Abstract
Background
The COVID-19 pandemic has served as a catalyst for recognizing the challenging environments in which healthcare workers operate, underscoring the urgent need to enhance their wellness to better support themselves and others. The implementation of a culture of wellness within the context of healthcare education, with a particular emphasis on individual-level strategies, allows for the realization of its intrinsic value and significance as a foundation for broader organizational strategies. This approach facilitates the establishment of a sustainable culture of wellness that benefits both current and subsequent generations of healthcare professionals.
Methods
We implemented our wellness program using a pragmatic pre-post study design for different settings. Our wellness intervention program was tested in three ways by creating combinations of different intensities (high, moderate, or low), delivery methods (face-to-face vs. virtual), different motivations (incentive, mandatory, or volunteer participation), and different timings (during medical programs or before entering into healthcare programs) among medical and nursing students. The effects of the wellness program were measured on quality of life, emotional intelligence, and efficacy scores among healthcare students. Statistical methods included repeated measures analysis of variance and paired t-tests.
Results
A total of 224 students (13 in high, 145 in moderate, and 66 in low-dose interventions) participated in our study program. Most scores were significantly improved except for a few factors in the high-dose face-to-face Well-Teach intervention cohort. Among quality of life components, the average psychological scores were markedly increased after high (13.2 vs. 14.7, p = .018), moderate (13.9 vs. 14.8, p < .001), and low (12.8 vs. 13.4, p < .001) intensity intervention cohorts. The moderate and low intensity of wellness intervention cohorts had the highest impact on the total emotional intelligence scores (mean difference = 3.021, 95%CI:0.553–5.488, p = .008) and (mean difference = 5.197, 95%CI:3.057–7.337, p = < 0.001), respectively. The low-dose healthcare intervention program yielded improvements in all components of all scores to a greater extent than moderate-dose or high-dose with face-to-face intervention programs.
Conclusions
This study demonstrates that our multifaceted Well-Teach model can be used to improve the quality of life, emotional intelligence, and self-efficacy of healthcare students. Low- or moderate-intensity intervention programs integrated into the curriculum may be more practical in health sciences education to sustain and promote lifelong wellness practices as solid steps toward attaining a “culture of wellness”. Our model should be considered to be beneficial, sustainable, cost-effective, comprehensive, and effective for current and future generations of healthcare providers.
Keywords: Wellness programs, Healthcare education, Burnout prevention, Indivisible Self model, Healthcare education curriculum, Wellness culture
Background
The COVID-19 pandemic exacerbated the already existing burnout, stress, and anxiety epidemic among healthcare workers [1–4]. These professionals operate in emotionally demanding environments, which significantly impact their well-being, emphasizing the crucial need for dedicated support and care to maintain their overall wellness.
The importance of wellness in healthcare education
From their formative years, health professions students face a competitive environment facing higher risks of insecurity, depression, alcohol abuse, anxiety, and suicide compared to the general population [5]. Burnout is the most prevalent of the psychosocial problems faced by healthcare professionals. It is a three-dimensional construct resulting from chronic stress [6–11]. Burnout is common among students in health professions like medicine, nursing and dental and dental hygiene [12–15] and remains prevalent among pharmacists, medical residents, nurses, and physicians [16–19]. About 50% of medical students experience burnout before residency [20]. Although burnout isn’t a mental illness, 90% of people with burnout test positive for depression [21]. Burnout affects professional performance and quality of care, and is associated with absenteeism and disability [22, 23]. Given the close relationship between burnout and depression, it is therefore not surprising that physicians with a positive diagnosis of depression also have a higher rate of medical error and deteriorated personal health [24]. Although the deficiency in wellness among healthcare professionals is recognized as a potential contributor to their health issues, the academic field currently lacks evidence-based defined pathways, assessment methodologies, and empirical data to substantiate the benefits of achieving wellness.
Different attempts to educate healthcare providers on the concept of wellness have been developed using a variety of activities, policies, and approaches [25–29]. A substantial portion of these strategies focused on elucidating the reasoning behind the vital role of wellness for healthcare professionals. Despite the failure of numerous attempts to provide conclusive or comprehensive results, the analysis of implementation strategies alongside our experiences led us to identify the root cause, which we have defined as a lack of a solid wellness culture among students and professionals at all levels, as well as the corresponding integration and support of their organizations.
The importance and relevance of fostering a culture of wellness
Establishing a culture of wellness in healthcare institutions supports employee well-being, improves patient outcomes, enhances quality of care, and contributes to the sustainability of the healthcare system requires an individualized and institutional approach [30]. This multifaceted approach is best when influenced by internal factors such as individual member characteristics, beliefs, and behaviors, as well as external elements including the environment, social structures, cultural norms, policies, and regulations [31]. The unwavering dedication, support, active involvement, and leadership displayed by individuals at all tiers of healthcare establishments are key to ensuring the longevity, flexibility, and progression of such programs [32]. This commitment of healthcare providers is evidenced through the assistance and endorsement provided for example by the National Academy of Medicine Action Collaborative on Clinician Well-Being and Resilience. This support encompasses the integration of mentoring programs, leadership development, training, and collaborative initiatives [33].
Challenges in developing a culture of wellness
The importance and visibility of wellness programs in the healthcare sector are clearly apparent. However, this acknowledgment alone does not guarantee the necessary backing and sustainability. To achieve enduring support, a pivotal shift is essential, transitioning the focus from the “why” of wellness importance to the “how” of its implementation, evaluation, and recognition.
Recognizing the importance of a wellness culture is a critical first step for any organization. Establishing and valuing a wellness-centered culture can be difficult, especially when the current leadership lacks familiarity with the necessary methods to nurture, embrace, and champion such a culture. This critical aspect was absent from their training or professional background, potentially setting the stage for the continuation of this pattern among upcoming students. Additionally, a discrepancy is evident in the alignment of individual and system-level interventions and the resources allocated. Furthermore, inconsistencies have been identified concerning wellness programs, the challenges in evaluating subjective outcomes, standardization, the integration of academic performance measures, and the issue of stigmatization [34].
At the individual level among healthcare students, support and engagement are typically constrained by two primary factors: time limitations required to balance academic demands with involvement in wellness initiatives, and the lack of a generalizable value associated with wellness concepts. Consequently, it is challenging to obtain evidence-based information from studies that employ non-randomized control designs or longitudinal methodologies, obtain larger sample sizes, or generalize findings across multiple studies. Moreover, students demonstrate diverse preferences, levels of knowledge, and resistance to wellness programs, resulting in challenges related to engagement, participation, and program delivery. The potential for selection bias exists, prompting questions about whether voluntary workshop participants have greater needs than non-attendees. Additionally, safety and ethical considerations need to be considered in regard to all aspects of program preparation encompassing both individual and organizational levels.
Promoting sustainable wellness practices among healthcare students
Holistic approaches to wellness deserve consideration in alignment with the shift towards exploring the implementation of wellness. A holistic approach to wellness refers to a comprehensive and integrated method that considers various aspects of an individual’s well-being. Overpasses both the concepts of health and wellness that might be hindering the efforts to develop strategies for effective solutions [35]. Health cannot be compartmentalized or isolated but instead needs to be conceived with a holistic approach into a model composed of elements of physical, behavioral, psychological, social and spiritual well-being [36]. Considering this approach allows to understand health achievable even by those that suffer illnesses, chronic diseases, or disabilities [37–39].
Wellness initiatives and programs are referenced in various sectors of health education with the rationale that they are implemented based on the understanding that self-care is a critical aspect of effectively navigating the challenges associated with academic and professional pursuits.
Certain wellness programs in educational settings which adopt a holistic approach, encompass mind-body techniques, stress management, self-care, and mindfulness practices for medical students [40]. Programs also involve mindfulness-based interventions for preclinical medical students [41] and utilize Compassion Cultivation Training to enhance medical student wellness and improve clinical care [42]. Furthermore, there are shortened mindfulness interventions designed to improve wellness in first-year medical students [43], programs that concentrate on exercise interventions to enhance health and well-being among medical students [44], and interventions that specifically target fitness to boost exercise levels and well-being in medical students [45]. Several programs suggest curriculum changes while promoting a holistic strategy. For instance, they aim to develop a culture of wellness among medical students and faculty to address burnout in the medical profession [46]. One well-known program is the Vanderbilt Medical Student (VMS) Wellness Program [47]. The program features a structured wellness curriculum with three primary domains: the Faculty Advisory College System, the Student Wellness Committee, and the VMS Live curriculum. These components integrate student, faculty, and curriculum modifications to establish a holistic approach to wellness. The curriculum modifications detailed in the research highlight the effectiveness of integrating student input, allowing students to actively guide and contribute to the development of their wellness curriculum. These changes also involve organizational adjustments aimed at fostering a supportive learning environment with increased flexibility to accommodate individual needs while maintaining educational standards [48–50].
These strategies all highlighted comparable challenges at both individual and organizational levels as mentioned previously. To instigate organizational transformations that foster a wellness culture in healthcare education, focusing on individual-level interventions is essential as the initial step. Hence, interventions should span the healthcare spectrum, commencing with students who represent the upcoming healthcare workforce. Integrating this strategy aims to develop sustainable, cost-effective, comprehensive and effective programs that promote, sustain and advance wellness [28, 51–53]. Emphasizing wellness can empower healthcare individuals to take a proactive approach in advocating for organizational changes or working towards improvements within the workplace. Those who prioritize their well-being tend to possess enhanced self-awareness, resilience, and motivation to address issues affecting health and well-being. This proactive approach has the potential to drive initiatives that improve workplace culture, bolster mental health support, enhance work-life balance, and establish a positive and enduring work environment for all. Prioritizing individual changes before implementing broader organizational strategies is crucial for fostering a lasting culture of wellness in healthcare education [54–58]. Furthermore, organizational changes to promote wellness will necessitate a transformation in the existing culture to acknowledge that wellness is not merely a nice-to-have skill, but a crucial asset. The transition involves recognizing that the journey towards holistic wellness in healthcare students is continuous and should ideally begin early, potentially through adjustments in the curriculum. This process also necessitates ongoing support and adaptations to prepare students for anticipated and unforeseen challenges in the future. Lastly in approaching wellness as a holistic model, a comprehensive approach is essential, so any wellness effort that focuses on one or a few activities (e.g., installing a gym, teaching mindfulness, or hosting conferences on wellness philosophy) does not necessary constitute a holistic wellness program.
Reflecting on these foundational principles and advancing from our previous models, we unveiled a holistic wellness initiative known as “Well-Teach” Teaching Wellness. The program, supported by cognitive and emotional competencies, was evaluated at the individual level, using diverse modes, doses, and settings of intervention with the objective of enhancing the quality of life and emotional intelligence of healthcare students.
Materials and methods
Study design and population
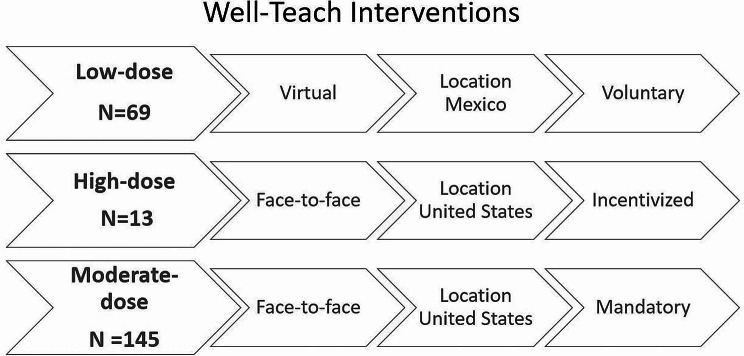
To test our wellness program, we adopted a pragmatic pre-post study design for different settings, due to differences in the methods of implementation of our program. The program was tested in three ways by creating combinations of different lengths (intensive, moderate, or short), delivery methods (face-to-face vs. virtual), different motivations (incentive, mandatory, or volunteer participation), and different timings (during medical programs or before entering into programs) among medical and nursing students. Figure 1 provides a detailed account of the different interventions, including the specific locations where they were conducted. We sought Institutional Review Board (IRB) approval from Texas Tech University Health Sciences Center El Paso prior to initiating our study. The IRB approved our study for assessing the intervention using an incentive method, while other assessments were exempt from IRB approval as they did not meet the criteria for human subject research, per 46.102(e)(1)(ii), as the information was not identifiable.
Fig. 1.
Well-Teach Interventions
Well-teach wellness intervention program
Our model is founded on two well-established theories in the field, one focusing on wellness [59] and the other on emotional intelligence [60], highlighting the importance of recognizing the interconnected nature of cognitive and emotional aspects. The program operationalizes theoretical frameworks via practical applications and tailored interventions employing an integrated instructional methodology encompassing lectures, multimedia resources, case studies for critical analysis, and interactive hands-on activities. Furthermore, it integrates practical elements such as meditation techniques, breathing exercises, and additional practices [61–63]. The wellness intervention program was overseen and conducted exclusively by the two principal investigators involved in the study, with the objective of maintaining consistency in the curriculum for the purposes of impact assessment. We believe the concepts proposed by these theories are closely related and can be synergistic. Wellness theory is anchored in the Indivisible Self model that reflects a single holistic factor (“Wellness”) to which five second order factors contribute: Essential Self, the Creative Self, the Social Self, the Physical Self, and the Coping Self. Supported by research, the Indivisible-Self model has demonstrated the multiple and interrelated dimensions of wellness and is probably the most researched and well-known wellness model in the counseling profession [64]. Its structure proved ideal to be transformed into systematic presentations that would interrelate and connect with each other to build the resources healthcare students require to empower themselves, engage in a meaningful life process, and ensure their wellness is sustained over time. In the Fig. 2, we show the components of our model called Teaching Wellness “Well-Teach”.
Fig. 2.
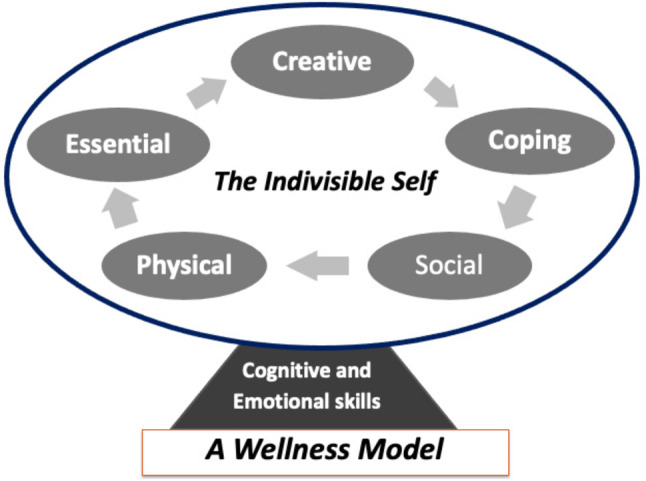
Teaching Wellness “Well-Teach” Model
Modes, doses and motivation of well-teach wellness intervention
We tested Well-Tech intervention into three modes with different strengths and timings: Low-dose virtual intervention with voluntary participation during an immersion week before classes in Mexico. High-dose face-to-face intervention for first- or second-year students with incentives in the USA. Moderate-dose face-to-face intervention requiring mandatory participation during an immersion week before classes in the USA.
Low-dose virtual intervention (voluntary, location Mexico)
In this mode, the intervention was delivered in 1 virtual session. The session lasted for 2 h. The quality of life, emotional intelligence, and self-efficacy were assessed before and at the end of the workshop session. Medical and nursing students had the option to voluntarily participate in the wellness workshop during immersion week prior to starting classes.
High dose face-to-face well-teach intervention (incentivized, location United States (USA)
In this mode, the intervention was delivered in 3 face-to-face sessions separated by one day. Sessions lasted for seven and a half hours. Workshops were conducted Friday (2 h and 30 min) and Saturday (5 h) which included a light breakfast and a lunch break. The participants perception of their quality of life, emotional intelligence, and self-efficacy were assessed before, at the end of workshops, and again a month later. Enrolled participants were emailed a link to complete a 1-month posttest survey. Those who attended the workshops and completed post-intervention surveys received $25.00, with an additional $40.00 provided upon completion of the final survey a month later.
Moderate-dose face-to-face intervention (mandatory, location USA)
In this mode, the intervention was delivered in 2 face-to-face sessions separated by one day. Each session lasted for 2 h (a total of 4 h). The quality of life, emotional intelligence, and self-efficacy were assessed before and at the end of the workshop sessions. Medical and nursing students were required to participate in the wellness workshop during immersion week prior to starting classes.
Variables and measurement
Quality of life
The quality of life was measured with the World Health Organization Quality of Life Instrument (WHOQOL) questionnaire based on a brief version of the WHOQOL- BREF. This instrument is composed of 26 items with response options that vary from 1 (very dissatisfied/very poor) to 5 (very satisfied/very good). The questionnaire includes four factors: physical health, psychological health, social relations, and environment [65].
Cognitive and emotional skills
These skills were evaluated using two emotional intelligence instruments. The first one was the trait emotional meta-mood scale (TMMS-24) [66] adapted by Fernández-Berrocal et al. This scale is based in the original version of the trait meta-mood scale [67]]. It has 24 items divided into three factors: emotional attention, emotional clarity, and emotional repair. Responses use a five-point Likert scale which ranged from 1 = strongly disagree to 5 = strongly agree. The second was the Wong and Law Emotional Intelligence Scale (WLEIS) [68] containing 16 items and four factors: Self Emotion Appraisals, Others’ Emotion Appraisals, Regulation of Emotion (ROE), and Use of Emotion (UOE). Each item in the WLEIS uses a 7-point Likert scale ranging from 1 (totally disagree) to 7 (totally agree).
Self-efficacy
The General Academic Self-Efficacy scale (GASE) [69] was used to measure academic self-efficacy in two of the sessions. The four items self-report scale measure academic self-efficacy on a five-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree).
Statistical analysis
All the scales were summarized with mean and standard deviation (SD). We applied a repeated measure analysis of variance (rANOVA) followed by Bonferroni’s posthoc multiple comparisons to evaluate the effect of high-dose face-to-face Well-Teach intervention on outcome measures. In the rANOVA, the assumption of sphericity was violated, as assessed by Mauchly’s test of sphericity therefore, a Greenhouse-Geisser correction was applied [70]. Paired t-tests were used to compare pre-to posttest surveys for evaluating the effects of Well-Teach interventions. The effect size was summarized with mean change along with 95%CI and percent relative improvements computed by pre-to-post scores divided by respective pre-test scores. Cohen effect sizes were used as small (d = 0.2), medium (d = 0.5), and large (d ≥ 0.8) [71]. A p-value less than 5% was considered a statistically significant result. Considering first of kin study, we did not adjust for multiplicity. All the statistical analyses were performed using IBM SPSS version 23.
Results
Effect of low-dose virtual well-teach intervention
The sample consisted of 44 medical students (63.8%) and 25 nurses (36.2%), with women representing 43 individuals (62.3%). The mean age was 21.46 (SD = 2.8), with a range of 20 to 29 years. All scores improved except for regulation scores. The largest improvement was noticed for quality of life in the psychological construct (mean difference = 3.021, 95%CI:0.553–5.488, p = .008), in the cognitive and emotional skills measured with the Emotional Intelligence scales in the total assessed by the TMMS-24 (mean difference = 5.197, 95%CI:3.057–7.337, p = < 0.001) and the mean difference for the WLEIS scale (Others’ Emotions Construct) is 0.432 (0.197–0.667) (Table 1).
Table 1.
Effect of low dose virtual well-teach intervention on quality of life emotional intelligence and self-efficacy scores (n = 69)
| Outcomes | T1 (pre) | T2(post) | Change (95% CI) | P value | Effect size |
|---|---|---|---|---|---|
| Quality of life measured with WHOQOL- BREF | |||||
| Physical | 14.36 ± 2.49 | 14.68 ± 2.41 | 0.312(0.057–0.681) | 0.048 | 0.208 |
| Psychological | 12.77 ± 2.99 | 13.41 ± 2.79 | 0.646(0.283–1.010) | < 0.001 | 0.437 |
| Social | 13.23 ± 3.75 | 13.66 ± 3.22 | 0.424(0.033–1.854) | 0.034 | 0.228 |
| Environmental | 14.11 ± 2.40 | 14.52 ± 2.56 | 0.411(0.101–0.721) | 0.005 | 0.326 |
| Emotional intelligence measured with TMMS24 | |||||
| Attention | 27.61 ± 7.47 | 29.80 ± 7.03 | 2.197(1.083–3.311) | < 0.001 | 0.485 |
| Clarity | 27.12 ± 7.09 | 28.67 ± 7.62 | 1.545(0.606–2.484) | < 0.001 | 0.405 |
| Repair | 27.59 ± 6.98 | 29.05 ± 6.99 | 1.455(0.354–2.555) | 0.005 | 0.325 |
| Total | 82.32 ± 18.13 | 87.52 ± 18.64 | 5.197(3.057–7.337) | < 0.001 | 0.597 |
| Emotional intelligence measured with WLEIS | |||||
| Self-emotions | 4.91 ± 1.41 | 5.26 ± 1.26 | 0.352(0.128–0.576) | 0.001 | 0.387 |
| Regulation | 5.46 ± 1.09 | 5.63 ± 1.13 | 0.167(0.044–0.377) | 0.059 | 0.195 |
| Use of Emotions | 5.11 ± 1.15 | 5.43 ± 1.11 | 0.318(0.135–0.501) | < 0.001 | 0.428 |
| Others’ Emotions | 4.55 ± 1.22 | 4.98 ± 1.25 | 0.432(0.197–0.667) | < 0.001 | 0.452 |
| Total | 5.01 ± 0.93 | 5.32 ± 0.99 | 0.317(0.173–0.462) | < 0.001 | 0.539 |
WHOQOL-BREF: Quality of life; TMMS24: Emotional intelligence; WLEIS: Emotional intelligence; GAZE: Self-efficacy; CI: confidence interval
Effect of high-dose face-to-face well-teach intervention
The sample consisted of 13 medical students, with women representing 9 individuals (69.2%). The mean age was 25.31 (SD = 2.0), with a range of 23 to 29 years. In the quality of life survey, physical scores showed a significant improvement at 1-month following the initial intervention (mean difference = 1.044, 95%CI:0.235–1.852, p = .011), psychological scores showed a significant improvement following immediate intervention (mean difference = 1.205, 95%CI:0.423–1.987, p = .003) as well as 1-month later (mean difference = 1.359, 95%CI:0.227–2.491, p = .018). In addition, a borderline improvement in environment scores at 1-month later was also observed (mean difference = 1.154, 95%CI:0.007–2.314, p = .05). A sustained improvement was observed for cognitive and emotional skills including the two emotional intelligence scales: TMMS-24 1-Month later (mean difference = 10.692, 95%CI:0.848–20.536, p = .032) primarily driven by clarity scores and WLEIS 1-Month later (mean difference = 0.519, 95%CI:0.112–0.927, p = .012) primarily driven by self-emotions at immediate post-intervention (mean difference = 0.481, 95%CI:0.100-0.862) and 1-month post-intervention (mean difference = 0.712, 95%CI:0.093–1.330). In the emotional intelligence scale, the improvement in mean total scores was observed at 1-month post-intervention only (93 vs. 104, p = .032). This was primarily driven by clarity scores (Table 2).
Table 2.
Effect of high-dose face-to-face well-teach intervention on quality of life, emotional intelligence, and self-efficacy scores (n = 13 students)
| Outcomes | T1 (baseline pre) |
T2 (immediate post) |
T3 (one month later post) |
T1 to T2 p-value |
T1 to T3 p-value |
Effect size at T2 | Effect size at T3 |
|---|---|---|---|---|---|---|---|
| Quality of life measured with WHOQOL- BREF | |||||||
| Physical | 15.91 ± 1.51 | 16.44 ± 1.75 | 16.96 ± 1.29 | 0.246 | 0.011 | 0.526 | 0.995 |
| Psychological | 13.23 ± 2.31 | 14.51 ± 2.58 | 14.67 ± 2.48 | 0.003 | 0.018 | 1.188 | 0.925 |
| Social | 14.87 ± 3.44 | 15.28 ± 4.13 | 16.72 ± 3.11 | 0.130 | 0.169 | 0.626 | 0.586 |
| Environmental | 15.46 ± 1.96 | 16.00 ± 2.40 | 16.62 ± 1.50 | 0.172 | 0.051 | 0.583 | 0.767 |
| Emotional intelligence measured with TMMS24 | |||||||
| Attention | 30.15 ± 6.50 | 32.33 ± 4.85 | 34.77 ± 2.95 | 0.255 | 0.121 | 0.521 | 0.637 |
| Clarity | 32.08 ± 5.38 | 33.77 ± 4.90 | 35.23 ± 3.52 | 0.584 | 0.037 | 0.381 | 0.815 |
| Repair | 31.00 ± 5.46 | 33.00 ± 4.67 | 33.92 ± 5.07 | 0.480 | 0.199 | 0.416 | 0.560 |
| Total | 93.23 ± 9.84 | 99.00 ± 9.03 | 103.92 ± 7.11 | 0.250 | 0.032 | 0.524 | 0.837 |
| Emotional intelligence measured with WLEIS | |||||||
| Self-emotions | 5.46 ± 0.083 | 5.94 ± 0.77 | 6.17 ± 0.49 | 0.013 | 0.023 | 0.973 | 0.886 |
| Regulation | 5.88 ± 0.56 | 5.94 ± 0.47 | 6.10 ± 0.44 | 0.997 | 0.656 | 0.443 | 0.990 |
| Use of Emotions | 5.48 ± 0.81 | 5.63 ± 0.99 | 6.02 ± 0.70 | 0.996 | 0.108 | 0.264 | 0.655 |
| Others’ Emotions | 5.54 ± 0.85 | 5.71 ± 0.84 | 5.90 ± 1.13 | 0.745 | 0.459 | 0.337 | 0.423 |
| Total | 5.59 ± 0.48 | 5.85 ± 0.58 | 6.11 ± 0.48 | 0.097 | 0.012 | 0.671 | 0.982 |
| Self-efficacy measured through GAZE | |||||||
| Self-Efficacy | 16.08 ± 3.69 | 16.39 ± 3.36 | 17.38 ± 2.99 | 0.970 | 0.164 | 0.181 | 0.591 |
WHOQOL-BREF: Quality of life; TMMS24: Emotional intelligence; WLEIS: Emotional intelligence; GAZE Self-efficacy
Effect of moderate dose face-to-face well-teach intervention
The sample consisted of 91 medical students (62.8%) and 54 nurses (37.2%), with women representing 95 individuals (65.5%). The mean age was 23.86 (SD = 3.4), with a range of 21 to 34 years. All the scores of quality of life except for physical scores were improved following a mandatory face-to-face Well-Teach intervention. The highest improvement in scores was for psychological health (mean change = 0.870, 95%CI:-0.514-1.227, p < .001), following social health (mean difference = 0.501, 95%CI:-0.193-0.809, p < .001), and environmental health (mean difference = 0.307, 95%CI:-0.073-0.541, p = .005). Similarly, all components of cognitive and emotional skills assessed with the two emotional intelligence scales except for attention factor were found to be significantly improved following the Well-Teach intervention. The largest improvement in the TMMS-24 was observed for clarity scores (mean difference = 1.441, 95%CI:0.241–2.373, p = .009) and repair scores (mean difference = 1.310, 95%CI:0.107–2.514, p = .017). The effect of wellness intervention had the highest impact on the total emotional intelligence scores as measured by TMMS-24 (mean difference = 3.021, 95%CI:0.553–5.488, p = .008) and WLEIS (mean difference = 0.192, 95%CI:0.112–0.272, p < .001) among all surveys. In the emotional intelligence subscales, self-emotion scores (mean difference = 0.234, 95%CI:0.054–0.415, p = .006), regulation of emotions (mean difference = 0.100, 95%CI:0.018–0.218, p = .018), use of emotion scores (mean difference = 0.253, 95%CI:0.149–0.358, p < .001), and other emotion scores (mean difference = 0.193, 95%CI:0.045–0.342, p = .006) yielded significant improvements following the intervention. In addition, self-efficacy scores were also improved after intervention (mean difference = 0.400, 95%CI:0.110–0.690, p = .004) (Table 3).
Table 3.
Effect of moderate dose face-to-face well-teach intervention on quality of life, emotional intelligence, and self-efficacy scores (n = 145 students)
| Variables | T1 (pre) | T2(post) | Change (95% CI) | p value | Effect size |
|---|---|---|---|---|---|
| Quality of life measured with WHOQOL- BREF | |||||
| Physical | 15.81 ± 2.13 | 15.90 ± 2.17 | 0.087(-0.316-0.143) | 0.228 | 0.062 |
| Psychological | 13.90 ± 2.62 | 14.77 ± 2.46 | 0.870(0.514–1.227) | < 0.001 | 0.402 |
| Social | 15.45 ± 3.08 | 15.95 ± 2.90 | 0.501(0.193–0.809) | < 0.001 | 0.267 |
| Environmental | 15.62 ± 2.25 | 15.92 ± 2.37 | 0.307(0.073–0.541) | 0.005 | 0.215 |
| Emotional intelligence measured with TMMS24 | |||||
| Attention | 35.90 ± 8.96 | 36.17 ± 9.88 | 0.269(0.907–1.445) | 0.326 | 0.038 |
| Clarity | 35.58 ± 8.64 | 37.02 ± 9.93 | 1.441(0.241–2.642) | 0.009 | 0.197 |
| Repair | 36.94 ± 8.92 | 38.26 ± 9.76 | 1.310(0.107–2.514) | 0.017 | 0.179 |
| Total | 108.42 ± 19.95 | 111.44 ± 24.42 | 3.021(0.553–5.488) | 0.008 | 0.201 |
| Emotional intelligence measured with WLEIS | |||||
| Self-emotions | 5.61 ± 1.01 | 5.84 ± 0.88 | 0.234(0.054–0.415) | 0.006 | 0.213 |
| Regulation | 5.75 ± 0.92 | 5.85 ± 0.92 | 0.100(0.018–0.218) | 0.048 | 0.139 |
| Use of Emotions | 5.81 ± 0.93 | 6.06 ± 0.82 | 0.253(0.149–0.358) | < 0.001 | 0.397 |
| Others’ Emotions | 5.31 ± 1.25 | 5.50 ± 1.18 | 0.193(0.045–0.342) | < 0.006 | 0.213 |
| Total | 5.62 ± 0.71 | 5.81 ± 0.72 | 0.192(0.112–0.272) | < 0.001 | 0.201 |
| Self-efficacy measured with GAZE | |||||
| Self-Efficacy | 19.30 ± 3.05 | 19.70 ± 2.95 | 0.400(0.110–0.690) | 0.004 | 0.227 |
WHOQOL-BREF: Quality of life; TMMS24: Emotional intelligence; WLEIS: Emotional intelligence; GAZE: Self-efficacy; CI: confidence interval
Discussion
The study findings demonstrate improved scores in all areas related to participants’ quality of life, emotional intelligence, and self-efficacy. These enhancements were consistent regardless of the duration of training, the delivery method (face-to-face or virtual), participants’ motivation (incentivized, mandatory or voluntary), and the intensity of the training (low, moderate, or high dose). Most scores were significantly improved except for a few factors in the high-dose face-to-face Well-Teach intervention cohort. The discrepancy may be attributed to the sample size or the nature of the intervention, which was more intensive. It is noteworthy that one month following the intervention, all scores increased in the high-dose intervention, suggesting the potential for a synergistic effect.
The studies described in the manuscript began with the program’s launch at a Mexican university through virtual means and later expanded to the USA, targeting medical students and nurses. In the USA, the program started with a high-intensity voluntary participation approach. Despite achieving satisfactory results with a limited number of participants, it was evident that challenges commonly found in academic literature persisted, particularly related to engagement. Reasons for non-participation, according to those who did attend, included those non-participants were stressed, overwhelmed, and felt that they could not devote those hours to a workshop when they could be using that time to prepare for their academic demands. Thanks to the institutional support and endorsement from organizational leaders which enabled the introduction of mandatory workshops before classes, it was possible to delve deeper into the holistic wellness model. This became achievable following the demonstration of alignment with crucial competencies in medical and nursing preceptorships, indicating that integrating wellness workshops into the curriculum could be a promising and feasible strategy.
In order to have a sustainable cultural shift, Wellness needs to become part of their workload and might be part of their learning/recall of lifelong wellness resources, tools and competencies. For example, those included by the Accreditation Council for Graduate Medical Education (ACGME) involving competencies in patient care, knowledge for practice, practice-based learning and improvement, interpersonal and communication skills, professionalism, systems-based practice, interprofessional collaboration, and personal and professional development for medical students [72, 73]. Nursing student competencies and sub-competencies identified in the © 2021 American Association of Colleges of Nursing curriculum [74] suggest the workshop can be linked to Person-Centered Care, Population Health, Quality and Safety and Interprofessional Partnerships competencies. In the Mexican university included in this study the competencies are regulated by the “Consejo Mexicano para la acreditacion de la educacion médica A.C.” and the “School of Nursing from the Consejo Méxicano para la acreditación de enfermería A.C.”
The study faced limitations like a small sample size in the high-dose face-to-face voluntary intervention, a 54% attrition rate (with only 13 out of 35 students participating). Missing results due to data matching challenges. While all students in the USA. intervention cohort attended the mandatory workshops as part of the Well-Teach intervention, which included a moderate dose of face-to-face interaction, the pre-post measures could not be matched due to errors made by participants in recalling and entering their anonymous IDs. The same thing happened in Mexico with the voluntary workshop, which reduced the sample size; providing students with pre-assigned IDs rather than requiring them to create their own is recommended. The sample includes only students from the school of Medicine and Nursing at two universities, one in the USA and on in Mexico, and may not be generalizable. These workshops have not been tested against another intervention or a placebo-control group that may achieve similar results. Longitudinal measures to observe the effects at long term, were not collected in all the intervention cohorts with the exception of one short measure at one month in high-dose face-to-face voluntary intervention. Improvements in the outcome measures considered may not necessarily be related to our Well-Teach Workshop with respect to wellness, cognitive and emotional abilities, and/or effectiveness, but may be attributable to other causes. Organizational change was not assessed in the present study because our proposal posits the need for preliminary steps to cultivate a culture of wellness that can foster both individual and organizational change in the future. Therefore, it is possible that the implementation of these initial steps may not have a long-term and/or organizational impact. The wellness model, despite limitations, demonstrated a systematic benefit with consistent perceived improvement sustained for one month, suggesting the potential for a synergistic effect. The workshops (not presented here) were met with high satisfaction by participants, which may prove to be an effective strategy for addressing the challenges of low engagement and/or attrition. By incorporating wellness into their practices, students can understand the lasting importance of well-being and adhere to its principles.
Moving forward, it is essential to assess the competencies and skills acquired in wellness and determine their long-term sustainability in future studies. Success in future studies must be evaluated by assessing the competencies and skills acquired in relation to wellness, and whether these are sustained in the long term. Organizational transformations post-pandemic, driven by visionary leadership, underscore the imperative of cultivating, appreciating, and nurturing a wellness-oriented culture to ensure that these changes become intrinsic to the organization and ingrained as a personal philosophy of life at the individual level [75]. Nevertheless, in order to implement and evaluate organizational changes, it is necessary to consider that the question of why wellness is relevant is not the issue at hand. In contrast, greater significance is ascribed to the question of how to implement comprehensive wellness programs that demonstrate tangible outcomes at the individual level, as a precursor to achieving and maintaining the requisite organizational changes. In order to support and sustain the investment required, a culture of wellness is necessary and can start by considering preliminary early steps in education. Based on our experience, it is advised that these steps be included in the curriculum by taking a holistic approach, in line with the approach used in this study. The concept of wellness permits a multiplicity of approaches to its delivery, reflecting the intrinsic diversity of human beings and their needs. The advent of new pedagogical approaches has been accompanied by a shift in the very nature of learning and teaching. This suggests that the implementation of a culture of wellness will necessarily evolve in response to these changes.
Acknowledgements
We thank Nayla Bejarano for her assistance throughout the pilot study in recruiting participants and for her helpful comments regarding published scientific evidence during the conduct of the study.
Author contributions
Conceptualization, data curation, investigation, supervision, methodology, formal analysis, validation, writing original draft of manuscript – Marie Leiner & Beverley Argus-Calvo. Data curation, investigation, supervision, validation, review of and editing manuscript – Maureen Frances, Paul CarrolaMethodology, writing original draft of manuscript- Deborah Clegg & Alok Dwivedi.
Funding
Drs Leiner and Argus-Calvo received an institutional seed grant for the IRB approved study for the assessment of intervention based on an incentive method classified as a High dose face-to-face Well-Teach intervention.
Data availability
Data availability: The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request before acceptance. The data will be available in a public repository database. The DOI/accession codes will be made available at acceptance.
Declarations
Ethics approval and consent to participate
We sought Institutional Review Board (IRB) approval from Texas Tech University Health Sciences Center El Paso prior to initiating our study. The IRB approved our study for the assessment of our intervention based on an incentive method waving informed consent while other assessments were exempted from IRB approval as they did not meet the definition of human subject research, per 46.102(e)(1)(ii), as the information was not identifiable. During workshops offered to students in the USA and Mexico, this unidentified data was collected voluntarily.
Consent for publication
All authors have contributed substantially to the conception of the work that has not been submitted for publication elsewhere and have given consent for publication.
Clinical trial number
A clinical trial number was not obtained because our research study did not prospectively assign people or groups of people to receive one or more health-related interventions to evaluate the effects on health outcomes.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.National Academies of Sciences E, Medicine. National Academy of, Medicine, Committee on Systems Approaches to improve patient care by supporting Clinician W-B. Taking Action against Clinician Burnout: A systems Approach to Professional Well-Being. edn. Washington (DC): National Academies Press (US); 2019. [PubMed] [Google Scholar]
- 2.Nituica C, Bota OA, Blebea J, Cheng CI, Slotman GJ. Factors influencing resilience and burnout among Resident Physicians - A National Survey. BMC Med Educ 2021, 21(1). [DOI] [PMC free article] [PubMed]
- 3.Zhou T, Xu C, Wang C, Sha S, Wang Z, Zhou Y, Zhang X, Hu D, Liu Y, Tian T et al. Burnout and well-being of Healthcare Workers in the post-pandemic period of COVID-19: a perspective from the job demands-resources Model. BMC Health Serv Res 2022, 22(1). [DOI] [PMC free article] [PubMed]
- 4.Alrawashdeh HM, Al-Tammemi AB, Alzawahreh MK, Al-Tamimi A, El-Kholy MS, Sarireh FA, Abusamak M, Elehamer NMK, Malkawi A, Al-Dolat W et al. Occupational burnout and job satisfaction among Physicians in Times of COVID-19 Crisis: a convergent parallel mixed-method study. BMC Public Health 2021, 21(1). [DOI] [PMC free article] [PubMed]
- 5.Iktidar MA, Ara R, Roy S, Ahmed M, Chowdhury S, Eva FN, Trisha SM, Sharif AB. Imposter phenomenon among health professionals and students: a protocol for systematic review and meta analysis. Med (Baltim). 2023;102(29):e34364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maslach C, Schaufeli WB, Leiter MP. Job Burnout. Ann Rev Psychol. 2001;52(1):397–422. [DOI] [PubMed] [Google Scholar]
- 7.Chirico F, Ferrari G, Nucera G, Szarpak L, Crescenzo P, Ilesanmi O. Prevalence of anxiety, depression, burnout syndrome, and mental health disorders among healthcare workers during the COVID-19 pandemic: a rapid umbrella review of systematic reviews. J Health Soc Sci. 2021;6(2):209–20. [Google Scholar]
- 8.Ghahramani S, Lankarani KB, Yousefi M, Heydari K, Shahabi S, Azmand S. A systematic review and meta-analysis of burnout among healthcare workers during COVID-19. Front Psychiatry. 2021;12:758849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meira-Silva VS, Freire ACT, Zinezzi DP, Ribeiro FC, Coutinho GD, Lima IM, Crispi IC, Porto JD, Silva LG, Miranda LHA. Burnout syndrome in healthcare workers during the COVID-19 pandemic: a systematic review. Revista Brasileira De Med Do Trabalho. 2022;20(1):122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharifi M, Asadi-Pooya AA, Mousavi-Roknabadi RS. Burnout among healthcare providers of COVID-19; a systematic review of epidemiology and recommendations. Archives Acad Emerg Med 2021, 9(1). [DOI] [PMC free article] [PubMed]
- 11.Leo CG, Sabina S, Tumolo MR, Bodini A, Ponzini G, Sabato E, et al. Burnout among healthcare workers in the COVID 19 era: a review of the existing literature. Front Public Health 2021:9. https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2021.750529. 10.3389/fpubh.2021.750529 [DOI] [PMC free article] [PubMed]
- 12.Deeb GR, Braun S, Carrico C, Kinser P, Laskin D, Golob Deeb J. Burnout, depression and suicidal ideation in dental and dental hygiene students. Eur J Dent Educ. 2018;22(1):e70–4. [DOI] [PubMed] [Google Scholar]
- 13.Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, Shanafelt TD. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89(3):443–51. [DOI] [PubMed] [Google Scholar]
- 14.Hope V, Henderson M. Medical student depression, anxiety and distress outside North America: a systematic review. Med Educ. 2014;48(10):963–79. [DOI] [PubMed] [Google Scholar]
- 15.Rudman A, Gustavsson JP. Burnout during nursing education predicts lower occupational preparedness and future clinical performance: a longitudinal study. Int J Nurs Stud. 2012;49(8):988–1001. [DOI] [PubMed] [Google Scholar]
- 16.Durham ME, Bush PW, Ball AM. Evidence of burnout in health-system pharmacists. Am J Health Syst Pharm. 2018;75(23 Supplement 4):S93–100. [DOI] [PubMed] [Google Scholar]
- 17.Friganovic A, Selic P, Ilic B, Sedic B. Stress and burnout syndrome and their associations with coping and job satisfaction in critical care nurses: a literature review. Psychiatr Danub. 2019;31(Suppl 1):21–31. [PubMed] [Google Scholar]
- 18.Rodrigues H, Cobucci R, Oliveira A, Cabral JV, Medeiros L, Gurgel K, Souza T, Goncalves AK. Burnout syndrome among medical residents: a systematic review and meta-analysis. PLoS ONE. 2018;13(11):e0206840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Guillebon E, He C, Akhtar S, Pietrzak RH, Ripp J, Peccoralo L. Association of Psychological Safety with burnout and intent to leave among Physician Faculty in New York city. J Gen Intern Med 2024:1–7 [DOI] [PubMed]
- 20.Frajerman A, Morvan Y, Krebs MO, Gorwood P, Chaumette B. Burnout in medical students before residency: a systematic review and meta-analysis. Eur Psychiatry. 2019;55:36–42. [DOI] [PubMed] [Google Scholar]
- 21.Bianchi R, Schonfeld IS, Laurent E. Is burnout a depressive disorder? A reexamination with special focus on atypical depression. In., vol. 21. International Journal of Stress Management; 2014: 307–324.
- 22.Panagioti M, Geraghty K, Johnson J, Zhou A, Panagopoulou E, Chew-Graham C, Peters D, Hodkinson A, Riley R, Esmail A. Association between Physician Burnout and Patient Safety, Professionalism, and patient satisfaction: a systematic review and Meta-analysis. JAMA Intern Med. 2018;178(10):1317–30. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 23.Regehr C, Glancy D, Pitts A, LeBlanc VR. Interventions to reduce the consequences of stress in physicians: a review and meta-analysis. J Nerv Ment Dis. 2014;202(5):353–9. [DOI] [PubMed] [Google Scholar]
- 24.Pereira-Lima K, Mata DA, Loureiro SR, Crippa JA, Bolsoni LM, Sen S. Association between Physician depressive symptoms and medical errors: a systematic review and Meta-analysis. JAMA Netw Open. 2019;2(11):e1916097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dunn HL. What high-level wellness means. Can J Public Health/Revue Canadienne De Sante’e Publique. 1959;50(11):447–57. [PubMed] [Google Scholar]
- 26.Hettler B. Wellness Promotion on a University campus. Fam Community Health 1980, 3(1). [DOI] [PubMed]
- 27.Tarfarosh S, Achakzai BK. Promoting resilience in Healthcare Students through psychological interventions. Bjpsych Advances; 2022.
- 28.Townsley AP, Li-Wang J, Katta R. Healthcare Workers’ Well-Being: A Systematic Review of Positive Psychology Interventions. Cureus 2023. [DOI] [PMC free article] [PubMed]
- 29.McVeigh C, Ace L, Ski CF, Carswell C, Burton SG, Rej S, Noble H. Mindfulness-based interventions for undergraduate nursing students in a University setting: a narrative review. Healthcare; 2021. [DOI] [PMC free article] [PubMed]
- 30.Nanda A, Wasan A, Sussman J. Provider Health and Wellness. J Allergy Clin Immunol Pract. 2017;5(6):1543–8. [DOI] [PubMed] [Google Scholar]
- 31.Munn LT, Huffman C, Connor CD, Swick M, Danhauer SC, Gibbs M. A qualitative exploration of the National Academy of Medicine Model of Well-being and Resilience among Healthcare workers during COVID‐19. J Adv Nurs. 2022;78(8):2561–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kalina P. Resilient and Inclusive Healthcare Leadership: <scp > black swans, COVID-19, and Beyond</scp >. Int J Health Plann Manag. 2020;35(6):1611–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dzau VJ, Kirch D, Murthy V, Nasca T. National Plan for Health Workforce Well-being. In. Washington, DC: National Academies; 2024. [Google Scholar]
- 34.Bourcier D, Far R, King LB, Cai G, Mader J, Xiao MZ, Simon C, McFadden T, Flynn L. Medical student wellness in Canada: time for a national curriculum framework. Can Med Educ J. 2021;12(6):103–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nobile M. The WHO definition of health: a critical reading. Med L. 2014;33:33. [PubMed] [Google Scholar]
- 36.Goins RT, Spencer SM, Williams K. Lay meanings of health among rural older adults in Appalachia. J Rural Health. 2011;27(1):13–20. [DOI] [PubMed] [Google Scholar]
- 37.Leonardi F. The definition of health: towards new perspectives. Int J Health Serv. 2018;48(4):735–48. [DOI] [PubMed] [Google Scholar]
- 38.Bircher J, Kuruvilla S. Defining health by addressing individual, social, and environmental determinants: new opportunities for health care and public health. J Public Health Policy. 2014;35:363–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Venkatapuram S. Health, vital goals, and central human capabilities. Bioethics. 2013;27(5):271–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Greeson JM, Toohey MJ, Pearce MJ. An adapted, four-week mind-body skills group for medical students: reducing stress, increasing mindfulness, and enhancing self-care. Explore (NY). 2015;11(3):186–92. [DOI] [PubMed] [Google Scholar]
- 41.Lampe LC, Müller-Hilke B. Mindfulness-based intervention helps preclinical medical students to contain stress, maintain mindfulness and improve academic success. BMC Med Educ. 2021;21(1):145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Weingartner LA, Sawning S, Shaw MA, Klein JB. Compassion cultivation training promotes medical student wellness and enhanced clinical care. BMC Med Educ. 2019;19(1):139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Erogul M, Singer G, McIntyre T, Stefanov DG. Abridged mindfulness intervention to support wellness in first-year medical students. Teach Learn Med. 2014;26(4):350–6. [DOI] [PubMed] [Google Scholar]
- 44.Worobetz A, Retief PJ, Loughran S, Walsh J, Casey M, Hayes P, Bengoechea EG, O’Regan A, Woods C, Kelly D, et al. A feasibility study of an exercise intervention to educate and promote health and well-being among medical students: the ‘MED-WELL’ programme. BMC Med Educ. 2020;20(1):183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Morris A, Do D, Gottlieb-Smith R, Ng J, Jain A, Wright S, Shochet R. Impact of a fitness intervention on medical students. South Med J. 2012;105(12):630–4. [DOI] [PubMed] [Google Scholar]
- 46.Pipas CF, Damianos JA, Montalbano L, Matous AL, Hua J, Shoop GH. A curriculum to promote a culture of Wellness among Medical Students and Faculty. PRiMER. 2020;4:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Drolet BC, Rodgers S. A comprehensive medical student wellness program–design and implementation at Vanderbilt School of Medicine. Acad Med. 2010;85(1):103–10. [DOI] [PubMed] [Google Scholar]
- 48.Butcher M, Thompson KM, Williams M, Cooke BK, Merlo LJ. Assessment of Student perspectives on Improving Wellness in Medical School: qualitative results from a cross-sectional survey of medical students in Florida. Adv Med Educ Pract 2021. [DOI] [PMC free article] [PubMed]
- 49.Hill MS, Goicochea S, Merlo LJ. In their own words: stressors facing medical students in the millennial generation. Medical Education Online; 2018. [DOI] [PMC free article] [PubMed]
- 50.Reis AC, Mortimer T, Rutherford E, Sperandei S, Saheb R. Students as leaders in supporting Campus Well-being: peer‐to‐peer Health Promotion in Higher Education. Health Promotion J Australia 2021. [DOI] [PubMed]
- 51.Yurayat P, Seechaliao T. Effectiveness of online positive psychology intervention on Psychological Well-being among undergraduate students. J Educ Learn 2021.
- 52.Neufeld A. A commentary on Medical student wellness in Canada: time for a national curriculum framework. Can Med Educ J. 2022;13(2):103–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ripp JA, Kiely S, Frieman A. Institutional Responses and the Role of the Chief Wellness Officer. Caring for Caregivers to Be: A Comprehensive Approach to Developing Well-Being Programs for the Health Care Learner 2023:322.
- 54.Gonzalez CA, Gentile NE, Angstman KB, Craner JR, Bonacci RP. The associations between Preceptor Team lead relationships and Resident Wellness in an Academic Medicine setting: an exploratory study. PRiMER. 2017;1:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Brazeau CMLR, Shanafelt T, Durning SJ, Massie FS, Eacker A, Moutier C, Satele DV, Sloan JA, Dyrbye LN. Distress among Matriculating Medical Students relative to the General Population. Acad Med 2014, 89(11). [DOI] [PubMed]
- 56.O’Flynn J, Dinan TG, Kelly JR. Examining stress: an investigation of stress, mood and exercise in medical students. Ir J Psychol Med. 2018;35(1):63–8. [DOI] [PubMed] [Google Scholar]
- 57.Hirotsu C, Tufik S, Andersen ML. Interactions between sleep, stress, and metabolism: from physiological to pathological conditions. Sleep Sci. 2015;8(3):143–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ludwig AB, Burton W, Weingarten J, Milan F, Myers DC, Kligler B. Depression and stress amongst undergraduate medical students. BMC Med Educ. 2015;15(1):141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Myers JE, Sweeney TJ. The indivisible self: an evidence-based model of wellness. J Individual Psychol. 2004;60:234–44. [Google Scholar]
- 60.Mayer JD, Salovey P. The intelligence of emotional intelligence. In., vol. 17: Elsevier; 1993: 433–442.
- 61.Gómez C, Lamas A, Ramirez-Martinez FR, Blunk D, Leiner M. Rethinking strategies and programs to Improve Physical and Emotional Well-being among Healthcare professionals: facing the New Normalcy. Med Sci Educ. 2021:1–8. [DOI] [PMC free article] [PubMed]
- 62.Medina MDC, Calderon A, Blunk DI, Mills BW, Leiner M. Organizational Wellness Program Implementation and evaluation: a holistic Approach to improve the wellbeing of Middle managers. J Occup Environ Med. 2018;60(6):515–20. [DOI] [PubMed] [Google Scholar]
- 63.Leiner M, Reyes-Chacón MT, Ramírez-Martínez FR, Márquez-Miramontes B. Evaluating a wellness intervention including micro-practices for healthcare professionals before and during COVID-19. Horizonte Sanitario. 2022;22(1):19–25. [Google Scholar]
- 64.Myers JE, Sweeney TJ, Witmer JM. The wheel of wellness counseling for wellness: a holistic model for treatment planning. J Couns Dev. 2000;78(3):251–66. [Google Scholar]
- 65.Group W. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. 1998;28(3):551–8. [DOI] [PubMed] [Google Scholar]
- 66.Fernández-Berrocal P, Extremera N, Ramos N. Validity and reliability of the Spanish modified version of the Trait Meta-Mood Scale. Psychol Rep. 2004;94(3):751–5. [DOI] [PubMed] [Google Scholar]
- 67.Salovey P, Mayer JD, Goldman SL, Turvey C, Palfai TP. Emotional attention, clarity, and repair: Exploring emotional intelligence using the Trait Meta-Mood Scale. 1995.
- 68.Wong CS, Law KS. The effects of leader and follower emotional intelligence on performance and attitude: an exploratory study. In Leadership perspectives. edn.: Routledge; 2017. pp. 97–128.
- 69.Nielsen T, Dammeyer J, Vang ML, Makransky G. Gender fairness in self-efficacy? A rasch-based validity study of the General Academic Self-Efficacy Scale (GASE). Scandinavian J Educational Res. 2018;62(5):664–81.
- 70.Greenhouse SW, Geisser S. On methods in the analysis of profile data. Psychometrika. 1959;24(2):95–112. [Google Scholar]
- 71.Cohen J. Statistical power analysis for the behavioral sciences. Academic; 2013.
- 72.Nursing AAC. The essentials: Core competencies for professional nursing education. In.; 2021.
- 73.Englander R, Cameron T, Ballard AJ, Dodge J, Bull J, Aschenbrener CA. Toward a Common Taxonomy of Competency Domains for the Health Professions and competencies for Physicians. Acad Med. 2013;88(8):1088–94. [DOI] [PubMed] [Google Scholar]
- 74.The Essentials. Core competencies for professional nursing education. [https://www.aacnnursing.org/Portals/42/AcademicNursing/pdf/Essentials-2021.pdf]
- 75.Five Essentials for Workplace. Mental Health & Well-Being
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data availability: The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request before acceptance. The data will be available in a public repository database. The DOI/accession codes will be made available at acceptance.