Abstract
Background
Internship is a phase of training wherein medical graduates acquire the skills and competencies required to function independently. It has been reported that interns lack confidence in performing common procedures, as these skills are often learnt through self-learning or performing without supervision. This type of learning endangers patient safety and fails to instil the required confidence in the student. Training in skills laboratories provide opportunity to learn clinical skills in a safe environment. However, skills laboratories are resource-intensive, and there is limited information on different training approaches, such as blended learning, and how the trainees perceive their usefulness. Hence, we conducted this pilot study to assess the perceived usefulness of a blended learning approach for skills training among medical interns.
Methods
This mixed methods study was conducted in the skills laboratory of an apex medical institute in India, among 42 interns posted for the Interns Skill-based Clinical Induction Program (ISCIP). In this training, a blended learning approach was adopted, which comprised of two components - an online e-learning module, followed by a hands-on training session. The trainees were asked to complete a feedback form and grade different components of the online session, and hands-on session on a five-item Likert-based scale. The scores were expressed as the mean (SD) of a maximum possible score of 5 for each of the components. In order to gain insight of the perceived usefulness of skills training among learners, focused group discussions (FGDs) were conducted.
Results
The mean (SD) score for perceived importance ranged from 5 (0) to 4.9 (0.2) for various skills. The proportion of interns who felt confident in performing the skill after the training was 88.1% for IV cannulation to 97.6% handwashing, and gloving and gowning. The findings of the qualitative component revealed that interns found the training to be useful and interesting. It was perceived to be more ethical, uniform, well-structured, and provided an opportunity to practice a skill repeatedly.
Conclusions
The blended learning approach was perceived to be useful among the medical interns. Further research may be conducted in other medical institutes to assess the effectiveness of skills training.
Clinical trial registration number
Not applicable, as the study is not a trial.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12909-024-06379-x.
Keywords: Medical interns, Skills training, Blended learning, Skills laboratory
Introduction
Internship is a phase of training wherein medical graduates acquire the skills and competencies for practice under supervision, so that they may become capable of functioning independently, and providing clinical care as doctor of first contact in the community [1]. To fulfil this role, competence in certain procedural skills is essential. Although early clinical skills training is currently emphasized in many medical colleges today, however, many students still feel unprepared about starting their internship [2]. Studies conducted in various countries have reported that interns lack confidence in performing common procedures such as intravenous (IV) cannulation, venepuncture and suturing [3, 4].
It has also been reported that students often learnt the clinical procedures through self-learning or learning by doing so on the patient without instructor supervision [5]. The traditional methods of learning procedural skills are known to have various concerns such as patient safety, non-availability of equal opportunities for the students to learn all the skills on patients, inability to correct faults, and failure to instill the required confidence in the student. This calls for provision of training in facilities such as skill laboratories, that provide a space for the students to hone their clinical skills before applying them in real-world situations [6]. Training in skills laboratory enhances and creates opportunities for students to learn clinical skills in a safe environment, without endangering the patients.
However, skill laboratories are resource-intensive, and currently few medical institutes in India are equipped with such facilities. Additionally, the information regarding different approaches utilized for skills training, including blended learning, is limited. The perceived usefulness of a blended learning model, from the perspective of the learners, has not been studied extensively within the Indian context. Since educational practices and levels of technological support may differ significantly across institutions, we have delineated our model of skills training, which utilized an institutional learning management system (LMS), and assessed its perceived utility among the interns.
The assessment of training is important to identify the gaps in teaching-learning methods, and resolution of these gaps will not only improve the quality of skill-based teaching, but also more efficient use of skill laboratories.
In this study, we focused our evaluation on the first level of the Kirkpatrick model i.e. ‘Reaction’ and aimed to assess whether the learners found the training to be relevant to their role, engaging and useful [7]. Our study aims to provide a deeper understanding of the interns’ perception of model, and anaylzes the measures suggested for improvement by the learners.
Objective
To assess the perceived usefulness of a blended learning approach for skills training in the Interns Skill-based Clinical Induction Program (ISCIP) among the medical interns.
Methodology
This mixed methods study was conducted at the All India Institute of Medical Sciences (AIIMS), New Delhi. The institute has a newly devopled state-of-the-art facility i.e. SET (Skills, e-Learning, Telemedicine) facility to impart skills training to medical undergraduates, postgraduates and nursing staff so that they are better prepared when managing patients in wards and clinics [8].
Development of the skills training program
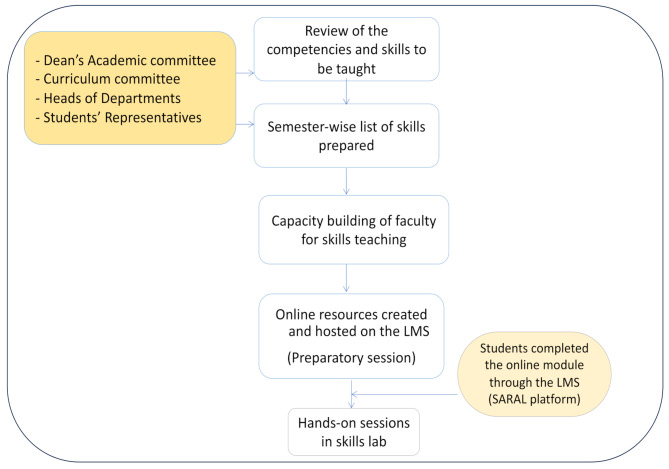
For designing this program, the Dean’s academic committee, heads of various departments, representatives of medical students, interns and other relevant stakeholders were involved at each step.
We followed the “The Ds for Designing Learning Interventions,” described by S Eagleton, for our program [9]. The model consisted of four steps- Determining Learning Task Requirements, Designing Learning Interventions, Developing Learning Interventions, and lastly Delivering learning Interventions.
-
(i)
Determining Learning Task Requirements- This step involved indentification of learning needs of the students for the skills based learning (SBL) program. Brainstorming sessions were held with faculty members of various departments, medical students and interns. Clinical skills relevant during the course of medical training were identified. Thus, a comprehensive list of essential clinical skills (ECSs), to be taught in various semesters, and during the internship, was prepared.
-
(ii)
Designing Learning Interventions- We decided to use a ‘blended learning methodology’ for the SBL program. Specific learning outcomes were defined for each skill module and the online content was prepared to achieve these outcomes. To create the online content, we chose a standard format for all the modules. This format consisted of a three-part online segment.The first section was a structured, standard operating procedure (SOP), which was to be adopted during skill performance. It provided an introduction regarding the respective procedure, description of the equipment and instruments required for the procedure, and a step-by-step description of how to perform the skill. The second section was an audio-visual file showing and describing the skill. The third section consisted of 5–10 multiple-choice questions (MCQs) based on the first two sections. Thus, the online component ensured that the cognitive domain related to the skill was covered adequately. This was followed by a hands-on training session in the skills laboratory. The hands-on session aimed to develop the psychomotor and affective components of the skills.
-
(iii)
Developing Learning Interventions- Faculty members from various discplines were oriented to the SBL. Capacity-building workshops were held for faculty members who were willing to create content for the skill modules. Training for creation of SOPs, audio-visual content, and MCQs was provided in small groups (6–8 faculty members) from time to time. For creation of audio-visual content simple tools on power point, keynote and i-movie maker were used. Some of the videos were made during the live procedure (after obtaining consent from the patients).
The faculty members, thus trained, developed the content for the ECS, relevant to their respective disciplines.
-
(iv)
Delivering Learning Interventions
A blended learning approach was utilized for delivery of the SBL program. Each skill session consisted of two components - an online module, and a hands-on training session.
The online component was made available on the Learning Management System (LMS) of the institute. The LMS is known as the SARAL (Student Advanced Resources and Learning) platform. All the students of the institute were routinely registered on this LMS. The students could access these modules after logging in with their credentials. The students could go through the online module at a time convenient to them, and could learn the content at their own pace. They could also view the content multiple times, if needed. The online module served as a preparatory session before the hands-on training, and provided more in-class active learning time.
After completion of the online module and qualification of the MCQ based test (i.e. atleast 80% score), an e-certificate was generated for the online module. The same was mandatory for attending the hands-on session in the skills laboratory.
After the students successfully completed the online module, they performed the skills on mannequins and task trainers in the skills laboratory, under the supervision of faculty members.
The development and delivery of the skills training program in the study institute is depicted briefly in Fig. 1.
Fig. 1.
Development and Delivery of the Skills Training Program
Validation of the training program
The content was peer reviewed by at least two other faculty members who were considered experts in the field to which the particular skill belonged. In addition, feedback regarding the online and hands-on training was sought from students belonging to different semesters. Twenty skill modules were randomly selected for field testing. The modules were altered and modified according to the comments received from students. The final skill modules were thus distributed over the four and half years of curriculum according to their clinical relevance as well as difficulty level. A few skills were identified for teaching during the first few weeks of the internship, as a part of the Interns Skill-based Clinical Induction Program (ISCIP).
The interns skill-based clinical induction program (ISCIP)
After deliberations among the stakeholders, the skills for the ISCIP were finalized. These skills were- surgical hand washing, sterile gloving and gowning, intravenous cannulation, urethral catheterization, basic suturing and episiotomy repair.
The training was conducted during the initial two months of the beginning of the intership. This was done to ensure that the students were still relatively naïve to the skills and would understand the clinical implications of the skills taught. Each training session was held over half a day (4–5 h). The trainings took place twice a week and 10–12 students attended each session. The program was planned in such a way that students could learn all skills in a single session, however, in event of students not being able to do all skills in one session, they were encouraged to attend subsequent sessions.
The manikins used in the training program were unbranded, locally procured models with reusable skin. Part task trainers were used for learning episiotomy repair, IV canulation and basic suturing skills.
Data collection
The study participants included the interns who were posted for the ISCIP training. The training was provided to a batch of 10–12 interns. In the present study, the first five batches of interns posted for the ISCIP were approached. Consecutive sampling was adopted and all the interns were invited to participate in the study. Those who consented to participate were enrolled. Thus, a total of 42 interns were included in the study.
Quantitative component
An online questionnaire based on five-item Likert scale was used to collect information regarding the perceived usefulness of the online module and the hands-on sessions for each of the skills taught in the ISCIP (Supplementary file 1) The interns were asked to grade the SOPs, video, and hands-on session respectively on a scale of 1 to 5, ranging from least useful to most useful. They were also asked to grade the perceived importance in clinical practice, and how confident they felt after attending the training program.
Qualitative component
To gain an insight of the perceived usefulness of skill-based program among the learners, focused group discussions (FGDs) were conducted. A homogenous group of 5–7 interns each was selected by purposive sampling, and was invited to participate in these FGDs. A topic outline guide (TOG) was used to facilitate the discussion (Supplementary file 2). A team consisting of a moderator, a co-moderator (faculty members engaged in skills teaching and trained in qualitative research), and a recorder conducted the sessions.
The outline guide included the perception of interns regarding training of clinical procedures in a skills laboratory, its perceived usefulness, advantages/disadvantages of learning a skill in a skills laboratory as compared to real patients, factors that motivated them to attend the skills training program, facilitators and barriers for attending the ICSIP, and suggestions to improve the training program. Audio recording of the FGDs was done. A total of five FGDs were conducted. There were 6–8 participants in each FGD. The audio-recorded discussions were transcribed in verbatim. Textual analysis of the data was performed.
Statistical analysis
The quantitative data were entered in Microsoft Excel spreadsheet and analyzed using STATA version 14. The scores were expressed as Mean (SD), out of a maximum score of 5 for each of the components. Categorical data were expressed as frequencies and percentages.
For the qualitative component, textual analysis was performed manually. Coding was conducted using a thematic approach, identifying key concepts and ideas expressed by medical interns during the focus group discussions. These codes were then grouped into broader themes that emerged from the data, such as “perceived benefits of blended learning,” “challenges faced in blended learning,” and “suggestions for improvement.” The coding process was iterative, allowing for refinement and the identification of subthemes within the main themes. To strengthen the validity and credibility of the qualitative data obtained from focus group discussions, member checking was conducted with selected medical interns, to verify the accuracy of the researchers’ understanding of the interns’ perspectives and experiences. Furthermore, peer debriefing was employed to critically evaluate the interpretations and to identify any potential biases in the analysis.
Validity was achieved by triangulation of findings from quantitative analysis of feedback forms and the FGDs. The results obtained from the feedback forms, including the scores assigned to each module and the recommendations for improvements identified in the quantitative analysis, were corroborated by the findings derived from the focus group discussions.
Results
A total of 42 interns participated in the study. The mean (SD) score for the perceived importance of the skill was 5 (0) for uretheral cathertarization, gloving and gowning, surgical hand washing, and basic suturing, while it was 4.9 (0.2) for IV cannulation and episiotomy repair. A total of 88.1% of the interns felt confident in performing the skills after the training was for IV cannulation, while this percentage ranged from 92.9 for uretheral cathertarization, and episiotomy repair, to 97.6 for handwashing, and gloving and gowning. The mean (SD) scores for the perceived usefulness of various components (i.e. SOPs, videos and hands-on sessions) of the skills module are shown in Table 1.
Table 1.
Feedback regarding various components of skill modules under the ICSIP
| Name of the skill module | Mean Score (SD) Maximum = 5 |
Number (percentage) who felt confident N = 42 |
|||
|---|---|---|---|---|---|
| SOPs | Video | Hands on | Perceived importance in clinical practice | ||
| IV Cannulation | 4.7 (0.4) | 4.4 (0.6) | 4.6 (0.7) | 4.9 (0.2) | 37 (88.1) |
| Urethral Catheterisation | 4.7 (0.4) | 4.6 (0.6) | 4.7 (0.5) | 5 (0) | 39 (92.9) |
| Gowning and Gloving | 4.8 (0.3) | 4.8 (0.4) | 4.9 (0.2) | 5 (0) | 41 (97.6) |
| Basic suturing | 4.3 (0.6) | 4.5 (0.5) | 4.2 (1.1) | 5 (0) | 40 (95.2) |
| Hand-Washing | 4.9 (0.2) | 4.7 (0.5) | 4.8 (0.3) | 5 (0) | 41 (97.6) |
| Episiotomy repair | 4.6 (0.4) | 4.4 (0.6) | 4.3 (0.9) | 4.9 (0.2) | 39 (92.9) |
Findings from the focussed group discussions (FGDs)
The content analysis of all the five FGDs indicated that the interns found the training to be useful and interesting. While common themes emerged in domains of perceived usefulness, newer themes were identified in the domains of perceived motivators and barriers, and suggestions for improvement. These included conducive learning environment (Group 1), pereceived lack of relevance to exams (Group 3), need for improved models (Group 2), and timely commencement of training (Group 5).
The interns were enthusiastic to attend this program. These findings are corroborated by the following statements:
“Our batch is the first batch that underwent training in a skills lab. We never got such an opportunity to do hands on training earlier.”
“When I got to know that this type of training is happening, I was so excited… I didn’t want to miss it.”
Advantages of learning in a skills laboratory
The group highlighted various advantages of skills training using the blended learning model. The emergent themes and supporting verbatims are described below:
Increase in confidence
The interns expressed that they used to feel anxious or scared when asked to perform a procedure on a patient for the first time. However, after being trained in the skills lab, they feel much more confident.
“Earlier, I used to be scared and anxious when asked to perform a procedure for the first time. I thought I might harm the patient, but now I feel confident that I can perform cannulation and cathertarization in real patients.”
Ethical and empathetic approach
The participants felt that it was more ethical to first practice the skill in the mannequins or models, rather than performing it directly on the patient.
“Performing a procedure directly on a real patient without any practice may harm the patient. The patients are already in pain and they become frustrated if you cannot place a cannula or catheter on the first attempt.”
“We try to learn on sick patients and it feels bad when the patient gets uncomfortable.”
Possibility of repeated attempts
“When you fail to perform a procedure successfully on a patient in the first attempt, you don’t have the courage to perform it for a second time. This really affects your confidence.”
“In the skills lab, I could perform the procedure repeatedly without fear until I could do all the steps correctly. This increased my confidence.”
Equal opportunity
The interns found the training program to be very useful, as it provided them with the opportunity to practice the skill compared to traditional teaching in clinical settings, where only a few enthusiastic students had the opportunity to perform the skills.
“In the skills lab, all of us got an equal opportunity to practice. On the other hand, in the ward or clinic, only those who are outspoken or enthusiastic have this opportunity.”
Uniformity of the content
“Earlier we used to learn from different residents in the ward. Generally, there was a variation in the steps.However, now everyone learns the same steps as there are Standard Operating Procedures.”
“Even if a teacher is not very enthusiastic about teaching, the availability of a checklist ensures that none of the steps are missed in skills training.”
Well-structured sessions
“I can say that in my entire degree, this is the most structured session that I have ever attended.”
“Since we had gone through the online content, it provided more time for hands on practice.”
“All the classes should be conducted like this.”
Disadvantages of skills training in skills laboratory
The participants described some disadvantages of skills training. A major concern was that it did not mimic the real situation. Additionally, there was lack of training regarding difficult scenarios.
“Sometimes it does not feel real…also, there is lack of experience with difficult patients such as those with poor venous access.”
Motivating factors and barriers
In this domain, the factors that motivated the interns to attend the skills sessions were explored. The participants expressed that the skills included in the training program were the ones that they were required to perform routinely during their clinical postings. The availability of good online content and positive feedback from previous batches were the other motivating factors. The fact that attending this program was not compulsory and was perceived to be of little value in clearing the examination for post graduate entrance, was thought to be a deterrent for those who did not attend the sessions.
The suggestions for improvement included better logistics in terms of improved quality of models, more number of stations and equipment, and more time for practice, particularly for basic suturing and episiotomy repair.
Table 2 shows the domains and description of the motivating factors and perceived barriers in attending the skills training program, and the suggestions for improvement.
Table 2.
Perceived motivators, barriers and suggestions for improvement of skills training
| Domain | Themes and sub themes identified | Description | Supporting quotes |
|---|---|---|---|
| Motivating factors | Alignment with the requirement | The interns found the training valuable because it covered the skills essential for their daily tasks. | “ The skills that are being taught are the ones that we are required to perform everyday in our postings.” |
| Quality of online content | High-quality e-modules motivated the interns to attend hands-on sessions. | “The quality of the online content was so good that we were inspired to attend the skills session.” | |
| Credibility of the content | Content prepared by faculty of the institute ensured accuracy and authenticity | “ A lot of material is available on the internet, but we are not sure of its credibility. The online content available in the e-modules is prepared by the faculty of the institute, and hence we are assured that the information provided is correct and authentic” | |
| Positive feedback from the peers | Endorsement from previous batches encouraged current interns to participate. | “ The previous batches who attended this training told us that the sessions are very useful, hence we also got motivated to attend” | |
| Use of innovative techniques | Introduction to new methods such as hands-on practice with mannikins and technology-enhanced the learning. | “ We never had hands on practice on dummies and mannequins. It felt really good. Also use of technology like online quiz was enticing” | |
| Conducive learning environment | State-of-the-art facilities contributed to a positive learning experience. | “The environment is very conducive…it’s a state of the art facility.” | |
| Barriers | Non-compulsory Attendance | Lack of mandatory attendance might have led some interns to skip sessions. | “The attendance is not compulsory, so some people might have missed it” |
| Perceived lack of relevance to exams | Some interns believed that the training did not help them prepare for postgraduate entrance exams. | “In internship, everyone’s focus is to clear the postgraduate entrance examination. Some interns think that this training will not help them to solve the MCQs. Hence, they didn’t give importance to it”. | |
| Suggestions for improvement | Better logistics | Improved organization and availability of resources. | “There should be more cathetars and more stations for practice. Also, female cathertarization should be included” |
| Improved models | Better quality and variety of tools, including suturing materials and model textures. |
“For basic suturing, the quality of suture sets was not good…the texture didn’t resemble skin.” “For episiotomy, the material of the model could have been better…. the foam was tearing apart.” “The size of the needle was too big for the given dummy.” |
|
| More practice time | Interns suggested more time dedicated to practical sessions. |
“More time should have been given for suturing and episiotomy” Also there should be provision for practice even after the skill session” |
|
| Challenging quizzes | Interns desired more stimulating quiz questions to encourage deeper study. | “For all the skill modules, the quiz was very simple and easy. Difficult questions would have motivated us to study more” | |
| Timely commencement of training | Interns suggested starting training earlier to align with clinical postings. | “ It should have been started earlier…atleast before the rural posting, we perform many procedures independently there” |
Discussion
The present study showed that the skills training program was perceived to be very useful by the medical interns. Before the skills training, they felt scared and anxious that they could harm the patient, and found it unethical to perform the procedures directly on patients. Similar findings were reported by Hannon [10], and Sarikaya et al. [11], where students expressed high levels of anxiety and fear of harming the patients. The interns in our study expressed that skills training increased their confidence and alleviated the anxiety. This finding is similar to other studies that have shown that skills training improved the confidence and preparedness of medical students [12–14].
The participants in our study revealed that there were significant variations in their skills training by traditional methods in wards or clinics, while the skills training program was well- structured. Morris et al. (2016) in Ireland and Ringsted et al. (2001) in Denmark, also reported that the interns experienced significant variations in skills teaching [2, 15]. On the other hand, skills training in skill laboratories has been reported to ensure a more structured and uniform training [16].
The disadvantage of the skills laboratories cited by the interns in our study was that they did not equate to the of real scenario of performing skills in patients. Additionally, this type of training did not provide an opportunity to handle difficult situations, such as IV canulation in patients with difficult venous access. This has also been reported by Morris et al. [2] and Mansoorian et al. [17] as well. However, it is understood that skills training in laboratories is supplementary, and not an alternative to bedside teaching [18, 19]. Training in skills laboratories is believed to prepare the students for better patient encounters in clinical settings. Another area of concern is the retention of skills. It has been highlighted earlier that skills training in laboratories may lead to immediate improvement in performance, however, there is a lack of well-designed studies that assessed acquisition and retention of skills over time [20].
Provision of better quality of models, more number of stations, and more time for practice were some of the suggestions for improvement in our study. The studies by Mansoorian et al. [17] and Hashim et al. [21] also highlighted that the trainees suggested more stations and more time for practice for better skills learning.
The interns in our study emphasized their felt need to initiate skills training in the initial semesters, at least before their rural posting, where they were expected to perform the procedures independently. This study was conducted in the initial phase of skills training in the institute, however, the program has been updated and the skills training is presently being initiated as early as third semester. The importance of skills training in the pre-clinical years has been highlighted in many studies, as it prepares the students for internship [17, 20–22].
Our study is one of the few studies in India that assessed the usefulness of a blended learning approach for skills training among the medical interns. Easy availability and engagability of digital technologies have brought new dimensions to how we approach learning, teaching, and interacting with the millennial students. In blended learning, part of the teaching is imparted via online portions, and part of it is provided via faculty-guided face to face teaching. The blended learning approach provides an option that combines the technological advances of today’s world with traditional face-to-face interactive teaching methods, thus combining the advantages of both the methods.
The use of a mixed method study design is another strength of this study.
However, our study had certain limitations. Since the study was conducted among few medical interns at a single institute and the sample size was small, the generalizability of our study is limited. We did not have a comparison group in our study, which would have increased the validity of our findings.
Furthermore, we focused on the first level of Kirkpatrick’s model that provided a limited perspective on the effectiveness of our skills training model. However, the primary objective of our study was to gain an insight of initial perceptions of the interns regarding the blended learning approach. Since this was a novel intervention in our setting, we felt it was critical to first understand how well it was received by the participants before proceeding to more complex levels of evaluation. Additionally, the timing and logistical constraints associated with our intern rotations made it challenging to conduct more longitudinal assessments, more so in the wake of the COVID-19 pandemic, which led to suspension of face to face teaching activities for a significant period of time. Given the importance of long-term evaluation of retention of skills, follow-up studies to assess the impact of this training on knowledge and clinical performance have been planned.
Our research may be viewed as a pilot study and further research may be developed to evaluate the acquisition and retention of skills, across multiple centres in the country. It is also necessary to evaluate how well such skill-training programs work to create real competence in clinical settings.
The study highlights the users’ perspective of a skills training program, which will be useful in improving the skills training for the future trainees. The recently introduced competency based medical curriculum in India emphasizes on skills training at all levels. Medical institutions are required to create skill sessions in which essential/desirable and certifiable skills are acquired [23]. At present, skill labs are being established in the country and the findings from our study may be beneficial for other institutes in designing their skills training programs.
Conclusions
The ISCIP was perceived to be useful among the interns in order to instil confidence in performing clinical skills and ensuring patient safety. Further research is needed about the long-term effectiveness of skills training with regard to the retention of acquired skills and actual competence during the internship.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author contributions
RR, RK, AR and AKD conceptualised and designed the study. RR, RK and PG collected the data, facilitated the sessions and conducted the interviews. RK, RR and PG analyzed the data. RK, RR, PG, AR and AKD interpreted the data. RK and PG prepared the tables. RK drafted the major part of the manuscript, while RR drafted sections of the manuscript. AR, PG and AKD edited and reveiwed the manuscript. All authors read and approved the final manuscript.
Funding
The authors did not receive any specific grant, for conduct of this study, from funding agencies in the public, commercial, or not-for-profit sectors.
The financial support for publication is provided by the Novo Nordisk Foundation, Denmark, through the grant awarded to Rashmi Ramachandran (Project N 2365). The funder has no role in conceptualization, design, data collection, analysis, decision to publish or preparation of the manuscript.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on request.
Declarations
Ethics approval and consent to participate
The participation in the study was voluntary. Written informed consent was obtained from the participants. The study was conducted after obtaining approval from the Institute Ethics Committee of the All India Institute of Medical Sciences, New Delhi (Reference no. IEC-276/03.05.2019).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.National Medical Commission. Draft regulations for compulsory rotating internship 2021. Available online at: https://www.nmc.org.in. Accessed on 28 Oct, 2023.
- 2.Morris M, O’Neill A, Gillis A, Charania S, Fitzpatrick J, Redmond A, et al. Prepared for Practice? Interns’ Experiences of Undergraduate Clinical Skills Training in Ireland. J Med Educ Curric Dev. 2016;3. JMECD.S39381. [DOI] [PMC free article] [PubMed]
- 3.Gazibara T, Nurkovic S, Maric G, Kurtagic I, Kovacevic N, Kisic-Tepavcevic D, et al. Ready to work or not quite? Self-perception of practical skills among medical students from Serbia ahead of graduation. Croat Med J. 2015;56:375–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carr P, Glynn R, Dineen B, Devitt D, Flaherty G, Kropmans TJ, et al. Interns’ attitudes to IV cannulation: a KAP study. Br J Nurs. 2011;20(4):S15–20. [DOI] [PubMed] [Google Scholar]
- 5.Nikendei C, Schilling T, Nawroth P, Hensel M, Ho a D, Schwenger V, et al. Integrated skills laboratory concept for undergraduate training in Internal Medicine. Dtsch Med Wochenschr. 2005;130:1133–8. [DOI] [PubMed]
- 6.Yazdani R, Yazdan-Panah E, Shafian H, Ahmadi- Pour H. Self-Assessment of Clinical skills in Medical Internship. Strides Dev Med Educ. 2017;14(3):e68137. [Google Scholar]
- 7.Smidt A, Balandin S, Sigafoos J, Reed VA. The Kirkpatrick model: a useful tool for evaluating training outcomes. J Intellect Dev Disabil. 2009;34(3):266–74. [DOI] [PubMed] [Google Scholar]
- 8.All India Institute of Medical Sciences. Skills, e-Learning, Telemedicine facility – SET facility AIIMS.Available online at: https://setfacility.in. Accessed on 24 May, 2024.
- 9.Eagleton S. Designing blended learning interventions for the 21st century student. Adv Physiol Educ. 2017;41(2):203–11. [DOI] [PubMed] [Google Scholar]
- 10.Hannon F. A national medical education needs’ assessment of interns and the development of an intern education and training programme. Med Educ. 2000;34(4):275–84. [DOI] [PubMed] [Google Scholar]
- 11.Sarikaya O, Civaner M, Kalaca S. The anxieties of medical students related to clinical training. Int J Clin Pract. 2006;60:1414–8. [DOI] [PubMed] [Google Scholar]
- 12.Makoul G, Altman M. Early assessment of medical students’ clinical skills. Acad Med. 2002;77(11):1156. 10.1097/00001888-200211000-00020. PMID: 12431933. [DOI] [PubMed]
- 13.Razavi M, Meshkani Z, Panahkhahi M. Teaching and testing basic surgical skills with using patients. J Med Edu. 2004;6(1):e105143. [Google Scholar]
- 14.Shahid H. How to develop a core curriculum in clinical skills for undergraduate medical teaching in the school of medical sciences at Universiti Sains Malaysia? Malays J Med Sci. 2007;14:4–10. [PMC free article] [PubMed] [Google Scholar]
- 15.Ringsted C, Schroeder T, Henriksen J, et al. Medical students’ experience in practical skills is far from stakeholders’ expectations. Med Teach. 2001;23(4):412–6. [DOI] [PubMed] [Google Scholar]
- 16.Bugaj TJ, Nikendei C. Practical clinical training in skills labs: theory and practice. GMS J Med Educ. 2016;33(4). Doc63. PMID: 27579363; PMCID: PMC5003146. [DOI] [PMC free article] [PubMed]
- 17.Mansoorian MR, Jalili M, Khosravan S, Shariati M. Exploring undergraduate medical students’ perception of learning procedural skills and its outcomes in clinical settings. J Adv Med Educ Prof. 2019;7(4):175–82. 10.30476/jamp.2019.74866.0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alhaqvi AI, Taha WS. Promoting excellence in teaching and learning in clinical education. J Taibah Univ Med Scie. 2015;10(1):97–101. [Google Scholar]
- 19.Coberly L, Goldenhar LM. Ready or not, Here they come: acting interns’ experience and perceived competency performing Basic Medical procedures. J Gen Intern Med. 2007;22(4):491–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lynagh M, Burton R, Sanson-Fisher R. A systematic review of medical skills laboratory training: where to from here? Med Educ. 2007;41(9):879–87. [DOI] [PubMed] [Google Scholar]
- 21.Hashim R, Qamar K, Khan MA, Rehman S. Role of Skill Laboratory Training in Medical Education - Students’ perspective. J Coll Physicians Surg Pak. 2016;26(3):195–8. [PubMed] [Google Scholar]
- 22.Gastura FM. Medical students’ perceptions on skills laboratory training for clerkship preparedness at the University of Rwanda: a pilot study. Rwanda J Med Health Sci. 2019;2:25–9. [Google Scholar]
- 23.Medical Council of India. Skills Training Module for Undergraduate Medical Education program. 2019: pp 1–49.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on request.