Abstract
Background
Hydatid disease, a parasitic infection caused by the larval form of Echinococcus granulosus, infrequently involves the thyroid gland, whether through direct invasion or hematogenous spread.
Case presentation
We report the case of a 62-year-old female patient from Morocco who presented with an anterior cervical mass, initially suspected to be a goiter. A histopathological evaluation of the thyroidectomy specimen identified the presence of a hydatid cyst. A comprehensive review of the literature is also included.
Conclusion
Given that Morocco is an endemic region for hydatid disease, clinicians should consider this parasitic infection in the differential diagnosis of thyroid cystic lesions, recognizing the clinical and laboratory indicators of the disease.
Keywords: Hydatid cyst, Thyroid, Anatomical pathology, Diagnosis
Introduction
Hydatid disease is an infection caused by the larval stage of Echinococcus granulosus. It is common in North Africa, parts of the Mediterranean, New Zealand, Australia, and America. It constitutes a significant public health challenge. The prevalence varies, with the Maghreb being a moderately affected area. Hydatid cysts can develop in almost any organ but frequently affect liver (50–77%), lungs (15–47%), spleen (0.5–8%), and kidneys (2–4%) [1]. Less commonly, they can affect the brain, muscles, heart, retroperitoneal organs, pancreas, and thyroid gland. The thyroid gland is rarely involved, even in regions where the disease is common. This disease can affect the thyroid gland either directly or through the blood circulation [2]. Our aim is to report a case of a thyroid hydatid cyst discovered incidentally during a pathological examination, along with a review of literature.
Case report
Patient information: A 62-year-old Moroccan woman with no significant medical history presented with an anterior neck mass and intermittent discomfort with solid food swallowing evolving for months. Clinical finding: Physical examination revealed a goiter. Cervical ultrasound classified the goiter as EU-TIRADS 3, showing cystic and tissue nodules, was isoechoic, and was well limited, with a peripheral capsule often clearly visible and in relation to the perinodular thyroid tissue and without lymphadenopathy. Cytology was not performed because the patient showed signs of compression. No other paraclinical examination was requested. Total thyroidectomy was planned. Diagnosis assessment: Macroscopic examination revealed a thyroid weighing 76 g. The right lobe measured 5.8 cm × 4 cm × 2.3 cm, the left lobe measured 9.5 cm × 4.3 cm × 2.5 cm, and the isthmus measured 3.5 cm × 2 cm. The sectioning showed multiple well-defined nodules of colloid appearance, ranging from 0.3 to 4.3 cm in size, including a 2 cm right cystic nodule with a whitish content. Microscopic examination revealed nodular follicular thyroid disease (Fig. 1) with a lamellar, eosinophilic membrane. This membrane adhered to a thin fibrous layer containing an inflammatory infiltrate (Figs. 2 and 3) and rounded calcified formations resembling a scolex within the 2 cm right lobar cyst (Fig. 4). The pathological diagnosis was a 2 cm right lobar hydatid cyst. Therapeutic intervention: No additional treatment was performed after thyroidectomy. Follow-up and outcomes: The evolution was good with absence of hydatid cysts in other locations.
Fig. 1.
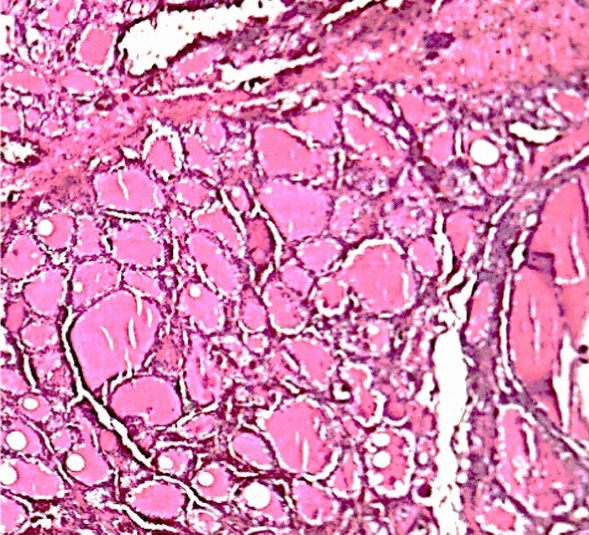
Nodal follicular thyroid disease
Fig. 2.
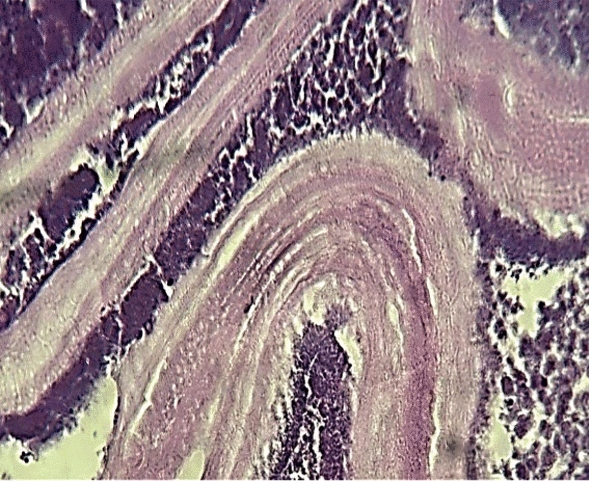
Lamellar eosinophilic membrane with an inflammatory infiltrate
Fig. 3.
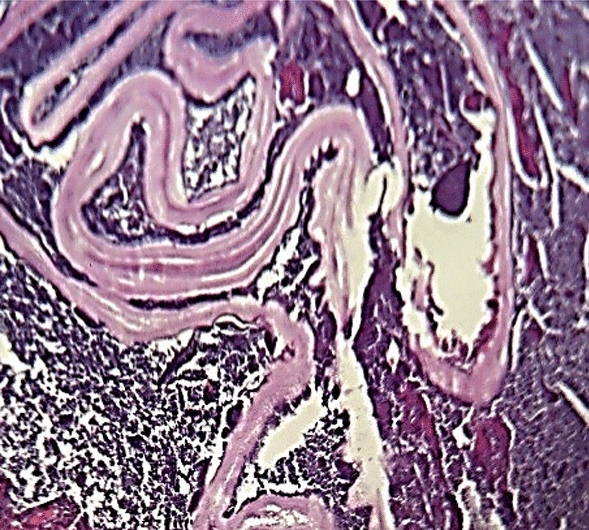
Lamellar eosinophilic membrane. This membrane adhered to a thin fibrous layer containing an inflammatory infiltrate
Fig. 4.
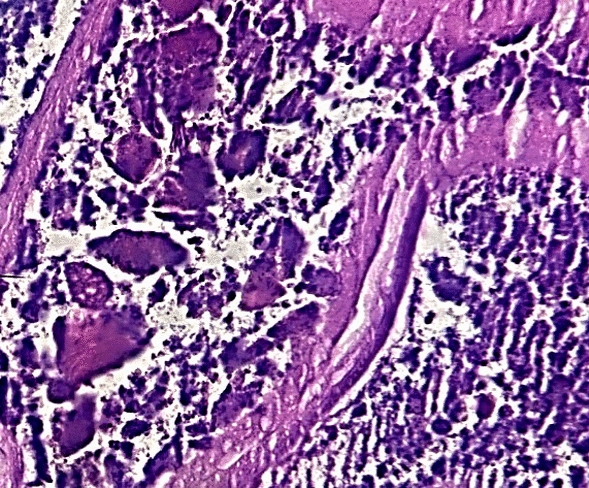
Calcified formations resembling a scolex
Discussion
Hydatid cyst disease (cystic echinococcosis) is a significant public health issue in many regions where sheep and cattle farming are prevalent [3, 4]. It remains an endemic in Morocco, affecting all organs, particularly the liver and lungs. After larvae emerge from ruptured eggs in the host’s gastrointestinal system, they penetrate the intestinal wall and enter the portal system, reaching the hepatic sinusoids. Small larvae pass through the liver filtration system to reach the lungs. Those that bypass lung filtration can spread to other organs, including the spleen, kidneys, heart, bones, muscles, pancreas, retroperitoneum, breast, and thyroid gland. The thyroid gland is rarely affected, [5, 6] even in endemic countries such as Morocco [38]. A literature review identified the cases listed in (Table 1).
Table 1.
Reported cases of thyroid hydatic cysts in literature
| References | Location | Year | Number of case | Age | Sex | Diagnosis | Management |
|---|---|---|---|---|---|---|---|
| [11] | India | 1946 | 1 | ||||
| [36] | Turkey | 1989 | 1 | 54 | F | Total thyroidectomy | |
| [36] | Iran | 1999 | 2 |
16 27 |
F |
Excision Excision |
|
| [30] | 1995 | 3 |
16 24 60 |
F F F |
Lobectomy Excision Excision |
||
| [25] | Italy | 1999 | 1 | 54 | F | Pathology | Surgery |
| [38] | Morocco | 2004 | 1 | 21 | M | Resection | |
| [27] | France | 2005 | 1 | 28 | M | Pathology | Lobectomy and isthmectomy |
| [31] | India | 2005 | 1 | 55 | F | Excision | |
| [35] | Turkey | 2005 | 2 |
21 70 |
M F |
Hemithyroidectomy Total thyroidectomy | |
| [34] | 2007 | 1 | 18 | M | Lobectomy and isthmectomy | ||
| [26] | Bihar | 2007 | 1 | 30 | M | The patient refused the operation | |
| [37] | Turkey | 2010 | 1 | 48 | M | Albendazole and aspiration | |
| [32] | Morocco | 2011 | 1 | 23 | F | Subtotal thyroidectomy | |
| [5] | Turkey | 2013 | 1 | 23 | M | Pathology | Subtotal thyroidectomy |
| [2] | Saoudi Arabia | 2013 | 1 | 48 | F | Pathology | Albendazole for 6 weeks, then thoracotomy and thyroidectomy |
| [2] | Turkey | 2013 | 3 |
18 25 21 |
M F M |
Indirect hemagglutinin + pathology Pathology Pathology |
Albendazole and left lobectomy and isthmectomy Total thyroidectomy Total thyroidectomy |
| [3] | India | 2014 | 1 | 30 | F | Cytology | Albendazole for 28 days(conservative) |
| [13] | Turkey | 2015 | 2 |
25 57 |
F F |
Pathology Pathology |
Total thyroidectomy Total thyroidectomy |
| [14] | Turkey | 2015 | 1 | 32 | F | Pathology | Total thyroidectomy |
| [28] | Romania | 2015 | 1 | 26 | F | Total thyroidectomy | |
| [15] | Turkey | 2016 | 1 | 44 | F | Cytology | Hemithyroidectomy |
| [16] | Turkey | 2016 | 1 | 65 | F | Pathology | Total thyroidectomy |
| [17] | Morocco | 2016 | 1 | 35 | M | Pathology | Total thyroidectomy |
| [24] | Pakistan | 2016 | 1 | 35 | F | Pathology | Total thyroidectomy |
| [19] | Iran | 2016 | 1 | 34 | F | Pathology | Left lobectomy and isthmectomy |
| [18] | Turkey | 2018 | 1 | 32 | F | Immunology, histopathology | Total thyroidectomy |
| [20] | China | 2019 | 1 | 54 | M | Immunology, histopathology | Cyst removal |
| [29] | India | 2019 | 1 | 14 | F | Neck ultrasonography | Surgical excision with perioperative albendazole |
| [21] | Iraq | 2021 | 1 | 48 | F | Pathology | Left lobectomy |
| [22] | Syria | 2021 | 1 | 26 | F | Pathology | Total thyroidectomy |
| [23] | Iran | 2023 | 2 |
35 50 |
F F |
Cytology Cytology |
Right thyroid lobectomy and isthmectomy Near-total thyroidectomy |
| [40] | South Africa | 1 | 29 | F | |||
| [41] | Spain | 1 | 66.5 | M | |||
| [42] | Austria | 1 | 14 | F | |||
| [43] | Turkey | 1 | 50 | F | |||
| [44] | Turkey | 1 | 9 | M | |||
| [45] | Turkey | 1 | 49 | F | |||
| [6] | Turkey | 1 | 25 | M | |||
| [10] | Turkey | 1 | 33 | M | |||
| [46] | Libyan | 1 | 12 | M | |||
| [47] | Kurdistan | 1 | 48 | F | |||
| [48] | Tunisia | 1 | 8 | ||||
| [49] | Spain | 1 | 64 | M | |||
| [50] | India | 1 | 12 | M | |||
| Our case | Morocco | 1 | 62 | F | Pathology | Total thyroidectomy |
Thyroid hydatid cyst disease can be primary or secondary. Diagnosis relies on clinical and paraclinical analyses, such as ultrasound and cytology results. However, most cases are diagnosed post surgery, and anatomical pathology remains the gold standard for diagnosis, as confirmed in our case [7–9]. Similar to other hydatid cyst locations, thyroid hydatid cysts are primarily treated with surgical excision [10, 11]. The recommended surgical approach involves careful removal of the cyst(s) to avoid rupture. In cases of localized cysts or small cysts within a lobe, subtotal thyroidectomy may be considered [12]. To prevent anaphylactic reactions and cyst dissemination, it is advised to protect the surgical field with hypertonic saline-soaked sponges, minimize cyst manipulation, and administer preoperative medical treatment for diagnosed cysts. Antiparasitic medications such as mebendazole, albendazole, and praziquantel cannot be used for a complete cure but can kill live parasites and prevent contamination during surgery [26]. Our patient underwent surgery alone.
Conclusion
Morocco is an endemic country, and physicians should be aware of the clinical and paraclinical presentation of hydatid disease among differential diagnosis of thyroid cystic pathology. A multidisciplinary approach involving radiologists, pathologists, and otorhinolaryngologist surgeons is essential for optimal patient management.
Acknowledgements
To anyone who has participated in the care of this patient directly or indirectly.
Author contributions
IB, IA, and FB: drafted and corrected the manuscript. AE-N: clinical and surgical management of the patient.
Funding
No funding.
Availability of data and materials
Data available
Declarations
Ethics approval and consent to participate
The patient authorizes the publication of this article.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Venara A, Mehinto D, Lermite É, Chabasse D, Hamy A, Arnaud JP. Localisations primitives inhabituelles du kyste hydatique. Presse Med. 2011;40(4):438–42. French. [DOI] [PubMed] [Google Scholar]
- 2.Yilmaz M, Akbulut S, Sogutlu G, Arabaci E, Kayaalp C. Kyste hydatique de la glande thyroïde : à propos de trois cas. Surg aujourd’hui. 2013;43(8):937–41. French. [DOI] [PubMed] [Google Scholar]
- 3.Dey AK, Mandal PK, Dutta A, Pramanik S, Maji S, Chakraborti N. Un cas de kyste hydatique de la glande thyroïde. Asiatique J Med Science. 2014;5:143–5. French. [Google Scholar]
- 4.Harmouch T, Benlemlih A, Hammas N, Bendahou M, Oudidi A, El Alami M, Amarti A. Présentation clinique atypique d’un kyste hydatique thymique primitif: à propos d’une observation Marocaine. Pan Afr Med J. 2012;11:44. French. [PMC free article] [PubMed] [Google Scholar]
- 5.Oksuz S, Pektas E, Yavuz M, Aksungur N, Cayir Y, Akcay MN. Une cause inhabituelle d’enrouement : le kyste hydatique de la thyroïde. Trop Bioméd. 2013;30(4):642–4. French. [PubMed] [Google Scholar]
- 6.Ozaydin I, Ozaydin C, Oksuz S, Yildirim M. Kyste échinocoque primaire de la thyroïde : à propos d’un cas. Acta Med Iran. 2011;49(4):262–4. French. [PubMed] [Google Scholar]
- 7.Jain S, Jamdade P, Muneshwar S, Ambulgekar V, Panzade S. Kyste hydatique de la thyroïde : une cause inhabituelle de stridor. Indian J Otolaryngol Chirurgie de la tête et du cou. 2005;57(1):80–1. French. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gürses N, Baysal K, Gürses N. Kyste hydatique dans la thyroïde et les glandes salivaires sous-maxillaires chez un enfant. Z Kinderchir. 1986;41(06):362–3. French.3825303 [Google Scholar]
- 9.Moghimi M, Kamrava SK, Behzadi AH, Asghari AM, Jalessi M, Naraghi MM, Afshar EE. Kyste échinococcique primaire dans la glande thyroïde : à propos d’un cas en Iran. J Infect Dev Ctries. 2009;3(9):732–4. French. [DOI] [PubMed] [Google Scholar]
- 10.Gökçe C, Patiroglu T, Akşehirli S, Durak AC, Keleştimur F. Kyste hydatique dans la glande thyroïde diagnostiqué par biopsie par aspiration à l’aiguille fine. Thyroïde. 2003;13(10):987–9. French. [DOI] [PubMed] [Google Scholar]
- 11.Reddy DG, Thangavelu M. Kyste hydatique-thyroïde. Indien J Surg. 1946;8:49. French. [Google Scholar]
- 12.Sersar SI, Batouk AO. Echinococcosis, bilateral pulmonary complicated and non complicated with bilateral thyroid gland. Asian Cardiovasc Thorac Ann. 2013;21(4):485. [DOI] [PubMed] [Google Scholar]
- 13.Akbulut S, Demircan F, Sogutcu N. Hydatid cyst disease of the thyroid gland: report of two cases. Int Surg. 2015;100(4):643–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bartın MK, Yılmaz EM, Arslan H, Tekeli AE, Karataş S. A case of primary hydatid cyst in the thyroid gland. Ulus Cerrahi Derg. 2015;31(2):94–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eken H, Isik A, Balci G, Firat D, Cimen O, Soyturk M. A rare case of isolated cystic hydatid of thyroid gland. Medicine (Baltimore). 2016;95(10): e2929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dissanayake PI, Chennuri R, Tarjan G. Fine-needle aspiration diagnosis of primary hydatid disease of the thyroid; first reported case in the USA. Diagn Cytopathol. 2016;44(4):334–7. [DOI] [PubMed] [Google Scholar]
- 17.El Bousaadani A, El Mahdoufi R, Roubal M, Mahtar M. Thyroid hydatid cyst: an unusual site. Eur Ann Otorhinolaryngol Head Neck Dis. 2016;133(1):75–6. [DOI] [PubMed] [Google Scholar]
- 18.Aydin S, Tek C, DilekGokharman F, Fatihoglu E, Nercis KP. Isolated hydatid cyst of thyroid: an unusual case. Ultrasound. 2018;26(4):251–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eshraghi M, Shahmoradi L, Ghoddoosi M, Sadati SJA. Diagnosis of primary hydatid cyst of thyroid gland: a case report. Biomol Concepts. 2019;10(1):106–10. [DOI] [PubMed] [Google Scholar]
- 20.Jiang T, Guo Q, Ran B, Zhang R, Aji T, Shao Y. Hydatid cyst of the thyroid gland with tracheal fistula: a case report and review of the literature. Exp Ther Med. 2019;18(1):573–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Salih AM, Abdulla ZY, Mohammed DA, Jwamer VI, Ali PG, Hamasaeed AG, et al. Hydatid cyst of thyroid gland, a rare case report with a literature review. Int J Surg Case Rep. 2020;67:267–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ghanem M, Al Kazzaz MZ, Soliman A. Hydatid cyst in the neck, an unusual localization of the disease: a case report. Int J Surg Case Rep. 2021;85: 106274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Safarpour MM, Aminnia S, Dehghanian A, Borazjani R, Abbassi HR, Boland Parvaz S, Paydar S. Primary hydatid cyst of the thyroid glands: two case reports and a review of the literature. J Med Case Rep. 2023;17:417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sultana N, Shah W, Ullah S, Ali M, Basharat S. Primary hydatid cyst of the thyroid gland: a case report. Ann Clin Pathol. 2016;4(3):1070. [Google Scholar]
- 25.Cossu ML, Palermo M, Coppola M, Fais E, Ruggiu M, Tanda F, Cossu Rocca P, Noya G. A case of primary hydatidosis of the thyroid gland. Panminerva Med. 1999;41(3):269–72. [PubMed] [Google Scholar]
- 26.Qadir AA, Abdullah IY, Ali MB, Mohammed RO, Dhair HM, Saeed YA, Muhialdeen AS, Kareem HO, Qaradakhy AJ, Ahmed SM, Ahmed SF. Presentation and management of thyroid hydatid cyst: a comprehensive systematic review of the literature. Barw Med J. 2024;2(1):56–62. [Google Scholar]
- 27.Lada P, Lermite E, Hennekinne-Mucci S, Etienne S, Pessaux P, Arnaud JP. Arnaud JP Kyste hydatique primaire de la thyroïde, localization inhabituelle de l’hidatidose. Presse Med. 2005;34(8):580. French. [DOI] [PubMed] [Google Scholar]
- 28.Danilă R, Ionescu L, Livadariu R, Vulpoi C, Ciobanu D. Ungureanu MC Kyste hydatique primaire de la thyroïde. Acta Endocrinol (Buc). 2015;11(4):529. French. [Google Scholar]
- 29.Hoysal DR, Kulkarni S. Maladie hydatique primaire isolée de la thyroïde se présentant comme un nodule solitaire : une maladie rare. Ind J Case Rep. 2019;5(1):79–81. French. [Google Scholar]
- 30.Bastanhagh MH, Fatourechi V, Rajabian R. Kyste hydatique se présentant comme un nodule thyroïdien : à propos de trois cas. Acta Med L’Iran. 1995;33(12):31–4. French. [Google Scholar]
- 31.Jain SK, Jamdade PT, Muneshwar SS, Ambulgekar VK, Panzade SM. Kyste hydatique de la thyroïde: une cause inhabituelle de stridor. Indien J Otolaryngol Chirurgie de la tête et du cou. 2005;57(1):80–1. French. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Azendour I, Boulaich M, Ayoubi A, Oujilal A, Essakalli L, Kzadri M. Kyste hydatique primaire de la glande thyroïde. Int J Otolaryngol. 2011;201(1):1–3. French. [Google Scholar]
- 33.Rajabian R, Tavassoli M, Ggiassi T. Shslib IM Kyste hydatique de la thyroïde. Méd J Répub Islam Iran (MJIRI). 1991;5(3):165–6. French. [Google Scholar]
- 34.Söğütlü G, Çıkım AS, Pişkin T, Dirican A, Mecit E, Kahraman L, Olmez A, Kırımlıoğlu V. Kyste hydatique dans la glande thyroïde : à propos d’un cas. Inönü Üniv Tip Fak Derg. 2007;14(3):185–7. French. [Google Scholar]
- 35.Erbil Y, Barbaros U, Baspinar I, Deveci U, Kapran Y, Bozbora A, Aral F, Özarmagan S. Kyste hydatique de la glande thyroïde : deux rapports de cas. Infect Dis Clin Entraînez-vous. 2005;13(6):318–20. French. [Google Scholar]
- 36.Özdemir A, Korkmaz A, Darcin H, Aras N. Kyste hydatique primaire de la glande thyroïde et autres localisations d’organes de la maladie. Turc Kline J Case Rep. 1989;7(3):195–9. French. [Google Scholar]
- 37.Avcu S, Ünal Ö, Kotan Ç, Öztürk M, Özen Ö. Atteinte sous-maxillaire et thyroïdienne des kystes hydatiques: une association très rare avec un traitement percutané. Diagn Interv Radiol. 2010;16(3):251. French. [DOI] [PubMed] [Google Scholar]
- 38.Amahzoune M, El Malki HO, Benkhraba K, Mohcine R, Ifrine L, Belkouchi A, Balafrej S. Kyste hydatique récidivant de la thyroïde : à propos d’un cas. Ann Endocrinol (Paris). 2004;65(5):469–71. French. [DOI] [PubMed] [Google Scholar]
- 39.Woolsey ID, Miller AL. Echinococcus granulosus sensu lato and Echinococcusmultilocularis: a review. Res Vet Sci. 2021;135:517–22. [DOI] [PubMed] [Google Scholar]
- 40.Sathekge MM, Muthuphei MN, Mandiwana I. Primary hydatidosis of the thyroid gland: a case report. S Afr J Radiol. 2018;3(3):a1572. 10.4102/sajr.v3i3.1572.
- 41.Valverde C, Lam J, Ibáñez P, Cruzat C. Neck hydatidosis. Thyroid and submaxillary gland involvement in 2 cases. Case Reports. Rev Med Chil. 1999;127(9):1108–11. Spanish. [PubMed]
- 42.Rauhofer U, Prager G, Hörmann M, Auer H, Kaserer K, Niederle B. Cystic echinococcosis of the thyroid gland in children and adults. Thyroid. 2003;13(5):497–502. 10.1089/105072503322021179. [DOI] [PubMed]
- 43.Zulfikaroglu B, Ozalp N, Keskek M, Koc M. Primary echinococcal cyst of the thyroid: report of a case. Surg Today. 2008;38:833–5. 10.1007/s00595-007-3796-x. [DOI] [PubMed]
- 44.Erkılıç S, Özsaraç C, Koçer NE, Bayazıt YA. Hydatid cyst of the thyroid gland in a child. Int J Pediatr Otorhinolaryngol. 2004;68(3):369–71. 10.1016/j.ijporl.2003.11.002. [DOI] [PubMed]
- 45.Çapoğlu İ, Ünüvar NE, Erdogan F, Yilmaz O, Caydere M. A hydatid cyst of the thyroid gland. J Int Med Res. 2002;30(2):206–9. 10.1177/147323000203000216. [DOI] [PubMed]
- 46.Ghawil M, Ben Omar N, Shatani A, Belhaj S, Doggah M. Primary hydatid cyst of the thyroid gland in a Libyan child. In: Hormone research in paediatrics (Vol. 96). Basel, Switzerland: Karger; 2023. p. 437.
- 47.Salih AM, Abdulla ZY, Mohammed DA, Jwamer VI, Ali PG, Hamasaeed AG, Shkur HH, Omer JK, Salih RQ, Mohammed SH, Muhialdeen AS, Mohammed K, Othman S, Kakamad FH. Hydatid cyst of thyroid gland, a rare case report with a literature review. Int J Surg Case Rep. 2020:67:267–70. 10.1016/j.ijscr.2020.02.019. [DOI] [PMC free article] [PubMed]
- 48.Bouomrani S, Souissi O, Regaieg N, BenHamed M. Primary hydatid cyst of the thyroid gland revealed by primary hypothyroidism. J Infect Dis Travel Med. 2(3).
- 49.Pérez PJA, Felmer EO, Carrasco EC, Gabrielli NM, Torrijos CC, Bastías NJA. Thyroid hydatid cyst: report of one case. Rev Med Chil. 2008;136(7):896–9. Spanish. [PubMed]
- 50.Chandra T, Prakash A. A case of hydatid cyst of thyroid. Br J Surg. 1965;52(3):235–7. 10.1002/bjs.1800520324. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available


