Abstract
Purpose
The conversion of knee arthrodesis to total knee arthroplasty (TKA) is a challenging procedure. This article aims to report a case of fusion knee with patellar absence who was converted to TKA and has achieved good results.
Methods
The patient, a 23 years old Tibetan Buddhist monk, sustained a left knee joint injury at the age of 12 due to a car accident, leading to subsequent knee arthrodesis at 18 years old as a result of recurrent severe infections. However, this procedure hindered his ability to perform daily meditation practices that required bending both knees and sitting cross-legged. After adequate preoperative preparation, with the help of customized osteotomy guide plate and customized 3D-printed porous tantalum patella, the 3D preoperative plan assisted TKA after arthrodesis was performed. The knee function was followed up to explore the clinical effect of above-mentioned surgical procedure.
Results
A 1-year follow-up showed significant improvement in postoperative knee function with improved scores for function outcomes, and the patient was satisfied with the conversion. The patient’s left knee improved significantly from preoperative immobility with 5° of fixed fusion to postoperative ROM of 0° to 100°, and the patient could squat and stand up, walk on the flat ground, and go up and down stairs.
Conclusion
Adequate preoperative communication with patients and good expectation management are crucial for ensuring favorable prognoses. Perfect preoperative planning and its reliable implementation during operation are essential. Additionally, postoperative rehabilitation and proactive management of complications play pivotal roles in achieving optimal clinical outcomes.
Level of evidence
IV.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12891-024-08086-6.
Keywords: Total knee arthroplasty, Arthrodesis, Fusion knee, Patellar absence, Customized 3D-printed porous tantalum patella, 3D preoperative plan, Customized osteotomy guide plate
Introduction
The knee arthrodesis is mainly used in destructive knee infection or trauma, which could improve the stability of knee joints and reduce pain [1]. Even the knee arthroplasty has been widely accepted, the arthrodesis is still applicable for some special occasion. However, the fusion of knee joint could cause severe loss of joint mobility and low quality of life. In addition, the negative impact of knee arthrodesis on patients’ social function cannot be ignored. It is reported that about 17 of 30 patients with knee arthrodesis have attempted suicide because of discrimination [2]. In some cases, it may be an option to convert the previous knee arthrodesis to total knee arthroplasty (TKA) [3]. Therefore, when facing with serious functional defects, discomfort of the fusion knee, poor quality of life, or extremely high expectation of knee mobility, we may convert the knee arthrodesis into TKA [4].
The conversion of knee arthrodesis to TKA is an extremely challenging surgical procedure. Sufficient soft tissue and an integrated knee extensor mechanism are essential for conversion [1]. Previous literature shows that its postoperative complications of even more than 50% [1, 5–7]. The purpose of this study is to report a case of fusion knee with patellar absence who was converted to TKA with good results.
Case report
Medical history
The case reported a 23-year-old male patient. He had a car accident when he was 12 years old, which injured his left knee joint and came up with serious knee infection. Because of the difficulty of routine treatment for infection, he had multiple surgeries and at last he had left knee arthrodesis in another hospital at the age of 18. The postoperative soft tissue healing and bone fusion were good. As a Tibetan Buddhist monk, the patient’s daily practice requires meditation that needs to bend both knee joints and sit cross-legged, which were not possible because of the knee arthrodesis. The preoperative infection-related test results of the patient are shown in Table 1.
Table 1.
Preoperative and postoperative infection-related test results
| Date | WBC (109/L) | NEU (109/L) | CRP (mg/L) | ESR (mm/h) |
|---|---|---|---|---|
| Pre-operation (3rd Day) | 4.1 | 2.9 | 2.4 | 3 |
| Post-operation (1st Day) | 11.9 | 11.3 | 8.7 | 2 |
| Post-operation (3rd Day) | 7.7 | 6.5 | 6.4 | 2 |
| Post-operation (5th Day) | 4.5 | 3.0 | 4.0 | 7 |
| Post-operation (7th Day) | 7.2 | 5.6 | 75.7 | 24 |
| Post-operation (9th Day) | 4.4 | 3.11 | 114.0 | 37 |
| Post-operation (11th Day) | 5.2 | 3.7 | 58.3 | 27 |
WBC: White blood cell; NEU: Neutrophil; CRP: C-reactive protein; ESR: Erythrocyte sedimentation rate
Examination
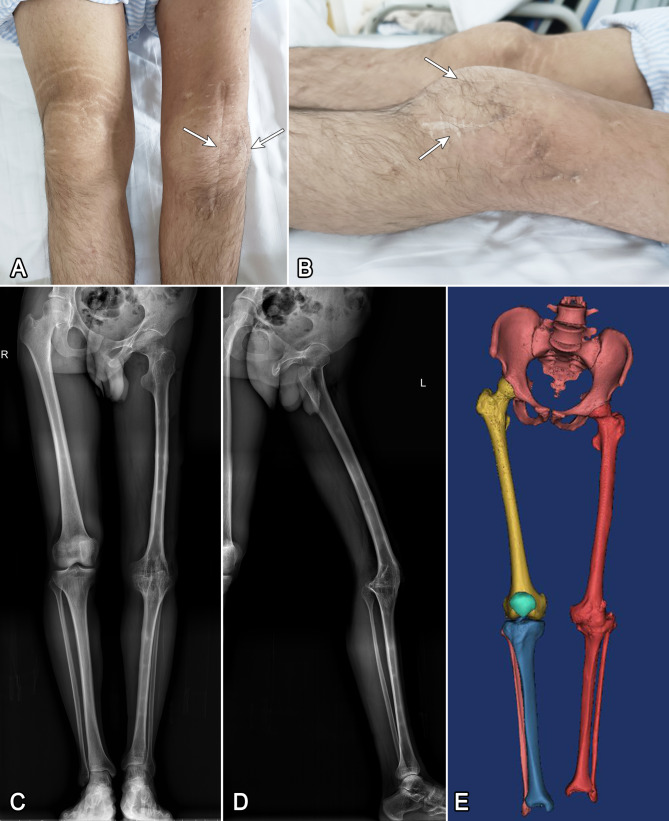
The left lower limb was significantly shorter than that of the opposite side, with scoliosis; the left quadriceps femoris was obviously atrophic, with muscle strength of grade V (MRC scale); two old surgical scars with longitudinal length of about 15 cm and 7 cm could be seen at the left knee joint; the patella could not be touched; the left knee joint had no degree of motion before operation, and it was about 5° fusion with knee flexion (Fig. 1). The patient could walk up and down stairs after compensation (Video 1).
Fig. 1.
A and B are the front and side views of the old surgical scar respectively; C and D are the full-length anteroposterior and lateral radiographs of the lower limb before operation; E shows the preoperative 3D reconstruction image, showing the shortening of the left lower limb and the absence of patella
Preoperative plan
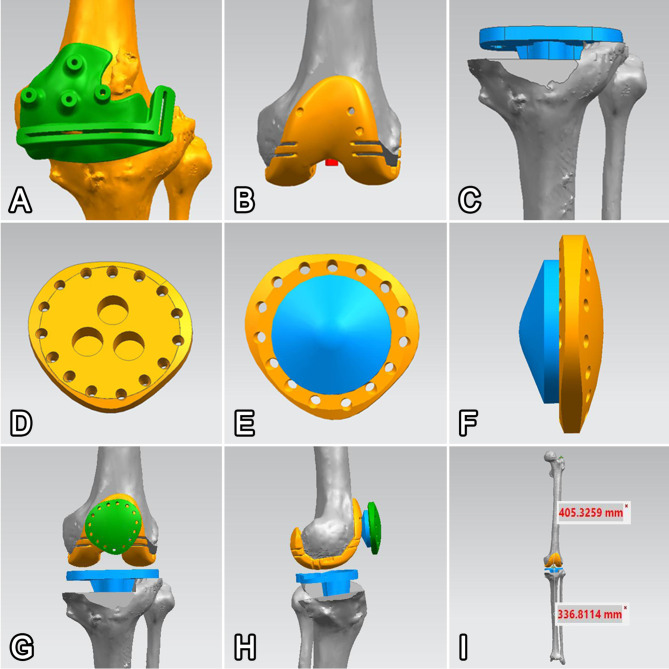
Three-dimensional (3D) reconstruction was performed by using the patient’s preoperative computed tomography (CT) data (1 mm slice thickness scan at the knee joint and 3 mm slice thickness scan at other parts to reduce the radiation) through the Mimics Research software (Version 19.0, Materials Inc., Belgium). With the help of CATIA (Version 5.20, Dassault Systèmes Inc., France) and Siemens NX (Version 12.0, Siemens PLM Software Inc., Germany), the patients were provided with personalized 3D preoperative planning [8, 9], customized personalized osteotomy guide plate and 3D-printed porous tantalum patella [10] (Fig. 2).
Fig. 2.
A shows personalized osteotomy guide plate; B shows the simulated femoral prosthesis; C shows the simulated assembled tibial prosthesis; D shows customized tantalum patellar base; E and F show tantalum patellar base with conventional polyethylene components; G and H are the general schematic diagram of knee joint after conversion; I shows the overall view of the lower limb after conversion
Customized osteotomy guide plate
Since the joint line of the patient moved down and was not easy to distinguish, it was relatively difficult to determine the height of the osteotomy plane. We found the relatively accurate mechanical axis of the femur by mirroring the opposite femur, determined the vertical osteotomy plane of the distal femur according to the mechanical axis, and adjusted the final position of the osteotomy plane according to the relatively fuzzy fusion surface, which called plane A; found the relatively accurate mechanical axis of the tibia through the mirror image of the opposite tibia, determined the vertical osteotomy plane of the proximal tibia according to the mechanical axis, and adjusted the final position of the osteotomy plane according to the relatively fuzzy fusion surface, which called plane B; we were surprised to find that plane A and plane B were almost identical, which will be collectively referred to as plane C. According to the osteotomy plane C and the bony sign at the front of the fusion knee, the corresponding osteotomy guide plate was designed and printed; calculated the depth of osteotomy on the plane C to reduce the risk of vascular and nerve injury.
Customized 3D-printed porous tantalum patella
We referred to the thinnest patellar polyethylene prosthesis to fabricate 3D-printed porous tantalum patella. Porous pure tantalum structure design was adopted, with wire diameter 0.35 mm and pore size ranging 450–500 μm. The porosity was 85%. The polyethylene surface and back were designed as trabecular structure to facilitate the fixation of polyethylene components with bone cement and the growth of soft tissue. Biomechanics was used to measure the tension and compressive stress it could bear, and the thickness of the thickest part in the center was determined as 8 mm. Fifteen round holes were designed around the base of the tantalum patella for suture, with an aperture of 2.8 mm. Using 3D printing technology to print the designed tantalum patellar base according to the original scale and the reduced scale of 3%.
Intraoperative condition
Preparation and exposure
The patient received combined spinal and epidural anesthesia. The tourniquet was placed at the root of his left thigh and the pressure was set at 300 mmHg.
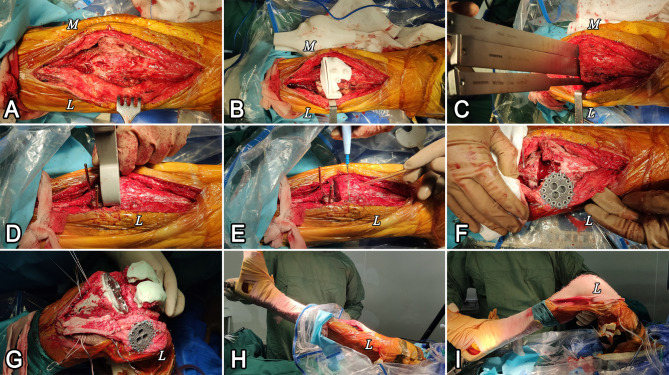
The knee was cut anteriorly along the original median length of 15 cm layer by layer to the joint. Then, a tibial tuberosity osteotomy of approximately 7 cm in length was performed (Fig. 3A).
Fig. 3.
A shows the tibial tubercle after osteotomy; B shows the installation of osteotomy guide plate; C shows osteotomy using osteotome; D shows the measurement of the extension gap with the spacer block; E shows the determination of distal femoral osteotomy line; F shows fixed tantalum patellar base; G shows prosthesis installation; H shows that the knee joint is completely straightened after operation; I shows knee flexion after operation
Osteotomy using the guide plate
Referring to the printed knee joint model, the osteotomy guide plate was fixed at the predetermined position during operation, and then a graduated osteotome was applied to drive along the osteotomy gap to the predetermined depth, and carefully cut off the posterior cortex of the knee joint to avoid damaging the posterior blood vessels and nerves (Fig. 3B-C). An intramedullary locator was used to determine the plane of the proximal tibial osteotomy in the knee flexion position to complete the tibial osteotomy.
Gap balance method
The testing of the flexion-extension gap after the tibial osteotomy revealed that the extension gap was almost non-existent and the flexion gap was also small. Based on this result, a further tibial osteotomy was performed and the posterior joint capsule was released. Then, the gap-balance method [11] was used to perform distal femoral osteotomy until the extension gap was satisfied (Fig. 3D-E). The size of the femur was measured, and the osteotomy of femoral posterior condylar was also completed by gap-balance method [11]. At this time, the flexion and extension gaps were balanced. After completing the above steps, the prosthesis test mold was installed. Tests showed that the flexion and extension activities were satisfactory.
Test of the patellar prosthesis
The tantalum patellar base and patellar polyethylene test mold were placed at the horizontal position of the joint line of the knee extensor mechanism, and the patellar tracking was tested. The tantalum patellar base was firmly sutured with two ultra-strong wires (Fig. 3F).
Prosthesis installation and tubercle fixation
Because of the long duration of knee fusion and the incapability of testing the strength of the lateral collateral ligament, a short rod semi-restrictive prosthesis (NexGen LCCK, Zimmer Biomet, USA) was used. After washing, the prosthesis was fixed with bone cement, and the polyethylene component of patella was fixed on the tantalum patellar base (Fig. 3G). The pad was placed, and the knee extension position was maintained until the bone cement was completely solidified. Three embedded steel wires were used to bind and fix the tibial tubercle (Fig. 3G). The ROM of the knee joint tested was 0° to 90° (Fig. 3H-I).
Intraoperative bleeding and operation time
The total operation time was 210 min, the first tourniquet time was 109 min, and the second tourniquet time was 63 min.
Postoperative condition
The full-length radiographs of the lower limb showed that the alignment of the lower limb and the alignment of the prosthesis were good (Fig. 4). At one week after operation, the wound healed, and the patient began to bend and stretch without weight-bearing and walk with partial weight-bearing when getting out of bed. At 6 weeks after operation, the ROM was about 0° to 90°. The patient could walk on the flat ground with full weight-bearing when wearing brace, but there was a lag in knee extension (Video 2). At 3 months after operation, the knee extension lag disappeared, and the patient could walk on the flat ground and go up and down stairs (Video 3). At the same time, the patient was finally able to complete one daily meditation that needs to bend both knee joints and sit cross-legged after the fusion procedure. At 4 months after operation, the ROM was about 0° to 100°, and the patient could squat and stand up, walk on the flat ground, and go up and down stairs (Video 4). The knee movement function was significantly improved compared with those before the operation (Video 5). In addition, the patient was evaluated by knee function scores, including the Hospital for Special Surgery scores (HSS), the Knee Society Score (KSS), the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), the Knee injury and Osteoarthritis Outcome Score (KOOS) and the36-item Short-Form for Health Survey Questionnaire (SF-36), 2 days preoperatively and 1 year postoperatively, and the results of comparing the scores between the two periods showed a significant improvement in the patient’s knee function, which the patient was very satisfied with (Table 2). The postoperative infection-related test results of the patient are shown in Table 1. It should be noted that the patient’s C-reactive protein and erythrocyte sedimentation rate indexes increased from the seventh postoperative day, due to excessive postoperative rehabilitation exercise. After the subsequent reduction of activity, both indicators fell to the normal range. Throughout the whole period, the patient’s incision was free of obvious redness, swelling, pain and temperature increase.
Fig. 4.
A, B shows the full-length anteroposterior/lateral radiograph of lower limb 2 days after operation, respectively; C, D shows the full-length anteroposterior/lateral radiograph of lower limb one year after operation, respectively
Table 2.
Comparison of patient reported outcome measures
| Pre-operation (2 Days) | Post-operation (1 Year) | |
|---|---|---|
| HSS | 72 | 94 |
| KSS Knee | 75 | 90 |
| Function | 90 | 90 |
| WOMAC Pain | 100 | 95 |
| Stiffness | 56 | 94 |
| Function | 76 | 93 |
| KOOS Pain | 100 | 97 |
| Symptoms | 43 | 96 |
| ADL | 79 | 96 |
| Sport/Rec | 50 | 80 |
| QOL | 44 | 88 |
| SF-36 Physical Functioning | 55 | 85 |
| Role-Physical | 50 | 100 |
| Bodily Pain | 74 | 84 |
| General Health | 62 | 77 |
| Vitality | 30 | 45 |
| Social Functioning | 75 | 100 |
| Role-Emotional | 100 | 100 |
| Mental Health | 76 | 76 |
| Reported Health Transition | 50 | 100 |
HSS: Hospital for Special Surgery scores; KSS: Knee Society Score; WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index; KOOS: Knee injury and Osteoarthritis Outcome Score; SF-36: 36-item Short-Form for Health Survey Questionnaire. Higher scores indicate better performance. WOMAC scores were standardized as a range from 0 (worst) to 100 (best) according to current guidance [21]
Discussion
Adequate preoperative communication and good expectation management are the solid foundation for optimistic prognosis. In this case, the patient was a Tibetan Buddhist monk who often needs to meditate during his daily practice, which required bending his knees and sitting cross-legged. Objectively speaking, his previous knee fusion was painless and strong, but the patient’s expectation of sitting cross-legged due to the need of belief was extremely high. After fully communicating with the patient and his relatives about the possible complications of the operation and the long and arduous postoperative recovery process, we believed that the patient’s subjective demands and religious beliefs should be respected and his dream of meditation should be realized while ensuring that the operation was relatively safe and controllable.
Perfect preoperative planning and its reliable implementation during surgery are essential. Preoperatively, the design of a 3D printed porous tantalum patella base needs to be completed and simulated osteotomies need to be performed using personalized 3D preoperative models [8, 9]. Intraoperatively, personalized 3D printed osteotomy tools are required as a guarantee of accurate osteotomy planning [10]. In addition to the above factors, the following issues are also the key to ensure the effectiveness of the procedure.
The first is the exposure of joints. The tibial tubercle osteotomy was performed to ensure good exposure. It is reported that 45–100% of the conversions require tibial tubercle osteotomy [12].
The second is the choice of prosthesis. Even though the lateral collateral ligament is stable under anesthesia during operation, its future stability is still unpredictable due to long-term knee fusion. So if the ligament is stable during operation, semi-restrictive implants can be used [4]. However, the collateral ligament was often damaged in the previous fusion, with a proportion of 43–48%. In this case, it is necessary to prepare a completely restrictive prosthesis [12–14]. In this case, we used the gap-balanced method for osteotomy, and the ligaments were complete, so the semi-restrictive prosthesis was selected. But we prepared the fully restrictive prosthesis before the operation to prevent any accidents.
The third is the absence of patella. Extensor mechanism is an important factor affecting the postoperative effect [4]. Previous studies have shown that about 17% of patients have patellar loss after fusion [13–15]. In this case, the patient’s patella was completely absent. In order to reconstruct a high-quality knee extensor mechanism, we used our unique porous pure tantalum 3D printing technology to customize the patellar base, and combined with conventional patellar polyethylene components to replace the absent patella. With its unique physical and chemical properties, excellent biological inertness and biocompatibility, tantalum metal has become a new biological material after titanium metal [16, 17]. A large number of literatures have confirmed that pure tantalum as a human implant has not had adverse reactions [17, 18]. The patient was followed one year after operation, and the imaging position of tantalum metal did not change. We did not use the patellar base products from Zimmer, such as its Trabecular Metal Augmentation Patella, in order to design smaller and thinner patellar prosthesis as far as possible to reduce the tension of the incision and improve the success rate of implantation.
The fourth is the consideration of the tolerance of knee joint soft tissue. The patient needs to implant customized patella, which would increase the tension of soft tissue in front of the knee, and rehabilitation exercise is required after operation, resulting in increased possibility of difficult incision closure and poor healing [13]. To this end, on the premise of ensuring sufficient strength, we reduced the thickness and size of customized patella before operation. During the operation, the joint capsule was tightly sutured with techniques such as tension reduction and dislocation to reduce leakage, and the tourniquet was loosened to check the blood supply of the local skin and ensure that the skin was ruddy after the subcutaneous and skin sutures were completed. The blood was stopped by local and intravenous application of tranexamic acid and appropriate pressure bandage. Intravenous application of mannitol and dexamethasone reduced local edema and skin tension. Flexion of the knee joint was avoided within 1 week after operation. Fortunately, the patient did not have any wound healing problems.
The fifth is the postoperative rehabilitation. It is easy to have dysfunction after conversion. The patient’s will of exercise would even determine the functional results after operation. As a devout monk, the patient has a strong desire to achieve high knee flexion. The patient works very hard after operation, and has achieved good functional results. Literature reported that only 61% of the patients’ knees were completely painless after conversion [15]. In this study, the patient had no obvious pain after 6 months of operation, which might be closely related to his early active recovery and young age without any underlying diseases. Knee extension lag is also commonly reported, ranging from 0° to 40° [5, 6, 12, 15]. Six weeks after operation, the patient had knee extension lag at about 15°, but the symptoms disappeared after one month of exercise. Other complications such as ligament relaxation, prosthesis loosening, polyethylene abrasion, infection, contracture or rupture of knee extensor mechanism, ossifying myositis or peroneal nerve paralysis were not found in this patient within one year after operation.
Previous literature shows that the revision rate of this conversion can be as high as 62% [6, 13], and some patients (11-28.5%) must undergo a second knee arthrodesis [4, 11, 14], such as the reactivation of chronic knee instability or sepsis. However, it is surprising that despite the high incidence of complications and revision, most patients are very satisfied with their movable knee joint [13, 15]. Different from the biconvex polyethylene prosthesis, the tantalum patella prosthesis does not require a cortical margin of the patella to support the implanted prosthesis [19]. Nasser et al. [20] studied 11 patients who underwent tantalum patellar arthroplasty for patellar loss, all of whom underwent TKA revision, and found that the knee function and pain scores improved by an average of 45 and 33 respectively (KSS), and the ROM improved by an average of 41 degrees. Unlike this case, which was accompanied by a 5-year left knee arthrodesis, most of their patients did not have knee stiffness. Only one 69-year-old female patient of theirs had a preoperative ROM of 10 degrees [20], close to that of the present case, and her postoperative ROM improved by 80 degrees. In this case, the patient was very satisfied with the operation, as his ROM in the left knee improved from 0 degrees to 100 degrees, which fulfilled his “meditation dream”.
The full-length radiographs of the lower limb in this case showed that the limb shortening was still 6 cm, and the patient’s claudication was still obvious. This is because the bone development of the patient’s left knee joint is not mature, the overall length of the left lower limb is not well developed, and TKA cannot significantly extend the limb. In view of this, we have fully communicated with the patient before operation. The patient said that he was used to shortening and temporarily refused to do limb lengthening. If there is a need to extend limbs in future life, we will do further clinical work and report.
There are still some limitations. First, the follow-up period is relatively short, and the long-term outcome of the operation is not yet clear. The case will be followed up to clarify the long-term outcome. Second, the shortening of the patient’s left lower limb was not resolved due to his refusal to undergo another surgery. However, this did not seriously affect the patient’s daily needs.
Conclusion
Adequate preoperative communication with patients and good expectation management are crucial for ensuring favorable prognoses. Perfect preoperative planning and its reliable implementation during operation are essential. Additionally, postoperative rehabilitation and proactive management of complications play pivotal roles in achieving optimal clinical outcomes.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We acknowledge the support received the National Key R&D Program of China (No.2021YFC2401304).
Abbreviations
- TKA
Total Knee Arthroplasty
- 3D
Three-Dimensional
- CT
Computed Tomography
- HSS
Hospital for Special Surgery scores
- KSS
Knee Society Score
- WOMAC
Western Ontario and McMaster Universities Osteoarthritis Index
- KOOS
Knee injury and Osteoarthritis Outcome Score
- SF-36
36-item Short-Form for Health Survey Questionnaire
Author contributions
LLM and KL composed the manuscript, LLM completed revisions of the manuscript, KL completed the data collection, LG and PFY conceived the idea of the study; All authors contributed to the writing of the manuscript and approved the final manuscript.
Funding
This study was funded by National Key R&D Program of China (No.2021YFC2401304). There was no financial conflict of interest with regards to this study.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from all the participants prior to the enrollment or for the publication of this study.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Li-Ming Liu and Kai Lei contributed equally and should be regarded as co-first authors.
Contributor Information
Peng-Fei Yang, Email: ks330301668@126.com.
Lin Guo, Email: guolin6212@163.com.
References
- 1.Kernkamp WA, Verra WC, Pijls BG, Schoones JW, van der Linden HMJ, Nelissen RGHH. Conversion from knee arthrodesis to arthroplasty: systematic review. Int Orthop. 2016;40(10):2069–74. [DOI] [PubMed] [Google Scholar]
- 2.Kim YH, Kim JS, Cho SH. Total knee arthroplasty after spontaneous osseous ankylosis and takedown of formal knee fusion. J Arthroplasty. 2000;15(4):453–60. [DOI] [PubMed] [Google Scholar]
- 3.Anatone AJ, Uppstrom TJ, Fletcher C, Baral E, Gomoll AH, Strickland SM. Patellofemoral arthroplasty conversion to total knee arthroplasty: an updated retrieval analysis and clinical outcomes. Knee. 2023;43:28–33. [DOI] [PubMed] [Google Scholar]
- 4.Cermak K, Baillon B, Tsepelidis D, Vancabeke M. Total knee arthroplasty after former knee fusion in a patient with Ehlers Danlos syndrome. Acta Orthop Belg. 2013;79(3):347–50. [PubMed] [Google Scholar]
- 5.Cho SH, Jeong ST, Park HB, Hwang SC, Kim DH. Two-stage conversion of fused knee to total knee arthroplasty. J Arthroplasty. 2008;23(3):476–9. [DOI] [PubMed] [Google Scholar]
- 6.Clemens D, Lereim P, Holm I, Reikerås O. Conversion of knee fusion to total arthroplasty: complications in 8 patients. Acta Orthop. 2005;76(3):370–4. [PubMed] [Google Scholar]
- 7.Denyer S, Hoyt AK, Schneider AM, Brown NM. Knee arthrodesis: an analysis of Surgical Risk factors and complications using a National Database. Arthroplast Today. 2023;20:101098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lei K, Liu L, Yang P, Xiong R, Yang L, He R, Guo L. Robotics versus personalized 3D preoperative planning in total knee arthroplasty: a propensity score-matched analysis. J Orthop Surg Res. 2022;17(1):227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lei K, Liu LM, Xiang Y, Chen X, Fan HQ, Peng Y, Luo JM, Guo L. Clinical value of CT-based patient-specific 3D preoperative design combined with conventional instruments in primary total knee arthroplasty: a propensity score-matched analysis. J Orthop Surg Res. 2020;15(1):591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sun M-L, Zhang Y, Peng Y, Fu D-J, Fan H-Q, He R. Accuracy of a novel 3D-Printed patient-specific Intramedullary Guide to Control Femoral Component Rotation in total knee arthroplasty. Orthop Surg. 2020;12(2):429–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sheth NP, Husain A, Nelson CL. Surgical techniques for total knee arthroplasty: measured resection, gap balancing, and hybrid. J Am Acad Orthop Surg. 2017;25(7):499–508. [DOI] [PubMed] [Google Scholar]
- 12.Holden DL, Jackson DW. Considerations in total knee arthroplasty following previous knee fusion. Clin Orthop Relat Res. 1988;227:223–8. [PubMed] [Google Scholar]
- 13.Cameron HU, Park YS. Total knee replacement following high tibial osteotomy and unicompartmental knee. Orthopedics. 1996;19(9):807–8. [DOI] [PubMed] [Google Scholar]
- 14.Henkel TR, Boldt JG, Drobny TK, Munzinger UK. Total knee arthroplasty after formal knee fusion using unconstrained and semiconstrained components: a report of 7 cases. J Arthroplasty. 2001;16(6):768–76. [DOI] [PubMed] [Google Scholar]
- 15.Kim Y-H, Oh SH, Kim JS. Conversion of a fused knee with use of a posterior stabilized total knee prosthesis. J bone Joint Surg Am Volume. 2003;85(6):1047–50. [DOI] [PubMed] [Google Scholar]
- 16.Zhang C, Lin Y, Yang L, Duan X. 3D Printing-assisted Supramalleolar Osteotomy for Ankle Osteoarthritis. ACS Omega. 2022;7(46):42191–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ao Y, Guo L, Chen H, He R, Yang P, Fu D, Gu L, Peng Y, Xiong R, Yang L, et al. Application of three-dimensional-printed porous tantalum cones in total knee arthroplasty revision to reconstruct bone defects. Front Bioeng Biotechnol. 2022;10:925339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Martino I, Mancino F, Di Matteo V, Singlitico A, Maccauro G, Gasparini G. Tantalum cones for severe bone defects in revision knee arthroplasty: a minimum 10-Year Follow-Up. J Arthroplasty. 2023;38(5):886–92. [DOI] [PubMed] [Google Scholar]
- 19.Garcia RM, Kraay MJ, Conroy-Smith PA, Goldberg VM. Management of the deficient patella in revision total knee arthroplasty. Clin Orthop Relat Res. 2008;466(11):2790–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nasser S, Poggie RA. Revision and salvage patellar arthroplasty using a porous tantalum implant. J Arthroplasty. 2004;19(5):562–72. [DOI] [PubMed] [Google Scholar]
- 21.Singh J, Sloan JA, Johanson NA. Challenges with health-related quality of life assessment in arthroplasty patients: problems and solutions. J Am Acad Orthop Surg. 2010;18(2):72–82. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.