Abstract
Background
The anatomical structure of the elbow joint makes it vulnerable to contractures. While elbow arthroscopy minimizes soft tissue damage and enhances early rehabilitation, the optimal duration for postoperative Continuous Passive Motion (CPM) therapy is unclear. This retrospective study aims to establish the appropriate duration of CPM following arthroscopic elbow contracture release.
Methods
We analyzed postoperative outcomes from patients undergoing CPM rehabilitation for 1, 3, or 5 months. Metrics such as ASES, VAS, DASH, MEPS scores, grip strength, and range of motion were assessed before surgery and at 1,3,6 and 12 months post-surgery.
Results
Patients who received 3 or 5 months of CPM therapy showed statistically significant improvements in elbow flexion-extension, range of motion, and functional scores (ASES, VAS, DASH, MEPS) compared to the 1-month group (p < 0.05). However, no significant differences were observed between the 3- and 5-month groups.
Conclusions
A 3-month CPM period is effective for patients with higher functional demands, with no additional benefit from extending therapy to 5 months.
Keywords: Contracture release, Elbow Joint Rehabilitation, Range of Motion Enhancement, Postoperative recovery, Joint stiffness
Background
The unique anatomical structure of the elbow joint makes it particularly vulnerable to contractures, which can significantly restrict joint mobility and cause functional impairment [1]. Elbow arthroscopy offers several advantages in treating elbow contractures, such as minimal soft tissue disruption, clear visualization of joint structures, and the facilitation of early postoperative rehabilitation [2, 3]. However, effective rehabilitation is just as critical as surgery in achieving optimal outcomes, with CPM playing a pivotal role in the recovery process.
CPM has been widely used in clinical practice to improve postoperative outcomes, particularly in patients recovering from elbow contracture release [4]. The key mechanisms through which CPM accelerates recovery include the prevention of scar tissue and adhesion formation [5], reduction of inflammation [4], promotion of blood circulation and tissue repair [6]and reduction of pain and swelling [7]. By continuously mobilizing the joint, CPM helps maintain the range of motion achieved during surgery, prevents the accumulation of inflammatory mediators that contribute to fibrosis, and promotes faster healing of the surrounding tissues through improved blood flow. Additionally, CPM has been shown to reduce postoperative pain and swelling, which facilitates quicker recovery of joint function, especially in flexion and extension movements [8].
Despite the widespread use of CPM, the optimal duration for postoperative CPM therapy following arthroscopic release of elbow contracture has yet to be determined. Existing studies have demonstrated the effectiveness of CPM in improving joint function and reducing recovery time, but there is no consensus on how long CPM should be applied to maximize benefits. Therefore, this retrospective study aims to investigate the appropriate duration of postoperative CPM therapy to enhance functional recovery, improve range of motion, and reduce pain in patients undergoing elbow arthroscopy for contracture release.
Methods
Study design
This is a cohort, retrospective study. After the approval of the Wuxi Ninth People’s Hospital, medical records of 104 patients who were diagnosed with elbow stiffness between January 1, 2021, and December 31, 2023, were reviewed. They were outpatients at a sports medicine clinic of the Wuxi Ninth People’s Hospital. All patients underwent a standardized history and physical examination by the lead author: passive and active range of motion, functional rating scale, forearm circumference, and grip strength. Inclusion criteria were as follows: (1) Patients who have a lack of elbow flexion and extension causing functional impairment that has been present for at least 6 months; (2) There is no effective treatment except for operation; (3) Patients who are 18 years of age or older; (4) Patients who are scheduled to accept an Elbow Arthroscopic Osteocapsular Arthroplasty (AOA) or Capsulectomy. Exclusion criteria were as follows: (1) Patients with bleeding disorders, long-term use of anticoagulants, and other conditions that interfere with performing postoperative elbow CPM training; (2) Patients with progressive or recalcitrant neuropathy or neuritis; (3) Muscle strength of the affected limb less than or equal to grade 3; (4) Patients who do not have standardized CPM training or who cannot afford CPM rehabilitation training; (5) Patients with anatomical abnormalities of the elbow joint who are unable to perform normal upper limb activities; (6) Patients with intraoperative elbow infections or previous infections affecting function.; (7) Patients without adequate postoperative analgesia in the elbow region; (8) Patients with limited movement of the shoulder and wrist joints affecting the functional movement of the elbow joints.
The diagnosis of elbow contracture is based on the presence of marked limitation of elbow motion including flexion and extension with muscle tension, pain and discomfort, increased muscle tone, joint erythema and tenderness, and neurological symptoms, with imaging suggestive of capsular contracture, bony growth in the ulnar fossa of the hawksbill fossa, and ectopic ossification in the vicinity of the elbow joint.
Arthroscopic release
In this study, a cohort of 104 patients who underwent elbow arthroscopic release between 2021 and 2023 was recruited. However, due to non-completion of the rehabilitation program and loss to follow-up, only 50 patients were included in the final analysis. All patients scheduled for elbow arthroscopic release underwent at least 1 month of preoperative physiotherapy without significant benefit. The arthroscopic release procedure followed a standard surgical technique. The first step of the procedure involved identifying and protecting the ulnar nerve. The second step involved manipulating the posterior cubital compartment to remove debris and free bodies, excise fat pads, and perform synovectomy if deemed necessary, followed by the removal of osteophytes and restoration of the olecranon to its normal shape. The third step involved manipulating the anterior cubital compartment, incising the scar, osteophyte, and anterior joint capsule. Elbow arthrodesis was performed based on the degree of loss of range of motion of elbow flexion, with the medial gutter being cleared first, followed by the lateral gutter. The fourth step involved checking elbow flexion-extension after the arthroscopic device was removed, and the postoperative range of motion was measured. Finally, the wound was sutured without placing drains, and the elbow joint was fixed in a straight position with a brace [9]. Intraoperative care was taken to protect the nerve, and ulnar nerve release was performed in each operation of experimental patients to prevent delayed-onset ulnar neuritis [10]. Subcutaneous ulnar nerve translocation was only performed if ulnar neuropathy was present preoperatively. The same experienced sports medicine surgeon performs all surgeries.
Continues passive motion
Following the surgical procedure, patients across all cohorts were administered continuous brachial plexus block for 48 h to alleviate the pain. The CPM intervention was performed in the hospital within 24 h of the surgical procedure, for at least four hours per day. Patients were discharged from the hospital on the third day after surgery, with a 21-day prophylactic dose of indomethacin to prevent heterotopic ossification and opioid medication to manage breakthrough pain [11–14].
Following hospital discharge, patients are given the option to continue CPM rehabilitation at home. Prior to discharge, both the patient and their caregivers receive comprehensive training from a professional sports rehabilitation therapist on the correct and safe use of the CPM device (CANWELL JK-H2 Elbow CPM Machine), including its setup, angle adjustments, and time scheduling. It is recommended that patients establish a dedicated, quiet, and comfortable rehabilitation space at home, with sufficient room to accommodate the equipment. Patients are required to engage in at least four hours of CPM therapy daily, with each session involving three-minute holds at maximum flexion and extension, followed by repetitive flexion-extension movements. To avoid fatigue or discomfort from prolonged sessions, patients are encouraged to divide the training into multiple intervals.
During the rehabilitation period, if patients experience significant pain, they are advised to promptly communicate with their physician via a mobile application to ensure appropriate pain management. The app also serves as a platform for patients to report their daily training progress and any discomfort experienced during the sessions. Based on this feedback, the physician or rehabilitation therapist can adjust the treatment plan as necessary. Additionally, weekly virtual check-ins are conducted by the rehabilitation therapist to ensure proper execution of the training regimen and to provide remote guidance when needed. The involvement of family members plays a critical role in the home rehabilitation process, as they assist with device adjustments, remind patients to adhere to the prescribed schedule, and monitor the patient’s condition.
Despite the option for home-based rehabilitation, patients are required to attend monthly follow-up visits at the hospital, where the physician will assess joint function, pain levels, and adjust the rehabilitation plan accordingly. Through professional remote supervision and active involvement of family members, patients are able to achieve rehabilitation outcomes at home comparable to those of in-hospital therapy, thus facilitating a successful recovery of joint function.
Outcome measurements
Compare the elbow flexion, extension, range of motion, pronation-supination arc, grip strength, American Shoulder and Elbow Surgeons (ASES) function score, Visual Analog Scale (VAS) score, Disabilities of the Arm, Shoulder and Hand (DSAH) score, and Mayo Elbow-Performance Score (MEPS) of patients who underwent CPM rehabilitation training for 1 month, 3 months, and 5 months following arthroscopic contracture release surgery, measured at four-time points: 1 month, 3 months, 6 months, and 12 months post-surgery.
The ASES elbow joint function score is comprised of eight components, encompassing both self-assessment by the patient and assessment by the physician during a physical examination. It encompasses various indicators of the patient’s elbow joint functionality and their ability to perform daily activities. A higher score indicates better function [15]. The DASH score is a patient self-assessment scale designed to evaluate upper limb dysfunction, featuring 30 indicators related to daily activities and 7 indicators of upper limb discomfort symptoms. Each indicator is rated on a 5-level scale, ranging from effortless (1 point) to impossible (5 points). A higher score indicates more severe dysfunction [16]. MEPS is a functional assessment tool primarily based on medical examinations, covering evaluations of elbow pain, motion, and stability. A lower score reflects more severe impairment [17]. VAS assesses a patient’s pain by asking them to look at a scale marked with numbers from 0 to 10, where 10 represents unbearable pain and 0 indicates no pain. The patient can simply say a number [18].
The range of motion of the patient’s elbow was assessed using a joint measuring ruler, encompassing maximum flexion, extension, and rotation. Each movement was assessed three times, with the average serving as the final result. The values measured during brachial plexus block anesthesia following intraoperative release represent the passive motion angles achieved by the surgeon’s assistance. Grip strength was assessed using a handheld grip device on both hands of the patient. Each measurement was repeated three times, with the average serving as the final result. The final ratio is presented as the percentage of grip strength on the affected side compared to that on the healthy side. Forearm circumference was measured 1.5 cm distally from both lateral epicondyles. Bilateral upper limb measurements were conducted, with each repetition yielding an average value. The final figure represents the difference in forearm circumference between the affected and healthy sides.
Statistical analysis
Comparing the demographic characteristics of the three groups of patients, categorical variables were analyzed using the chi-square test or Fisher’s exact test, depending on the type of data collected, while continuous variables were analyzed using analysis of variance (ANOVA) or Kruskal-Wallis tests. For comparisons of outcomes across multiple time points within the same group (e.g., preoperative, 1 month, 3 months, 6 months, and 12 months postoperatively), repeated measures ANOVA was utilized to account for intra-subject correlations. For comparisons between different groups at the same time point, one-way ANOVA was conducted to detect differences among the groups. The ASES-function score, DASH score, VAS score, ASES score, and MEPS score were compared using these ANOVA methods. A p-value less than 0.05 was considered statistically significant. These statistical analyses were conducted using GraphPad Prism 10 and SPSS Statistics 24.0 software.
Results
This study examined cases that underwent arthroscopic contracture release of the elbow from January 1, 2022, to December 1, 2023. Among the 104 cases meeting the inclusion criteria, 23 lacked complete follow-up information, 31 did not finish the required CPM rehabilitation training, and 50 were ultimately included in the analysis. Within this group, 18 cases underwent CPM training for 1 month (CPM 1 m), 20 for 3 months (CPM 3 m), and 12 for 5 months (CPM 5 m).
The duration of postoperative CPM training for patients is determined based on their functional needs and the doctor’s recommendations. The basic characteristics and surgical indications of the three groups of patients are similar and are listed in Table 1.
Table 1.
Demographic and baseline characteristics of the patients and Operative Data
| Characteristic | CPM 1 M (N = 18) | CPM 3 M (N = 20) | CPM 5 M (N = 12) | All Patients (N = 50) |
|---|---|---|---|---|
| Age (yr) | ||||
|
Mean and standard deviation Range |
47.8 ± 11.7 27–70 |
41.8 ± 17.4 14–71 |
46.6 + 12.5 26 ~ 71 |
45 ± 15 14–71 |
| Sex (no. of patients) | ||||
|
Male Female |
13(72%) 5(28%) |
16(80%) 4(20%) |
6(50%) 6(50%) |
35(70%) 15(30%) |
| Elbow contracture etiology (No. of patients) | ||||
|
Primary osteoarthritis Posttraumatic Inflammatory |
13(72%) 2(11%) 3(17%) |
12(60%) 5(25%) 3(15%) |
8(67%) 2(17%) 2(17%) |
33(66%) 9(18%) 8(16%) |
| Preoperative arc of elbow motion (deg) | ||||
|
Mean and standard deviation Range |
58.39 ± 9.77 41–75 |
59.55 ± 9.21 40–72 |
61.33 ± 6.58 51–69 |
59.56 ± 8.78 40–75 |
| Severity of elbow contracture (No. of patients) | ||||
|
Mild (arc > 90°) Moderate (arc 61°-90°) Severe (arc 31°-60°) Very severe (arc ≤ 30°) |
0(0%) 7(17%) 11(78%) 0(0%) |
0(0%) 12(35%) 8(65%) 0(0%) |
0(0%) 8(67%) 4(33%) 0(0%) |
0(0%) 27(54%) 23(46%) 0(0%) |
|
History of previous surgery for elbow contracture (no. of patients) |
||||
|
No Yes |
15(83%) 3(17%) |
13(65%) 7(35%) |
10(83%) 2(17%) |
38(76%) 12(24%) |
| Operative data (no. of patients) Type of elbow contracture release | ||||
|
Osteocapsular arthroplasty Capsular release (soft tissue only) |
14(78%) 4(22%) |
13(65%) 7(35%) |
9(75%) 3(25%) |
36(72%) 14(28%) |
| Ulnar nerve management | ||||
|
Limited decompression Subcutaneous transposition |
14(78%) 4(22%) |
17(85%) 3(15%) |
10(83%) 2(17%) |
41(82%) 9(18%) |
| Additional surgical procedures | ||||
|
Removal of heterotopic ossification Radial head excision with or without interposition arthroplasty Hardware removal Other procedures |
11(61%) 0(0%) 1(5%) 0(0%) |
16(80%) 0(0%) 0(0%) 0(0%) |
8(67%) 0(0%) 0(0%) 0(0%) |
35(70%) 0(0%) 1(2%) 0(0%) |
| Tourniquet time (min) | ||||
|
Mean and standard deviation Range |
81.32 ± 15.93 45–105 |
83.37 ± 15.38 54–112 |
86.08 ± 13.17 62–107 |
83.24 + 14.91 45–112 |
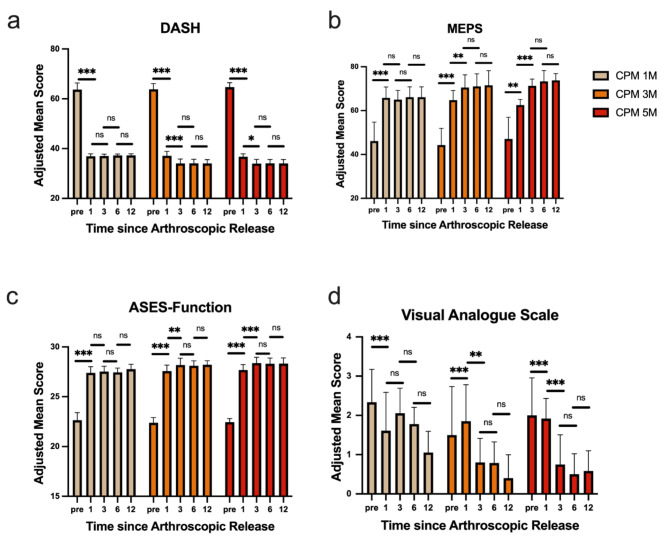
Patients in the CPM 1 M group experienced a significant reduction in DASH scores from pre-operative to 1-month post-operative(p < 0.001), with no significant differences observed at 1,3,6 or 12 months post-operative(p > 0.05). Similarly, the DASH scores for patients in the CPM 3 M and CPM 5 M groups also showed a significant reduction from pre-operative to 1 month post-operative(p < 0.001), with no notable changes at 3 months post-operative(p > 0.05). There were no significant changes in DASH scores at 3,6 or 12 months post-operative (p > 0.05, Fig. 1a). MEPS scores for all three groups increased significantly pre- and postoperatively (p < 0.001), with no notable changes observed in the CPM 1 M group at 1, 3, 6, or 12 months postoperative (p > 0.05). The CPM 3 M and CPM 5 M groups demonstrated a significant increase in MEPS scores at 3 months postoperative compared to 1 months postoperative (p < 0.01), with no significant changes observed at 6 or 12 months (p > 0.05, Fig. 1b). ASES function scores for all three groups of patients showed a significant increase from pre-operative levels to 1 month post-operative(p < 0.001). There were no significant differences in ASES function scores between the CPM 1 M group at 1 month, 3 months, 6 months, and 12 months post-operatively(p > 0.05). The ASES function scores for the CPM 3 M and CPM 5 M groups showed a significant increase at 3 months post-operative compared to 1 month post-operative(p < 0.01), with no significant changes observed at 3 months, 6 months, and 12 months post-operatively (p > 0.05, Fig. 1c). VAS scores for all three groups of patients showed a significant reduction from pre-operative levels to 1 month post-operative(p < 0.001). There were no significant differences in VAS scores between the CPM 1 M group at 1 month, 3 months, 6 months, and 12 months post-operatively(p > 0.05). The VAS scores for the CPM 3 M and CPM 5 M groups showed a significant decrease at 3 months post-operative compared to 1 month post-operative(p < 0.01), with no significant changes observed at 3 months, 6 months, and 12 months post-operatively (p > 0.05, Fig. 1d).
Fig. 1.
The changes in functional scores for the three groups of patients over time following elbow release surgery. (a) DASH scores for the three groups before and 1,3,6 and 12 months post-surgery. (b) MEPS scores for the three groups before and 1,3,6 and 12 months post-surgery. (c) ASES-Function scores for the three groups before and 1,3,6 and 12 months post-surgery. (d) VAS scores for the three groups before and 1,3,6 and 12 months post-surgery. pre: pre operation *:p < 0.05; **:p < 0.01;***:p < 0.001,NS: Not Statistically
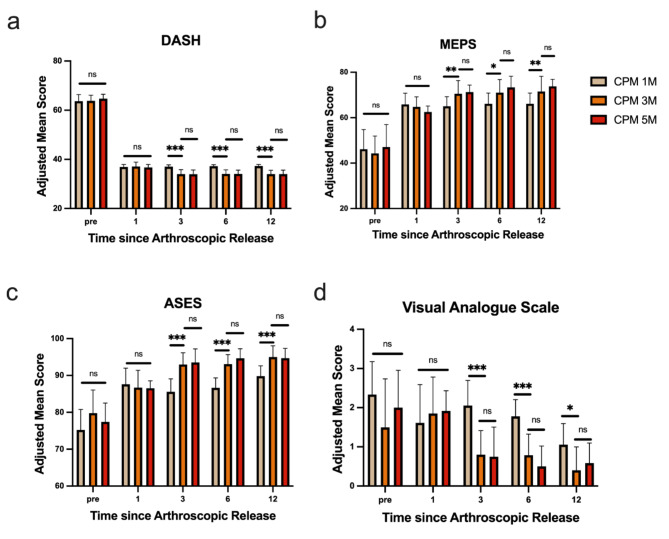
There were no significant differences in DASH score, MEPS, ASES-function score, and VAS among the three groups of patients before and 1 month after surgery(p > 0.05). However, significant differences were observed in these scores between the CPM 1 M group and the CPM 3 M and CPM 5 M groups at 3 months, 6 months, and 12 months post-surgery(p < 0.05). There were no significant differences noted between the CPM 3 M and CPM 5 M groups. (p > 0.05, Fig. 2a-d).
Fig. 2.
Comparison of functional assessment among three groups of patients before and after elbow joint release surgery at various time points. (a) Difference in DASH scores among the three groups before and 1,3,6 and 12 months post-surgery. (b) Difference in MEPS scores among the three groups before and 1,3,6 and 12 months post-surgery. (c) Difference in ASES-Function scores among the three groups before and 1,3,6 and 12 months post-surgery. (d) Difference in VAS scores among the three groups before and 1,3,6 and 12 months post-surgery. pre: pre operation *:p < 0.05; **:p < 0.01;***:p < 0.001, NS: Not Statistically
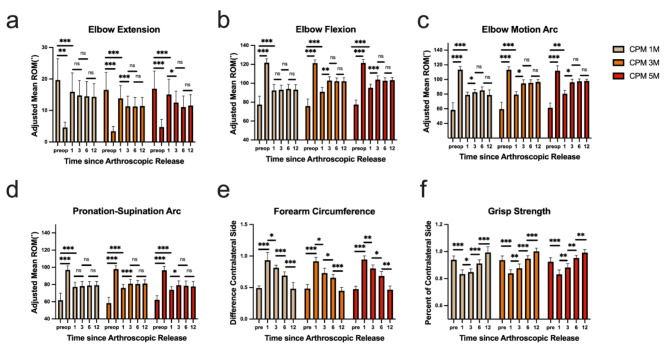
The extension and flexion angles of the elbow joint, as well as the ranges of motion and forearm rotation, measured under anesthesia after surgery, showed significant improvements in all three patient groups compared to their pre-operative levels(p < 0.01). 1 month post-surgery, significant differences were observed in the extension and flexion angles of the elbow joint, as well as in range of motion and forearm rotation among the three groups(p < 0.05). However, the CPM 1 M group did not show any significant differences at 1,3,6 and 12 months post-surgery. The forearm rotation range improved at 3 months post-surgery compared to 1 month, with no significant changes thereafter(p > 0.05). The CPM 3 M and CPM 5 M groups exhibited significant differences in elbow extension, flexion, and forearm rotation angles at 3 months post-surgery compared to 1 month(p < 0.05), with no notable changes afterwards(p > 0.05). (Fig. 3a-d) There were significant differences in forearm circumference and grip strength among the three groups post-surgery, with notable improvements noted at all subsequent measurements: 1, 3, 6, and 12 months after surgery. (p < 0.05, Fig. 3e-f)
Fig. 3.
Changes in elbow joint parameters over time before and after release surgery in three groups. (a) The elbow flexion degrees of the three groups before, during, and 1, 3, 6, and 12 months after surgery. (b) The elbow extension degrees of the three groups before, during, and 1, 3, 6, and 12 months after surgery. (c) The elbow range of motion of the three groups before, during, and 1, 3, 6, and 12 months after surgery. (d) The rotation degrees of the forearm before, during, and 1, 3, 6, and 12 months after surgery in the three groups. (e) The forearm circumference of the three groups before surgery and at 1, 3, 6, and 12 months after surgery. (f) The grip strength of the three groups before surgery and at 1, 3, 6, and 12 months after surgery. pre: pre operation; op:in operation *:p < 0.05; **:p < 0.01;***:p < 0.001, NS: Not Statistically
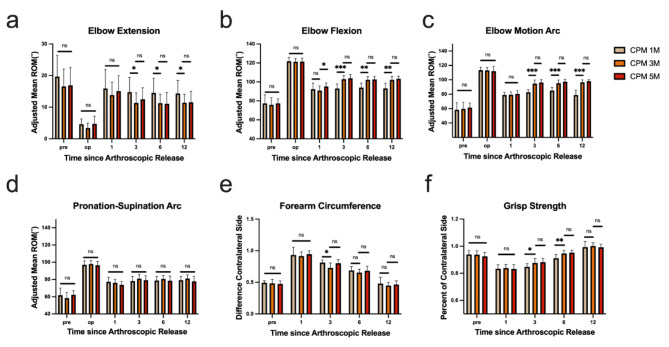
No significant differences were found in the elbow joint extension and flexion angles, as well as the range of motion, among the three groups before, during, and 1 month after the release surgery under anesthesia(p > 0.05). The CPM 3 M group showed significant differences in the elbow joint extension and flexion angles, range of motion, and forearm rotation compared to the CPM 1 M group at 3,6 and 12 months post-surgery(p < 0.05). However, there were no significant differences between the CPM 5 M group and the CPM 3 M group(p > 0.05). Forearm rotation range did not show significant differences among the three groups at each time point (p > 0.05, Fig. 4a-d). At 3 months post-surgery, the CPM 3 M group displayed a difference in forearm circumference compared to the CPM 1 M group(p < 0.05). Furthermore, no significant differences were observed in any individual component before surgery, 1 month post-surgery, or at 6 or 12 months post-surgery (p > 0.05, Fig. 4e). Grip strength did not differ significantly between the three groups before and 1 month after surgery(p > 0.05). Significant differences in grip strength between the CPM 3 M group and the CPM 1 M group were observed at 3 and 6 months post-surgery(p < 0.05); however, no significant differences were noted between the CPM 3 M and CPM 5 M groups(p > 0.05). At 12 months post-surgery, grip strength did not differ significantly among the three groups (p > 0.05, Fig. 4f).
Fig. 4.
Comparison of elbow joint movement parameters among three groups of patients at different time points before and after the release surgery. (a) Differences in elbow flexion degrees among the three groups were observed before surgery, during the operation, and at 1,3,6 and 12 months post-surgery. (b) Differences in elbow extension degrees among the three groups were observed before surgery, during the operation, and at 1,3,6 and 12 months post-surgery. (c) Variations in elbow joint range of motion among the three groups were noted before, during, and at 1,3,6 and 12 months post-surgery. (d) Rotation degrees of the forearm varied among the three groups before surgery, during the operation, and at 1,3,6 and 12 months post-surgery. (e) Forearm circumference differences were observed among the three groups before surgery and at 1,3,6 and 12 months post-surgery. (f) Grip strength variations among the three groups were noted before surgery and at 1,3,6 and 12 months post-surgery. pre: pre operation; op:in operation *:p < 0.05; **:p < 0.01;***:p < 0.001, NS: Not Statistically
Undergoing 3 or 5 months CPM training post-surgery can lead to a superior and accelerated recovery of elbow joint function compared to 1 month training, which enhances patients’ adaptability to life and better fulfills their daily living needs. However, extending CPM training beyond 3 months does not significantly improve the daily function of the patient’s elbow joint. It is hypothesized that patients with heightened functional needs benefit most from a 3-month CPM training following arthroscopic release surgery, as extending rehabilitation to 5 months does not significantly improve postoperative elbow joint motion or functional activities.
Discussion
Pathological changes in elbow contracture often involve the thickening of soft tissues, especially the joint capsule, leading to a decrease in elbow joint motion [8]. These thickened joint capsules typically resemble scar tissue, which is known to originate from mesenchymal stem cells [19]. Cohen et al. noted that contracture-affected elbow joints exhibit significant thickening of the joint capsule, along with structural changes in the extracellular matrix, disruptions in inflammatory factors, and fibroblast infiltration, creating a localized inflammatory fibrosis environment that worsens elbow stiffness [7]. Hildebrand et al. found a notable increase in fibroblast infiltration into relaxed muscles after joint capsule release procedures, resulting in capsule thickening, with anterior capsule thickening being more pronounced than the posterior side [6]. Studies suggest that the extent of fibroblast infiltration is inversely related to the range of motion in the elbow joint. However, in patients with elbow stiffness lasting over five months, local fibroblasts may decrease or disappear, indicating a potential role primarily in the early stages of the disease progression [20–22]. O’Driscoll et al. proposed that joint stiffness primarily involves four stages: (1) Bleeding, (2) Edema, (3) Granulation Tissue, (4) Fibrosis. During this phase, the swelling and bleeding of the elbow joint lead to the release of numerous inflammatory factors, which promote the deposition, maturation, and fibrosis of granulation tissue. An increase in type 1 collagen in the extracellular matrix exacerbates the stiffness of the elbow joint. These pathological changes primarily occur in the weeks or months following trauma or surgery; thus, preventive measures for these processes should be initiated promptly following arthroscopic release of contracture in the elbow [5]. The theory suggests that postoperative bleeding-induced hematomas and granulation tissue formation may be critical factors in elbow stiffness. Immediate postoperative CPM effectively eliminates local hematomas and fluid accumulations, reduces the accumulation of local inflammatory factors and mesenchymal stem cells, and effectively controls the deposition and fibrosis of granulation tissue. However, months later, when granulation tissue has matured and fibrosis has progressed, continued CPM training does not effectively inhibit the formation of dense and hardened scar tissue, resulting in no significant improvement in elbow joint range of motion.
A prolonged and rigorous rehabilitation protocol after elbow release is crucial for preserving the arc of motion achieved during surgery [23]. Previous research has demonstrated that CPM rehabilitation can significantly enhance elbow function in patients post-arthroscopic release of elbow contracture [4]. However, the implementation of CPM requires substantial time, effort, and financial investment. While existing studies support the effectiveness of CPM in enhancing function, there is a lack of consensus on the optimal duration of CPM training following arthroscopic release of elbow contracture. This study aimed to compare the outcomes of patients undergoing CPM rehabilitation for 1 month, 3 months, and 5 months post-surgery, with a maximum follow-up period of 1 year. The results showed that extending CPM training to 3 months post-surgery led to significant improvements in elbow function, including flexion, extension, range of motion, and grip strength. Additionally, it helped alleviate postoperative pain and expedited the reduction of swelling in the forearm and elbow joint. However, there was no notable enhancement in forearm rotational function. The functional activities of the elbow joint primarily depend on flexion and extension movements [24]. Although there was a statistically significant increase in the extension angle post-surgery, this did not result in significant functional benefits for the patients. However, the notable increase in flexion angle significantly improved elbow function. Therefore, extending postoperative CPM time appropriately enhances elbow flexion function improvement. Extending CPM training to 5 months did not show further improvements in the mentioned functions.
This study provides critical clinical insights for the postoperative rehabilitation protocol for elbow contracture. The results indicate that extending CPM training to three months post-surgery significantly improves elbow function, including flexion, extension, range of motion, and grip strength. Additionally, it helps alleviate postoperative pain and accelerates the reduction of swelling in the forearm and elbow joint. These findings have important clinical implications, particularly for rehabilitation planning, indicating that to achieve optimal functional recovery, CPM rehabilitation should be initiated immediately after surgery and maintained for at least three months. The study further highlights that CPM training has no significant effect on forearm rotational function, suggesting that future rehabilitation protocols should be tailored to individual patient needs. For patients requiring greater flexion recovery, three months of CPM training is sufficient. Extending CPM training to five months did not yield further functional improvements, providing clear guidance on the optimal duration of rehabilitation. Based on this study, clinicians can set the appropriate duration of CPM training according to patient recovery needs, avoiding unnecessary prolongation of rehabilitation without significant benefit, thus optimizing resource allocation and patient experience.
Overall, the study supports a three-month CPM rehabilitation protocol following elbow contracture release surgery and provides evidence-based guidance for rehabilitation planning, especially for patients with higher functional demands. For those who do not achieve the desired functional outcome after three months of CPM training, further extension is unlikely to be beneficial, providing clinicians with valuable insights for personalized decision-making during the rehabilitation process.
Study limitation
First, this study is a retrospective cohort analysis, and despite our best efforts, there were limitations in data collection and measurement. Second, the grouping in the study was primarily based on patients’ treatment preferences and functional needs rather than random assignment, which could impact the final conclusions. Third, CPM rehabilitation training was primarily conducted outside the hospital. Although we provided detailed guidance on CPM training before discharge and established a doctor-patient communication platform to address any issues during rehabilitation, the absence of full supervision by professional rehabilitation physicians may have impacted the treatment outcomes. Fourth, this study did not conduct a detailed comparative analysis of postoperative CPM rehabilitation training durations. This is due to the unavailability of precise and suitable training durations, which may necessitate larger clinical sample sizes and more sophisticated follow-up methods, such as artificial intelligence-based wearable devices. To address these limitations, future research should consider the use of prospective randomized controlled trials. Randomized controlled trials, through random group assignments, can reduce selection bias and provide clearer assessments of the effects of different CPM training durations on postoperative functional recovery. Additionally, RCTs can better control for confounding variables, making the results more robust and generalizable. By addressing these limitations, future studies can provide stronger evidence to optimize CPM rehabilitation protocols following elbow contracture release surgery.
Conclusion
This retrospective cohort analysis study investigated the impact of different durations of CPM rehabilitation training on functional recovery following elbow arthroscopic contracture release over a 1-year follow-up period. The findings revealed that CPM at three months post-surgery was more effective in restoring elbow joint function compared to one month, particularly showing greater improvements in elbow joint flexion than extension, along with quicker reduction in postoperative forearm swelling. Evaluation scales such as MEPS, DASH, and ASES indicated significant enhancements in patients’ abilities for work and daily activities. However, extending CPM training to 5 months did not result in further functional benefits. Therefore, the study recommends that patients with stiff elbow joints undergo CPM rehabilitation training after arthroscopic contracture release, with the option to extend training to 3 months for those with higher functional demands. Continuing CPM training beyond this point may not be advantageous, suggesting the consideration of alternative approaches like physical therapy or combination therapies.
Acknowledgements
Not applicable.
Abbreviations
- CPM
Continuous Passive Motion
- AOA
Arthroscopic Osteocapsular Arthroplasty
- ASES
American Shoulder and Elbow Surgeons function score
- VAS
Visual Analog Scale
- DSAH
Disabilities of the Arm, Shoulder and Hand
- MEPS
Mayo Elbow-Performance Score
- ANOVA
analysis of variance
Author contributions
xhW designed the overall experiment, participated fully in the experiment process, wrote the main manuscript text, and submitted it. qyL contributed to the overall trial design and collected basic patient information. jyM guided the experimental design and conduct throughout the process. jyT participated in discussions on experimental design and data measurement methodology. At the same time, jnW and qwY offered guidance on the rehabilitation professional skills required during the trial process. wxC and jyZ were responsible for collecting and classifying the patient information needed for the trial, and fX and hyY participated in and provided guidance on the experimental design and article writing.All authors read and approved the final manuscript.
Funding
1.“Wuxi Taihu Talent Plan” High-level Talents in Medical and Health (2020). 2.Major scientific research project of Wuxi Municipal Health Commission (Z202108). 3.Shanghai Key Laboratory of Peripheral Nerve and Microsurgery NHC Key Laboratory of Hand Reconstruction(Fudan University) (20DZ2270200).
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval
This study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki and approved by the Medical Ethics Committee of Wuxi Ninth People’s Hospital (Approval Number: KS2024022). Written informed consent was obtained from all participants prior to their inclusion in the study. The privacy and confidentiality of all participants were strictly maintained throughout the study. All data were anonymized and handled according to applicable data protection regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xunhao Wang, Qianyuan Liu these authors equally contributed to this work.
References
- 1.Haglin JM, Kugelman DN, Christiano A, Konda SR, Paksima N, Egol KA. Open surgical elbow contracture release after trauma: results and recommendations. J Shoulder Elb Surg. 2018;27(3):418–26. [DOI] [PubMed] [Google Scholar]
- 2.Kodde IF, van Rijn J, van den Bekerom MP, Eygendaal D. Surgical treatment of post-traumatic elbow stiffness: a systematic review. J Shoulder Elb Surg. 2013;22(4):574–80. [DOI] [PubMed] [Google Scholar]
- 3.Edwards SG, Rhodes DA, Jordan TW, Sietsema DL. The Olecranon Osteotomy-facilitated elbow release (OFER). J Bone Joint Surg Am. 2017;99(21):1859–65. [DOI] [PubMed] [Google Scholar]
- 4.O’Driscoll SW, Lievano JR, Morrey ME, Sanchez-Sotelo J, Shukla DR, Olson TS, Fitzsimmons JS, Vaichinger AM, Shields MN. Prospective randomized trial of continuous Passive Motion Versus Physical Therapy after arthroscopic release of elbow contracture. J Bone Joint Surg Am. 2022;104(5):430–40. [DOI] [PubMed] [Google Scholar]
- 5.O’Driscoll SW, Giori NJ. Continuous passive motion (CPM): theory and principles of clinical application. J Rehabil Res Dev. 2000;37(2):179–88. [PubMed] [Google Scholar]
- 6.Hildebrand KA. Posttraumatic elbow joint contractures: defining pathologic capsular mechanisms and potential future treatment paradigms. J Hand Surg Am. 2013;38(11):2227–33. [DOI] [PubMed] [Google Scholar]
- 7.Cohen MS, Schimmel DR, Masuda K, Hastings H 2nd, Muehleman C. Structural and biochemical evaluation of the elbow capsule after trauma. J Shoulder Elb Surg. 2007;16(4):484–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Masci G, Cazzato G, Milano G, Ciolli G, Malerba G, Perisano C, Greco T, Osvaldo P, Maccauro G, Liuzza F. The stiff elbow: current concepts. Orthop Rev (Pavia). 2020;12(Suppl 1):8661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O’Driscoll SW, Blonna D. Osteocapsular arthroplasty of the elbow: Surgical technique. JBJS Essent Surg Tech. 2014;3(3):e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fan C, Yushan M, Liu Y, Bahesutihan Y, Liu K, Yusufu A. Treatment outcome of tardy ulnar nerve palsy associated with traumatic cubitus valgus by supracondylar shortening wedge rotary osteotomy and ulnar nerve in situ tension release. BMC Musculoskelet Disord. 2022;23(1):369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bugada D, Cantu D, Benigni A, Lorini LF. Continuous erector spinae plane block: effective analgesia and rehabilitation after elbow surgery for traumatic injury. J Clin Anesth. 2021;71:110222. [DOI] [PubMed] [Google Scholar]
- 12.Caron MMJ, Emans PJ, Cremers A, Surtel DAM, van Rhijn LW, Welting TJM. Indomethacin induces differential effects on in vitro endochondral ossification depending on the chondrocyte’s differentiation stage. J Orthop Res. 2017;35(4):847–57. [DOI] [PubMed] [Google Scholar]
- 13.Cichos KH, Spitler CA, Quade JH, Almaguer A, McGwin G Jr., Ghanem ES. Do Indomethacin or Radiation for Heterotopic Ossification Prophylaxis increase the rates of infection or wound complications after Acetabular fracture surgery? J Orthop Trauma. 2020;34(9):455–61. [DOI] [PubMed] [Google Scholar]
- 14.Rojas Lievano J, Rotman D, Shields MN, Morrey ME, Sanchez-Sotelo J, Shukla DR, Olson TS, Vaichinger AM, Fitzsimmons JS, O’Driscoll SW. Patients use fewer Opioids Than prescribed after arthroscopic release of elbow contracture: an evidence-based Opioid Prescribing Guideline to reduce excess. Arthrosc Sports Med Rehabil. 2021;3(6):e1873–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heyworth B, Cohen L, von Heideken J, Kocher MS, Iversen MD. Validity and comprehensibility of outcome measures in children with shoulder and elbow disorders: creation of a new Pediatric and adolescent shoulder and elbow survey (Pedi-ASES). J Shoulder Elb Surg. 2018;27(7):1162–71. [DOI] [PubMed] [Google Scholar]
- 16.Angst F, Schwyzer HK, Aeschlimann A, Simmen BR, Goldhahn J. Measures of adult shoulder function: disabilities of the arm, shoulder, and Hand Questionnaire (DASH) and its short version (QuickDASH), Shoulder Pain and Disability Index (SPADI), American Shoulder and elbow surgeons (ASES) society standardized shoulder assessment form, constant (Murley) score (CS), simple shoulder test (SST), Oxford Shoulder score (OSS), shoulder disability questionnaire (SDQ), and western Ontario shoulder instability index (WOSI). Arthritis Care Res (Hoboken). 2011;63(Suppl 11):S174–188. [DOI] [PubMed] [Google Scholar]
- 17.Evans JP, Smith CD, Fine NF, Porter I, Gangannagaripalli J, Goodwin VA, Valderas JM. Clinical rating systems in elbow research-a systematic review exploring trends and distributions of use. J Shoulder Elb Surg. 2018;27(4):e98–106. [DOI] [PubMed] [Google Scholar]
- 18.Schiffke-Juhasz B, Knobloch K, Vogt PM, Hoy L. Proprioceptive elbow training reduces pain and improves function in painful lateral epicondylitis-a prospective trial. J Orthop Surg Res. 2021;16(1):468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martin P, Nunan R. Cellular and molecular mechanisms of repair in acute and chronic wound healing. Br J Dermatol. 2015;173(2):370–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mellema JJ, Lindenhovius AL, Jupiter JB. The posttraumatic stiff elbow: an update. Curr Rev Musculoskelet Med. 2016;9(2):190–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Everding NG, Maschke SD, Hoyen HA, Evans PJ. Prevention and treatment of elbow stiffness: a 5-year update. J Hand Surg Am. 2013;38(12):2496–507. quiz 2507. [DOI] [PubMed] [Google Scholar]
- 22.Lindenhovius AL, Jupiter JB. The posttraumatic stiff elbow: a review of the literature. J Hand Surg Am. 2007;32(10):1605–23. [DOI] [PubMed] [Google Scholar]
- 23.Yu S, Chen M, Fan C. Team Approach: elbow contracture due to Heterotopic Ossification. JBJS Rev 2017, 5(1). [DOI] [PubMed]
- 24.Yin P, Zhang L, Mao Z, Zhao Y, Zhang Q, Tao S, Liang X, Zhang H, Lv H, Li T, et al. Comparison of lateral and posterior surgical approach in management of extra-articular distal humeral shaft fractures. Injury. 2014;45(7):1121–5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.