Abstract
Background
Extra ocular sebaceous carcinoma is a very rare, aggressive, malignant tumor arising in the adnexal epithelium of sebaceous gland that account for only about 25% of all sebaceous carcinomas (Wick et al. in Cancer 56(5):1163–72, 1985). The diagnosis of this tumor is difficult because its clinical appearance is atypical. The common treatment consists in wide local excision of the lesion with removal of local lymph node. We report the second case of sebaceous carcinoma involving the back. It was treated with surgical excision and sentinel lymph node biopsy.
Case presentation
A 69 year-old Caucasian woman presented with an erythematous, violaceus and exophytic lesion with central ulceration and leakage of purulent material in dorsal region at the level of T10–T11, measuring 7 × 6 cm in size. A biopsy of the lesion reported a moderately differentiated sebaceous carcinoma with lymph, vascular and perineural invasion. Extension studies revealed axillary lymphadenopathy and a renal lesion suggestive of angiomyolipoma based on tomographic findings. A biopsy of the axillary lymphadenopathy was performed, which was negative for malignancy. A wide excision of the lesion with a 2 cm margin and sentinel lymph node biopsy were performed. On histopathological examination was confirm the diagnosis of sebaceous carcinoma of the back. The patient had a good clinical course, and it was decided to follow up clinically every 6 months.
Conclusion
Sebaceous carcinoma can occur in locations other than the ocular region. It is frequently difficult to diagnose and has an unpredictable prognosis. The back is a particularly unusual site for this lesion. Surgery remains the mainstay of treatment, and a sentinel lymph node biopsy can be performed instead of removing all regional lymph nodes.
Keywords: Sebaceous carcinoma, Extraocular sebaceous carcinoma, Surgery, Sentinel lymph node biopsy, Case report
Introduction
Sebaceous carcinoma predominantly occurs in the ocular region. Extraocular presentations account for only about a quarter of the cases and can occur on the trunk, extremities, genitalia, lungs, salivary glands, and breast [1, 2]. However, extraocular manifestations usually include the skin of the head and neck region. Regardless of localization, it is important to accurately identify sebaceous carcinomas because they are considered aggressive neoplasms with potential for regional and distant metastases. The diagnosis of this tumor is complicated because it shows no pathognomonic gross or clinical characteristics, has a low incidence, and lacks a universally accepted histopathological classification. The treatment of this neoplasm consists of radical surgical excision with a 2-cm margin, achieving negative margins in approximately 95% of cases [3]. Additionally, lymphadenectomy is indicated, and in some cases, a sentinel lymph node biopsy could be an option to mitigate the morbidity associated with removing all local lymph nodes [4, 5]. However, there is insufficient data regarding the value of completion lymph node dissection after a biopsy of a suspicious lymph node; clinical judgment and multidisciplinary consultation are suggested to guide management [3]. Testing for Muir–Torre syndrome is recommended for individuals with a Mayo Muir–Torre syndrome risk score of 2 or higher.
There is still disagreement about the efficacy of adjuvant radiotherapy [5, 6]. Literature reports that tumors treated with a combination of surgery and radiotherapy include locally advanced primaries and those with positive margins or perineural invasion. Nevertheless, data regarding radiotherapy for perineural invasion and radiotherapy for the nodal basin in cases of confirmed lymph node involvement are too limited to draw firm conclusions about its efficacy [7–9].
The purpose of this review was to present a case of sebaceous carcinoma of the back and review literature on its histological characteristics, clinical behavior, and appropriate therapy. To the best of our knowledge, this is the second case described at this location. This case report has been prepared in accordance with the Surgical CAse REport (SCARE) criteria [4]
Case report
A 69 year-old Caucasian woman with a history of hypertension and diabetes mellitus presented with an erythematous, violaceus, and exophytic lesion with central ulceration and suppuration on the skin of the dorsal region at the level of T10–T11, measuring 7 × 6 cm in size (Fig. 1).
Fig. 1.

Clinical features of the lesion before surgical treatment
An incisional biopsy of the lesion reported a moderately differentiated sebaceous carcinoma with lymph, vascular and perineural invasion. No other skin lesions of the body were identified.
Staging studies were performed using computed tomography (CT) of the chest and abdomen, which incidentally revealed a lesion suggestive of an angiolipoma in the left kidney. In the chest, a pulmonary nodule was identified in the lower left lobe, with low suspicion and nonspecific characteristics. Additionally, an axillary ultrasound was performed, revealing axillary adenopathy, for which a fine-needle aspiration biopsy was conducted, and it was negative for malignancy.
The clinical differential diagnosis included squamous cell carcinoma, melanoma, and basal cell carcinoma with sebaceous differentiation.
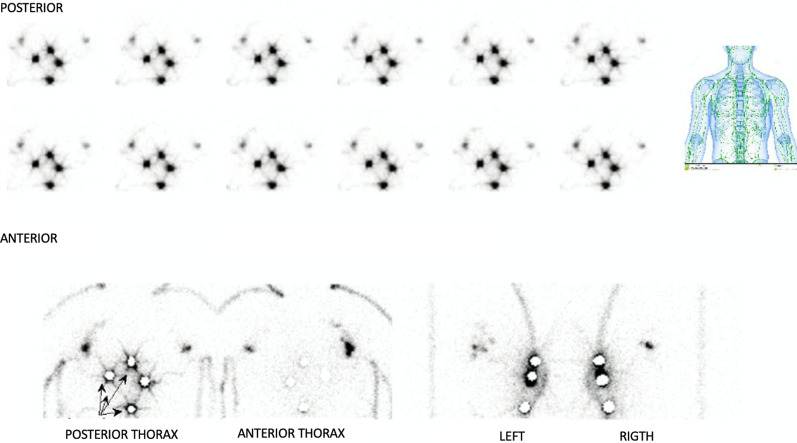
Preoperative lymphoscintigraphy demonstrated drainage to the left axillary sentinel lymph node (Fig. 2). Surgical management was indicated, and the procedure was performed under general anesthesia. A wide local excision with a 2-cm margin and resection of the left axillary sentinel lymph node was conducted. The skin defect required closure with rotational flaps, involving the participation of the plastic surgery team (Fig. 3). There were no complications in the postoperative period.
Fig. 2.
Preoperative lymphoscintigraphy. Note an axillary left sentinel lymph node
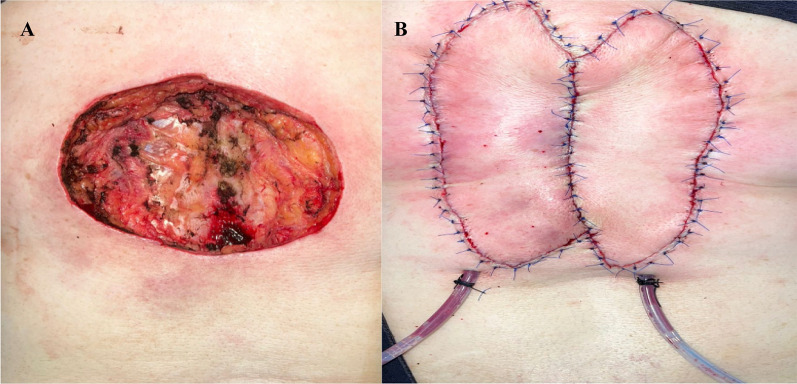
Fig. 3.
Findings after excision of the lesion. A excision of the neoplasm with 2 cm of free margins. B Appearance after closure of the defect by plastic surgery
The pathologic examination revealed a skin fragment measuring 9.5 × 8.5 cm in surface area, with 3 cm of subcutaneous tissue. A large exophytic mass with a broad, indurated, whitish/yellowish base and lobed appearance measuring 9 × 8 × 4 cm was identified.
Histopathological examination showed a large tumoral lesion that ulcerates the epidermis and infiltrates deeply, compromising the full thickness of the dermis and subcutaneous fatty tissue. The tumor forms lobules consisting mainly of basaloid cells, accompanied by clear cells, some of which exhibit frank sebaceous differentiation. Basaloid cells tend to be located at the periphery of the tumor lobules, while clear cells are found toward the center, where squamous morulae are also identified. There is moderate nuclear pleomorphism, increased mitotic activity, and foci of necrosis. There is no evident lymphatic, vascular, or perineural invasion.
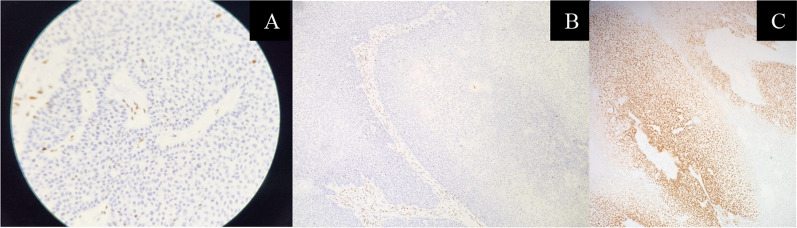
Neoplastic cells were positive for CKAE1/AE3, androgen receptors, and EMA, but negative for Ber-EP4. There was preserved expression for MLH1 and PMS2, but loss of expression for MSH2 and MSH6 (Fig. 4).
Fig. 4.
Immunohistochemistry. A Loss of expression of MSH2. B Loss of expression of MSH6. C Neoplastic cells positive for androgen receptors
In consideration of these findings, a pathological diagnosis of a moderately differentiated extraocular sebaceous carcinoma of the back with loss of expression of MSH2 and MSH6 proteins was made. The sentinel lymph node biopsy reported two lymph nodes negative for metastatic involvement. Because no metastases were detected, no further treatment was necessary and biannual clinical follow-up was considered.
Discussion
Sebaceous carcinoma is an uncommon malignant neoplasm, accounting for approximately 0.2–4.6% of cutaneous neoplasms [5], typically arising from the eyelid epithelium, with extraocular manifestation is an exceedingly uncommon occurrence. Extraocular manifestations are predominantly observed in older adults and women [2], with a predilection for the head, neck, and trunk. The presentation site in this case, the back, is one of the rarest, with only one other reported case in literature.
The loss of MSH2 and MSH6 protein expression is frequently observed in sebaceous carcinomas. These proteins are involved in DNA mismatch repair, and their loss can lead to the accumulation of genetic mutations that contribute to tumorigenesis. Loss of MSH2 and MSH6 protein expression is associated with a more aggressive clinical course and a higher risk of recurrence and metastasis [6].
Additionally, on the basis of preoperative lymphoscintigraphy that identified a left sentinel lymph node, the sentinel lymph node was removed for histological studies; considering that the most common site of metastasis is the draining lymph node [5], with reported involvement in 10–28% of cases [7]. It is also important to consider the risk of metastatic involvement; according to Bailet et al. and Pnajwani et al. [2, 6], the risk of distant metastases is reported to be between 20% and 25%, with the main sites including the abdomen, lung, brain, bone, and subcutaneous tissue. Our patient presented with two visceral lesions of low suspicion based on their imaging characteristics on CT scans: a pulmonary nodule and a renal mass. Therefore, close follow-up is necessary to assess the behavior of these lesions, given the suspicion of Muir–Torre syndrome, a variant of Lynch syndrome characterized by the coexistence of sebaceous tumors with visceral tumors [8]. Therefore, imaging surveillance and identification of personal and family risk factors for colorectal cancer are warranted, as recommended by Roberts et al. [9]. Given this suspicion, genetic counseling should be considered.
On the basis of the literature review and the decision of a multidisciplinary tumor board, it was concluded that the patient would not benefit from adjuvant treatments, such as radiotherapy or chemotherapy. However, decisions should be made in consultation with experienced teams, tailored to each individual case, owing to the lack of strong evidence justifying any of the available therapeutic alternatives.
Conclusion
Sebaceous carcinoma can manifest outside the ocular region, posing diagnostic challenges and exhibiting an unpredictable prognosis. The occurrence of this lesion on the back is exceptionally rare. In our case, postoperative chemotherapy and radiotherapy were omitted due to negative tumor margins and absence of lymph node metastasis on pathology. Surgery remains the mainstay of treatment, and sentinel lymph node biopsy can be performed instead of removing all regional lymph nodes. Nevertheless, the efficacy of adjuvant therapies, such as radiotherapy, for regional lymph nodes in cases with confirmed lymph node involvement remains uncertain, warranting further investigation.
Acknowledgements
Department of Plastic Surgery, School of Medicine, Pontificia Universidad Javeriana, Hospital Universitario San Ignacio, Bogotá D.C., Colombia. Department of Pathology, School of Medicine, Pontificia Universidad Javeriana, Hospital Universitario San Ignacio, Bogotá D.C., Colombia
Author contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas. All authors took part in drafting, revising or critically reviewing the article, gave final approval of the version to be published, have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Availability of data and materials
No applicable.
Declarations
Ethics approval and consent to participate
We received approval from the ethics committee of the Faculty of Medicine, Pontificia Universidad Javeriana. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wick MR, Goellner JR, Wolfe JT, Su WP. Adnexal carcinomas of the skin. II. Extraocular sebaceous carcinomas. Cancer. 1985;56(5):1163–72. [DOI] [PubMed] [Google Scholar]
- 2.Panjwani PK, Tirumalae R, Crasta JA, Manjunath S, Rout P. Extraocular sebaceous carcinoma: a series of three cases with varied presentation. Dermatol Pract Concept. 2012;2(1):39–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Owen JL, Kibbi N, Worley B, Kelm RC, Wang JV, Barker CA, et al. Sebaceous carcinoma: evidence-based clinical practice guidelines. Lancet Oncol. 2019;20(12):e699–714. [DOI] [PubMed] [Google Scholar]
- 4.Agha RA, Borrelli MR, Farwana R, Koshy K, Fowler AJ, Orgill DP, et al. The SCARE 2018 statement: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg. 2018;60:132–6. [DOI] [PubMed] [Google Scholar]
- 5.Mohamed M, Boussofara L, Slama A, Denguezli M, Belajouza C, Sriha B, et al. Extra-ocular sebaceous carcinoma of the skin: a report of five cases and a review of the literature. Am J Med Case Rep. 2015;3(9):291–6. [Google Scholar]
- 6.Moreno C, Jacyk WK, Judd MJ, Requena L. Highly aggressive extraocular sebaceous carcinoma. Am J Dermatopathol. 2001;23(5):450–5. [DOI] [PubMed] [Google Scholar]
- 7.Knackstedt T, Samie FH. Sebaceous carcinoma: a review of the scientific literature. Curr Treat Options Oncol. 2017;18(8):47. [DOI] [PubMed] [Google Scholar]
- 8.Shah RR, Allman P, Schwartz RA. Muir-torre syndrome: a cutaneous finding amidst broader malignancies. Am J Clin Dermatol. 2023;24:375–80. [DOI] [PubMed] [Google Scholar]
- 9.Roberts ME, Riegert-Johnson DL, Thomas BC, Rumilla KM, Thomas CS, Heckman MG, et al. A clinical scoring system to identify patients with sebaceous neoplasms at risk for the Muir-Torre variant of Lynch syndrome. Genet Med. 2014;16(9):711–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No applicable.