Abstract
Background
Complications from prolonged esophageal foreign body impaction are well-documented, yet the significance of non-foreign body factors has not been thoroughly explored. This study aims to investigate non-foreign body risk factors for complications during esophageal foreign-body removal and to evaluate the impact of treatment timing.
Study
We conducted a retrospective evaluation of patients diagnosed with esophageal foreign bodies requiring gastroscopic removal in our hospital between January 2019 and December 2020. Non-foreign body factors, such as whether endoscopic treatment was on the day of the visit, visiting time, complaint time (from ingestion to presentation), anesthesia method, and holidays, were considered.
Results
In total, 831 patients were included. The success rate of endoscopic treatment was 97.8%. The overall probabilities of mucosal injury, bleeding, and perforation were 90.3%, 53.3%, and 6.9%, respectively. The treatment was performed on the day of the patient’s visit for 70.4% patients, under sedation anesthesia for 50.7% patients, and in the early night for 44.6% patients. Treatment on the day of the visit did not affect the success rate. Same-day treatment was a protective factor for mucosal injury and perforation on univariate logistic regression analysis, but did not independently influence mucosal injury, bleeding, or perforation on multivariate analysis. Visiting time, complaint time, and holidays affected the complication rate. During the COVID-19 period in China, visiting time and anesthesia method were found to be independent predictors of same-day treatment.
Conclusions
Complaint time, visiting time and same-day treatment are significant and practical factors influencing the complications of endoscopic foreign-body removal. Certain patients, notably night-time visitors, might benefit from delaying treatment until the following day to utilize sedative anesthesia to minimize risks.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12876-024-03532-0.
Keywords: Esophageal foreign-body, Endoscopic removal, Non-foreign body-associated risk factors, Complication, Treatment time
Introduction
Prolonged esophageal foreign body impaction is associated with an increased risk of complications and a lower success rate of endoscopic treatment [1–3], which emphasizes the importance of the timing of endoscopic treatment. Clinically, the selection of the timing of endoscopic treatment should depend on the patient’s symptoms; the type, location, and duration of the foreign body; the duration of fasting; the timing of the patient’s visit (in the daytime vs. nighttime); endoscopic tolerance; the anesthesia method required; and the patient’s wishes [4, 5]. Thus far, previous studies on esophageal foreign bodies have focused on the characteristics of the foreign body itself [6–8], such as type, size, and shape, as well as the impaction time.
However, there is limited research exploring the patient-related aspects, endoscopic physician-related aspects, and other aspects of esophageal foreign bodies. For example, patients with mental retardation tend to experience increased complications [9]. Additionally, repeated ingestion of esophageal foreign bodies has been reported in individuals with borderline personality disorder [10]. Factors such as inadequate equipment in rural areas, the location of treatment facilities or departments, and cultural holidays may also impact the management of esophageal foreign bodies [11–13]. Therefore, the present study aimed to identify the non-foreign body-associated risk factors for complications in patients undergoing endoscopic removal of esophageal foreign bodies as well as to identify factors that influenced the timing of endoscopic treatment. Moreover, this study investigated the impact of the COVID-19 period, providing insights for the management and prevention strategies during similar epidemics in the future.
Materials and methods
Study population
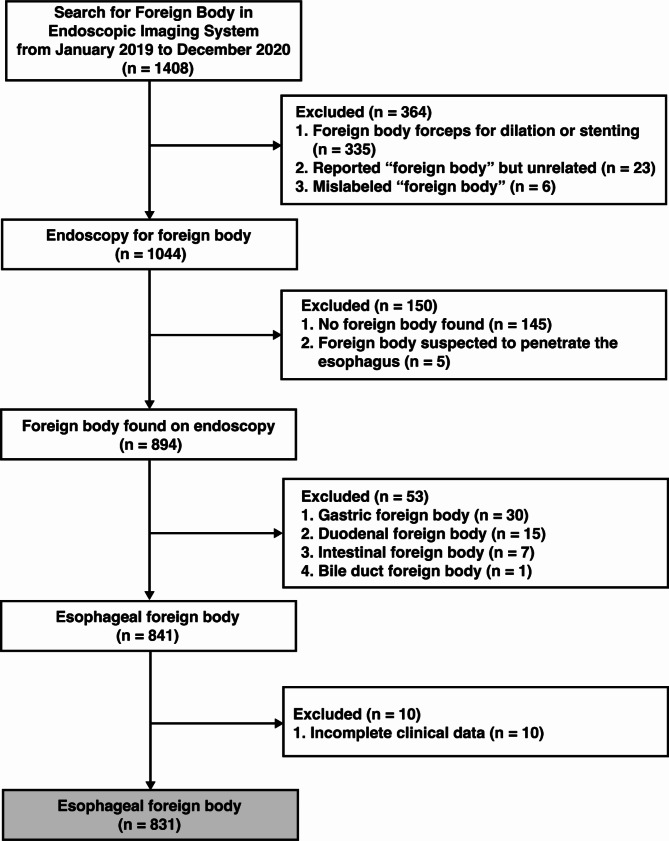
A search of our hospital endoscopic imaging system for all cases with the keyword “foreign body” between January 2019 and December 2020 yielded a total of 1408 records. The clinical data of these patients, including data from the outpatient, emergency, and inpatient departments as well as telephone follow-up, were retrieved through the hospital computer system. The type, size, location, and other information of the foreign bodies were collected from the endoscopic report; where this information was not described, it was added by referring to the CT and medical records. Finally, 831 cases were included in this analysis (shown in Fig. 1). This study protocol was reviewed and approved by the ethics committee of the First Affiliated Hospital of Nanjing Medical University (no. 2023-SR-013).
Fig. 1.
Flow chart of patient selection
The white boxes show the selection of patients who met the eligibility criteria, the grey boxes show patients who were included in the current study
Methods of endoscopic treatment
In our Endoscopy Center, there was a dedicated room for emergency endoscopic procedures, including foreign body removal, although endoscopic ultrasound therapy might also be scheduled in the morning. Emergency patients were prioritized for treatment, and in the afternoon, the room was typically reserved exclusively for emergency endoscopic procedures. During holidays, the endoscopy room was available for use at any time. Nurses and anesthetists on duty were required to remain on standby at the hospital during these periods. The endoscopy room was generally equipped with an anesthesia machine, along with anesthesia and rescue medications. Esophageal foreign bodies without perforation and those perforating the upper or lower third of the esophagus were preferentially treated in the endoscopy room. For foreign bodies perforating the middle third of the esophagus, endoscopic removal was attempted in the operating room with surgical assistance. Patients with an existing aortic injury or a high risk of aortic injury could be treated by endoscopy after endovascular stenting [14]. The type of anesthesia was selected based on fasting duration, with topical pharyngeal anesthesia for 4–6 h of fasting and sedation anesthesia for 6–8 h of fasting. The timing of endoscopic treatment and the method of anesthesia were ultimately decided by both the doctors and patients. All patients signed relevant informed consent forms. A transparent cap was routinely used for foreign body removal, and commonly used instruments included grasping forceps, snare, and baskets [15, 16].
Definition of evaluation criteria and related factors
We used the endoscopic text reports and endoscopic and CT images to assess esophageal mucosal injury, bleeding, and perforation. The endoscopic findings were reviewed and confirmed by both a senior and a junior endoscopist from the department of gastroenterology. The senior endoscopist could perform endoscopic ultrasound and endoscopic submucosal dissection, while the junior endoscopist only performed gastrointestinal endoscopy or complete endoscopic mucosal resection. Mucosal injuries included hyperemic edema, erosions, ulcers, mucosal avulsion, and hematoma formation. Bleeding was categorized as a small or active. Perforations referred to endoscopically visible outer tissue or leakage of air out of the lumen on CT. Suspected perforations and obvious fistula formation recorded in endoscopic reports were also classified as perforations. In this study, endoscopists were also categorized as junior or senior based on their experience in performing gastroenteroscopy procedures. An endoscopist with over 2 years of experience was considered a senior endoscopist, while one with less than 2 years of experience was considered a junior endoscopist. Successful foreign-body removal was defined as removing the foreign body from the esophagus and through the mouth or actively pushing the esophageal foreign body into the stomach for digestion (primarily meat or rice lump, rather than hard or sharp foreign bodies). According to the working hours of our hospital, it is defined that 8:00 to 11:30 as the morning, 11:30 to 14:00 as the noon, 14:00–17:30 as the afternoon, 17:30 − 24:00 as the early night, and 0:00–8:00 as the late night. Same-day endoscopic treatment was defined as endoscopic treatment performed on the day of the patient’s visit. Holidays included weekends and Chinese statutory holidays. In the gastroenterology department, the day shift on weekdays was typically staffed by junior endoscopists, while the holiday day shifts were generally handled by senior endoscopists, with evening shifts assigned randomly. The schedule of endoscopists in other departments was also random. The patients presenting from January 2020 were classified as being in the COVID-19 period, during which the government took several public health interventions such as traffic restrictions, social distancing, home isolation and centralized isolation. In our Endoscopy Center, non-emergency patients need to wait for nucleic acid test results to detect COVID-19 infection, while critically ill patients need to be treated in time, and medical staff need to take precautions in the absence of nucleic acid results. The time from the ingestion of the foreign body to the patient’s visit to our hospital was termed the “complaint time”.
Statistical analysis
Data were analyzed using SPSS software (version 26.0; IBM Corp., Armonk, NY, USA), and descriptive statistics were evaluated using frequency analysis. Univariate and multivariate logistic regression were used to analyze the risk factors. The chi-square test or Fisher exact test was used for the between-group comparisons of potential risk factors. Statistical significance was indicated by P < 0.05.
Results
Clinical characteristics
The clinical characteristics of the patients are shown in Table 1. The patients included 358 (43.1%) male patients and 473 (56.9%) female patients, with an average age of 54.1 ± 16.43 years. Most patients visited in the early night (52.5%), and 41.8% of the patients had first visited another hospital. The complaint time was < 6 h in 55.8% of patients. During endoscopic treatment, new esophageal masses (possibly malignant tumors) were found in 1.4% patients, and esophageal stenosis was detected in 1.1% patients, including 1 patient with CT-confirmed external compression by a lung mass and 1 patient with possible achalasia. The characteristics of the esophageal foreign bodies are detailed shown in Supplementary Table 1. The broken avian bones often have sharp ends.
Table 1.
Patient characteristics
| Parameter | Result, n (%) |
|---|---|
| Total number | 831 |
| Age, years | 54.1 ± 16.43 |
| Gender, male | 358 (43.1) |
| Visit time | |
| Morning | 85 (10.2) |
| Noon | 88 (10.6) |
| Afternoon | 169 (20.3) |
| Early night | 436 (52.5) |
| Late night | 53 (6.4) |
| Holiday | 301 (36.2) |
| COVID-19 epidemic period | 370 (44.5) |
| Prior visit to another hospital | 347 (41.8) |
| Examination or treatment in another hospital | |
| Laryngoscopy | 30 (3.6) |
| X-ray | 16 (1.9) |
| CT | 283 (34.1%) |
| Gastroscopic treatment | 38 (4.6) |
| Complaint time | |
| < 6 h | 464 (55.8) |
| ≥ 6 h, < 12 h | 132 (15.9) |
| ≥ 12 h, < 24 h | 55 (6.6) |
| ≥ 24 h, < 72 h | 112 (13.5) |
| ≥ 72 h | 68 (8.2) |
| Findings on endoscopy | |
| Postoperative esophageal status | 34 (4.1) |
| Esophageal mass | 12 (1.4) |
| Esophageal stenosis | 9 (1.1) |
| Gastric mucosal lesions or mass | 7 (0.8) |
Details of the endoscopic treatment are summarized in Table 2. The treatment success rate for esophageal foreign bodies was 97.8%. Treatment time during late-night hours and the presence of dental prostheses were identified as significant risk factors for treatment failure (P < 0.05). Specifically, compared to morning treatment, the risk of treatment failure during late-night hours was significantly higher, with an odds ratio (OR) of 9.25 and a failure rate of 9.1%. No other factors were found to be significantly associated with treatment failure. Endoscopy was performed on the day of the patient’s visit for 70.4% of patients, and was performed under sedation anesthesia for 50.7% of patients. Endoscopic treatment was most performed in the early night (44.6%). In 8 patients, the foreign bodies fell off the forceps during endoscopic removal. One foreign body fell into the stomach but was successfully removed; 4 foreign bodies (including 3 in patients with poor cooperation) could not be removed due to food in the stomach; 1 foreign body fell in the airway while the patient was under sedation anesthesia, and was removed using bronchoscopy; 1 foreign body was vomited out of the body; and 1 foreign body disappeared after the patient started coughing. Twenty patients (2.4%) had poor cooperation with obvious vomiting or coughing during the endoscopic treatment, and only one of these patients was under sedation anesthesia. The overall rates of mucosal injury, bleeding, and perforation were 90.3%, 53.3%, and 6.9%, respectively.
Table 2.
Doctor and endoscopy characteristics
| Parameter | Result, n (%) |
|---|---|
| Total number | 831 |
| Successful treatment | 813 (97.8) |
| Same-day treatment | 585 (70.4) |
| Anesthesia method | |
| Topical pharyngeal anesthesia | 410 (49.3) |
| General anesthesia | 421 (50.7) |
| Treatment time | |
| Morning | 187 (22.5) |
| Noon | 54 (6.5) |
| Afternoon | 175 (21.1) |
| Early night | 371 (44.6) |
| Late night | 44 (5.3) |
| Events during endoscopy | |
| Falling down of foreign body | 8 (1.0) |
| Fracture of foreign body | 38 (4.6) |
| Patient vomited or coughed | 20 (2.4) |
| Removal in divided parts | |
| No | 769 (92.4) |
| Yes | 63 (7.6) |
| Gastric-cavity condition | |
| No food retention | 252 (30.2) |
| Food retention | 44 (5.3) |
| No record/Not entered | 535 (64.4) |
| Clinical department | |
| Gastroenterology | 573 (69.0) |
| Digestive Endoscopy | 191 (23.0) |
| Pancreas Center | 57 (6.9) |
| Geriatric Medicine | 10 (1.2) |
| Cases performed of seniority of physician | |
| Junior | 434 (52.2) |
| Senior | 397 (47.8) |
| Number of complications of physician | |
| Junior | 399 (48.1) |
| Senior | 354 (42.6) |
| Complications | |
| Mucosal injury | 750 (90.3) |
| Mucosal bleeding | 443 (53.3) |
| Mucosal perforation | 57 (6.9) |
| Treatment of complications | |
| Spraying norepinephrine | 14 (1.7) |
| Metal clips for wound | 9 (1.1) |
| Indwelling gastric tube | 29 (3.5) |
Risk factors for mucosal injury
Univariate logistic regression analysis showed that mucosal injury was related to same-day endoscopic treatment; patient’s visiting time; prior visit to another hospital; complaint time; timing of endoscopic treatment (morning, noon, etc.); the type, shape, size, number of impacted ends, and fracture of the foreign body; removal in divided parts; and condition of the gastric cavity (P < 0.05). Same-day endoscopic treatment was a protective factor for mucosal injury (OR = 0.344, 95% confidence interval (CI): 0.179–0.662, P = 0.001). Compared with morning visits, visits during other periods were associated with an increased risk of mucosal injury, and the OR values for noon, afternoon, early-night, and late-night visits were 2.879, 2.574, 3.298, and 7.341, respectively. Patients who had first visited other hospitals had a higher risk of mucosal injury (OR = 2.179, 95% CI: 1.309–3.686, P = 0.003). The risk of mucosal injury was significantly lower among patients with a complaint time of 1–3 days than among patients with a complaint time of 6–12 h (P < 0.05); no significant difference was observed between the other groupings of complaint time. The risk of mucosal injury was lower when the treatment was performed at noon than in the morning (P < 0.05). Removal in the divided portions and unemptied food in the stomach were protective factors for mucosal injury (P < 0.05).
Multivariate logistic regression analysis of the variables with statistical differences above showed that only the type, shape, number of impacted ends, and size of the foreign bodies were independent influencing factors for esophageal mucosal injury (Table 3). Same-day endoscopic treatment did not independently affect the risk of mucosal injury (P = 0.667).
Table 3.
Multivariate logistic regression analysis of mucosal injury
| Factor | β | Wald χ² | P value | OR (95% CI) |
|---|---|---|---|---|
| Foreign-body type | ||||
| Food bolus | 0.000 | 1.000 | ||
| Fish bone | 3.021 | 8.741 | 0.003 | 20.502 (2.768–151.859) |
| Avian bone | 3.334 | 11.406 | 0.001 | 28.060 (4.052–194.301) |
| Jujube pits | 3.860 | 10.305 | 0.001 | 47.442 (4.495–500.667) |
| Other | 1.959 | 2.384 | 0.123 | 7.094 (0.590–85.315) |
| Foreign-body shape | ||||
| Elongated | 0.000 | 1.000 | ||
| Multilateral, regular | 0.389 | 0.639 | 0.424 | 1.475 (0.569–3.826) |
| Irregular | 1.921 | 8.081 | 0.004 | 6.830 (1.816–25.689) |
| Round | -0.707 | 0.238 | 0.626 | 0.493 (0.029–8.439) |
| Foreign-body size | ||||
| < 2 cm | 0.000 | 1.000 | ||
| 2–3 cm | 0.697 | 4.513 | 0.034 | 2.008 (1.055–3.820) |
| ≥ 3 cm | 1.680 | 10.117 | 0.001 | 5.367 (1.906–15.116) |
| Foreign-body ends | ||||
| Free | 0.000 | 1.000 | ||
| One impacted end | 2.260 | 7.288 | 0.007 | 9.579 (1.857–49.403) |
| Two or more impacted ends | 3.565 | 16.941 | < 0.001 | 35.323 (6.470–192.852) |
Risk factors for mucosal bleeding
According to the univariate logistic regression analysis, the following factors potentially increased the risk of mucosal bleeding: visit on a holiday (OR = 1.447, 95% CI: 1.087–1.926, P = 0.011), age (OR = 1.021, 95% CI: 1.012–1.030, P < 0.01), prior visit to another hospital (OR = 1.377, 95% CI: 1.043–1.181, P = 0.024), and prior endoscopic treatment in another hospital (OR = 2.224, 95% CI: 1.088–4.546, P = 0.028). The complaint time; timing of endoscopic treatment; type, shape, size, and number of impacted ends of the foreign body; and gastric-cavity condition were also associated with mucosal bleeding (P < 0.05). Same-day endoscopic treatment was not associated with mucosal bleeding. Compared to a complaint time of < 6 h, the risk of mucosal bleeding was increased with complaint times of ≥ 6 to < 12 h (OR = 1.772), ≥ 12 h to < 24 h (OR = 1.925), ≥ 24 h to < 72 h (OR = 1.770), and ≥ 72 h (OR = 3.566). However, there was no significant difference in the risk of mucosal bleeding between all other groups of complaint times from 6 h to 72 h. The risk of bleeding was higher with nighttime endoscopic treatment than with daytime treatment (OR = 1.338, 95% CI: 1.018–1.758, P = 0.037).
Multivariate logistic regression analysis of the variables with statistical differences above and the variable of same-day endoscopic treatment showed that holidays; age; complaint time; timing of endoscopic treatment; type, shape, size, and number of impacted ends of the foreign body; and gastric-cavity condition were independent influencing factors for mucosal bleeding (Table 4). Same-day endoscopic treatment did not independently affect the risk of mucosal bleeding (P = 0.116).
Table 4.
Multivariate logistic regression analysis of mucosal bleeding
| Factor | β | Wald χ² | P value | OR (95% CI) |
|---|---|---|---|---|
| Holiday | 0.457 | 7.273 | 0.007 | 1.579 (1.133–2.201) |
| Age | 0.022 | 15.613 | < 0.01 | 1.022 (1.011–1.033) |
| Complaint time | ||||
| < 6 h | 0.000 | 1.000 | ||
| ≥ 6 h, < 12 h | 0.337 | 2.158 | 0.142 | 1.401 (0.893–2.198) |
| ≥ 12 h, < 24 h | 0.982 | 8.212 | 0.004 | 2.670 (1.364–5.226) |
| ≥ 24 h, < 72 h | 0.573 | 4.467 | 0.035 | 1.774 (1.043–3.020) |
| ≥ 72 h | 1.090 | 9.165 | 0.002 | 2.973 (1.468–6.019) |
| Treatment time | ||||
| Daytime | 0.000 | 1.000 | ||
| Nighttime | 0.638 | 10.342 | 0.001 | 1.893 (1.283–2.792) |
| Foreign-body type | ||||
| Food bolus | 0.000 | 1.000 | ||
| Fish bone | 1.720 | 5.551 | 0.018 | 5.586 (1.335–23.365) |
| Avian bone | 1.883 | 6.936 | 0.008 | 6.575 (1.619–26.704) |
| Jujube pits | 2.492 | 10.399 | 0.001 | 12.086 (2.658–54.963) |
| Others | 1.811 | 4.012 | 0.045 | 6.116 (1.040–35.976) |
| Foreign-body shape | ||||
| Elongated | 0.000 | 1.000 | ||
| Multilateral, regular | -0.170 | 0.494 | 0.482 | 0.844 (0.525–1.355) |
| Irregular | 0.921 | 17.603 | < 0.01 | 2.512 (1.633–3.862) |
| Round | 0.857 | 0.632 | 0.427 | 2.355 (0.285–19.475) |
| Foreign-body size | ||||
| < 2 cm | 0.000 | 1.000 | ||
| 2–3 cm | 0.848 | 20.942 | < 0.01 | 2.335 (1.624–3.358) |
| ≥ 3 cm | 1.258 | 27.622 | < 0.01 | 3.519 (2.201–5.626) |
| Foreign-body ends | ||||
| Free | 0.000 | 1.000 | ||
| One impacted end | 0.279 | 0.169 | 0.681 | 1.321 (0.351–4.977) |
|
Two or more impacted ends |
0.902 | 1.797 | 0.180 | 2.463 (0.659–9.204) |
| Gastric-cavity condition | ||||
| No food retention | 0.000 | 1.000 | ||
| Food retention | -0.604 | 2.186 | 0.139 | 0.547 (0.245–1.217) |
| No record/Not entered | 0.434 | 5.554 | 0.018 | 1.543 (1.076–2.214) |
Risk factors for mucosal perforation
Univariate logistic regression analysis showed that the coronavirus disease 2019 (COVID-19) period (OR = 2.085, 95% CI: 1.201–3.620, P = 0.009), age (OR = 1.018, 95% CI: 1.001–1.035, P = 0.037), prior visit to another hospital (OR = 2.014, 95% CI: 1.168–3.474, P = 0.012), prior endoscopic treatment in another hospital (OR = 4.817, 95% CI: 2.158–10.750, P < 0.01), and sedation anesthesia (OR = 3.128, 95% CI: 1.732–5.978, P < 0.01) were risk factors for mucosal perforation. Compared with a complaint time of < 6 h, complaint times of ≥ 6 h to < 12 h (OR = 3.109), ≥ 24 h to < 72 h (OR = 7.834), and ≥ 72 h (OR = 48.546) were associated with gradually increasing risks of mucosal perforation. However, the risk of mucosal perforation in patients with a complaint time of ≥ 12 h to < 24 h did not differ from that in patients with complaint times of < 6 h (OR = 3.766, P = 0.06) and ≥ 6 h to < 12 h (OR = 1.212, P = 0.792). Foreign bodies that were impacted at 2 or more ends were more likely to cause perforation than free foreign bodies or those impacted at one end (P < 0.01). The larger the foreign body, the higher the risk of perforation (P < 0.01). In addition, holidays (OR = 0.499, 95% CI: 0.264–0.941, P = 0.032), same-day endoscopic treatment (OR = 0.473, 95% CI: 0.275–0.816, P = 0.007), and no record of the gastric cavity in the endoscopy report (possibly because the gastric cavity was not entered during the procedure; OR = 0.393, 95% CI: 0.228–0.677, P = 0.01) were protective factors for mucosal perforation.
Multivariate logistic regression analysis of the variables with statistical differences above showed that only the complaint time, the size of the foreign body, and the number of impacted ends were independent influencing factors for mucosal perforation (Table 5). Although univariate logistic regression analysis showed that same-day endoscopic treatment was a protective factor for mucosal perforation, it was not an independent factor in the multivariate analysis.
Table 5.
Multivariate logistic regression analysis of mucosal perforation
| Factor | β | Wald χ² | P value | OR (95% CI) |
|---|---|---|---|---|
| Complaint time | ||||
| < 6 h | 0.000 | 1.000 | ||
| ≥ 6 h, < 12 h | 0.829 | 1.932 | 0.165 | 2.290 (0.712–7.367) |
| ≥ 12 h, < 24 h | 0.946 | 1.585 | 0.208 | 2.575 (0.591–11.226) |
| ≥ 24 h, < 72 h | 1.666 | 9.830 | 0.002 | 5.293 (1.868–14.999) |
| ≥ 72 h | 3.614 | 45.395 | < 0.01 | 37.130 (12.975–106.258) |
| Foreign-body size | ||||
| < 2 cm | 0.000 | 1.000 | ||
| 2–3 cm | 0.738 | 1.718 | 0.190 | 2.092 (0.694–6.307) |
| ≥ 3 cm | 1.786 | 9.909 | 0.002 | 5.967 (1.962–18.147) |
| Foreign-body ends | ||||
| Free or one impacted end | 0.000 | 1.000 | ||
| Two or more impacted ends | 1.434 | 13.530 | < 0.01 | 4.197 (1.954–9.014) |
Same-day endoscopic treatment and associated factors
The success rate of same-day endoscopic treatment did not differ from that of later endoscopic treatment (97.8% vs. 98.0%, P = 0.864). Compared to later treatment, same-day endoscopic treatment was associated with a lower incidence of mucosal injury (88.0% vs. 95.5%, P < 0.01) and perforation (5.3% vs. 10.6%, P < 0.01), but had no significant effect on the incidence of mucosal bleeding (52.6% vs. 54.9%, P = 0.557). As mentioned above, same-day endoscopic treatment was a protective factor for mucosal injury and perforation in the univariate logistic regression analyses, but it was not an independent influencing factor for mucosal injury, bleeding, or perforation in the multivariate logistic regression analysis. Univariate logistic regression analysis showed that during the COVID-19 period, holidays, gender, visiting time, anesthesia method, and type of foreign body were influencing factors for same-day endoscopic treatment. The COVID-19 period, visiting time, and anesthesia method were independent influencing factors for same-day endoscopic treatment according to the multivariate logistic regression analysis (Table 6).
Table 6.
Multivariate logistic regression analysis of same-day treatment
| Factor | β | Wald χ² | P value | OR (95% CI) |
|---|---|---|---|---|
| COVID-19 epidemic period | -0.710 | 12.894 | < 0.01 | 0.492 (0.334–0.724) |
| Visit time | ||||
| Morning | 0.000 | 1.000 | ||
| Noon | 0.216 | 0.184 | 0.668 | 1.241 (0.462–3.336) |
| Afternoon | 0.188 | 0.171 | 0.680 | 1.207 (0.495–2.944) |
| Early night | -2.216 | 31.939 | < 0.01 | 0.109 (0.051–0.235) |
| Late night | -3.954 | 48.634 | < 0.01 | 0.019 (0.006–0.058) |
| Anesthesia method | ||||
| Topical pharyngeal | 0.000 | 1.000 | ||
| General | -2.402 | 117.996 | < 0.01 | 0.091 (0.059–0.140) |
Discussion
The study particularly investigated the non-foreign body-related influencing factors, including complaint time, visiting time, endoscopic treatment time, and whether endoscopic treatment was performed on the day of the patient’s visit, and analyzed the factors affecting the timing of endoscopic treatment.
We found that the complaint time was not equivalent to the duration of foreign body impaction, which is the time from ingestion to endoscopic removal. Moreover, the complaint time was an independent influencing factor for mucosal bleeding and perforation. Many studies have reported that endoscopic treatment within 24 h of the ingestion of an esophageal foreign body can reduce the risk of complications [3, 17, 18]. In our study, 21.7% of patients had a complaint time of > 24 h, and 8.2% had a complaint time of > 72 h. This delay may be attributed to some patients choosing to monitor their condition at home or being unable to seek treatment at the nearest hospital. Notably, people with mental retardation, drunkenness, deaf-mutes, and prison criminals are occasionally encountered, each presenting unique challenges in the management of foreign bodies [9, 10, 19]. For instance, patients with mental retardation often struggle with self-care, leading to delayed recognition of esophageal foreign bodies. In fact, mental retardation and/or poor cognitive function may serve as independent risk factors for complications, separate from the presence of the foreign body itself [9]. The visiting time affected the risk of mucosal injury but was not an independent factor; the risk was higher for nighttime visits than for daytime visits, and late-night visits had the highest risk. This may be related to the degree of fatigue of doctors and patients at night, and even the night staff management [20]. Prior visit to another hospital was a risk factor for all complications, and attempted endoscopic treatment in another hospital was a risk factor for mucosal bleeding and perforation. Some patients had been diagnosed in nearby primary hospitals, and were then transferred to our hospital due to a lack of endoscopic equipment or a high risk of treatment [21]. This prolonged the duration of foreign-body impaction and probably increased risk of complications [2, 3]. The esophageal foreign bodies that had been attempted to be removed at other hospitals may have been difficult to remove or associated with a high risk of bleeding and perforation. The associated risk may also have increased after the foreign body was pulled on in the other hospital. Therefore, it is essential to improve the diagnosis and treatment of esophageal foreign bodies in primary hospitals and transfer patients with difficult-to-remove foreign bodies to specialized or tertiary hospitals in time.
No significant differences were found in complications among doctors from different departments and with differing levels of seniority (Table 2). The anesthesia method did not significantly affect the risk of mucosal injury or bleeding in patients with esophageal foreign body, but sedation anesthesia was a risk factor for mucosal perforation, which was related to the fact that doctors often prefer to perform endoscopic treatment under general anesthesia for patients with perforation or a high risk of perforation. Clinically, improper endoscopic treatment or poor patient cooperation may lead to failure of foreign-body removal or serious complications, especially in the case of sharp foreign bodies [22] or foreign bodies in the esophageal entrance (where removal may cause the patient nausea). Compared with endoscopy under sedation anesthesia, routine gastroscopy under topical pharyngeal anesthesia often causes severe nausea, vomiting, and pharyngeal muscle contraction due to pharyngeal irritation, which can also affect the doctor’s operative performance. In the present study, poor cooperation occurred in 20 patients, only one of whom was under sedation anesthesia. In 8 patients, the foreign body fell off the forceps during endoscopic removal, and only one of these patients was under sedation anesthesia. This suggested that endoscopic treatment under sedation anesthesia could reduce the operational risk caused by poor patient cooperation. However, we did not find that sedation anesthesia significantly impacted the success rate of endoscopic treatment, which is consistent with previous study [1]. In addition, this study found that endoscopy in the nighttime was an independent risk factor for mucosal bleeding, while same-day endoscopic treatment did not affect the risk of mucosal bleeding. Therefore, considering only the bleeding risk, treatment in the daytime of the next day may be a better choice for patients who visit at night.
This study found that the COVID-19 period was a risk factor for mucosal perforation, as it prolonged the duration of foreign-body impaction due to the traffic during the epidemic period and the surveys of COVID-19 infection. The COVID-19 period was an independent risk factor for non-same-day endoscopic treatment. The decrease in the number of patients with esophageal foreign body in 2020 compared with 2019 may be related to the reduction of dinner activities and traffic during the epidemic period. Some studies have reported that there is a difference in the clinical characteristics of patients with esophageal foreign bodies presenting on the weekdays and on holidays [12, 23], and that complications are more common in patients who present on holidays [23]. We also found that endoscopic treatment during holidays was an independent risk factor for mucosal bleeding.
The recommended time for removing esophageal foreign bodies is within 24 h, because a delay decreases the rate of successful removal and increases the risk of complications [3, 17, 18]. However, some studies show that delayed intervention or removal beyond 24 h did not affect the complication rate [24, 25], and endoscopic treatment could wait until the following morning [26]. Our study found that patients with a complaint time of 6–12 h had a significantly higher risk of complications than patients with a complaint time of 1–3 days, which may be related to the acute phase of esophageal wall edema. Early endoscopic treatment could also increase the risk of mucosal injury due to the poor observation caused by food reflux and esophageal edema. No significant difference in bleeding risk was found between groups with complaint times varying from 6 h to 72 h. Same-day endoscopic treatment also did not affect the risk of mucosal bleeding. Therefore, according to the results of this study, patients with complaint times of < 6 h or ≥ 72 h should be treated as early as possible, while those with complaint times of ≥ 6 h can be treated within 3 days from impaction. Notably, the risk of mucosal perforation did not differ between groups of patients with complaint times of 6–24 h, while same-day endoscopic treatment was a protective factor. Therefore, esophageal foreign bodies that may cause or have already caused perforation should be treated as early as possible in patients with complaint times of < 6 h or ≥ 24 h; In patients with complaint times of ≥ 6 h but < 24 h, the treatment could be delayed but should still be performed on the same day.
The timing of endoscopic treatment is affected by many factors, and whether patients who visit at night require immediate treatment is worthy of careful consideration [20]. Early endoscopic treatment may increase the operational risk due to the choice of routine gastroscopy. If sedation anesthesia is selected, the risk of aspiration may be increased. Esparaz et al. found that waiting until the following morning had minimal impact on the complications and success rate of esophageal foreign-body removal [26]. In addition, non-emergent foreign bodies could be removed within 18.5 h to decrease the rate of serious complications [27]. This study also suggests that waiting until the following day is a feasible option for patients with a low risk of perforation and no obvious symptoms. However, delayed treatment can result in a possibility of foreign body spontaneously dropping and getting displaced. A negative identification rate of 67% has been reported for suspected esophageal foreign bodies that remained in the esophagus for more than 24 h [2]. This study found that factors such as visiting time, anesthesia method, and gender could affect the timing of endoscopic treatment. Patients who visited the hospital late at night with no obvious symptoms were often advised by doctors to undergo endoscopy the next day. The fasting time required for sedation anesthesia may also cause the treatment to be delayed until the next day for patients visiting at night. This study found that female patients were more willing to undergo routine gastroscopy under topical pharyngeal anesthesia; however, the reason for their preference for same-day endoscopic treatment is yet to be determined. Clinically, the choice of the anesthesia method and endoscopic treatment timing deserve more research for patients who visit at night or have prolonged foreign-body impaction.
The study has some limitations. First, factors such as the type and shape of the foreign body are well-established risk factors associated with complications, which may influence patients’ behaviors and contribute to practical considerations. Second, conducting subgroup analyses based on the factors of the foreign-body itself and implementing multicenter studies could reduce the selection bias and provide more evidence. Finally, as this is a retrospective study, some clinically important factors, such as patients with mental retardation were not collected for analysis, and the perforations resulting from endoscopic procedures was also not be distinguished. Future prospective, interventional research is necessary to validate these findings and provide stronger evidence for guiding clinical practice.
In conclusion, the complications of esophageal foreign-body removal are not only related to the foreign body itself but also to practical factors like the complaint time, visiting time, and same-day treatment. After a full risk assessment, an appropriate waiting period and more comfortable sedation anesthesia may be beneficial for selected patients, especially for those visiting at night. These findings could serve as a valuable reference for establishing guidelines for the retrieval of esophageal foreign bodies, particularly in non-emergency cases.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors want to thank all the staff in the Department of Gastroenterology and the Endoscopy Center for their technical support.
Abbreviations
- COVID-19
Coronavirus disease 2019
Author contributions
Study design, interpretation of data and funding acquisition: Feng Ye; Study design and Interpretation of data: Guoxin Zhang. Acquisition of data: Zhi He, Qing Xu, Wentao Fan and Jinjin Shi. Statistical analysis: Zhi He and Qing Xu. Drafting the article: Zhi He and Feng Ye. All authors had full access to all of the data and approved the final version of this manuscript submitted.
Funding
This study was supported in part by Six Talent Peaks Project in Jiangsu Province (No. 2018-WSW-003), Jiangsu Provincial Medical Key Disciplines (No. ZDXK202206). Education Research Project of Nanjing Medical University (No. 2023LX052).
Data availability
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
This study protocol was reviewed and approved by the ethics committee of the First Affiliated Hospital of Nanjing Medical University (no. 2023-SR-013). All patients signed relevant informed consent forms.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Zhi He and Qing Xu are contributed equally to this work.
References
- 1.Geng C, Li X, Luo R, Cai L, Lei X, Wang C. Endoscopic management of foreign bodies in the upper gastrointestinal tract: a retrospective study of 1294 cases. Scand J Gastroenterol. 2017;52(11):1286–91. [DOI] [PubMed] [Google Scholar]
- 2.Park YK, Kim KO, Yang JH, Lee SH, Jang BI. Factors associated with development of complications after endoscopic foreign body removal. Saudi J Gastroenterology: Official J Saudi Gastroenterol Association. 2013;19(5):230–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang X, Jiang Y, Fu T, Zhang X, Li N, Tu C. Esophageal foreign bodies in adults with different durations of time from ingestion to effective treatment. J Int Med Res. 2017;45(4):1386–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Committee ASP, Ikenberry SO, Jue TL, Anderson MA, Appalaneni V, Banerjee S, Ben-Menachem T, Decker GA, Fanelli RD, Fisher LR, et al. Management of ingested foreign bodies and food impactions. Gastrointest Endosc. 2011;73(6):1085–91. [DOI] [PubMed] [Google Scholar]
- 5.Birk M, Bauerfeind P, Deprez PH, Hafner M, Hartmann D, Hassan C, Hucl T, Lesur G, Aabakken L, Meining A. Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48(5):489–96. [DOI] [PubMed] [Google Scholar]
- 6.Zhang X, Zhang X, Tu C, Yu Q, Fu T. Analysis of the management and risk factors for complications of esophageal foreign body impaction of jujube pits in adults. Wideochirurgia i inne Techniki Maloinwazyjne = Videosurgery Other Miniinvasive Techniques. 2018;13(2):250–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruan WS, Li YN, Feng MX, Lu YQ. Retrospective observational analysis of esophageal foreign bodies: a novel characterization based on shape. Sci Rep. 2020;10(1):4273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feng S, Peng H, Xie H, Bai Y, Yin J. Management of Sharp-Pointed Esophageal Foreign-Body Impaction With Rigid Endoscopy: A Retrospective Study of 130 Adult Patients. Ear, nose, & throat journal. 2020;99(4):251–258. [DOI] [PubMed]
- 9.Topaloglu O, Kilic KN, Karapolat S, Aydin Y, Turkyilmaz A, Taslak Sengul A, Eroglu A, Basoglu A. Diagnosis, treatment, and management of esophageal foreign bodies in patients with mental retardation: a retrospective study from three centers. Turk Gogus kalp damar cerrahisi dergisi. 2024;32(2):179–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scheppach W, Hauschild M, Zwicker M, Konwisorz A, Schubring M, Reissmann N. [Ingestion of foreign bodies by young patients with borderline personality disorder]. Z Gastroenterol. 2022;60(5):779–83. [DOI] [PubMed] [Google Scholar]
- 11.Kadriyan H, Primayanti I, Syamsidar S, Fakhrussiam LF, Rozi MF, Hijrinelly H. Case Report: modified endoscopic hook for extracting magnetic esophageal foreign bodies in a rural area. F1000Research. 2023;12:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu L, Lei G, Liu Y, Wei Z, Yin Y, Li Y, Wang G. Retrospective analysis of esophageal foreign body ingestion: differences among weekday, weekends, and holidays. Risk Manage Healthc Policy. 2021;14:2499–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sagvand BT, Najafali D, Yardi I, Sahadzic I, Afridi L, Kohler A, Afridi I, Kaur N, Tran QK. Emergent Endoscopy for esophageal foreign body removal: the impact of location. Cureus. 2022;14(2):e21929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gong H, Wei W, Huang Z, Hu Y, Liu XL, Hu Z. Endovascular stent-graft treatment for aortoesophageal fistula induced by an esophageal fishbone: two cases report. World J Clin Cases. 2022;10(7):2206–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang S, Wang J, Wang J, Zhong B, Chen M, Cui Y. Transparent cap-assisted endoscopic management of foreign bodies in the upper esophagus: a randomized, controlled trial. J Gastroenterol Hepatol. 2013;28(8):1339–42. [DOI] [PubMed] [Google Scholar]
- 16.Ooi M, Young EJ, Nguyen NQ. Effectiveness of a cap-assisted device in the endoscopic removal of food bolus obstruction from the esophagus. Gastrointest Endosc. 2018;87(5):1198–203. [DOI] [PubMed] [Google Scholar]
- 17.Triadafilopoulos G, Roorda A, Akiyama J. Update on foreign bodies in the esophagus: diagnosis and management. Curr Gastroenterol Rep. 2013;15(4):317. [DOI] [PubMed] [Google Scholar]
- 18.Sung SH, Jeon SW, Son HS, Kim SK, Jung MK, Cho CM, Tak WY, Kweon YO. Factors predictive of risk for complications in patients with oesophageal foreign bodies. Digestive and liver disease: official journal of the Italian Society of Gastroenterology and the Italian Association for the study of the liver. 2011;43(8):632–5. [DOI] [PubMed]
- 19.Tambakis G, Schildkraut T, Delaney I, Gilmore R, Loebenstein M, Taylor A, Holt B, Tsoi EH, Cameron G, Demediuk B, et al. Management of foreign body ingestion in adults: time to STOP and rethink endoscopy. Endoscopy Int open. 2023;11(12):E1161–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Karb D, DeLozier S, Raad D, Dumot J, Mok S. Effect of delayed endoscopy protocol on timing and safety of Endoscopy for Foreign Body Ingestion and Esophageal Food Impaction. J Clin Gastroenterol. 2023;57(9):890–4. [DOI] [PubMed] [Google Scholar]
- 21.Li L, Du T, Hu Y. The effect of different classification of hospitals on medical expenditure from perspective of classification of hospitals framework: evidence from China. Cost effectiveness and resource allocation: C/E. 2020;18:35. [DOI] [PMC free article] [PubMed]
- 22.Hong KH, Kim YJ, Kim JH, Chun SW, Kim HM, Cho JH. Risk factors for complications associated with upper gastrointestinal foreign bodies. World J Gastroenterol. 2015;21(26):8125–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhong Q, Jiang R, Zheng X, Xu G, Fan X, Xu Y, Liu F, Peng C, Ren W, Wang L. Esophageal foreign body ingestion in adults on weekdays and holidays: a retrospective study of 1058 patients. Medicine. 2017;96(43):e8409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu WT, Chiu CT, Kuo CJ, Lin CJ, Chu YY, Tsou YK, Su MY. Endoscopic management of suspected esophageal foreign body in adults. Dis Esophagus: Official J Int Soc Dis Esophagus. 2011;24(3):131–7. [DOI] [PubMed] [Google Scholar]
- 25.Krill T, Samuel R, Vela A, Marcondes F, Zaibaq J, Guturu P, Parupudi S. Outcomes of delayed endoscopic management for esophageal soft food impactions. Gastrointest Endosc. 2020;91(4):806–12. [DOI] [PubMed] [Google Scholar]
- 26.Esparaz JR, Carter SR, Mathis MS, Chen MK, Russell RT. Esophageal foreign body management in children: can it wait? J Laparoendoscopic Adv Surg Techniques Part A. 2020;30(12):1286–8. [DOI] [PubMed] [Google Scholar]
- 27.Lei T, Lu Q, Yang J, Re. Esophageal foreign body management in children: can it wait? By Esparaz. J Laparoendoscopic Adv Surg Techniques Part A. 2021;31(6):710–1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author upon reasonable request.