Abstract
AIM
To present a technique of transcapsular scleral fixation of the standard capsular tension ring (CTR) through equatorial capsulotomy and in-the-bag intraocular lens (IOL) implantation in subluxated lenses.
METHODS
This retrospective consecutive case series included patients with subluxated lenses by more than 180 degrees who underwent lens extraction, transcapsular scleral fixation of the standard CTR through equatorial capsulotomy, in-the-bag IOL implantation and with at least 6mo follow-up. Preoperative and postoperative best corrected visual acuity (BCVA), intraocular pressure (IOP), complications, and postoperative IOL tilt and decentration were recorded.
RESULTS
Nine eyes of 7 patients with a mean follow-up of 11.0±3.7mo were included in this study. The BCVA was significantly improved from 0.64±0.22 logMAR preoperatively to 0.21±0.19 logMAR postoperatively (P<0.001). The IOP was within the normal range postoperatively. The mean tilt of the IOL was 4.30°±2.31° (range, 1.0° to 8.9°) and the mean decentration of the IOL was 0.37±0.12 mm (range, 0.14 to 0.50 mm). No visually threatened intraoperative and postoperative complications were detected during the follow-up period.
CONCLUSION
This is a safe and effective surgical technique for managing patients with severely subluxated lenses. It has achieved favorable outcomes with fewer surgical manipulations and less need for advanced capsular support devices.
Keywords: lens subluxation, surgical technique, capsular tension ring, transcapsular scleral fixation, in-the-bag IOL implantation
INTRODUCTION
Lens subluxation is the displacement of the lens from its anatomical location caused by zonular weakness or defect, which is always associated with several conditions such as Marfan syndrome, Weill-Marchesani syndrome, homocystinuria, trauma as well as iatrogenic zonular damage[1]–[4].
Surgical strategies vary according to the degree of lens subluxation. The standard capsular tension ring (CTR), designed to provide circumferential support at the capsular equator, is sufficient when the zonular abnormality is less than 120 degrees. But it may not achieve adequate stabilization of the capsular bag and the intraocular lens (IOL) in more severe cases. The current approaches to managing them can broadly fall into two categories, one is to remove the subluxated lens followed by IOL extracapsular fixation, including anterior or posterior iris-claw IOL implantation[5]–[6], iris-sutured IOL implantation[7], and transscleral or intrascleral IOL fixation[8]–[9]. The other is to recentralize the capsular bag by advanced capsular support devices, such as modified CTR (MCTR)[10], capsular tension segment (CTS)[11], capsular anchor[12], capsular hook[13], and endocapsular hemi-ring segment[14], which have attracted more attention because of the advantages of preserving the capsular bag and reducing the posterior segmental disturbance. However, those devices are still difficult to access at the hospitals in grassroots and backward areas where those are not available.
In this study, we reported a safe and effective surgical technique of transcapsular scleral fixation of the standard CTR through equatorial capsulotomy, enabling in-the-bag IOL implantation for severely subluxated lenses. It has achieved reliable short-term results with fewer surgical manipulations and less need for advanced capsular support devices.
PARTICIPANTS AND METHODS
Ethical Approval
This retrospective consecutive case series study adhered to the Declaration of Helsinki and was approved by the Institutional Ethics Committee of the Eye Hospital of Wenzhou Medical University (ID H2023-048-X-02-01). Informed consent was obtained from the patients or their guardians.
Study Participants
This study included patients with subluxated lenses who underwent lens extraction, capsular bag fixation, and in-the-bag IOL implantation at the Eye Hospital of Wenzhou Medical University between February 2022 and May 2023. The inclusion criteria were patients with a lens dislocated by more than 180 degrees, and the etiology was traumatic or spontaneous. The exclusion criteria were patients with eye diseases that needed to be treated besides lens subluxation, such as retinal detachment, and postoperative follow-up of less than 6mo.
Surgical Technique
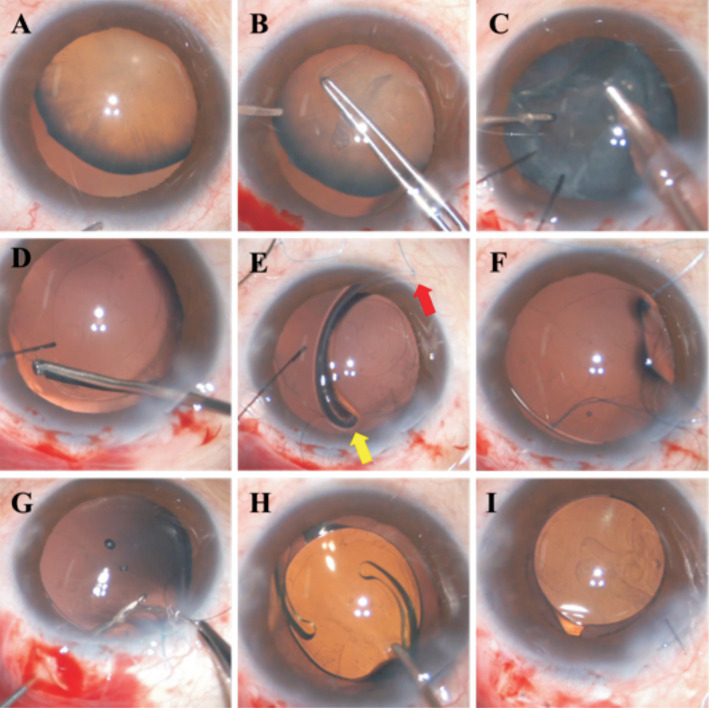
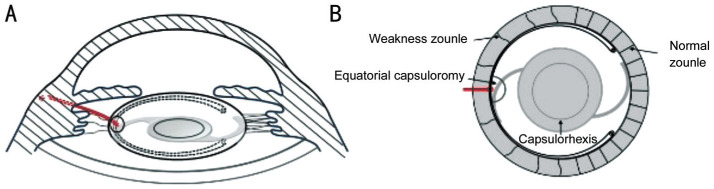
All the surgeries were performed by the same senior surgeon (Zhao YE). Surgical procedures were performed as follows: a clear corneal incision was made followed by the injection of the ophthalmic viscoelastic device (OVD) to maintain the anterior chamber space (Figure 1). A vitrectomy, if required, was performed to remove vitreous prolapsing into the anterior chamber from the area of zonular dialysis. A continuous curvilinear capsulorhexis was performed gently and capsular hooks were applied to centralize and stabilize the capsular bag. Hydrodissection and hydrodelineation were performed followed by phacoemulsification and cortex aspiration. The OVD was further injected to inflate the capsular bag and the capsular hooks were loosened. A 23-gauge vitrector or capsulorhexis forceps was then introduced into the capsular bag through the capsulorhexis to create a 1.5-2 mm diameter capsulotomy at the capsular equator toward the middle location of zonular abnormalities. A double-strand 8-0 polypropylene suture was attached at the middle point of a standard CTR and another guiding suture was temporarily threaded through the leading eyelet of the CTR. Then delivered the CTR into the capsular bag and aligned the middle point of it to the equatorial capsulotomy made earlier, during this process, pulled the leading eyelet centrally by tightening the guiding suture to avoid the edge of the CTR penetrating through the equatorial capsulotomy. A hollow needle was passed through the scleral pocket bed 2 mm posterior to the limbus at the middle location of zonular abnormalities and entered into the capsular bag through the equatorial capsulotomy. Then introduced the needle of the 8-0 polypropylene suture into the hollow needle through the capsulorhexis and passed it through the scleral pocket bed with the guidance of the hollow needle. Adjusted the suture to provide perfect centration of the capsular bag, after which the CTR was sutured to the sclera followed by conjunctival closure with a 10-0 nylon suture. A foldable IOL was, thereafter, implanted into the capsular bag. Residual OVD was removed and antibiotics were applied. All patients were treated postoperatively with topical steroids to reduce inflammation. Figure 2 demonstrated the schematic figure of the postoperative anterior segment.
Figure 1. Intraoperative view of the surgical procedures.
A: A subluxated lens with a zonular abnormality of about 180 degrees; B: Continuous curvilinear capsulorhexis was performed gently; C: Phacoemulsification and cortex aspiration were performed with the aid of capsular hooks; D: A 23-gauge vitrector was introduced into the capsular bag through the capsulorhexis to create a 1.5-2 mm diameter capsulotomy at the capsular equator toward the middle location of the zonular abnormality; E: Attached a double-strand 8-0 polypropylene suture (red arrow) at the middle point of a standard CTR and temporarily threaded another guiding suture (yellow arrow) through the leading eyelet of the CTR; F: Delivered the CTR into the capsular bag and aligned the middle point of it to the equatorial capsulotomy made earlier; G: Introduced the needle of the 8-0 polypropylene suture into the hollow needle through the capsulorhexis and passed it through the scleral pocket bed with the guidance of the hollow needle; H: A foldable IOL was implanted into the capsular bag; I: Well-positioned IOL at the end of the surgery. CTR: Capsular tension ring; IOL: Intraocular lens.
Figure 2. Schematic figure of the postoperative anterior segment.
A: Side view of the postoperative anterior segment; B: Top view of the postoperative anterior segment.
Preoperative and Postoperative Evaluation
All patients underwent an ophthalmologic examination including slit-lamp examination, best corrected visual acuity (BCVA), intraocular pressure (IOP) at preoperative and postoperative visits. Intraoperative and postoperative complications were recorded. IOL tilt and decentration were identified by slit lamp examination and swept-source optic coherence tomography (SS-OCT; CASIA2; Tomey Corporation, Nagoya, Japan) relative to the corneal topographic axis[15].
Statistical Analysis
The continuous variables were represented by mean±standard deviation (SD) and the categorical variables were expressed by counts and percentages. Wilcoxon signed-rank test was used to compare preoperative and postoperative results. All the statistical analyses were conducted using SPSS software (version 26.0, IBM Inc., Armonk, NY, USA).
RESULTS
Patient demographics and clinical data were presented in Table 1. Nine eyes of 7 patients were included in the study (4 right eyes and 5 left eyes). The etiologies were congenital (n=4) and trauma (n=5). All of them had at least 180° of zonular dialysis (range 180° to 240°). The mean preoperative logMAR BCVA was 0.64±0.22 (range, 0.40 to 1.00). One eye was concurrent with vitreous prolapse and one with IOP rise.
Table 1. Patient demographics and clinical data.
| Case No. | Gender | Eye | Age (y) | Etiology | Area of subluxation (°) | Preop. BCVA (logMAR) | Preop. IOP (mm Hg) | Associated ocular condition |
| 1 | Female | Left | 62 | Trauma | 180 | 0.70 | 26.9 | IOP rise |
| 2 | Male | Right | 58 | Trauma | 210 | 0.52 | 17.4 | None |
| 3 | Female | Left | 60 | Trauma | 180 | 1.00 | 18.0 | Vitreous prolapse |
| 4 | Female | Left | 72 | Trauma | 180 | 0.52 | 15.6 | None |
| 5 | Male | Right | 63 | Trauma | 210 | 1.00 | 13.7 | None |
| 6 | Male | Right | 7 | Congenital | 240 | 0.52 | 11.3 | None |
| 7 | Male | Left | 7 | Congenital | 240 | 0.40 | 12.9 | None |
| 8 | Male | Right | 8 | Congenital | 210 | 0.52 | 18.5 | None |
| 9 | Male | Left | 8 | Congenital | 210 | 0.60 | 19.7 | None |
BCVA: Best corrected visual acuity; logMAR: Logarithm of the minimum angle of resolution; IOP: Intraocular pressure.
Follow-up data were presented in Table 2. The mean follow-up duration was 11.0±3.7mo (range, 6 to 16mo). There was a significant postoperative improvement in logMAR BCVA (0.21±0.19, P<0.001). The IOP was within the normal range at all postoperative visits. No eyes developed optic visible IOL dislocation throughout the follow-up period. The mean tilt of the IOL was 4.30°±2.31° (range, 1.0° to 8.9°) and the mean decentration of the IOL was 0.37±0.12 mm (range, 0.14 to 0.50 mm) at the final visit.
Table 2. Follow-up data of patients.
| Case No. | Etiology | Area of subluxation (°) | Follow-up (mo) | BCVA (logMAR) | IOP (mm Hg) | Associated ocular condition |
| 1 | Trauma | 180 | 11 | 0.52 | 15.4 | None |
| 2 | Trauma | 210 | 8 | 0.00 | 14.4 | None |
| 3 | Trauma | 180 | 7 | 0.10 | 16.8 | None |
| 4 | Trauma | 180 | 9 | 0.10 | 15.1 | None |
| 5 | Trauma | 210 | 6 | 0.52 | 18.3 | None |
| 6 | Congenital | 240 | 13 | 0.10 | 14.2 | None |
| 7 | Congenital | 240 | 13 | 0.10 | 13.4 | None |
| 8 | Congenital | 210 | 16 | 0.22 | 12.6 | None |
| 9 | Congenital | 210 | 16 | 0.22 | 13.1 | Mild capsular wrinkling |
BCVA: Best corrected visual acuity; logMAR: Logarithm of the minimum angle of resolution; IOP: Intraocular pressure.
There were no intraoperative complications in all cases. Mild capsular wrinkling was observed in one case seven months postoperatively without significant visual influence. No vitreous hemorrhage, capsular rupture, suture breakage, or retinal detachment was detected during the follow-up period.
DISCUSSION
Surgical management for subluxated lenses presents surgeons with numerous challenges, especially in cases with extensive insufficient zonular support. Various IOL suspension strategies have been published recently[16]–[17], those operations were still sophisticated and prone to result in many complications due to the posterior segmental disturbance. With the aim of reconstructing the capsular bag-zonules diaphragm, lots of advanced capsular support devices also have been applied[11]–[14]. However, those devices are still difficult to access and popularized in many areas. Under the circumstance, we described a new standard CTR transcapsular scleral fixation technique. To the best of our knowledge, this is the first study reporting the surgical procedures to fixate the capsular bag through equatorial capsulotomy with a standard CTR followed by IOL in-the-bag implantation in subluxated lenses with severe zonular abnormality.
In the current study, we reported favorable outcomes from 9 eyes with moderate or severe subluxated lenses undergoing lens extraction, capsular bag fixation, and in-the-bag IOL implantation. This technique recentralizes and stabilizes the dislocated capsular bag by transcapsular scleral fixation of the standard CTR through equatorial capsulotomy, and reduces the posterior segmental disturbance. The BCVA of all eyes in our study improved and there were no visually threatened complications were detected during the follow-up period. The mean tilt and decentration of the IOL in our study were both less than those in a recent comparative study of transscleral sutured IOL fixation and sutureless flanged IOL fixation for the management of lens subluxation using CASIA2 (tilt: 8.20°±3.76° vs 8.22°±4.11°; decentration: 0.59±0.33 vs 0.59±0.39)[18]. Our results were also within the range of previous findings following uneventful cataract surgery[15],[19]. Although different studies could not be compared directly, the results suggest that our technique may provide more IOL stability.
Same with other advanced capsular support devices, our technique retained the capsular bag and the vitreous was therefore largely undisturbed or otherwise intact, decreasing the incidence of postoperative posterior segment complications such as vitreous hernia, cystoid macular edema and retinal detachment[20]–[21]. Besides, compared with IOL extracapsular fixation, IOL in-the-bag implantation was more physiologic with less postoperative IOL decentration or tilt[22] and provided less variations in predicted refraction[23]. Other than some devices designed to stabilize the capsular bag by holding the capsulorhexis rim such as capsular anchor, capsular hook, endocapsular hemi-ring segment and T-shaped capsule stabilization hook[12]–[14] and the technique developed by Cionni and Osher[24] passing the suture attached at the standard CTR over the capsulorhexis to the scleral, we stitched the suture into the sclera directly from the CTR exposed at the equatorial capsulotomy, which simulated the biomechanics of the zonular fibers without distorting the configuration of the capsulorhexis, contributing to the postoperative IOL stability[25]. Besides, our technique could also avoid some infrequent complications caused by the fixation eyelets in MCTR or CTS, which were placed between the under surface of iris and the anterior capsule. An overtight scleral suture may lead the fixation eyelets to contact and irritate the ciliary process, which could increase aqueous humor secretion and result in intraocular hypertension[26]. Besides, the fixation eyelets may also chafe the undersurface of the iris, resulting in pigment dispersion and chronic uveitis[27]. Moreover, the fixation eyelets could lift the anterior capsule away from the surface of the IOL, which facilitated lens epithelial cells migration into this zone[28].
There are some cautions when performing this surgical technique. First, we attempted to create the equatorial capsulotomy by capsulorhexis forceps in our previous cases and found it hard to manipulate the size and roundness. In the current study, we modified this procedure by using a 23-gauge vitrector, this manipulation turned out to be more controllable with less operative time and better controllability and the rim of the equatorial capsulotomy was invisible through dilated pupils postoperatively (Figure 3). Second, given that suture breakage was one of the severe complications, we used the 8-0 polypropylene suture in this technique, which was thicker and had higher tensile strength than the 10-0 and 9-0 polypropylene suture reducing the risk of suture breakage. It should be attached at the middle point of the CTR and aligned toward the middle location of zonular abnormalities, while a significant malposition may cause uneven force distribution. Third, a guiding suture was temporarily threaded through the leading eyelet of the CTR, we could pull the leading eyelet centrally by tightening it to avoid the edge of the CTR penetrating through the equatorial capsulotomy and entanglement occurrence. Fourth, after insertion of the CTR, the attached suture should be performed with suitable tension to center the capsular bag according to the strength of the residual suspensory ligament. Loose traction could cause attachment slippage, while excessive traction could cause damage to the residual zonular fibers. Nevertheless, caution should be taken during the operation as the equatorial capsulotomy might extend, in which condition this technique would need to be abandoned.
Figure 3. Postoperative anterior segment photographs and SS-OCT examination.
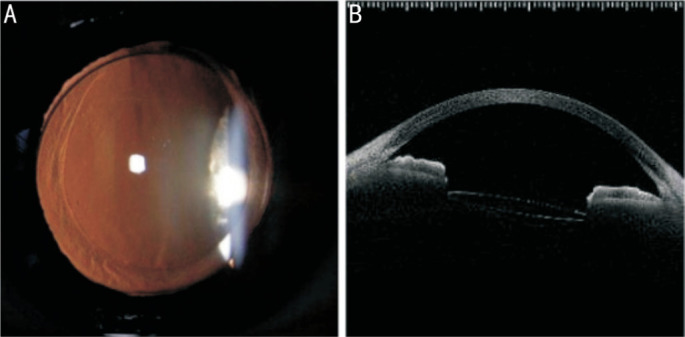
A: Postoperative anterior segment photograph; B: Postoperative SS-OCT examination. SS-OCT: Swept-source optic coherence tomography.
The limitation of this study is the relatively small sample size and short-term observation. Besides, zonulopathy is progressive in some systemic diseases such as pseudoexfoliation syndrome, Marfan syndrome, and Weill-Marchesani syndrome, we should be cautious with the technique in those conditions, especially for young patients. More quadrant fixation with this technique in those patients was worth exploring in the future.
In summary, we presented a safe and effective surgical technique for managing patients with moderate or severe subluxated lenses. It has achieved favorable outcomes with fewer surgical manipulations and less need for advanced capsular support devices.
Footnotes
Foundation: Supported by Wenzhou Basic Research Foundation (No.2024Y1244).
Conflicts of Interest: Li HZ, None, Yang FM, None, Zhu ZH, None, Zhao YY, None, Chang PJ, None, Zhao YE, None.
REFERENCES
- 1.Kinori M, Wehrli S, Kassem IS, Azar NF, Maumenee IH, Mets MB. Biometry characteristics in adults and children with Marfan syndrome: from the Marfan eye consortium of Chicago. Am J Ophthalmol. 2017;177:144–149. doi: 10.1016/j.ajo.2017.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al Motawa MNA, Al Shehri MSS, Al Buali MJ, Al Agnam AAM. Weill-marchesani syndrome, a rare presentation of severe short stature with review of the literature. Am J Case Rep. 2021;22:e930824. doi: 10.12659/AJCR.930824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rahman M, Sharma M, Aggarwal P, Singla S, Jain N. Homocystinuria and ocular complications - a review. Indian J Ophthalmol. 2022;70(7):2272–2278. doi: 10.4103/ijo.IJO_309_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ke G, Zhou E, Zhu K, Wei Y, Wang Z, Jia Y, Wang S, Gu Y. Retinal break associated with traumatic lens dislocation or subluxation requiring vitrectomy. Graefes Arch Clin Exp Ophthalmol. 2020;258(3):693–697. doi: 10.1007/s00417-019-04530-9. [DOI] [PubMed] [Google Scholar]
- 5.Güell JL, Verdaguer P, Elies D, Gris O, Manero F, Mateu-Figueras G, Morral M. Secondary iris-claw anterior chamber lens implantation in patients with aphakia without capsular support. Br J Ophthalmol. 2014;98(5):658–663. doi: 10.1136/bjophthalmol-2013-304035. [DOI] [PubMed] [Google Scholar]
- 6.Gonnermann J, Maier AK B, Klamann M, Brockmann T, Bertelmann E, Joussen A, Torun N. Posterior iris-claw aphakic intraocular lens implantation and Descemet membrane endothelial keratoplasty. Br J Ophthalmol. 2014;98:1291–1295. doi: 10.1136/bjophthalmol-2014-304948. [DOI] [PubMed] [Google Scholar]
- 7.Hirashima DE, Soriano ES, Meirelles RL, Alberti GN, Nosé W. Outcomes of iris-claw anterior chamber versus iris-fixated foldable intraocular lens in subluxated lens secondary to Marfan syndrome. Ophthalmology. 2010;117(8):1479–1485. doi: 10.1016/j.ophtha.2009.12.043. [DOI] [PubMed] [Google Scholar]
- 8.Si SC, Zhang JH. An electrocoagulation fixation technique for one-piece intraocular lens scleral flapless fixation with sutures without knots. Retina. 2023;43(12):2068–2071. doi: 10.1097/IAE.0000000000003756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Czajka MP, Frajdenberg A, Stopa M, Pabin T, Johansson B, Jakobsson G. Sutureless intrascleral fixation using different three-piece posterior chamber intraocular lenses: a literature review of surgical techniques in cases of insufficient capsular support and a retrospective multicentre study. Acta Ophthalmol. 2020;98(3):224–236. doi: 10.1111/aos.14307. [DOI] [PubMed] [Google Scholar]
- 10.Cai L, Han XY, Jiang YX, Qiu XD, Qian DJ, Lu Y, Yang J. Three-year outcomes of cionni-modified capsular tension ring implantation in children under 8 years old with ectopia lentis. Am J Ophthalmol. 2021;224:74–83. doi: 10.1016/j.ajo.2020.11.011. [DOI] [PubMed] [Google Scholar]
- 11.Chang-Sotomayor M, Gϋell JL, de Rojas Silva MV, Corretger X, Bandeira F, Mendez-Mourelle A, Veillet LZ, Adán A, Figueras-Roca M. Comparison of intraocular lens tilt after capsular sutured scleral fixation with capsular segments versus uneventful cataract surgery. Eur J Ophthalmol. 2024;34(5):1450–1457. doi: 10.1177/11206721231223997. [DOI] [PubMed] [Google Scholar]
- 12.Goldfeather Ben-Zaken S, Kleinmann G. Results of using the AssiAnchor capsule device for subluxated crystalline lenses. Indian J Ophthalmol. 2021;69(12):3511–3514. doi: 10.4103/ijo.IJO_576_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ou ZM, Zhao PQ, Zhang Q, Jin HY. Intrascleral fixation of implantable polypropylene capsular hook(s): a sutureless technique to fixate the capsular bag for intraocular lens implantation in subluxated lenses. Retina. 2019;39Suppl 1:S33–S38. doi: 10.1097/IAE.0000000000002425. [DOI] [PubMed] [Google Scholar]
- 14.Jacob S, Agarwal A, Agarwal A, Sathish K, Prakash G, Kumar DA. Glued endocapsular hemi-ring segment for fibrin glue-assisted sutureless transscleral fixation of the capsular bag in subluxated cataracts and intraocular lenses. J Cataract Refract Surg. 2012;38(2):193–201. doi: 10.1016/j.jcrs.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 15.Tan X, Liu Z, Chen X, Zhu Y, Xu J, Qiu X, Yang G, Peng L, Gu X, Zhang J, Luo L, Liu Y. Characteristics and risk factors of intraocular lens tilt and decentration of phacoemulsification after pars plana vitrectomy. Transl Vis Sci Technol. 2021;10(3):26. doi: 10.1167/tvst.10.3.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu ZZ, Liu CJ, Xu YH, Dong W, Chen ZM. Modified technique for scleral-sutured fixation with the double knots technique for posterior chamber intraocular lens: short-term observation. J Ophthalmol. 2021;2021:6697230. doi: 10.1155/2021/6697230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen SJ, Yuan GQ, Zhu WT, Wang Q, Shi WY, Zhang JJ. Four-point scleral fixation of an akreos adapt AO intraocular lens using double-strand 9-0 polypropylene suture. Retina. 2023;43(12):2059–2063. doi: 10.1097/IAE.0000000000003601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cui Y, Li QY, Shi XY, Zhou D. A comparative study of transscleral sutured intraocular lens fixation and sutureless flanged intraocular lens fixation. BMC Ophthalmol. 2023;23(1):23. doi: 10.1186/s12886-023-02782-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gu X, Chen X, Yang G, Wang W, Xiao W, Jin G, Wang L, Dai Y, Ruan X, Liu Z, Luo L, Liu Y. Determinants of intraocular lens tilt and decentration after cataract surgery. Ann Transl Med. 2020;8(15):921. doi: 10.21037/atm-20-1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fan F, Luo Y, Liu X, Lu Y, Zheng TY. Risk factors for postoperative complications in lensectomy-vitrectomy with or without intraocular lens placement in ectopia lentis associated with Marfan syndrome. Br J Ophthalmol. 2014;98(10):1338–1342. doi: 10.1136/bjophthalmol-2013-304144. [DOI] [PubMed] [Google Scholar]
- 21.Wang AJ, Fan Q, Jiang YX, Lu Y. Primary scleral-fixated posterior chamber intraocular lenses in patients with congenital lens subluxation. BMC Ophthalmol. 2021;21(1):411. doi: 10.1186/s12886-021-02182-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu ZZ, Lin HT, Jin GM, et al. In-the-bag versus ciliary sulcus secondary intraocular lens implantation for pediatric aphakia: a prospective comparative study. Am J Ophthalmol. 2022;236:183–192. doi: 10.1016/j.ajo.2021.10.006. [DOI] [PubMed] [Google Scholar]
- 23.Shen JF, Deng S, Hammersmith KM, Kuo AN, Li JY, Weikert MP, Shtein RM. Intraocular lens implantation in the absence of zonular support: an outcomes and safety update: a report by the American Academy of Ophthalmology. Ophthalmology. 2020;127(9):1234–1258. doi: 10.1016/j.ophtha.2020.03.005. [DOI] [PubMed] [Google Scholar]
- 24.Cionni RJ, Osher RH. Management of profound zonular dialysis or weakness with a new endocapsular ring designed for scleral fixation. J Cataract Refract Surg. 1998;24(10):1299–1306. doi: 10.1016/s0886-3350(98)80218-6. [DOI] [PubMed] [Google Scholar]
- 25.Kránitz K, Miháltz K, Sándor GL, Takacs A, Knorz MC, Nagy ZZ. Intraocular lens tilt and decentration measured by scheimpflug camera following manual or femtosecond laser–created continuous circular capsulotomy. J Refract Surg. 2012;28(4):259–263. doi: 10.3928/1081597X-20120309-01. [DOI] [PubMed] [Google Scholar]
- 26.Lin HS, Zhou GM, Zhang SD, Huang F, Liang YB. One-year outcome of low dose laser cyclophotocoagulation for capsular tension ring-induced malignant glaucoma: a case report. Medicine (Baltimore) 2020;99(6):e18836. doi: 10.1097/MD.0000000000018836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Menapace R, Findl O, Georgopoulos M, Rainer G, Vass C, Schmetterer K. The capsular tension ring: designs, applications, and techniques. J Cataract Refract Surg. 2000;26(6):898–912. doi: 10.1016/s0886-3350(00)00446-6. [DOI] [PubMed] [Google Scholar]
- 28.Moreno-Montañés J, Sainz C, Maldonado MJ. Intraoperative and postoperative complications of Cionni endocapsular ring implantation. J Cataract Refract Surg. 2003;29(3):492–497. doi: 10.1016/s0886-3350(02)01604-8. [DOI] [PubMed] [Google Scholar]