on the second day of restimulation. Viable effector cells were isolated by centrifugation over a Fico/Lite cushion (Atlanta Biologicals; density, 1.086 g/ml) and were washed three times with 0.3 M α-methylmannoside (Sigma) to remove lectin.
Target cells (ATCC TIB-39 EL4 cells, ATCC CRL-1723 L5178Y-2 cells, or concanavalin A-stimulated spleen cells) were labeled with 200 μCi of 51Cr (New England Nuclear) for 1.5 h at 37°C and washed three times, and 5,000 cells were added to assay wells. Splenocytes from C57BL/6, B10.A(2R), or B10.A(5R) mice (Jackson Laboratories) were cultured for 4 days in RPMI-EHAA medium supplemented with 10 μg of concanavalin A (Sigma) per ml to produce blast cells. For peptide-coated target cells, Ebola virus NP peptide (VYQVNNLEEIC; purchased from Biosynthesis [>75% purity] or Sigma Genosys [>80% purity]) or irrelevant Lassa virus N peptide (RPLSAGVYMGNLSSQ; made using an Applied Biosystems, Inc., 341 synthesizer) was added directly to the assay wells at a final concentration of 50 μM. The Lassa virus peptide is based on a common arenavirus CTL epitope (19) and is recognized by CTLs induced by vaccination with VEE virus replicons expressing Lassa virus N (data not shown).
Percent specific lysis was calculated as [(experimental release − spontaneous release)/(maximum release − spontaneous release)] × 100. Spontaneous release by labeled target cells was determined from wells to which medium was added in the place of effector cells and did not exceed 8% of the maximum release obtained from wells in which the target cells were incubated with 1% Triton X-100 (Sigma).
Cell separation and analysis.
Effector cell cultures were separated using the Dynabeads mouse CD4 (L3T4) and mouse CD8 (Lyt 2) system (Dynal) according to the manufacturer's protocol. CD8-enriched cells were obtained by harvesting the cell suspension after depletion of CD4 cells with the mouse CD4 beads. CD4-enriched cells were obtained either by removal from the CD4 beads with DETACHaBEAD mouse CD4 (Dynal) or by harvesting the cell suspension after depleting CD8 cells with the mouse CD8 beads. No functional difference was observed between CD4 cells isolated using the two methods.
The phenotype of the effector cells was determined using fluorescein isothiocyanate-conjugated rat anti-mouse CD4 (L3/T4), rat anti-mouse CD8a (Ly2), and hamster anti-mouse T3 complex CD3ε (L3/T4) antisera from Cedarlane. Cells were incubated at 4°C for 30 min with antisera, washed in phosphate-buffered saline, fixed with 0.5% paraformaldehyde, and analyzed on a FACScan.
RESULTS AND DISCUSSION
The development of a mouse-adapted strain of Ebola virus (3) has facilitated the ability to examine the role of antibodies and CTLs in mediating protection from Ebola virus. The mouse-adapted virus is uniformly lethal to immunocompetent mice when delivered intraperitoneally (3). This virus is also lethal to guinea pigs and causes severe illness that can be lethal to rhesus monkeys (M. Bray, personal communication). The ability to transfer immune effectors into naive, genetically identical mice prior to challenge provides the opportunity to examine the in vivo contribution of CTLs in protection, thereby aiding in the identification of protective immune effectors critical for Ebola virus vaccine development.
Vaccination with Ebola virus NP expressed from a VEE virus replicon has been shown to induce protection in BALB/c mice against lethal challenge with mouse-adapted Ebola virus (12). Our studies extended this observation to C57BL/6 mice, which differ from BALB/c mice at the MHC. Two or three injections of 106 focus-forming units of VEE virus replicons expressing the Ebola virus NP induced protection from lethal Ebola challenge in 75 to 80% of the mice (Table 1). Ebola virus was detected in the sera of vaccinated animals after challenge (Table 1), indicating that mice vaccinated with the Ebola virus NP replicons were not resistant to infection. However, the viral load in Ebola virus NP-vaccinated mice was markedly reduced compared with that in control animals vaccinated with VEE virus replicons expressing the Lassa virus N gene (Table 1).
TABLE 1.
Protective efficacy of Ebola virus NP replicons in C57BL/6 micea
| Replicon injected | No. of injections | No. of survivors/ total | Days to deathb | No. viremic/totalc | Viremia, GMTe (log10 PFU/ml) |
|---|---|---|---|---|---|
| Ebola virus NP | 3 | 15/20 | 8.0 ± 0.8 | 5/5 | 4.1 ± 1.1 |
| 2 | 8/10 | 8.5 | NDd | ND | |
| Lassa virus N | 3 | 1/20 | 7.3 ± 0.6 | 4/4 | 8.6 ± 0.7 |
| 2 | 0/10 | 7.1 ± 0.3 | ND | ND |
Mice were injected two or three times at 1-month intervals with the Ebola virus NP replicon or the control Lassa virus N replicon. One month after the final injection, mice were challenged with mouse-adapted Ebola Zaire virus.
The time to death for mice that did not survive challenge is reported as the mean ± standard deviation for groups with at least three deaths or as the average for the group with two deaths.
Number of mice with measurable levels of Ebola virus in the sera 5 days post-Ebola virus challenge/total number of mice tested.
ND, not determined.
GMT, geometric mean titer of the virus detected in the sera 5 days post-Ebola challenge.
The vaccinated mice had mean end point antibody titers to the Ebola virus NP of 3 to 3.5 logs in ELISA prior to challenge. These antibodies did not inhibit plaque formation by mouse-adapted Ebola virus at a 1:20 dilution. To determine if antibodies to the Ebola virus NP were capable of protecting against lethal Ebola virus challenge, 1 ml of immune serum pooled from mice vaccinated three times with Ebola virus NP replicons was passively transferred to unvaccinated mice 24 h before lethal challenge with mouse-adapted Ebola Zaire virus. The recipient mice had serum antibodies to the Ebola virus NP (end point titers of 2.5 to 3 logs in ELISA) 5 h prior to challenge. However, as was observed with BALB/c mice (12), passive transfer of immune serum to the Ebola virus NP did not protect unvaccinated C57BL/6 mice from lethal disease (Table 2) or extend the time to death (data not shown).
TABLE 2.
CD8+ T lymphocytes protect against lethal Ebola virus challenge
| Cells or serum transferred | Amt transferred | No. of survivors/total after challenge with:
|
|
|---|---|---|---|
| 300 LD50s | 3,000 LD50s | ||
| Unfractionated T cells | 8 × 106 cells | 20/20 | 10/10 |
| 1 × 106 cells | 16/20 | 8/10 | |
| 1 × 105 cells | 3/20 | 1/10 | |
| 1 × 104 cells | 1/20 | 0/10 | |
| CD8-enriched T cellsa | 1 × 106 cells | 17/20 | 9/10 |
| CD4-enriched T cellsb | 1 × 106 cells | 0/20 | NDe |
| MLR control T cellsc | 8 × 106 cells | 1/20 | 0/10 |
| Naive control T cellsd | 8 × 106 cells | 0/20 | 0/10 |
| Ebola virus NP serum | 1 ml | 0/20 | ND |
| Lassa virus N serum | 1 ml | 0/20 | ND |
Combined results from different experiments, in which the CD8-enriched cultures were 94 to 96% CD8+ cells and <3% CD4+ cells.
Combined results from different experiments, in which the CD4-enriched cultures contained 95 to 98% CD4+ cells and 2 to 3% CD8+ cells.
MLR, mixed lymphocyte reaction. Control cells specific for allogeneic BALB/c cells and approximately 80% CD8+.
Naive control cells from unvaccinated C57BL/6 mice that were stimulated in vitro with the Ebola virus NP peptide.
ND, not determined.
To determine if NP-specific CTLs were involved in protection from lethal Ebola virus challenge, we used a computer algorithm (11) and predicted binding motifs (15) to examine the Ebola virus NP sequence for possible H-2b class I-restricted epitopes. Both methods predicted that an amino acid sequence contained within VYQVNNLEEIC would be bound by H-2Db class I molecules. This peptide was chemically synthesized and used to restimulate immune splenocytes in vitro before cells were examined for functional activity.
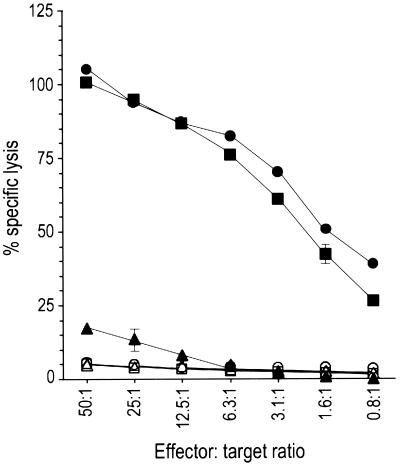
Spleen cells from mice vaccinated with the Ebola virus NP expressed from VEE virus replicons were restimulated in vitro with the NP peptide (VYQVNNLEEIC) and tested for lysis in a chromium release assay. These cells had high levels of cytolytic activity against syngeneic target cells (EL4) coated with the Ebola virus NP peptide (Fig. 1). These CTLs failed to lyse either untreated EL4 target cells, EL4 target cells coated with a peptide recognized by Lassa virus-specific CTLs, or H-2-incompatible cells (L5178Y, H-2d) coated with the Ebola virus NP peptide (Fig. 1). In vivo priming of the CTL response was required, as no lysis of Ebola virus NP peptide-coated target cells was observed after in vitro Ebola virus NP peptide stimulation of spleen cells from unvaccinated C57BL/6 mice or C57BL/6 mice vaccinated with the control Lassa virus N replicon (data not shown).
FIG. 1.
Lysis of target cells by cytotoxic T cells from mice vaccinated with the VEE replicon expressing the Ebola virus NP. Syngeneic EL4 cells coated with the Ebola virus NP peptide were tested for lysis by unfractionated (closed squares), CD8-enriched (closed circles), or CD4-enriched (closed triangles) effector cells. Unfractionated cells were also tested for lysis of untreated EL4 cells (open circles), EL4 cells coated with a Lassa virus N peptide (open triangles), and allogeneic L5178Y cells coated with Ebola virus NP peptide (open squares). Data from a representative experiment are shown as the mean specific lysis ± the standard deviation from triplicate wells.
FACScan analysis indicated that the cultures obtained in different experiments contained 6 to 33% CD4+ cells and 54 to 90% CD8+ cells. These cell populations were separated by magnetic beads coated with antibodies to CD4 or CD8 to determine the phenotype of the cells responsible for CTL activity. In separate experiments, FACScan analysis indicated that the cell separations yielded CD4-enriched cultures containing 95 to 98% CD4+ cells and 2 to 3% CD8+ cells and CD8-enriched cultures with 94 to 96% CD8+ cells and <3% CD4+ cells. Chromium release assays performed using the fractionated cell populations as effector cells demonstrated that the CD8+ cells mediated the CTL activity (Fig. 1). To confirm that the CTLs were restricted to the NP peptide bound by Db class I molecules, as predicted by the binding motif (11, 15), we tested for lysis of concanavalin A-stimulated spleen cells obtained from inbred mice with different K or D class I molecules. At an effector/target cell ratio of 50:1, 50% specific release was observed against Ebola virus NP peptide-coated H-2 KkDb target cells from B10.A(2R) mice, but only 16% specific release was observed using peptide-coated H-2KbDd target cells from B10.A(5R) mice.
To determine if the CTLs were efficacious in vivo, either the unfractionated, the CD8-enriched, or the CD4-enriched cells were injected i.p. into unvaccinated C57BL/6 mice 4 h before a lethal challenge with mouse-adapted Ebola Zaire virus. Mice were protected from Ebola virus challenge if they received either the unfractionated or the CD8-enriched T cells (Table 2). The adoptive transfer of as few as 1 million cells protected at least 80% of the mice from death after challenge with up to 3,000 times the Ebola virus LD50 (Table 2). This was similar to the efficacy achieved with vaccination. The survival of all mice receiving eightfold more CTLs suggests that the vaccination strategy may be optimized to achieve 100% efficacy.
In contrast to what was observed with the adoptive transfer of the unfractionated and CD8-enriched T cells, the CD4-enriched T-cell population did not protect mice from lethal disease (Table 2). Similarly, no protection was afforded by the transfer of either control CTLs specific for allogeneic BALB/c cells (approximately 80% CD8+) or cells that were obtained from unvaccinated C57BL/6 mice and stimulated in vitro with the Ebola virus NP peptide (Table 2). These data demonstrate that vaccination with replicons expressing the Ebola virus NP induces CTLs that are protective in vivo against Ebola virus challenge.
We chose to examine the efficacy of the CTLs by transferring cells into naive recipients rather than by in vivo depletion of CD4+ or CD8+ cells prior to vaccination or challenge. This strategy enabled us to directly examine the effect of specific T cells with defined lytic capability in the absence of any Ebola virus-specific antibodies that would be present as a result of vaccination or increased levels of cytokines and chemokines resulting from the in vivo lysis and clearance of cells. The latter point is relevant to Ebola virus challenge, as several reports have suggested that innate immunity or the production of cytokines and chemokines may affect the outcome of human disease progression (1, 9).
Examination of sera drawn from surviving mice 28 days after challenge demonstrated the presence of antibodies to the Ebola virus. This was not unexpected, as the lysis of virus-infected cells by CTLs exposes the humoral immune system to viral antigens. Therefore, it is not known whether the CTLs were entirely responsible for eliminating the virus or if they worked in conjunction with antibodies that were induced to other viral proteins, such as the Ebola virus GP, in response to viral replication in infected cells. However, the CTLs specific for the Ebola virus NP controlled infection sufficiently to enable survival of the mice, which would have otherwise succumbed to lethal infection within a week after challenge. The finding that control CD8+ CTLs neither protected mice nor extended the time to death after challenge suggests that the ability of the Ebola virus NP-specific CTLs to lyse infected cells was essential for protection from lethal Ebola challenge and that protection was not simply due to nonspecific mediators or cytokines being secreted by the transferred cells.
This study represents the first demonstration of CTL-mediated protection against a lethal Ebola virus challenge. This is important in that it formally demonstrates that CTLs contribute to protection from Ebola virus and stresses the need to closely examine the ability of all viral proteins to induce protective cellular immune responses for the development of effective vaccine strategies for Ebola hemorrhagic fever. Taking these results together with our previous study that identified protective monoclonal antibodies to the Ebola virus GP, it is likely that an optimal Ebola virus vaccine will need to induce protective humoral as well as protective cellular responses to efficiently clear both free virus and virus-infected cells. Due to the MHC -restriction of CTL responses and the limited number of CTL epitopes on viral proteins (17), the inclusion of several viral proteins capable of eliciting protective CTLs may be necessary to ensure the induction of adequate protection by an eventual human-use vaccine.
ACKNOWLEDGMENTS
We thank R. Bakken, J. Kondig, and M. Azarion for technical assistance; S. Trevino and T. Chanh for help with FACScan analysis; M. Bray for providing the mouse-adapted Ebola virus; P. Pushko and J. Smith for providing the Ebola virus NP and Lassa virus N replicon constructs; and A. Schmaljohn for providing the Lassa virus N peptide used in these studies.
J.A.W. was supported, in part, by a National Research Council fellowship.
REFERENCES
- 1.Baize S, Leroy E M, Georges-Courbot M-C, Capron M, Lansoud-Soukate J, Debré P, Fisher-Hoch S P, McCormick J B, Georges A J. Defective humoral responses and extensive intravascular apoptosis are associated with fatal outcome in Ebola virus-infected patients. Nat Med. 1999;5:423–426. doi: 10.1038/7422. [DOI] [PubMed] [Google Scholar]
- 2.Borisevich I V, Mikhailov V V, Krasnyanskii V P, Gradoboev V N, Lebedinskaya Y V, Potryvaeva N V, Timan'kova G D. Creation and study of immunoglobulin to Ebola fever. Russ Prog Virol. 1995;6:42–45. [PubMed] [Google Scholar]
- 3.Bray M, Davis K, Geisbert T, Schmaljohn C, Huggins J. A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J Infect Dis. 1998;178:651–661. doi: 10.1086/515386. [DOI] [PubMed] [Google Scholar]
- 4.Gilligan K J, Geisbert J B, Jahrling P B, Anderson K. Assessment of protective immunity conferred by recombinant vaccinia viruses to guinea pigs challenged with Ebola virus. In: Brown F, Burton D, Doherty P, Mekalanos J, Norrby E, editors. Vaccines 97. Cold Spring Harbor, N.Y: Cold Spring Harbor Laboratory Press; 1997. pp. 87–92. [Google Scholar]
- 5.Hart M K, Weinhold K J, Scearce R M, Washburn E M, Clark C A, Palker T J, Haynes B F. Priming of anti-human immunodeficiency virus (HIV) CD8+ cytotoxic T cells in vivo by carrier-free HIV synthetic peptides. Proc Natl Acad Sci USA. 1991;88:9448–9452. doi: 10.1073/pnas.88.21.9448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jahrling P B, Geisbert T W, Geisbert J B, Swearengen J R, Bray M, Jaax N K, Huggins J W, LeDuc J W, Peters C J. Evaluation of immune globulin and recombinant interferon-α2b for treatment of experimental Ebola virus infections. J Infect Dis. 1999;179(Suppl 1):S224–234. doi: 10.1086/514310. [DOI] [PubMed] [Google Scholar]
- 7.Khan A S, Tshiokoo F K, Heymann D L, Le Guenno B, Nabeth P, Kerstiens B, Fleerackers Y, Kilmarx P H, Rodier G R, Nkuku O, Rollin P E, Sanchez A, Zaki S R, Swanepoel R, Tomori O, Nichol S T, Peters C J, Muyembe-Tamfum J J, Ksiazek T G. The reemergence of Ebola hemorrhagic fever, Democratic Republic of the Congo, 1995. J Infect Dis. 1999;179(Suppl 1):S76–86. doi: 10.1086/514306. [DOI] [PubMed] [Google Scholar]
- 8.Kudoyarova-Zubavichene N M, Sergeyev N N, Chepurnov A A, Netesov S V. Preparation and use of hyperimmune serum for prophylaxis and therapy of Ebola virus infections. J Infect Dis. 1999;179(Suppl 1):S218–223. doi: 10.1086/514294. [DOI] [PubMed] [Google Scholar]
- 9.Leroy E M, Baize S, Volchkov V E, Fisher-Hoch S P, Georges-Courbot M-C, Lansoud-Soukate J, Capron M, Debré P, McCormick J B, Georges A J. Human asymptomatic Ebola infection and strong inflammatory response. Lancet. 2000;355:2210–2215. doi: 10.1016/s0140-6736(00)02405-3. [DOI] [PubMed] [Google Scholar]
- 10.Moe J B, Lambert R D, Lupton H W. Plaque assay for Ebola virus. J Clin Microbiol. 1981;13:791–793. doi: 10.1128/jcm.13.4.791-793.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10a.National Research Council. Guide for the care and use of laboratory animals. Washington, D.C.: National Research Council; 1996. [Google Scholar]
- 11.Parker K C, Bednarek M A, Coligan J E. Scheme for ranking potential HLA A2 binding peptides based on independent binding of individual peptide side chains. J Immunol. 1994;152:163–175. [PubMed] [Google Scholar]
- 12.Pushko P, Bray M, Ludwig G V, Parker M, Schmaljohn A, Sanchez A, Jahrling P B, Smith J F. Recombinant RNA replicons derived from attenuated Venezuelan equine encephalitis virus protect guinea pigs and mice from Ebola hemorrhagic fever virus. Vaccine. 2000;19:142–153. doi: 10.1016/s0264-410x(00)00113-4. [DOI] [PubMed] [Google Scholar]
- 13.Pushko P, Parker M, Geisbert J, Negley D, Schmaljohn A, Sanchez A, Jahrling P B, Smith J F. Venezuelan equine encephalitis virus replicon vector: immunogenecity studies with Ebola NP and GP genes in guinea pigs. In: Brown F, Burton D, Doherty P, Mekalanos J, Norrby E, editors. Vaccines 97. Cold Spring Harbor, N.Y: Cold Spring Harbor Laboratory Press; 1997. pp. 253–258. [Google Scholar]
- 14.Pushko P, Parker M, Ludwig G V, Davis N L, Johnston R E, Smith J F. Replicon-helper systems from attenuated Venezuelan equine encephalitis virus: expression of heterologous genes in vitro and immunization against heterologous pathogens in vivo. Virology. 1997;239:389–401. doi: 10.1006/viro.1997.8878. [DOI] [PubMed] [Google Scholar]
- 15.Rammensee H G, Bachmann J, Stevanovic S. MHC ligands and peptide motifs. Austin, Tex: Landes Bioscience; 1997. [Google Scholar]
- 16.Rao M, Matyas G R, Grieder F, Anderson K, Jahrling P B, Alving C R. Cytotoxic T lymphocytes to Ebola Zaire virus are induced in mice by immunization with liposomes containing lipid A. Vaccine. 1999;17:2991–2998. doi: 10.1016/s0264-410x(99)00170-x. [DOI] [PubMed] [Google Scholar]
- 17.Stevanovic S, Schild H. Quantitative aspects of T cell activation—peptide generation and editing by MHC class I molecule. Semin Immunol. 1999;11:375–384. doi: 10.1006/smim.1999.0195. [DOI] [PubMed] [Google Scholar]
- 18.Vanderzanden L, Bray M, Fuller D, Roberts T, Custer D, Spik K, Jahrling P, Huggins J, Schmaljohn A, Schmaljohn C. DNA vaccines expressing either the GP or NP genes of Ebola virus protect mice from lethal challenge. Virology. 1998;246:134–144. doi: 10.1006/viro.1998.9176. [DOI] [PubMed] [Google Scholar]
- 19.Whitton J L, Tishon A, Lewicki H, Gebhard J, Cook T, Salvato M, Joly E, Oldstone M B. Molecular analysis of a five-amino-acid cytotoxic T-lymphocyte (CTL) epitope: an immunodominant region which induces nonreciprocoal CTL cross-reactivity. J Virol. 1989;63:4303–4310. doi: 10.1128/jvi.63.10.4303-4310.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wilson J A, Hevey M, Bakken R, Guest S, Bray M, Schmaljohn A L, Hart M K. Epitopes involved in antibody-mediated protection from Ebola virus. Science. 2000;287:1664–1666. doi: 10.1126/science.287.5458.1664. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization. Ebola haemorrhagic fever in Zaire, 1976. Report of an international commission. Bull W H O. 1978;56:271–293. [PMC free article] [PubMed] [Google Scholar]
- 22.Xu L, Sanchez A, Yang Z-Y, Zaki S R, Nabel E G, Nichol S T, Nabel G J. Immunization for Ebola virus infection. Nat Med. 1998;4:37–42. doi: 10.1038/nm0198-037. [DOI] [PubMed] [Google Scholar]