Abstract
Background
Increasing studies focused on the efficacy of acupuncture on pregnancy outcomes in patients with polycystic ovary syndrome (PCOS) undergoing in vitro fertilization-embryo transfer (IVF-ET). However, debatable conclusions have been drawn from different randomized controlled trials (RCTs), which might be related to different doses of acupuncture.
Objective
To evaluate whether acupuncture has a dose-dependent effect on pregnancy outcomes in patients with PCOS undergoing IVF-ET in systematically reviewing.
Methods
Seven electronic databases were searched from inception to October 10th, 2024. The Cochrane Collaboration’s tool ROB 2.0 (ROB 2.0) provided an assessment for the risk of bias. The acupuncture dose was extracted, then categorized into high, medium, and low dose according to the scoring system results, the evidence was assessed by Slavin’s qualitative best-evidence synthesis approach in a rigours methodological way. Clinical pregnancy rate (CPR) was regarded as the primary outcome.
Results
A total of 953 subjects met the eligibility criteria in 12 RCTs were included, among which two studies were low dose, four were medium dose, and six were high dose. The overall quality of included studies was low, 50.00% (6/12) studies were low risk, 16.67% (2/12) studies were some concerns, and 33.33% (4/12) studies were high risk. Comparing the results, the consistent high-dose result among high-quality trials provides strong evidence for a positive correlation between high-dose acupuncture and pregnancy outcomes.
Conclusion
A trend indicates that higher acupuncture doses yield better outcomes for PCOS patients undergoing IVF-ET. Further confirmation through direct comparisons of different doses was needed.
Trial registration
The systematic review has been registered on PROSPERO (https://www.crd.york.ac.uk/prospero/), and the registration number is CRD42023400187.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12906-024-04695-9.
Keywords: Acupuncture therapy, Acupuncture treatment dose, Polycystic ovary syndrome (according to ICD-10 manual), Systematic review, Pregnancy rate
Background
Polycystic ovary syndrome (PCOS) characterized by metabolic disorder affecting women of childbearing age, is estimated at 6% to 10% [1] worldwide. Clinical symptoms encompass oligomenorrhea, amenorrhea, acne, and infertility in approximately 72% of cases [2]. In vitro fertilization-embryo transfer (IVF-ET) is a significant approach, chosen by 20% of PCOS patients [3]. Nevertheless, IVF-ET success rates for PCOS patients remains only 29% [4, 5]. Acupuncture, a fundamental component of traditional Chinese medicine, is garnering global recognition for its safety and efficacy in treating a wide range of diseases [6, 7] Acupuncture therapy has promising effects in promoting ovulation, improving high-quality embryo rate and endometrial receptivity by regulating the hypothalamic-pituitary-ovarian axis (HPOA) [8, 9], and finally achieving higher opportunity of pregnancy outcomes. Previous studies have suggested the essential role of the acupuncture dose–effect relationship in its therapeutic efficacy [10] as demonstrated in various non-gynecological conditions, including knee osteoarthritis, primary insomnia, and depressive disorders [11–13]. However, the dose-dependent relationship in PCOS patients undergoing IVF-ET remains unclear. This study endeavors to comprehensively collect and analyze all related RCTs to determine whether exhibit a dose-dependent effect on improving pregnancy outcomes in PCOS patients undergoing IVF-ET in systematic analysis and provide evidence for clinical treatment and further research in the future.
Methods and design
Study registration
The systematic review has been registered on PROSPERO (https://www.crd.york.ac.uk/prospero/, registration number: CRD42023400187). We conducted this review according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [14].
Search strategy
Seven databases were searched, including EMbase (via Ovid), Medline (via Ovid), Cochrane Library (via Ovid), China National Knowledge Infrastructure (CNKI), WanFang database (WF), Chinese Science and Technology Periodical Database (VIP), and Chinese Biological Medicine (CBM), and retrieved from inception to October 10th, 2024. Besides, language was restricted to English and Chinese. The search strategy was built on the rule of combining subject words with free words, and it was modified according to the different characteristics of each database. The details are shown in Supplementary Material S1.
The inclusion criteria
(1) Participants: Women diagnosed with PCOS according to the 2003 Rotterdam criteria [15] and receiving IVF-ET without restrictions of race, region, and education level. (2) Interventions: Traditional acupuncture or electroacupuncture on the verum acupoints or meridians was selected as the main adjuvant treatment. (3) Comparison: Sham acupuncture (SA) or placebo, medications, no adjuvant treatments, or the same acupuncture therapy with different doses compared with the intervention group. (4) Outcomes: The primary outcome was Clinical pregnancy rate (CPR). Clinical pregnancy is defined with [16] fetal heartbeat, fetal bud, or placenta in the 5th week after ET by transvaginal ultrasound Secondary outcomes were performed to access other pregnancy-related outcomes (biochemical pregnancy rate [BPR], ongoing pregnancy rate [OPR], live birth rate [LBR]),endometrial thickness, and the high-quality embryo rate (HQER). (5) Study design: only RCTs presented in English or Chinese were included.
The exclusion criteria
(1) Systematic retrospective studies, quasi-randomized trials, animal experiments, case reports, and conference abstracts. (2) Unavailable in the full text. (3) Duplicate data. (4) Acupuncture treatment was not the only variable between groups. (5) No corresponding outcome indicators were included. It was excluded if one of the above criteria was met.
Data extraction and methodological quality
Selection of studies
All identified studies were imported to the NoteExpress software Version 3.0 (Aegean Music Technology Co, Beijing, China) to eliminate duplicate studies. The reviewers (JJL and XYT) independently read the abstract, title, and keywords to further select potentially eligible article. The reviewers resolved discrepancies through discussion, the third reviewer (LH) was involved if they were not solved after discussion. If necessary, contact the corresponding author to obtain the missing information.
Data extraction and management
The two reviewers (YTL and CLL), accessed study eligibility based on Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) criteria [17] and extracted data referring to the predesigned extraction form, which included the following information: (1) Characteristics of baseline participants (age, sample size, and…..); (2) Intervention and control groups (stimulation style, duration, and frequency, needle retention time, number of acupoints); (3) Outcomes (specific values for primary and secondary outcomes and P versus 0.05, adverse events). Dissertations and journal articles with the same data were considered together for data extraction. If it could not reach a consensus, another reviewer (HY) was consulted and a decision was made by majority vote.
Assessment of risk of bias in included studies
We used the Cochrane Collaboration’s tool ROB 2.0 [18, 19] to access the risk of bias, which evaluates five domains: (1) Randomization process; (2) Deviations from the intended interventions; (3) Missing outcome data; (4) Measurement of the outcome; (5) Selection of the reported result. Overall low risk when all domains were labeled as low risk, and overall high risk or some concerns if at least one domain was noted as high risk or some concerns. Two reviewers (XYT and YTL) independently accessed and then cross-checked at the end. In cases of disagreement, the two reviewers discussed the issues to reach a consensus. If consensus couldn't be reached, a third reviewer (HY) was consulted.
Assessment of acupuncture treatment
The four criteria were presented to calculate the dose [20]: (1) The number of acupoints at each treatment; (2) De qi response; (3) Frequency of treatments per week; (4) The duration of treatments. Each of the four parameters was individually scored as either high or low dose based on specific criteria: (1) > 10 acupoints; (2) having de qi response; (3) Frequency was > 4 per week; (4) The duration of treatments was > 2 menstrual cycles. The high dose was scored + 1, the low dose was -1. Then, the high (range 2 to 4), medium (score -1 to 1), and low dose (range -4 to -2) groups were calculated by total of each parameter. Two reviewers (CLL and XYZ) independently scored each parameter, and a third reviewer (JJL) categorized the results as high, medium, or low. The reviewers were blinded to each other.
Outcome synthesis and analysis
Outcomes were considered valid if there was a significant difference (P < 0.05) between the acupuncture and control groups. Positive outcomes were defined as the intervention group having significant better results than the control group. Slavin’s qualitative best-evidence synthesis approach was applied to solve the heterogeneity [21]. The approach categorized evidence into four level (strong, moderate, limited, inconclusive) based on the quality and results of the included studies. Details shown in Supplemental Material S2.
Results
Search results
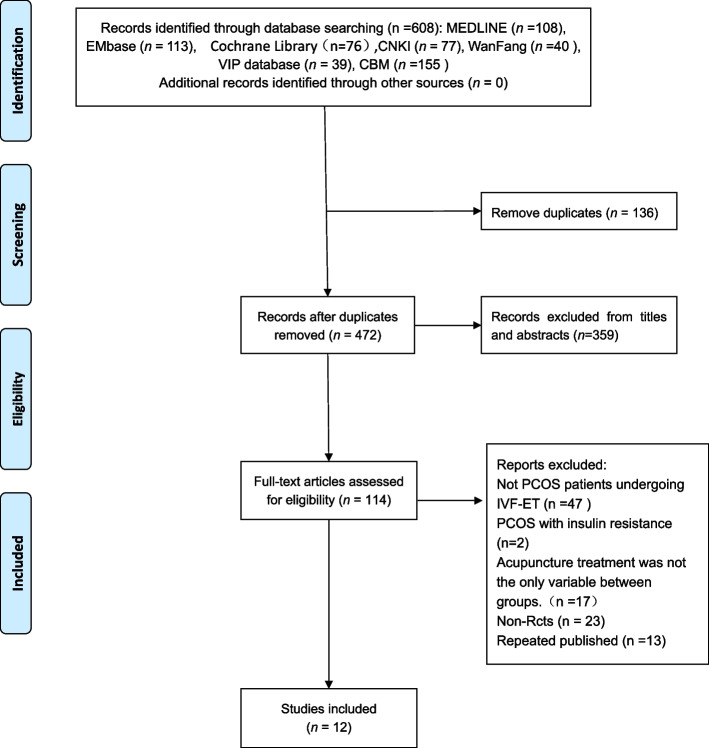
A total of 608 studies were retrieved according to a pre-set search strategy.136 duplicated studies were excluded, 359 studies were out of including criteria after screening the titles and abstracts. After an independent full-text review, 102 studies were excluded, 12 [22–33] studies for further analysis. The reasons for exclusion and the screening process are shown in Fig. 1.
Fig. 1.
The PRISMA flow diagram of study selection process
Characteristics of the eligible studies
Twelve eligible RCTs with 953 participants were published between 2009—2022 and conducted in two countries (11 in China and 1 in Iran). Four trials were conducted by the same research team. Two trials were designed in four-arm trials, and we extracted only the groups that met the criteria. Among these acupoints, the top three most frequently mentioned were Guanyuan (CV4), Zigong (EX-CA1), and Sanyinjiao (SP6), details of frequency can be found in Supplemental Material S3. In the high-dose studies, the total number of acupoints ranged from 10 to 15, in the medium-dose studies from 6 to 10, and in the low-dose studies from 6 to 8. The intervention was varied, such as manual acupuncture (MA) [26–31], electro-acupuncture (EA) [22, 23, 25, 32, 33], or EA with standard therapies [24]. Most of the control group received no acupuncture [22, 23, 26–33], with one studies comparing with the SA [25], and another study applied only standard therapies [24]. De qi response was found in all trials. Regarding the frequency of treatment, once daily was the most common, followed by once every other day, two studies was twice a week and only one study was three times a week. All studies uniformly adopted specific time points as their reference points for treatment initiation and conclusion within the IVF-ET process. This approach resulted in ambiguity in quantifying the duration of treatments due to the variability in IVF-ET protocols among patients. One study [31] received acupuncture intervention within the menstrual cycle, while two studies [26, 27] had three menstrual cycles of acupuncture before starting IVF-ET. Six studies [22, 23, 29, 32, 33, 28]conducted treatment procedures in the menstrual cycle before and also during controlled ovulation hyperstimulation (COH) until the HCG day. Two studies [24, 25] implemented acupuncture therapy within the COH cycle until the day of egg retrieval. Notably, only one study [30] performed a total of five acupuncture sessions separately at the start of down-regulation, the start of stimulation, two days before oocyte retrieval, and before and after embryo transfer (ET) day. All the characteristics we summarized in Table 1.
Table 1.
The characteristics of include studies
| Style | CPR(%) | HQER(%) | LBR(%) | BPR(%) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author | Location | Mean age(years) | N(A/C) | A | C | A | C | A | C | A | C | A | C | ||||
| Wu 2022 [31] | China | 29 | 83(40/43) | MA | No Acupuncture | 72.5 | 48.8 | + | 30.0 | 16.3 | - | ||||||
| Rashidi 2013 [30] | Iran | 31 | 62(31/31) | MA | No Acupuncture | 25.8 | 16.1 | - | 3.75; 0.45 | 3.5; 0.82 | + | 25.8 | 16.1 | - | |||
| Altutunji 2019 [29] | China | Unclear | 102(33/69) | MA | No Acupuncture | 33.33 | 14.5 | + | 42.40 | 21.70 | - | ||||||
| Chen 2009 [23] | China | 32.4 | 96(50/46) | EA | No Acupuncture | 37.77 | 31.07 | - | 63.53 | 50.11 | + | ||||||
| Li 2015 [22] | China | 31 | 217(119/98) | EA | No Acupuncture | 53.19 | 44.83 | - | 50.81 | 42.33 | + | ||||||
| Xing 2022 [27] | China | 34 | 68(34/34) | MA | No Acupuncture | 67.6 | 38.2 | + | 64.7 | 35.3 | + | 32.4 | 61.8 | + | |||
| Wu 2021 [26] | China | 31 | 100(50/50) | MA | No Acupuncture | 56 | 36 | - | 70.24 ± 24.79 | 48.79 ± 25.52 | + | ||||||
| Ye 2020 [28] | China | 29 | 83(40/43) | MA | No Acupuncture | 72.5 | 48.8 | + | 30 | 16.3 | - | ||||||
| Li 2011 [25] | China | 28 | 62(31/31) | EA | SA | 56 | 49 | + | 70 | 62 | + | ||||||
| Guo 2022 [24] | China | 30.16 | 100(50/50) | EA + Meds | Meds | 75 | 58 | + | 82.3 | 70.3 | + | ||||||
| Li 2012 [32] | China | 29.9 | 141(74/67) | EA | No Acupuncture | 48.48 | 37.70 | - | 61.52 ± 22.20 | 50.55 ± 16.15 | + | ||||||
| Li 2009 [33] | China | 32.56 | 43(23/20) | EA | No Acupuncture | 45.67 | 37.93 | - | 60.2 ± 22.20 | 50.55 ± 16.15 | + | ||||||
| OPR(%) | MR(%) | Endometrial thickness (mm) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author | A | C | A | C | A | C | Points needled | Frequency of treatment (in a week) | The total number of treatments (Menstrual Cycle) | |||
| Wu 2022 [31] | 9.77 ± 2.59 | 9.3 ± 1.98 | - | 11 | 4 | 3 | ||||||
| Rashidi 2013 [30] | 19.4 | 16.1 | - | 6.6 | 3.3 | - | 8 | < 1 | ||||
| Altutunji 2019 [29] | 33.30 | 14.50 | - | 0 | 2.90 | + | 10.4 ± 1.98 | 10.3 ± 2.05 | - | 15 | 7 | 1 ~ 2 |
| Chen 2009 [23] | 9 | 7 | 1 ~ 2 | |||||||||
| Li 2015 [22] | 4.0 | 5.13 | - | 6 | 5 | 1 ~ 2 | ||||||
| Xing 2022 [27] | 4.98 ± 0.71 | 5.23 ± 0.76 | + |
10/10/9/9 (4 stages) |
3 | 3 | ||||||
| Wu 2021 [26] | 2.01 ± 0.25 | 1.20 ± 0.24 | + | 11 | 4 | 3 | ||||||
| Ye 2020 [28] | 9.77 ± 2.59 | 9.39 ± 1.98 | - | 12 | 4 | 1 ~ 2 | ||||||
| Li 2011 [25] | 6 | 4 | < 1 | |||||||||
| Guo 2022 [24] | 6 | 10 | + | 12 | 7 | < 1 | ||||||
| Li 2012 [32] | 9.7 ± 1.8 | 10.00 ± 1.2 | - | 10 | 5 | 1 ~ 2 | ||||||
| Li 2009 [33] | 10.5 ± 1.3 | 10.00 ± 1.6 | - | 8 | 5 | 1 ~ 2 | ||||||
MA Manual Acupuncture, EA Electroacupuncture, SA Sham acupuncture, Meds Medicines, N(A/C) Numbers(Acupuncture group/Control group), A Acupuncture group, C Control group, CPR Clinical pregnancy rate, HQER High-quality embryo rate, LBR Live birth rate, BPR Bochemical pregnancy rate, OPR Ongoing pregnancy rate, MR Miscarriage rate
+ : Between-group differences were statistically significant (P < 0.01, P < 0.05)
-: Between-group differences were no statistically significant (P > 0.05)
Correlation between acupuncture dose and efficacy
Two studies [25, 30] evaluating the effects of acupuncture on pregnancy outcomes were low-dose, with a total parameter sum of -2; and another four studies [22, 23, 32, 33] were moderate dose, with a total parameter sum of 0. Six [24, 26–29, 31] studies were high-dose, and the results indicated that acupuncture was more effective for pregnancy outcomes (Tables 2 and 3). The consistent high-dose result among high-quality trials provides strong evidence for a positive correlation that high-dose acupuncture and pregnancy outcomes. The negative and positive results distribution was summarized in Table 4. All trials observed CPR outcomes, with Three [27, 28, 31] studies reporting LBR, seven [23–26, 30, 32, 33] reporting HQER, seven [26–29, 31–33] reporting endometrial thickness, three [27, 29, 30] reporting BPR, two [29, 30] studies reporting OPR, and Five [22, 24, 29, 30, 32] studies reporting MR. There were 100.00% (6/6) of the high-dose group, 0.00% (0/4) of the medium-dose group, and 50.00% (1/2) of the low-dose group showed positive CPR outcome.
Table 2.
The specific results of the scoring system
| Study | Primary outcome | |
|---|---|---|
| CPR | Sum | |
| High dose | ||
| Wu 2022 [31] | + | 4 |
| Altutunji 2019 [29] | + | 2 |
| Xing 2022 [27] | + | 2 |
| Wu 2021 [26] | + | 4 |
| Ye 2020 [28] | + | 2 |
| Guo 2022 [24] | + | 2 |
| Moderate dose | ||
| Chen 2009 [23] | - | 0 |
| Li 2015 [22] | - | 0 |
| Li 2012 [32] | - | 0 |
| Li 2009 [33] | - | 0 |
| Low dose | ||
| Rashidi 2013 [30] | - | -2 |
| Li 2011 [25] | - | -2 |
LD low dose, MD moderate dose, HD high dose, CPR Clinical pregnancy rate
+ : Between-group differences were statistically significant (P < 0.01, P < 0.05)
-: Between-group differences were no statistically significant (P > 0.05)
Table 3.
The specific results of the scoring system
| Parameter values | |||||
|---|---|---|---|---|---|
| Auther | Points needled | De qi responses | Frequency of treatment | The total number of treatment sessions | sum |
| Wu 2022 [31] | 1 | 1 | 1 | 1 | 4 |
| Rashidi 2013 [30] | -1 | 1 | -1 | -1 | -2 |
| Altutunji 2019 [29] | 1 | 1 | 1 | -1 | 2 |
| Chen 2009 [23] | -1 | 1 | 1 | -1 | 0 |
| Li 2015 [22] | -1 | 1 | 1 | -1 | 0 |
| Xing 2022 [27] | 1 | 1 | -1 | 1 | 2 |
| Wu 2021 [26] | 1 | 1 | 1 | 1 | 4 |
| Ye 2020 [28] | 1 | 1 | 1 | -1 | 2 |
| Li 2011 [25] | -1 | 1 | -1 | -1 | -2 |
| Guo 2022 [24] | 1 | 1 | 1 | -1 | 2 |
| Li 2012 [32] | -1 | 1 | 1 | -1 | 0 |
| Li 2009 [33] | -1 | 1 | 1 | -1 | 0 |
Table 4.
Percentage of negative and positive outcomes in different doses
| CPR | HQER | LBR | BPR | OPR | MR | Endometrial thickness | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dose | Results( +) | Results(-) | Results( +) | Results(-) | Results( +) | Results(-) | Results( +) | Results(-) | Results( +) | Results(-) | Results( +) | Results(-) | Results( +) | Results(-) |
| LD | 1/2 | 1/2 | 2/2 | 0/0 | 0/0 | 0/0 | 0/1 | 1/1 | 0/1 | 1/1 | 0/1 | 1/1 | 0/0 | 0/0 |
| MD | 0/4 | 4/4 | 4/4 | 0/0 | 0/0 | 0/0 | 0/0 | 0/0 | 0/0 | 0/0 | 0/2 | 2/2 | 0/2 | 2/2 |
| HD | 6/6 | 0/6 | 2/2 | 0/0 | 1/1 | 2/2 | 1/2 | 1/2 | 0/1 | 1/1 | 2/2 | 0/2 | 2/5 | 3/5 |
LD low dose, MD moderate dose, HD high dose, CPR Clinical pregnancy rate, HQER high-quality embryo rate, LBR live birth rate, BPR biochemical pregnancy rate, OPR ongoing pregnancy rate, MR miscarriage rate
Risk of bias assessment
The results of ROB 2.0 were displayed in Table 5. There were 50.00% (6/12) of studies assessed as low risk, 16.67% (2/12) studies were some concerns, and 33.33% (4/12) studies were high risk. The considerable drawbacks were the randomized process, the blinding settings, and the selective reporting outcomes. There was one study for some concerns and three studies for high risk in domain 1, one study was considered as some concerns in domain 2, one study was rated as high risk in domain 3, four studies were regarded as some concerns, and one for high risk in domain 5.
Table 5.
Risk of bias of included studies
| Randomization process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported result | Overall | |
|---|---|---|---|---|---|---|
| Li 2011 [25] |
|

|
|
|
|
|
| Li 2015 [22] |
|

|
|
|
|
|
| Wu 2021 [26] |
|

|
|
|
|
|
| Xing 2022 [27] |
|

|
|
|
|
|
| Wu 2022 [31] |
|

|
|
|
|
|
| Rashidi 2013 [30] |
|

|
|
|

|
|
| Altutunji 2019 [29] |
|

|
|
|
|
|
| Guo 2022 [24] |
|

|
|
|
|
|
| Ye 2020 [28] |
|

|
|
|
|
|
| Chen 2009 [23] |
|

|
|
|
|
|
| Li 2012 [32] |
|

|
|
|
|
|
| Li 2009 [33] |
|

|
|
|
|
|
 Low risk
Low risk
 Someconcerns
Someconcerns
 High risk
High risk
Discussion
We conducted a systematic review comprising 12 RCTs involving 953 participants to identify if acupuncture indicates dose-dependent efficacy. Six trials were regarded as low risk of bias, two as some concerns, and four as high risk. According to the results, the six high-dose studies showed a significant inclination towards a strong association with improved pregnancy outcomes in PCOS patients undergoing IVF-ET. However, this is only a preliminary conclusion based on the existing evidence. More relevant future RCTs are warranted to provide evidence or directly compare different doses to substantiate our conclusions.
In this systematic review, Guanyuan [CV4], Zigong [EX-CA1], Sanyinjiao [SP6] were the high frequency acupoints. Anatomically, the nerves responsible for the uterus, ovaries, and fallopian tubes predominantly originate from the eleventh thoracic nerve to the second lumbar nerve (T11—L2) and from the second to the fourth sacral nerve (S2—S4) [31]. The ganglionic innervation of these three acupoints (CV4, EX-CA1, and SP6) is precisely within this segmental range. It's evident that these high-frequency acupoints coherent with the distribution of nerves connected to reproductive function, with multiple segments of afferent nerves overlapping, potentially forming the neurological basis for a synergistic effect [32]. This multi-pathway, multi-link, multi-target neuro-endocrine network regulates the female reproductive endocrine system, thus reducing the cycle cancellation rate and improving IVF success rates [33, 34].
All the intervention group protocols emphasized inducing the De qi response, patients described De qi as sensations of soreness, heaviness, fullness, numbness, and warmth [34]. De qi response is generated when the needle insertion and manipulation create tension in the muscle fibers, triggering mast cell degranulation and accompanied with electrical signal transportation and biochemicals’ secretion to achieve the disease treatments [35–37]. Sham needling, a common control group setup in acupuncture studies, involves shallow or no skin punctures and does not elicit the same discomfort as De qi sensation [38]. The efficacy of acupuncture is generally determined by comparing the outcomes of the two group. Therefore, although De qi sensation is a subjective experience, it is also an objective therapeutic requirement of manipulation. This specific sensation is a key factor contributing to the efficacy of acupuncture and how to objectively quantify it needs to be further explored. Inadequate treatment courses can diminish the desired therapeutic effect. The duration of high-dose studies was 2—3 menstrual cycles. Prior studies have shown follicular growth spans approximately 3 to 4 months, and acupuncture can be beneficial when administered during the early stages of follicular development [30, 39]. This specific timeframe aligns with the treatment timing and duration of high-dose studies, further supporting the rationale that infertile PCOS patients benefit from extended interventions. Moreover, we also found that the dose effect was in fact related to the baseline characteristics of the study. In general, all high-dose trials were related to positive pregnancy outcomes. Unexpectedly, there was one exception of positive pregnancy outcomes with low-dose interventions. The characteristics of this low-dose study were the number of acupoints < 10 acupoints, frequency < 4 times per week; and duration < one menstrual cycle. The final score was -2, placing it within the low-dose range (-4 to -2). We hypothesized the reasons for this negative outcome by analyzing participants’ characteristics, offering innovative insights for future clinical practice. The mean age of participants was 28 years, and infertile duration was 3.0 ± 1.9 years, the baseline age was the youngest among all included studies. However, the aging uterus decreased ovarian reserve, and oocyte quality are key contributors to the aged-associated decline in fertility [40, 41]. Acupuncture may be particularly effective in younger patients with higher fertility, and these individuals might achieve improved pregnancy outcomes with low-dose interventions. Subsequent studies may consider enrolling infertile women of different ages and then respectively apply low, medium, or high dose acupuncture interventions to verify whether low-dose interventions were effective in young women. If results are favorable, optimization of clinical acupuncture protocols can serve the dual purpose of cost savings for patients while maximizing therapeutic efficacy.
Generally, study quality was low. In ROB.2.0, domain-1, domain-2, and domain-5 had considerable problems. In domain 1, the randomization was mentioned, but without detailing the method. In domain 2, the study failed to explain why there was a large difference in patient numbers between intervention and control groups. Moreover, one study failed to report all pre-established outcomes, and four studies rated some concerns for inadequate reporting about protocols and registration. These problems were prevalent in RCTs, future studies should employ rigorous experimental designs and provide more detail to reduce the risk of bias. Altogether, there were no direct comparisons about different doses, so this is only a narrative review of the extant indirect comparison, wherever possible, the effect of varying doses was compared within the same study may be more apparent.
To the best of our knowledge, this is the first review to comprehensively assess the relationship between pregnancy outcomes and acupuncture dose in PCOS patients undergoing IVF-ET from four aspects. We employed a four-parameters system, which was referential and feasible, drawing from previously published dose-related research, Chinese clinical experience and empirical data [20, 42]. The scoring results were verified by sensitivity analysis to reduce arbitrariness. To make the scoring criteria appropriate to the pregnancy-related study, we modified them according to the female characteristics and IVF-ET protocols. We still predetermined CPR as the primary outcome while the fact that the LBR is a visual predictor of pregnancy outcomes. The number of included studies reporting LBR was considerably lower than those reporting CPR, implying that CPR would allow for a larger dataset for analysis. Moreover, clinical pregnancy, being a practical and clinically relevant measure, approximates the ultimate live birth outcome [43, 44]. Our study covered a wide range of pregnancy-related outcomes, and both endometrial thickness and HQER, critical factors in IVF-ET success [45], providing more comprehensive perspectives and improving reliability. However, there were still several shortcomings. First, only the studies in the English and Chinese databases were screened due to language limitations, which may have resulted in inadequate inclusion. Second, because some studies did not specify the total number and frequency of treatments, we only infer an approximate range based on the descriptions of different IVF-ET protocols, which might lead to bias in our statistics. Therefore, adherence to STRICTA [17] requirements for reporting details and providing explicit evidence for dose-related studies is crucial. Third, the number of relevant studies we searched was limited, and the insufficient sample size may have impacted our statistics, so we conclusively state that there is a trend that high-dose acupuncture is consistently linked to better pregnancy outcomes. Fourth, Polycystic ovary syndrome (PCOS) is classified into four phenotypes according to Rotterdam criteria: A (sparse ovulation or anovulation [OA] + clinical manifestations of hyperandrogenism and/or hyperandrogenemia [HA] + ovarian polycystic changes [PCO]), B ([OA] + [HA]), C ([HA] + [PCO]), and D ([PCO] + [OA]) [46, 47]. All included studies diagnosed PCOS based on two out of three criteria: amenorrhea or oligomenorrhea, polycystic ovaries, and hyperandrogenism, without specifying the phenotype. including a population that met the Rotterdam criteria without explicitly limiting the subjects' phenotype prevented us from exploring the relationship between acupuncture dose and phenotype in detail. Lastly, our study is a narrative analysis that simply described and analyzed the relationship without figuring out an optimal acupuncture dose range. The Network meta-analysis (NMA) tool may compensate for this limitation.
Conclusion
Overall, this dose–effect review suggested an upward trend where higher acupuncture doses appear to improve pregnancy outcomes in PCOS patients undergoing IVF-ET. However, definitive conclusions are challenging to draw due to the absence of direct comparisons and the limited sample size, the exact quantitative-effectiveness relationship remains to be further clarified.
Supplementary Information
Acknowledgements
Not applicable.
Abbreviations
- PCOS
Polycystic ovary syndrome
- IVF-ET
In vitro fertilization-embryo transfer
- RCT
Randomized controlled trials
- CPR
Clinical pregnancy rate
- ART
Assisted reproductive treatment
- HOPA
Hypothalamic-pituitary-ovarian axis
- PRISMA
Preferred reporting items for systematic reviews and mata-analysis protocols
- STRICTA
Standards for Reporting Interventions in Clinical Trials of Acupuncture
- CNKI
China National Knowledge Infrastructure
- WF
WanFang database
- CBM
Chinese Biological Medicine
- VIP
Chinese Science and Technology Periodical Database
- SA
Sham acupuncture
- BPR
Biochemical pregnancy rate
- OPR
Ongoing pregnancy rate
- LBR
Live birth rate
- MR
Miscarriage rate
- HQER
High quality embryo rate
- CV4
Guanyuan
- EX-CA1
Zigong
- SP6
Sanyinjiao
- CV6
Qihai
- CV3
Zhongji
- HCG
Human chorionic gonadotropin
- COH
Controlled ovulation hyperstimulation
- ET
Embryo transfer
- CV
Conception vessel
- EOM
Endogenous opioid mechanisms
- NMA
Network meta-analysis
- OA
Sparse ovulation or anovulation
- HA
Clinical manifestations of hyperandrogenism and/or hyperandrogenemia
- PCO
Ovarian polycystic changes
Authors’ contributions
All the authors contributed to this review. YTL conceived and drafted the protocol and manuscript. JJL, XYT, and LH contributed to the literature search. YTL, CLL, and HY contributed to the data extraction. XYZ contributed to conducting the tables, and XYT, YTL, and HY contributed to the statistical analysis. JY, FRL, and XPT participated in reading and approving the final version of the manuscript. Furthermore, all authors approved the final version of the manuscript to submit. Due to the special characteristics of this manuscript, which was previously accepted in BMC pregnancy and childbirth and revised according to the reviewers ‘ comments, we added YZ as an author, who mainly contributed to polishing and revising the article according to the reviewers’ comments, and it was successfully accepted.
Funding
This study was supported by grants from the National Natural Science Foundation of China (No. 82174517 and No. 81973966).
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Xiao Ping Tian, Email: 5114438@qq.com.
Jie Yang, Email: jenny_yang_jie@126.com.
References
- 1.Barber TM, Dimitriadis GK, Andreou A, Franks S. Polycystic ovary syndrome: insight into pathogenesis and a common association with insulin resistance. Clin Med. 2016;16(3):262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen XX, Shi XS, Wang T. Clinical research progress on Chinese and Western integrative medicine treatment of polycystic ovarian syndrome. Asia-Pac Tradit Med. 2017;13(2):61–4.
- 3.Joham AE, Teede HJ, Ranasinha S, Zoungas S, Boyle J. Prevalence of Infertility and Use of Fertility Treatment in Women with Polycystic Ovary Syndrome: Data from a Large Community-Based Cohort Study. J Womens Health. 2015;24(4):299–307. [DOI] [PubMed]
- 4.Kotlyar AM, Seifer DB. Women with PCOS who undergo IVF: a comprehensive review of therapeutic strategies for successful outcomes. Reprod Biol Endocrinol. 2023;21(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu Y. Effectiveness of three controlled ovarian hyperstimulation protocols in IVF-ET for PCOS patients: A Systematic Review and meta-analysis. Lanzhou University; 2017. (in Chinese)
- 6.Liu BY, Chen B, Guo Y, Tian LX. Acupuncture-a national heritage of China to the world: international clinical research advances from the past decade. Acupunct and Herb Med. 2021;1(2):65–73.
- 7.Liang Y, Zhou J, Du JY, Shao XM, Fang JQ. Prospects for the development of acupuncture analgesia from an international perspective. World J Acupunct - Moxibustion. 2023;33(1):6–8. [Google Scholar]
- 8.Polycystic AR, Syndrome O. Obstet Gynecol. 2018;132(2):321–36. [DOI] [PubMed] [Google Scholar]
- 9.Huang DM, Huang GY, Lu FE, Dieterle S, Neuer A, Greb R. Acupuncture for infertility: is it an effective therapy? Chin J Integr Med. 2011;17(5):386–95. [DOI] [PubMed]
- 10.Shi XM. Study of the relationship between acupuncture dose and effect. Acupunct Herb Med. 2021;1(1):3–9. [Google Scholar]
- 11.Chung KF, Yeung WF, Yu BYM, Zhang SP, Zhang ZJ. Combined electroacupuncture and auricular acupuncture for primary insomnia: a randomised controlled trial of dose-response effect. 2019;25(1):28–33. [PubMed]
- 12.Sun N, Tu JF, Lin LL, et al. Correlation between acupuncture dose and effectiveness in the treatment of knee osteoarthritis: a systematic review. Acupunct Med. 2019;37(5):261–7. [DOI] [PubMed] [Google Scholar]
- 13.Xu GX, Lei HZ, Huang LY, et al. The dose-effect association between acupuncture sessions and its effects on major depressive disorder: A meta-regression of randomized controlled trials. J Affect Disord. 2022;310:318–27. [DOI] [PubMed] [Google Scholar]
- 14.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum Reprod (Oxford, England). 2004;19(1):41–7. [DOI] [PubMed]
- 16.Zegers HF, Nygren KG, Adamson GD, et al. The ICMART glossary on ART terminology. Hum Reprod. 2006;21(8):1968–70. [DOI] [PubMed] [Google Scholar]
- 17.MacPherson H, Altman DG, Hammerschlag R, et al. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): extending the CONSORT statement. J Alternative Complement Med (New York, NY). 2010;16(10):ST1–14. [DOI] [PubMed]
- 18.Cumpston M, Li T, Page MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:ED000142. [DOI] [PMC free article] [PubMed]
- 19.Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
- 20.Sun N, Tu JF, Lin LL, et al. Correlation between acupuncture dose and effectiveness in the treatment of knee osteoarthritis: a systematic review. medicine. J Br Med Soc. 2019;37(5):261–7. [DOI] [PubMed]
- 21.Re S. Best evidence synthesis: an intelligent alternative to meta-analysis. J Clin Epidemiol. 1995;48(1):9–18. [DOI] [PubMed]
- 22.Li J, Cui W, Sun W, Zhang QY, Guan Q. Effect of electro-acupuncture on the spindle and oocytes quality in patients with PCOS. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2015;35(3):304–9. [PubMed] [Google Scholar]
- 23.Chen J, Cui W, LI J, Sun W. Investigation on effect of electro acupunctrue intervention on in vitro fertilization and embryo transfer of patients with polycystic ovarian syndrome. Matern Child Health Care China. 2009;24(30):4262–4
- 24.Guo JJ, Wei AW, Song HY. Impact of Acupuncture Combined with Medicine on IVF-ET Fertility Outcomes of Polycystic Ovary Patients with Kidney Deficiency and Phlegm Dampness Syndrome. Acta Chin Med. 2022;10(37):2241–5.
- 25.Li YL. Clinical Study on Effect of Electro-acupuncture in Improving the Quality of Oocytes and Leukemia Inhibitory Factor in Follicular Fluid of polycystic ovarian syndrome patients Undergoing in vitro Fertilization and Embryo Transfer. Shandong University of Traditional Chinese Medicine; 2011. (in Chinese)
- 26.Wu JM, Zhuo YY, Tang M. Effect of Tiao Ren Tong Du Needling Method on Pregnancy Outcome After IVF -ET for Infertility Due to Polycystic Ovary Syndrome. Shanghai JAcu-mox. 2021;5(40):565–70.
- 27.Xing LW, Liu F, Dong QZ, Wu KN. Efficacy observation of staged acupuncture and moxibustion therapy based on the theory of thorough fare vessel being sea of blood' on frozen-thawed embryo transfer in patients with polycystic ovary syndrome. CJTCMP. 2022;5(37):2755–8.
- 28.Ye YY. Efects of Regulating Ren Du Acupuncture on IVF-ET Pregnancy Outcomes in PCOS Patients and Effects on Ovarian Granuosa Cells Based on ACTA/Smads Signaling Pathway. Guangzhou University of Chinese Medicine; 2020. (in Chinese)
- 29.Altutunji AZ, Liu L, Cai J, Wang Z, Gao Y. The effect of acupuncture on anti-mullerian hormone and assisted reproduction outcome in Polycystic Ovary Syndrome patients undergoing in vitro fertilization. J Pak Med Assoc. 2019;69(8):5. [PubMed] [Google Scholar]
- 30.Rashidi BH, Tehrani ES, Hamedani NA, Pirzadeh L. Effects of Acupuncture on the Outcome of in Vitro Fertilisation and Intracytoplasmic Sperm Injection in Women with Polycystic Ovarian Syndrome. Acupunct Med. 2013;31(2):151–6. [DOI] [PubMed] [Google Scholar]
- 31.Wu JM, Ning Y, Ye YY, et al. Effects of Acupuncture on Endometrium and Pregnancy Outcomes in Patients with Polycystic Ovarian Syndrome Undergoing in vitro Fertilization-Embryo Transfer: A Randomized Clinical Trial. Chin J Integr Med. 2022;28(8):736–42. [DOI] [PubMed] [Google Scholar]
- 32.Li J, Cui W, Sun W, Wen J, Feng J. Influence of using electro-acupuncture during COH on the pregnancy outcome in patients undergoing in-vitro-fertilization and embryo transfer. Shandong Medicine. 2012;52(37):7–10. [Google Scholar]
- 33.Li J, Cui W, Sun W. Electroacupuncture treatment on IVF-ET pregnancy outcome in patients with kidney deficiency PCOS. The Chinese Journal of Human Sexuality. 2009;18(07):28–30. [Google Scholar]
- 34.Sun R, He Z, Ma P, et al. The participation of basolateral amygdala in the efficacy of acupuncture with deqi treating for functional dyspepsia. Brain Imaging Behav. 2021;15(1):216–30. [DOI] [PubMed] [Google Scholar]
- 35.Hsiao IH, Liao HY, Cheng CM, Yen CM, Lin YW. Paper-Based Detection Device for Microenvironment Examination: Measuring Neurotransmitters and Cytokines in the Mice Acupoint. Cells. 2022;11(18):2869. [DOI] [PMC free article] [PubMed]
- 36.Li NC, Li MY, Chen B, Guo Y. A New Perspective of Acupuncture: The Interaction among Three Networks Leads to Neutralization. Evidence-based complementary and alternative medicine : eCAM. 2019;2019:2326867.30915143 [Google Scholar]
- 37.Gong YN, Li NC, Lv ZX, et al. The neuro-immune microenvironment of acupoints—initiation of acupuncture effectiveness. J Leukoc Biol. 2020;108(1):189–98. [DOI] [PubMed] [Google Scholar]
- 38.Liang ZH, Xie CC, Li ZP, Zhu XP, Lu AP, Fu WB. Deqi Sensation in Placebo Acupuncture: A Crossover Study on Chinese Medicine Students. Evidence-Based Complement Alternative Med. 2013;2013:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu DQ, Xiang S, Lian F. Effects of Electroacupuncture on In-Vitro Fertilization Outcomes and Differential Gene Expression in Polycystic Ovary Syndrome Patients with Phlegm-damp Syndrome. CJITWM. 2022;42(10):1180–6.
- 40.Nelson SM, Telfer EE, Anderson RA. The ageing ovary and uterus: new biological insights. Hum Reprod Update. 2013;19(1):67–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen L, Ma S, Xie M, et al. Oxygen concentration from days 1 to 3 after insemination affects the embryo culture quality, cumulative live birth rate, and perinatal outcomes. J Assist Reprod Gen. 2023:1–10. [DOI] [PMC free article] [PubMed]
- 42.Huang L, Xu G, Sun M, et al. Recent trends in acupuncture for chronic pain: A bibliometric analysis and review of the literature. Complement Ther Med. 2023;72:102915. [DOI] [PubMed] [Google Scholar]
- 43.Zhu C, Xia W, Huang J, et al. Effects of acupuncture on the pregnancy outcomes of frozen-thawed embryo transfer: A systematic review and meta-analysis. Front Public Health. 2022;10:987276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Clarke JF, van Rumste MM, Farquhar CM, Johnson NP, Mol BW, Herbison P. Measuring outcomes in fertility trials: can we rely on clinical pregnancy rates? Fertil Steril. 2010;94(5):1647–51. [DOI] [PubMed] [Google Scholar]
- 45.Gao CF. Effect of egg and embryo quality on biochemical pregnancy cycle during in vitro fertilization and embryo transplantation. China Modern Doc. 2020;58(04):5–7+11+193.
- 46.Lizneva D, Suturina L, Walker W, Brakta S, Gavrilova-Jordan L, Azziz R. Criteria, prevalence, and phenotypes of polycystic ovary syndrome. Fertil Steril. 2016;106(1):6–15. [DOI] [PubMed] [Google Scholar]
- 47.Feng Y, Tang Z, Zhang W. The role of macrophages in polycystic ovarian syndrome and its typical pathological features: A narrative review. Biomed Pharmacother. 2023;167:115470. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.