Abstract
To reduce long hospitalization durations and the high rate of compulsory psychiatric hospitalization in Korea, a revision of the Mental Health Welfare law was passed and implemented in 2017. This study quantitatively analyzed changes in hospitalization use behavior of patients with psychotic and mood disorders after revision of the Mental Health Welfare law in South Korea. The intervention time was June 2017. Data from the National Health Insurance claims were used. Participants were all patients with hospital visits involving psychotic disorders and mood disorders. We used the interrupted time-series method with segmented regression. In patients with psychotic disorders, admission decreased after the law revision. The average inpatient length of hospitalization decreased immediately after the revision, leading to a long-term decrease. Emergency room visits increased following the revision, and admission through the emergency room also increased. In patients with mood disorders, admission decreased both immediately and over the long-term after the revision. Additionally, the average inpatient length of hospitalization decreased immediately, with no significant change observed in the long term. Emergency room visits increased following the revision. Following the law revision, patients with psychiatric disorders showed a decrease in hospital admissions and length of hospital stay. However, an increasing trend in emergency room visits was identified, suggesting an increase in crisis situations. These findings indicate the need to reduce admissions and length of hospitalization while also protecting the rights of patients with psychiatric disorders. System improvements are thus necessary to prevent an increase in crisis situations and ensure appropriate treatment.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-80557-1.
Keywords: Mental health and welfare law, Patients with psychiatric disorders, Psychiatric crisis
Subject terms: Psychiatric disorders, Health policy
Introduction
The Mental Health and Welfare Act in South Korea was enacted to allow individuals with mental illness to receive proper treatment and prevent infringement of basic rights that may occur in the process. In South Korea, health services for individuals with mental illness began in the early 20th century; however, until the 1960s, involuntary institutionalization outside of hospitals was more common1,2. Psychiatrists introduced biological treatment for these patients and moved them from camps to hospitals; however, arguments regarding the human rights of patients are ongoing because of frequent compulsory admissions. The Mental Health Law of Korea was first enacted in 1995, and it allowed patients to receive appropriate treatment and prevented violations of the human rights of patients with psychiatric disorders. After several revisions, the Mental Health Law was completely revised as the Act on the Improvement of Mental Health and the Support for Welfare Services for Mental Patients (Mental Health and Welfare Law) in 2016, and it was implemented on May 30, 2017.
The revision of the Mental Health and Welfare Law was intended to supplement its previous limitations. The length of hospitalization for patients with psychiatric disorders was highest among Organization for Economic Cooperation and Development countries and approximately four times longer than the average3; therefore, the revision attempted to reduce compulsory admissions. Additionally, the Constitutional court decided in 2016 that the law regarding mental health did not conform to the Constitution because the definition of patients with psychiatric disorders is broad, and compulsory admission was decided by only one psychiatrist; therefore, these problems were reflected in the revision4. The definition of patients with psychiatric disorders has evolved, focusing on symptoms and functions rather than on the disease5. Additionally, compulsory admission requires an agreement regarding the diagnosis by two psychiatrists, one of whom must be a psychiatrist at a public hospital. The examination committee, who determined the legitimacy of admission, also reviewed compulsory admission.
This law was evaluated to determine its effect on individuals with mental illness 5 years after its revision and enforcement. In particular, for patients with schizophrenia and affective disorders, who are the main targets for long-term hospitalization, quantitative evaluation of the number of admissions and length of hospitalizations before and after the full law revision is necessary. According to the 2016 national statistics on mental disorders, the lifetime prevalence of schizophrenia spectrum disorders was 0.5%, and the lifetime prevalence of depressive disorders was 5.3%6. These disorders became the primary focus of the legislative amendment. Few previous studies have attempted to evaluate the impact of the Mental Health Law revision; however, those that have relied on statistical yearbooks or aggregated data, limiting their implications as they do not account for individual patient characteristics7,8. Analyzing data at the individual level allows for the inclusion of personal characteristics in the statistical model, which are not captured in aggregated-level or yearbook-based analysis. Therefore, this study aimed to investigate how the full revision of the Mental Health and Welfare Law in 2017 affected medical utilization by patients with psychiatric disorders in South Korea.
Methods
Study population and data
Data analyzed during this study were acquired from the Korean National Health Insurance Sharing Service (NHISS)9–11. The National Health Insurance Service (NHIS) routinely collects all claims data and provides a database for academic investigation and policymaking. The NHIS is the only insurer and covers approximately 97% of the total population of Korea. The claims data of patients receiving medical aid because of low income (approximately 3% of the total population) were also included in the database. We used diagnostic information and inpatient and outpatient utilization data from this database.
To explore the effect of the law revision on healthcare utilization by patients with psychiatric disorders, we targeted patients with severe symptoms that usually result in compulsory psychiatric department admission. We chose the psychiatric population by using the diagnostic codes defined by the International Classification of Disease, 10th revision (ICD-10). As psychotic and mood disorders constitute the majority of involuntary admissions, we selected patients with these conditions as our inclusion criteria for the analysis. From the dataset spanning from 2010 to 2021, we excluded data from 2010 to eliminate episodes involving individuals already hospitalized before the study period. Additionally, to avoid the confounding effects of the coronavirus disease 2019 pandemic on the evaluation of the impact of the law, we excluded data from 2020. Consequently, we analyzed 39,842,254 episodes, including 592,953 admission episodes and 39,249,301 outpatient episodes, from 2011 to 2019.
Variable of interest
In this study, the variable of interest was revision of the Mental Health and Welfare Law. The Mental Health and Welfare Law was revised on May 29, 2016, and enacted on May 30, 2017. Our analysis included monthly intervals; thus, we designated June 2017 as the time of implementation of the revision to the Mental Health and Welfare Law. Consequently, until May 2017, the intervention variable was coded as “0,” and from June 2017 onward, the intervention variable was coded as “1.”
Dependent variables and covariates
The dependent variables included metrics of healthcare utilization by the study population, such as number of admissions, length of hospitalization, and emergency department (ED) visits. The number of ED visits was defined as the monthly occurrences of psychiatric patients being admitted through the ED to reflect crisis situations. Additionally, the proportion of total hospital admissions that occurred through the ED was used in the analysis.
The independent variables in this study were age group (0–19 years, 20–29 years, 30–39 years, 40–49 years, 50–59 years, 60–69 years, or 70 years or older), sex (male or female), social security status (insurance or medical aid), income level (low, middle, or high), region (metropolitan, city, or rural), disability status (present or absent), and Charlson comorbidity index (low, middle, or high). Disability status in the data indicates whether an individual is registered as having a disability in the national welfare system. To assess patient comorbidities, the Charlson comorbidity index was used, a tool commonly applied in longitudinal studies using administrative data. The index was calculated by weighting scores of 1–6 for 19 comorbid diseases12.
Statistical analysis
The chi-squared test was performed to evaluate differences in the characteristics of the study population before and after the law revision. To evaluate the impact of the law revision, we performed a single interrupted time-series analysis with segmented regression at individual levels13–16. The following equation for interrupted time-series using a generalized estimating equation was used for the individual-level analysis17–19.
 |
In the aforementioned regression equation, “time” represents time on monthly basis, “intervention” is the dummy variable (which assigns a value of 1 if the time was after the law revision), “TAI” indicates the time after intervention (which is the time variable started at the intervention point), “X” indicates the covariate, and “ ” represents the residual error. Regarding the regression coefficients in this model, intercept “
” represents the residual error. Regarding the regression coefficients in this model, intercept “ ” estimates the baseline level of the outcome, “
” estimates the baseline level of the outcome, “ ” estimates the preintervention trend of the outcome, “
” estimates the preintervention trend of the outcome, “ ” estimates the level change after the intervention, thus indicating the immediate effect size of the intervention, and “
” estimates the level change after the intervention, thus indicating the immediate effect size of the intervention, and “ ” estimates the slope change after the intervention.
” estimates the slope change after the intervention.
The results are presented in terms of β coefficients, standard errors, and p-values, with significance considered at p < 0.05. For hospital admissions, ED visits, and readmissions for which a logit link function was used, the β coefficients were presented as exponentiated values. We categorized hospitals into two categories: general hospitals and psychiatric hospitals/clinics. While both types can perform involuntary admissions, psychiatric departments in general hospitals typically handle more cases involving acute conditions and shorter length of hospital stay, whereas psychiatric hospitals/clinics tend to manage more cases involving chronic conditions and longer length of hospital stay. To investigate whether the differences between these hospital types responded distinctively to the legislative amendment, we conducted a subgroup analysis using this classification. To verify the robustness of our results, we conducted a comparative interrupted time-series analysis. Here, the control group included patients with neurosis (ICD-10 F4x), as they were expected to be relatively less affected by the revised law.
Results
A total of 39,842,254 episodes comprised hospital visits involving psychotic and mood disorders as the primary and secondary diagnostic codes. Of these episodes, 592,953 resulted in hospitalizations and 39,249,301 corresponded to outpatient visits (Supplement Table 1). Table 1 shows the mean and standard deviation of dependent variables and the unadjusted differences before and after the law revision. The number of admissions and outpatient visits increased after the law revision, but the average number of inpatient days decreased. The unadjusted analysis revealed that ED visits decreased.
Table 1.
Unadjusted differences in dependent variables before and after the mental health law revision.
| Psychotic disorders | Mood disorders | |||||
|---|---|---|---|---|---|---|
| Before revision | After revision | Difference | Before revision | After revision | Difference | |
| (Mean ± SD) | (Mean ± SD) | (Mean ± SD) | (Mean ± SD) | |||
| Admissions, No. | 2835.89 ± 285.96 | 3105.52 ± 506.31 | 269.62 | 3191.57 ± 221.45 | 3444.35 ± 230.91 | 252.79 |
| Outpatients visits, No. | 81911.23 ± 5349.49 | 97208.9 ± 5127.82 | 15297.67 | 289542.14 ± 23315.89 | 392228.58 ± 35245.41 | 102686.44 |
| Average inpatient Days, Days | 173.24 ± 31.91 | 123.65 ± 19.27 | -49.58 | 53.05 ± 3.8 | 51.37 ± 3.23 | -1.68 |
| ER visits, No. | 998.42 ± 144.65 | 634.94 ± 47.93 | -363.48 | 709.11 ± 74.95 | 688.61 ± 67.55 | -20.49 |
SD standard deviation, ER emergency room.
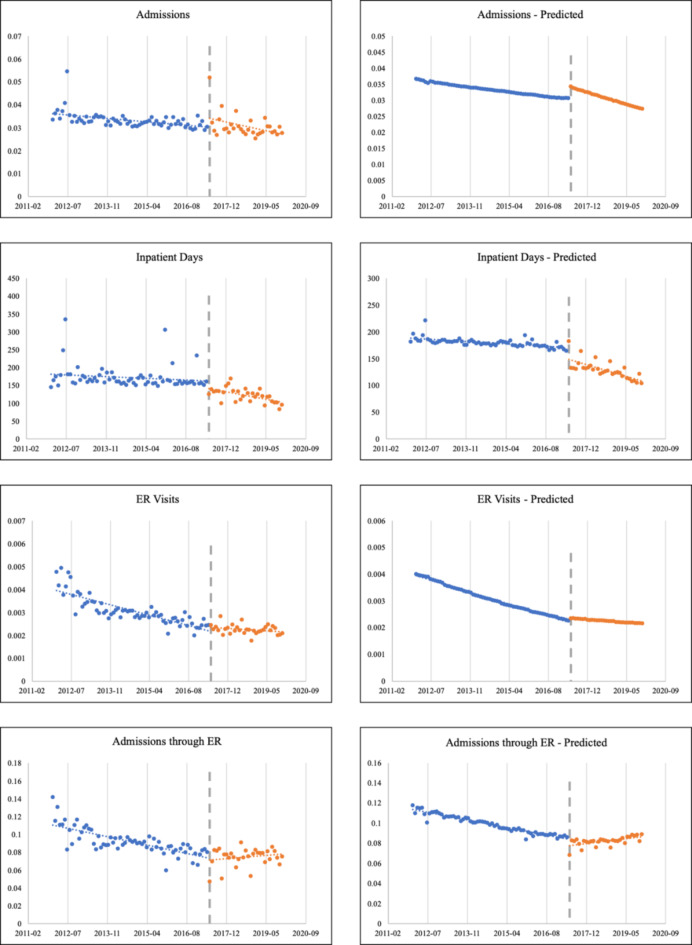
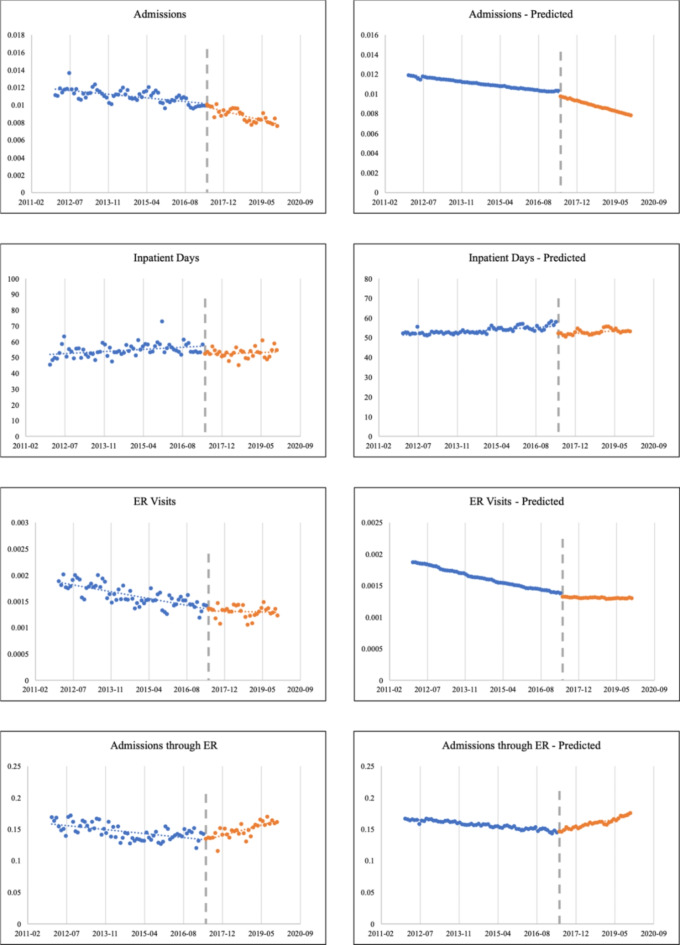
The results of the interrupted time-series analysis using the individual-level data are presented in Table 2. Among the patients with psychotic disorders, the average number of inpatient days decreased immediately after the law revision (β2=–32.7674; p < 0.0001), and the trend also decreased (β3=–0.6055; p < 0.0001). The trend of admissions decreased after the law revision (exp(β3) = 0.9952; p < 0.0001); however, it increased immediately after the revision (exp(β2) = 1.1247; p < 0.0001). The trend of ED visits by the participants increased after the revision (exp(β2) = 1.0056; p < 0.0001), and the trend of admissions through the ED also increased (exp(β2) = 1.0061; p = 0.0009). Among patients with mood disorders, the average number of inpatient days decreased immediately after the law revision (β2=–4.5986; p < 0.0001); however, the trend did not significantly change. The trend of admissions decreased after the law revision (exp(β3) = 0.9959; p < 0.0001) and decreased immediately after the law revision (exp(β2) = 0.9949; p < 0.0001). The trend of ED visits by participants increased after the revision (exp(β2) = 1.0033; p < 0.0001), and the trend of admissions through the ED also increased (exp(β2) = 1.0074; p = 0.0009). The trends of changes in healthcare utilization are presented in Figs. 1 and 2.
Table 2.
Results of segmented regression models estimating the impact of the law revision on healthcare utilization.
| Coefficient | SE | 95% CI | p-value | ||
|---|---|---|---|---|---|
| Psychotic disorders | Admission | ||||
| Baseline trend (exp(β1)) | 0.9973 | 1.0001 | (0.997 to 0.9975) | < 0.0001 | |
| Immediate change (exp(β2)) | 1.1247 | 1.0081 | (1.1069 to 1.1428) | < 0.0001 | |
| Trend change (exp(β3)) | 0.9952 | 1.0004 | (0.9944 to 0.996) | < 0.0001 | |
| Average inpatient days | |||||
| Baseline trend (β1) | -0.2801 | 0.0585 | (-0.3947 to -0.1655) | < 0.0001 | |
| Immediate change (β2) | -32.7674 | 2.7567 | (-38.1705 to -27.3644) | < 0.0001 | |
| Trend change (β3) | -0.6055 | 0.1205 | (-0.8417 to -0.3693) | < 0.0001 | |
| ER visits | |||||
| Baseline trend (exp(β1)) | 0.9914 | 1.0004 | (0.9906 to 0.9922) | < 0.0001 | |
| Immediate change (exp(β2)) | 1.0424 | 1.0297 | (0.9842 to 1.104) | 0.1565 | |
| Trend change (exp(β3)) | 1.0056 | 1.0014 | (1.0029 to 1.0084) | < 0.0001 | |
| Admission Through ER | |||||
| Baseline trend (exp(β1)) | 0.9947 | 1.0006 | (0.9935 to 0.996) | < 0.0001 | |
| Immediate change (exp(β2)) | 0.9591 | 1.0345 | (0.8974 to 1.0249) | 0.2175 | |
| Trend change (exp(β3)) | 1.0061 | 1.0019 | (1.0025 to 1.0097) | 0.0009 | |
| Mood disorders | Admission | ||||
| Baseline trend (exp(β1)) | 0.9973 | 1.0001 | (0.9971 to 0.9975) | < 0.0001 | |
| Immediate change (exp(β2)) | 0.9540 | 1.0076 | (0.9399 to 0.9684) | < 0.0001 | |
| Trend change (exp(β3)) | 0.9959 | 1.0004 | (0.9952 to 0.9966) | < 0.0001 | |
| Average inpatient days | |||||
| Baseline trend (β1) | 0.0318 | 0.0182 | (-0.0038 to 0.0674) | 0.08 | |
| Immediate change (β2) | -4.5986 | 1.1067 | (-6.7677 to -2.4295) | < 0.0001 | |
| Trend change (β3) | 0.0308 | 0.0505 | (-0.0682 to 0.1298) | 0.5419 | |
| ER visits | |||||
| Baseline trend (exp(β1)) | 0.9950 | 1.0003 | (0.9944 to 0.9956) | < 0.0001 | |
| Immediate change (exp(β2)) | 0.9518 | 1.0204 | (0.9148 to 0.9902) | 0.0144 | |
| Trend change (exp(β3)) | 1.0033 | 1.0009 | (1.0015 to 1.0051) | 0.0004 | |
| Admission Through ER | |||||
| Baseline trend (exp(β1)) | 0.9981 | 1.0004 | (0.9974 to 0.9989) | < 0.0001 | |
| Immediate change (exp(β2)) | 0.9980 | 1.0233 | (0.954 to 1.044) | 0.9315 | |
| Trend change (exp(β3)) | 1.0074 | 1.0011 | (1.0052 to 1.0095) | < 0.0001 |
SE standard error, CI confidence interval, ER emergency room.
Fig. 1.
Trends of healthcare utilization variables of patients with psychotic disorders. ER emergency room.
Fig. 2.
Trends of healthcare utilization variables of patients with mood disorders. ER emergency room.
The results of the interrupted time-series analysis sub-grouped by hospital type are presented in Table 3. Among the patients with psychotic disorders, the trend of the number of average inpatient days of both groups decreased after the law revision, but the immediate change was only significant for psychiatric hospitals/clinics (β2=–36.8740; p < 0.0001). The trends of admissions of both groups decreased after the law revision and increased immediately after the law revision. The trend of ED visits increased for psychiatric hospitals/clinics (exp(β3) = 1.0018; p < 0.0001) but decreased for general hospitals (exp(β3) = 0.9951; p = 0.0246). The trend of admissions through the ED also increased for psychiatric hospitals/clinics (exp(β3) = 1.0025; p < 0.0001). For patients with mood disorders, the average number of inpatient days of both groups decreased immediately after the law revision; however, the trend did not significantly change. The trend of admissions of both groups decreased after the law revision. The trend of ED visits in both groups increased, and the immediate change was only significant for psychiatric hospitals/clinics (exp(β2) = 1.0286; p < 0.0001). The trend of admissions through the ED of both hospital groups increased.
Table 3.
Results of segmented regression models estimating the impact of the law revision on healthcare utilization by hospital type.
| General hospital | Psychiatric hospital/Clinic | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Coefficient | SE | 95% CI | p-value | Coefficient | SE | 95% CI | p-value | ||
|
Psychotic disorders |
Admission | ||||||||
| Baseline trend (exp(β1)) | 0.9988 | 1.0004 | (0.9981 to 0.9995) | 0.0010 | 0.9971 | 1.0001 | (0.9968 to 0.9974) | < 0.0001 | |
| Immediate change (exp(β2)) | 1.2396 | 1.0231 | (1.1854 to 1.2963) | < 0.0001 | 1.1079 | 1.0087 | (1.0892 to 1.1269) | < 0.0001 | |
| Trend change (exp(β3)) | 0.9912 | 1.0011 | (0.9891 to 0.9934) | < 0.0001 | 0.9958 | 1.0004 | (0.9949 to 0.9966) | < 0.0001 | |
| Average inpatient days | |||||||||
| Baseline trend (β1) | -0.1981 | 0.0965 | (-0.3871 to -0.009) | 0.0400 | -0.2742 | 0.0654 | (-0.4024 to -0.1461) | < 0.0001 | |
| Immediate change (β2) | -5.1189 | 5.1273 | (-15.1682 to 4.9304) | 0.3181 | -36.8740 | 3.0654 | (-42.8822 to -30.8658) | < 0.0001 | |
| Trend change (β3) | -0.5210 | 0.2269 | (-0.9658 to -0.0762) | 0.0217 | -0.6496 | 0.1335 | (-0.9114 to -0.3879) | < 0.0001 | |
| ER visits | |||||||||
| Baseline trend (exp(β1)) | 0.9996 | 1.0007 | (0.9982 to 1.001) | 0.5851 | 0.9875 | 1.0005 | (0.9865 to 0.9885) | < 0.0001 | |
| Immediate change (exp(β2)) | 1.1445 | 1.0468 | (1.0466 to 1.2518) | 0.0031 | 0.9864 | 1.0390 | (0.915 to 1.0633) | 0.7208 | |
| Trend change (exp(β3)) | 0.9951 | 1.0022 | (0.9908 to 0.9994) | 0.0246 | 1.0120 | 1.0018 | (1.0083 to 1.0156) | < 0.0001 | |
| Admission Through ER | |||||||||
| Baseline trend (exp(β1)) | 1.0021 | 1.0011 | (0.9999 to 1.0043) | 0.0613 | 0.9900 | 1.0009 | (0.9884 to 0.9917) | < 0.0001 | |
| Immediate change (exp(β2)) | 0.9291 | 1.0577 | (0.8323 to 1.0372) | 0.1903 | 0.9621 | 1.0415 | (0.8883 to 1.0421) | 0.3434 | |
| Trend change (exp(β3)) | 1.0010 | 1.0032 | (0.9948 to 1.0072) | 0.7433 | 1.0106 | 1.0025 | (1.0056 to 1.0155) | < 0.0001 | |
|
Mood disorders |
Admission | ||||||||
| Baseline trend (exp(β1)) | 0.9977 | 1.0002 | (0.9972 to 0.9982) | < 0.0001 | 0.9971 | 1.0001 | (0.9968 to 0.9974) | < 0.0001 | |
| Immediate change (exp(β2)) | 1.0781 | 1.0153 | (1.0464 to 1.1106) | < 0.0001 | 0.9125 | 1.0088 | (0.8968 to 0.9284) | < 0.0001 | |
| Trend change (exp(β3)) | 0.9956 | 1.0007 | (0.9942 to 0.997) | < 0.0001 | 0.9971 | 1.0004 | (0.9963 to 0.998) | < 0.0001 | |
| Average inpatient days | |||||||||
| Baseline trend (β1) | -0.0324 | 0.0147 | (-0.0612 to -0.0036) | 0.0275 | 0.0736 | 0.0235 | (0.0276 to 0.1196) | 0.0017 | |
| Immediate change (β2) | -0.7660 | 0.8241 | (-2.3812 to 0.8493) | 0.3527 | -4.8712 | 1.4443 | (-7.7019 to -2.0405) | 0.0007 | |
| Trend change (β3) | -0.0200 | 0.0342 | (-0.0869 to 0.047) | 0.5588 | -0.0715 | 0.0654 | (-0.1997 to 0.0567) | 0.2743 | |
| ER visits | |||||||||
| Baseline trend (exp(β1)) | 0.9960 | 1.0005 | (0.9951 to 0.9969) | < 0.0001 | 0.9938 | 1.0004 | (0.993 to 0.9946) | < 0.0001 | |
| Immediate change (exp(β2)) | 1.0495 | 1.0296 | (0.9912 to 1.1112) | 0.0975 | 0.8738 | 1.0286 | (0.8269 to 0.9235) | < 0.0001 | |
| Trend change (exp(β3)) | 1.0052 | 1.0014 | (1.0025 to 1.0079) | 0.0001 | 1.0069 | 1.0013 | (1.0044 to 1.0094) | < 0.0001 | |
| Admission Through ER | |||||||||
| Baseline trend (exp(β1)) | 0.9990 | 1.0006 | (0.9979 to 1.0001) | 0.0850 | 0.9971 | 1.0005 | (0.996 to 0.9981) | < 0.0001 | |
| Immediate change (exp(β2)) | 0.9977 | 1.0351 | (0.9324 to 1.0675) | 0.9467 | 0.9476 | 1.0322 | (0.8905 to 1.0085) | 0.0903 | |
| Trend change (exp(β3)) | 1.0094 | 1.0017 | (1.0061 to 1.0128) | < 0.0001 | 1.0099 | 1.0015 | (1.007 to 1.0129) | < 0.0001 | |
SE, standard error; CI, confidence interval; ER, emergency room.
The results of the comparative interrupted time-series analysis, using patients with neurotic, stress-related, and somatoform disorders as the control group, are presented in Supplementary Table 2. We observed an increase in ER visits following the policy amendment (exp(β7) = 1.021; p < 0.0001 in patients with psychotic disorder and exp(β7) = 1.022; p < 0.0001 in patients with mood disorder).
Discussion
This study assessed the impact of the comprehensive revision of the Mental Health and Welfare Act on the medical utilization patterns of patients with psychiatric disorders in South Korea. Our findings indicated that after the law revision, the number of hospital admissions and hospital stay durations decreased for patients with psychiatric disorders. However, an upward trend was observed for ED visits.
For patients diagnosed with psychotic disorders, both frequency of hospital admissions and duration of inpatient stays exhibited decreasing trends. This pattern aligned with the findings of previous studies that used the Korean Health Insurance Statistical Yearbook20. However, a transient increase in hospital admissions was observed immediately after the law was implemented. We hypothesized that this finding might be attributable to a transitionary phase during which patients who were discharged after legislation were readmitted. For patients with mood disorders, the analysis did not show a significant decrease in the length of hospitalization; however, the admission trend decreased, mirroring that of patients with psychotic disorders. The reason for the disparity in the admission durations for patients with psychotic and mood disorders was evident when the average hospital stay durations were compared (Table 1). Patients with mood disorders had shorter average hospital stay durations than patients with psychotic disorders, suggesting that the mood disorder group might have been less affected relative to the psychotic disorder group.
An analysis of ED visits by patients with psychotic disorders revealed an increasing trend after the law revision. Although an overall decrease in ED visits was noted after the law was implemented, the decreasing trajectory before the law revision shifted toward an increasing trend after the revision (Fig. 1). Furthermore, the proportion of hospitalized patients admitted through the ED exhibited an even more pronounced increase. A similar pattern was also observed for patients with mood disorders. These findings suggest that the law revision might have caused an increase in ED visits among patients with psychiatric disorders. Among patients who were admitted, the increase in admissions through the ED, as opposed to admissions through outpatient departments, might imply an increase in psychiatric emergencies21. In particular, the increase in admissions through the ED among inpatients could indicate that patients who refuse voluntary admission, ultimately experience psychiatric emergencies that necessitate inpatient care. However, this study did not specify the reasons for ED visits by these patients; therefore, further investigations are warranted. When compared with neurosis patients, as shown in Supplementary Table 2, the trend of ER visits increased after the policy amendment, consistent with the results from the single ITS analysis. Notably, this finding is even more robust given that, in the pre-trend period, the ER visit trend was actually decreasing relative to the control group. This highlights a clear increase in ER visits following the policy change.
A comparison of healthcare utilization patterns based on hospital type showed that the overall impact appeared consistent, but that the amendments had a more pronounced effect on psychiatric hospitals and clinics than on general hospitals. Because the hospital stay durations were historically much longer at psychiatric hospitals and clinics, the decreasing trend after revision became more noticeable. Moreover, the trends related to ED visits at psychiatric hospitals and clinics were more prominently increased. The qualitative differences in mental health services across various types of medical institutions in South Korea might have influenced these outcomes22,23. Although general hospitals typically maintain higher standards of quality, psychiatric hospitals and clinics have a history of prolonged admissions, which previously sparked debates regarding human rights infringements and obstacles to societal reintegration. Because the primary target of the revision was psychiatric hospitals and clinics where long-term admissions were common, it is logical that the effects of the law were more evident in these settings24,25.
Before its revision, the Mental Health Law received much criticism regarding prolonged and unnecessary hospitalizations and consequent violations of the rights and self-determination of patients with mental disorders26–28; therefore, the decreases in the frequency and duration of hospitalization observed during this study align with the objectives of the law revision. However, the increase in ED utilization may indicate an increase in psychiatric emergencies among patients with mental disorders. Furthermore, the increase in admissions via EDs suggests that individuals in need of treatment may not be directly admitted through their outpatient care provider, and that they are more often admitted through the ED after emergency situations. To qualify for admission, a psychiatrist must determine both the necessity of psychiatric hospitalization and the presence of risks for self-harm or harm to others. Deviating from these guidelines can lead to discharge based on the assessment by another psychiatrist or the determination by the Committee for Examination as to Legitimacy of Admission. To minimize administrative and legal liabilities, a more defensive approach when initially admitting patients may be used29,30. Consequently, there might be an increasing tendency to conservatively admit patients who have caused harm or attempted to cause harm to themselves or others.
Furthermore, the crisis situations included in our results are limited to instances where patients with psychiatric disorders visited a medical institution and utilized healthcare services during their crisis. Our findings did not encompass situations involving the risks of self-harm or other harm that materialized into suicides or offenses leading to legal actions, thereby preventing individuals from accessing the healthcare system. Hence, the crisis situations that can be identified from our results might be underestimated. A study that investigated the crime rates of patients with schizophrenia reported an increase in the overall crime and violence rate among these patients after the law revision31. Furthermore, deinstitutionalization efforts in certain countries have inadvertently transitioned patients with psychiatric disorders from hospitals to prisons32. Moreover, studies performed in the United States have highlighted that the largest facility housing patients with psychiatric disorders is a prison, not a mental health institution33.
In this study, we employed the interrupted time-series analysis to assess the impact of the legislative amendment, which allowed for the examination of dependent variables over time and measurement of changes in these variables when a specific event or intervention occurs at a designated point. Interrupted time-series analysis is a widely adopted analytical approach for assessing policy effectiveness. Specifically, when conducting segmented regression within defined intervals, the trend before the policy intervention, the immediate change post-intervention, and the alteration in trends between the pre- and post-policy periods can be statistically verified using this analysis17,34–36. In our research, this method enabled us to track how medical service utilization trends among patients with psychiatric disorders changed over time before the revision of the Mental Health and Welfare Act. Moreover, we could statistically confirm the immediate changes in medical service utilization following the legislative modification and the subsequent trend alterations.
When conducting an interrupted time-series analysis for policy evaluation, aggregated statistical data from the entire population can be used37. As the legal amendment affected all patients with psychiatric disorders, an ecological study using statistical data can provide a broad evaluation of the policy. However, such methods are associated with the risk of ecological fallacy, as individual characteristics are not incorporated into the research design. Therefore, in this study, we utilized individual-level data that reflect personal characteristics and incorporated these data into our statistical model for analysis38. This allowed us to adjust for confounders that might influence an individual’s medical service utilization independently of the legal amendment. This adjustment ensured that we could isolate the effect of the Mental Health and Welfare Act. Additionally, the use of individual characteristics enabled us to conduct subgroup analyses. Particularly, the type of hospital used provided insight into distinct usage patterns, which might significantly affect the overall trends in medical service usage among patients.
Limitations and strengths
This study had some limitations. First, we could not discern the type of hospitalization for the patients. The revision had the most profound impact on involuntary admissions of patients with psychiatric disorders. However, the data utilized did not include information that distinguished whether individual hospitalization episodes were voluntary or involuntary. Thus, we could not confirm whether the law amendment directly influenced the changes in involuntary admissions. Second, we did not include all patients with psychiatric disorders. During this analysis, we only included those with psychotic and mood disorders because these patients are often subjected to involuntary admissions39, making them pertinent subjects for our research. However, significant differences were observed in hospitalization and medical behaviors of patients with substance abuse problems or dementia and those of patients with severe psychiatric disorders. Third, our study utilized segmented regression, but we did not account for seasonality or autocorrelation in our model, which may have influenced the results. However, when we plotted the data, the trend was evident, and we were able to adequately assess the effect of the policy with the existing model. Future studies should incorporate a model that accounts for seasonality and autocorrelation to provide a more refined evaluation of the impact of the policy. Finally, there may have been limitations related to the diagnosis codes. We defined diagnostic groups using the main diagnosis and sub-diagnoses codes of the ICD-10. However, some diagnosis codes might have been used for prescribing medications.
Despite these limitations, our study had several strengths. First, our research utilized health insurance claims data from South Korea. Even though the data provided were a random sampling of nine million individuals rather than of the entire population, it included a significant number of Korean individuals who visited medical institutions because of psychiatric disorders. This finding suggests that the data are sufficiently representative of the entire population for analysis purposes. Furthermore, this research analyzed more than the number and duration of hospitalizations. By including ED visits, we were able to capture the direct effects of the legislative revision and the potential psychiatric crises that might indicate negative effects of the law revision. Such findings can demonstrate unintended consequences or areas of concern associated with the policy change. This comprehensive approach provides a more holistic understanding of the impact of the Mental Health and Welfare Act revision on patients with psychiatric disorders. These results can serve as a foundation for future policy development and ensure that the Mental Health and Welfare Act evolves in a manner that respects human rights, while still safeguarding adequate medical care and support for patients.
Conclusions
After the comprehensive revision of the Mental Health and Welfare Act, decreasing trends were observed in hospital admissions and hospital stay durations of patients with psychiatric disorders, such as psychotic and mood disorders. However, an increasing trend in ED visits was identified, suggesting an increase in crises. Only participants who utilized medical services were included in this study; therefore, the negative effects of the law revision may have been underrepresented. The study results suggest that the legal amendment restricting involuntary admissions has achieved its intended outcomes, while also raising some concerns. Therefore, although it is crucial to reduce the number of admissions and hospital stay durations and protect the rights of patients with psychiatric disorders, system improvements are also needed to prevent an increase in crisis situations among these patients and to ensure appropriate treatment when required. Compared with previous practices, the more complex procedures and potential criminal penalties associated with the admission process may lead to more defensive decisions regarding hospitalization. This approach raises concerns that patients may miss opportunities for timely and safe treatment, both for themselves and those around them. Thus, it may be necessary to re-evaluate and adjust the amended law to ensure that these risks are adequately addressed.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author contributions
HK had full access to all of the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. HK and SHK were responsible for the concept and design of the study. HK was responsible for data acquisition, analysis, and interpretation, and was a major contributor in writing the manuscript. SYJ, SIJ, SKA, ECP contributed to the critical revision of the manuscript for important intellectual content. SIJ and ECP provided administrative, technical, or material support. ECP was responsible for the supervision. All authors read and approved the final manuscript.
Data availability
No data are available because the National Health Information Database can only be accessed by researchers authorized by the Korean National Health Insurance Service. Researchers interested in accessing data should apply to the National Health Insurance Service of Korea. Researchers must first obtain approval from the for their research topic and process. After receiving approval, they can access the National Health Insurance sharing service website (https://nhiss.nhis.or.kr/en/z/a/001/lpza001m01en.do), input the desired research topic, variables, and conditions, and then undergo the NHI review process. Once approved, the database will be made available; however, analysis can only be conducted in designated analysis rooms provided by the NHI.
Declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of Severance Hospital at Yonsei University College of Medicine (Institutional Review Board no. 4-2022-0939). The requirement for informed consent was waived because data of the NHIS national sample cohort do not contain any personally identifiable information.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lee, H. Y. & Past present and future of Korean psychiatry. Psychiatry Invest.1, 13–19 (2004). [Google Scholar]
- 2.Lee, D. A. Study on revision of the mental health welfare act for respect for human rights and deinstitutionalization. KMA Med. Policy Forum16, 75–79 (2019). [Google Scholar]
- 3.OECD Korea’s increase in suicides and psychiatric bed numbers is worrying, says OECD (Organization of Economic Co-operation and development. (2014).
- 4.Case on the. Involuntary hospitalization of mentally ill patients (Constitutional Court of Korea, 2016).
- 5.Go, D. S., Shin, K. C., Paik, J. W., Kim, K. A. & Yoon, S. J. A review of the admission system for mental disorders in South Korea. Int. J. Environ. Res. Public Health17, 9159. 10.3390/ijerph17249159 (2020). PMID:. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Center for Menta. Health The Survey of Mental Disorders in Korea (2017).
- 7.Heo, J., Yoon, N. H., Shin, S., Yu, S. Y. & Lee, M. Effects of the mental health and welfare law revision on schizophrenia patients in Korea: an interrupted time series analysis. Int. J. Mental Health Syst.15, 76. 10.1186/s13033-021-00499-3 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim, A. M. Psychiatric hospitalization in Korea, 2011–2020: the impact of the mental health act revision of 2017 in consideration of the COVID-19 pandemic. Asian J. Psychiatry. 68, 102934. 10.1016/j.ajp.2021.102934 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sang, C. S. et al. Data resource profile: the national health information database of the national health insurance service in South Korea. Int. J. Epidemiol.46, 799–800. 10.1093/ije/dyw253 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National health insurance service. medical aid statistical yearbook (2021). https://www.nhis.or.kr/nhis/together/wbhaec06500m01.do
- 11.National health insurance service, National health insurance statistical. yearbook (2021). https://www.nhis.or.kr/nhis/together/wbhaec06300m01.do
- 12.Sundararajan, V. et al. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J. Clin. Epidemiol.57, 1288–1294 (2004). [DOI] [PubMed] [Google Scholar]
- 13.Bernal, J. L., Cummins, S. & Gasparrini, A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int. J. Epidemiol.46, 348–355 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kontopantelis, E., Doran, T., Springate, D. A., Buchan, I. & Reeves, D. Regression based quasi-experimental approach when randomisation is not an option: interrupted time series analysis. BMJ: Br. Med. J.350, h2750. 10.1136/bmj.h2750 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Linden, A. Conducting interrupted time-series analysis for single- and multiple-group comparisons. Stata J.15, 480–500. 10.1177/1536867x1501500208 (2015). [Google Scholar]
- 16.Habib, N. et al. The use of segmented regression for evaluation of an interrupted time series study involving complex intervention: the CaPSAI project experience. Health Serv. Outcomes Res. Method.21, 188–205. 10.1007/s10742-020-00221-9 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Taljaard, M., McKenzie, J. E., Ramsay, C. R. & Grimshaw, J. M. The use of segmented regression in analysing interrupted time series studies: an example in pre-hospital ambulance care. Implement. Sci.9, 77. 10.1186/1748-5908-9-77 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Christopher, J. W. Z. Generalized estimating equation models for correlated Data: a review with applications. Am. J. Polit. Sci.45, 470–490. 10.2307/2669353 (2001). [Google Scholar]
- 19.Kim, S. H., Park, E. C. & Jang, S. Y. Impact of long-term care insurance on medical costs and utilization by patients with Parkinson’s disease. Soc. Sci. Med.317, 115563. 10.1016/j.socscimed.2022.115563 (2023). [DOI] [PubMed] [Google Scholar]
- 20.Kim, A. M. Psychiatric hospitalization in Korea, 2011–2020: the impact of the mental health act revision of 2017 in consideration of the COVID-19 pandemic. Asian J. Psychiatr. 68, 102934. 10.1016/j.ajp.2021.102934 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hanson, G. D. & Babigian, H. M. Reasons for hospitalization from a psychiatric emergency service. Psychiatr. Q.48, 336–351. 10.1007/BF01562157 (1974). [DOI] [PubMed] [Google Scholar]
- 22.Lee, Y. M. et al. Length of stay in the Mental Health Facilities in Korea. J. KOREAN NEUROPSYCHIATRIC ASSOCIATION. 37, 83–94 (1998). [Google Scholar]
- 23.Cho, S. J., Cho, L. B., Kim, M. J. & Suh T,Jung, Y. I. Length of Stay of Psychiatric Patient and its correlate in Mental Health-related facilities. J. Korean Neuropsychiatr Assoc.45, 372–381 (2006). [Google Scholar]
- 24.Go, D. S., Shin, K. C., Paik, J. W., Kim, K. A. & Yoon, S. J. A review of the Admission System for Mental disorders in South Korea. Int. J. Environ. Res. Public. Health. 17. 10.3390/ijerph17249159 (2020). [DOI] [PMC free article] [PubMed]
- 25.Kim, A. M. Why do psychiatric patients in Korea stay longer in hospital? Int. J. Mental Health Syst.1110.1186/s13033-016-0110-6 (2017). 2. [DOI] [PMC free article] [PubMed]
- 26.Lee, C. H. The Mental Health Law and the Human rights of persons with Mental disorders. Const. Law13, 229–258 (2007). [Google Scholar]
- 27.Lee, C. G., Kim, J. G., Rhyee, T. S. & Kim, E. A Survey on the current status of mental health act application. J. Korean Neuropsychiaric Assoc.41, 693–705 (2002). PMID:edskci.ARTI.251172. [Google Scholar]
- 28.Na, Y. Investigation of human rights violations in individuals with mental disorders. Mental Health Social Work29, 389–419 (2008). PMID:edspia.NODE06082115. [Google Scholar]
- 29.Kim, C. Y. The current mental health welfare Act is not sustainable. Health Policy Forum.15, 43–50 (2017). PMID:edspia.NODE07251120. [Google Scholar]
- 30.Lee, K. Risk for self-harm or harm to others: definition and assessment of dangerousness. Korean J. Schizophr Res.26, 12–17 (2023). PMID:edskci.ARTI.10223212. [Google Scholar]
- 31.Kim, A. M. & Sohn, J. H. The impact of the Mental Health Act revision for deinstitutionalization in Korea on the crime rate of people with schizophrenia. Psychiatry Res.321, 115089. 10.1016/j.psychres.2023.115089 (2023). [DOI] [PubMed] [Google Scholar]
- 32.Hartvig, P. & Kjelsberg, E. Penrose’s Law revisited: the relationship between mental institution beds, prison population and crime rate. Nord. J. Psychiatry63, 51–56. 10.1080/08039480802298697 (2009). [DOI] [PubMed] [Google Scholar]
- 33.Torrey, E. F. et al. The treatment of persons with mental illness in prisons and jails: a state survey. Treat. Advocacy Cent., 1–116 (2014).
- 34.Wagner, A. K., Soumerai, S. B., Zhang, F. & Ross-Degnan, D. Segmented regression analysis of interrupted time series studies in medication use research. J. Clin. Pharm. Ther.27, 299–309. 10.1046/j.1365-2710.2002.00430.x (2002). [DOI] [PubMed] [Google Scholar]
- 35.Schober, P. & Vetter, T. R. Segmented regression in an interrupted time series study design. Anesth. Analg.132, 696–697. 10.1213/ane.0000000000005269 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Valsamis, E. M., Husband, H. & Chan, G. K. Segmented linear regression modelling of time-series of binary variables in healthcare. Comput. Math. Methods Med. 3478598. (2019). 10.1155/2019/3478598 (2019). [DOI] [PMC free article] [PubMed]
- 37.Kobayashi, K. et al. Interrupted time-series analyses of routine vaccination program for elderly pneumonia patients in Japan; an ecological study using aggregated nationwide inpatient data. Hum. Vaccin Immunother. 17, 2661–2669. 10.1080/21645515.2021.1875760 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bazo-Alvarez, J. C., Morris, T. P., Carpenter, J. R. & Petersen, I. A Scoping review in health research. Clin. Epidemiol.13, 603–613. 10.2147/clep.S314020 (2021). Current Practices in Missing Data Handling for Interrupted Time Series Studies Performed on Individual-Level Data:. [DOI] [PMC free article] [PubMed]
- 39.Hwang, T. Y., Jung, G., Lee, C. J. & Kim, H. Y. Analysis of involuntary admissions in Korea through the admission management information system. Int. J. Law Psychiatry. 68, 101542. 10.1016/j.ijlp.2020.101542 (2020). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Bazo-Alvarez, J. C., Morris, T. P., Carpenter, J. R. & Petersen, I. A Scoping review in health research. Clin. Epidemiol.13, 603–613. 10.2147/clep.S314020 (2021). Current Practices in Missing Data Handling for Interrupted Time Series Studies Performed on Individual-Level Data:. [DOI] [PMC free article] [PubMed]
Supplementary Materials
Data Availability Statement
No data are available because the National Health Information Database can only be accessed by researchers authorized by the Korean National Health Insurance Service. Researchers interested in accessing data should apply to the National Health Insurance Service of Korea. Researchers must first obtain approval from the for their research topic and process. After receiving approval, they can access the National Health Insurance sharing service website (https://nhiss.nhis.or.kr/en/z/a/001/lpza001m01en.do), input the desired research topic, variables, and conditions, and then undergo the NHI review process. Once approved, the database will be made available; however, analysis can only be conducted in designated analysis rooms provided by the NHI.