Abstract
Abstract
Introduction
Amid the COVID-19 pandemic, outpatients’ concerns about infection risk have increased. It is crucial to understand the factors that contribute to this fear of infection to promote patient safety and encourage outpatients to seek proper follow-up treatment without fear. This study aims to understand the relationship between outpatients’ experiences of patient safety and their fear of infection.
Design
This was a secondary analysis of national data from the Healthcare Service Experience Survey in 2020.
Setting and participants
A total of 4416 patients with experience using outpatient services in the past year were included in South Korea.
Primary and secondary outcome measures
Demographic characteristics, fear of infection and safety experiences were assessed in the original survey. Fear of infection served as the dependent variable, with safety experiences—specifically, patient identification, preinjection explanations, hand hygiene, proper use of injection supplies, skin disinfection and adverse drug reactions—as the independent variables.
Results
Approximately 14% of outpatients had a fear of infection when receiving medical care. The unadjusted model showed that all patient safety categories were determinants of fear of infection, and the multivariate logistic model identified hand hygiene and medication safety experiences as significant factors associated with fear of infection.
Conclusions
This study revealed that patient safety experiences are associated with fear of infection in outpatient settings. Improving healthcare professionals’ hand hygiene and managing adverse drug reactions are crucial for enhancing patient safety.
Keywords: Hospitals, Patient Reported Outcome Measures, Infection control, Health & safety
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Our study sheds light on the psychological response to infection among patients in an outpatient setting.
We have elucidated the interplay between negative patient safety experiences and fear of infection.
This study strongly emphasises the necessity of implementing a policy that focuses on promoting proactive behaviours among healthcare professionals.
The survey items, which specifically address the fear of infection as a single question, have limitations in fully capturing a comprehensive range and various aspects of responses.
The original survey investigated experiences of outpatient utilisation within the past year, introducing the potential for recall bias.
Introduction
Patient-centred care has become an important concept for improving the quality of healthcare.1 In patient-centred care, the patient’s experience is crucial, and communication, the expertise of the healthcare team and the connection between patients and healthcare team members are emphasised in order to achieve the best possible patient experience.2 In the realm of patient safety, the focus is shifting beyond the healthcare provider system to patient engagement.3 Patient safety encompasses patient identification, communication with healthcare providers, infection prevention, surgical safety, fall prevention and more.4 Patients experience a variety of encounters in the healthcare services they receive, and experiences of patient safety play a crucial role in improving the quality of healthcare services.
In the outpatient setting, individuals have shorter hospital stays than in the inpatient setting but are more likely to be exposed to a larger number of unidentified individuals. COVID-19 has notably disrupted the utilisation of medical services, and visits to healthcare facilities have exhibited a more pronounced decline than hospital admissions.5 While a myriad of governmental policies, such as lockdowns and vaccination drives, may have influenced this trend in various nations,6 it is equally plausible that individuals have been reluctant to seek medical care due to apprehensions surrounding infection risks.7 Consequently, these factors have likely precipitated substantial changes in patient safety experiences compared with previous norms.
Healthcare-associated infections (HAIs) are a growing concern in healthcare settings around the world because they pose a significant risk to patient safety.8 HAIs refer not only to infections contracted during hospitalisation but also to infections related to medical activities within healthcare facilities, including outpatient care.9 The incidence of HAIs is estimated to range from 5% to 10% in South Korea.10 As concern about HAIs has increased, and with the ongoing spread of COVID-19, patients have become increasingly anxious about the risk of infection from exposure to other patients, contact with healthcare professionals (HCPs) and invasive procedures such as injections or blood tests during their visits to medical institutions. In fact, the percentage of outpatients who felt anxious about infection during the use of medical facilities has continued to increase, from 3% in 2018 to 6% in 2019, and then reaching 31.2% in 2021.11
The fear of infection is a crucial issue since it not only has a negative impact on a patient’s psychological state but also has the potential to trigger avoidance behaviour toward healthcare facilities.12 Lau et al13 found that individuals with a higher fear of infection, particularly related to SARS, were more likely to avoid hospital visits. Chatterji and Li14 analysed the relationship between COVID-19 and hospital utilisation, people tend to avoid visiting hospitals voluntarily when they perceive them as dangerous places due to the risk of catching infectious diseases. The utilisation of medical services, including emergency rooms, inpatient settings and outpatient settings, has decreased due to a fear of hospitals during the COVID-19 pandemic.15 This is a significant healthcare issue that leads to unmet medical needs and delays in treatment. In particular, assessing the fear of infection among outpatients is important, given that voluntary participation in follow-up observations is especially critical for outpatients.
Fear of infection can prompt individuals to avoid making outpatient visits to medical institutions, which can lead to delays in medical treatment and decreased quality of care.16 Research has indicated that fear of COVID-19 resulted in discontinuity of care and lost follow-up; it has even led to acute cardiovascular events among patients with cardiovascular diseases.17 Hence, there is a need for empirical research on the fear of infection at medical institutions in outpatient contexts, as well as for identifying the factors that would encourage patients to use hospitals without significant fear of infection.
Fear is an intense emotion triggered by perceiving an immediate threat.18 Fear of infection encompasses multiple complex concepts, including the fear of becoming infected or infecting others, as well as the suspicion that people in the vicinity may transmit the disease.19 These psychological responses are influenced by various factors, including personal characteristics, knowledge, experiences and cultural backgrounds.20 21 In fact, previous studies have shown that an individual’s age, sex, marital status, medical coverage, economic activity and prior experience with a disease are associated with their psychological response to infection.13 22 23 Although evidence has been published regarding factors influencing fear of infection among the general population,13 22 23 there is a lack of research that focuses specifically on experiences during hospital treatment. Since HAIs result from interactions between patients and HCPs, it is necessary to investigate the relationship between patients’ fear of infection and their experiences during medical treatment by HCPs.
Therefore, this study aimed to investigate the perceived fear of infection among outpatients and sought to understand the relationship between their experiences of patient safety and their fear of infection.
Methods
Study design
This study is a secondary cross-sectional analysis of existing data.
Source of data and data collection
We used 2020 public data from the Korean Ministry of Health and Welfare’s Healthcare Service Experience Survey (HSES).24 This survey has been conducted annually since 2017 to assess service levels at Korean healthcare institutions and public perceptions of the healthcare system. The HSES questionnaire was developed by incorporating the content of major patient experience surveys conducted in various countries and collecting expert opinions.25 It was refined through focus group interviews and a pilot survey targeting the general population, leading to the finalisation of the questionnaire and validation study was also conducted.25 26 This survey was conducted using a face-to-face tablet-assisted personal interviewing (TAPI) process based on household visits by well-trained investigators from 13 July 2020 to 7 October 2020.27 The participants were asked to recall their medical experiences over the past year, specifically from July 2019 to June 2020.25 The investigators received a 3-hour training session that covered an overview of the survey, survey completion guidelines and survey system usage, along with practical training. They were also required to complete privacy protection training. Additionally, survey guidelines were developed and distributed for investigators to bring to the field.25 27 As the HSES was conducted using a TAPI system, outliers were automatically excluded based on the internal validation logic installed on the tablets. The HSES obtained informed consent voluntarily from all participants. However, if participants had impaired cognitive function or disabilities, informed consent was obtained from their respective family members. The HSES data are accessible to any individual through the Microdata Integrated Service website (https://mdis.kostat.go.kr),24 and we obtained the raw data of the HSES after submitting a research proposal on 16 January 2023. Following the acquisition of the raw data on 16 January 2023, this secondary analysis was conducted through July 2023.
Study setting and sampling
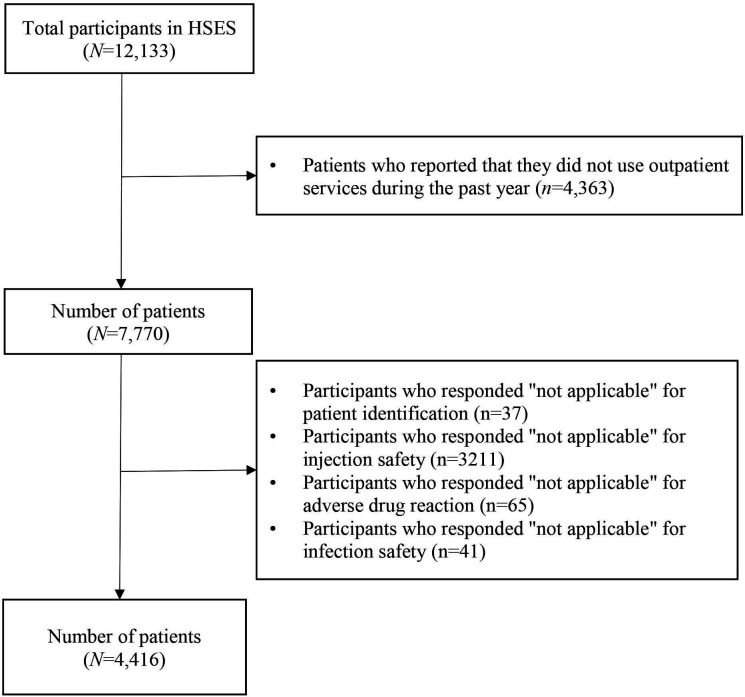
The setting of this study was Korea. The target population comprised people aged over 15, totalling 42 254 722 individuals from 20 343 188 households. Among them, a sample of 6000 households was selected using stratified two-stage cluster sampling methods. The strata comprised a total of 26 regions, and sample distribution was determined using square root proportional allocation based on the distribution of households in each stratum of the study population. The two-stage cluster sampling process consisted of first selecting survey areas and then secondarily selecting households and their members. In accordance with the 2020 HSES survey,26 27 total number of participants was 12 133 of 6000 households. After the raw data were obtained, the research selection process was conducted as illustrated in figure 1. Initially, only those who had used outpatient services during the prior 12 months were included in the sampling frame, which excluded those (N=4363) who had not used outpatient services. Additionally, those who answered ‘not applicable’ to the dependent or independent variables were also excluded (N=3354). As a result, a total of 4416 participants were analysed in this study.
Figure 1. Flow diagram of participant selection process. HSES, Healthcare Service Experience Survey.
Variables
Outcome variable: fear of infection
Fear of infection was used as a dependent variable. The outcome variable was obtained from the survey question ‘Have you experienced fear regarding infection while using healthcare facilities in the last 12 months?’ Responses were categorised as ‘yes’ or ‘no’.
Predictor: experiences of patient safety
Patient safety refers to the prevention of harm or injury to patients during the course of their healthcare and encompasses a range of practices and strategies designed to ensure that patients receive safe, effective care.28 In this study, six survey questions related to patient safety were included from the HSES. The first question concerned proper patient identification: ‘Did HCPs always verify your identity (name and date of birth) before administering injections, tests, surgeries or procedures?’ The next four questions were about injection safety topics, specifically providing an explanation (‘Did HCPs explain the reason for the injection before administering it?’), hand hygiene (‘Did HCPs clean their hands with hand sanitiser before administering the injection?’), the proper use of syringes and vials (‘Did you observe HCPs open the sealed syringe and injection supplies before administering the injection to you?’) and skin disinfection (‘Did HCPs disinfect your skin before administering the injection?’). The sixth question pertained to medication safety: ‘Did you experience any adverse drug reactions while visiting this healthcare facility?’ Each response was categorised as ‘yes’ or ‘no’.
Covariates
Sociodemographic factors and health status were used as covariates. Regarding the sociodemographic factors, we included sex, age, educational level, type of insurance, job status and income level. Age was categorised into two groups: <60 years and 60 years. Sex was classified as male or female. There were three levels of education: primary (elementary school graduate or no education), secondary (middle school or high school graduate) and higher (college, bachelor’s degree, postbaccalaureate degree). Insurance type was either national health insurance or, for some participants with lower incomes, Medical Aid. In Korea, health insurance is mandatory for all citizens, and Medical Aid is provided for those in low-income groups and the economically vulnerable who cannot afford the cost of insurance. Job status was classified into two categories: employed, which includes both self-employed individuals and workers, and unemployed, encompassing homemakers, students, and those currently without employment. Income was categorised into quintiles; the first quintile represented the lowest 20% of the population’s income, while the fifth represented the highest 20%. As health-related factors, we included underlying chronic disease status and self-perceived health status.
Statistical analysis
The original data collection method employed electronic systematic approaches to prevent non-responses and outliers by implementing error message pop-ups and setting predefined ranges to avoid the entry of outliers. Consequently, there were no instances of non-response and outliers in our research variables. We analysed the frequency and weighted percentages of each category to understand the general characteristics of the participants. Weighted percentages were used to generalise the findings to the population. To examine the association between the six patient safety experiences and fear of infection, we used the weighted χ2 test using the Rao-Scott correction and converted the results into F-statistics to determine statistical significance. Weighted univariate and multivariate logistic regression analyses were performed to calculate the likelihood that individuals would have a fear of infection at medical institutions. In the multivariate model, the patient’s safety experience at the medical institution (based on the six survey questions mentioned earlier) was considered along with the specified covariates. A p<0.05 was considered statistically significant using a two-tailed test. All statistical analyses were conducted by using Stata/MP V.18.0.
Patient and public involvement
This study is a secondary analysis of existing data, consequently, no patients were directly involved in the study design, recruitment or data collection phases. However, the findings from this analysis have the potential to significantly impact patient care by informing strategies to enhance outpatient healthcare experiences and improve patient safety.
Results
Table 1 shows the descriptive characteristics of the participants. Most of the participants were female (n=2514, 54.9%), were younger than 60 years (n=2569, 60.9%), had a secondary school education (n=2302, 50.1%), subscribed to national health insurance (n=4311, 97.5%) and were employed (n=2451, 55.2%). For chronic diseases, the prevalence was highest for hypertension (n=1137, 23.8%), followed by diabetes mellitus (n=540, 11.6%). Approximately 60% of the participants indicated that they perceived their health as good (n=2268, 53.0%) or very good (n=497, 10.5%), while smaller proportions of participants reported their health as bad (n=454, 9.8%) or very bad (n=75, 1.3%).
Table 1. Sociodemographic characteristics of participants*.
| Variable | Response | n | Weighted % | |
| Sociodemographic | Sex | Male | 1902 | 45.1 |
| Female | 2514 | 54.9 | ||
| Age | <60 years | 2569 | 60.9 | |
| ≥60 years | 1847 | 39.1 | ||
| Education | Primary | 601 | 11.8 | |
| Secondary | 2302 | 50.1 | ||
| Higher | 1513 | 38.1 | ||
| Insurance type | National health insurance | 4311 | 97.5 | |
| Medical aid | 105 | 2.5 | ||
| Job status | Employed | 2454 | 55.2 | |
| Unemployed | 1962 | 44.8 | ||
| Income | First quintile | 827 | 20.9 | |
| Second quintile | 860 | 18.4 | ||
| Third quintile | 811 | 19.4 | ||
| Fourth quintile | 914 | 19.6 | ||
| Fifth quintile | 1004 | 21.7 | ||
| Health-related variables | Hypertension | No | 3279 | 76.2 |
| Yes | 1137 | 23.8 | ||
| Diabetes mellitus | No | 3876 | 88.4 | |
| Yes | 540 | 11.6 | ||
| Mental disorders | No | 4403 | 99.8 | |
| Yes | 13 | 0.2 | ||
| Respiratory disease | No | 4326 | 98.2 | |
| Yes | 90 | 1.8 | ||
| Heart disease | No | 4287 | 97.4 | |
| Yes | 129 | 2.6 | ||
| Cerebrovascular disease | No | 4344 | 98.5 | |
| Yes | 72 | 1.5 | ||
| Neurological disorders | No | 4321 | 98.2 | |
| Yes | 95 | 1.8 | ||
| Cancer | No | 4360 | 98.9 | |
| Yes | 56 | 1.1 | ||
| Thyroid gland disorders | No | 4313 | 98.0 | |
| Yes | 103 | 2.0 | ||
| Liver disease | No | 4382 | 99.2 | |
| Yes | 34 | 0.8 | ||
| Chronic kidney disease | No | 4402 | 99.6 | |
| Yes | 14 | 0.4 | ||
| Miscellaneous disease | No | 4096 | 93.1 | |
| Yes | 320 | 6.9 | ||
| Self-perceived health | Very good | 497 | 10.5 | |
| Good | 2268 | 53.0 | ||
| Neutral | 1122 | 25.4 | ||
| Bad | 454 | 9.8 | ||
| Very bad | 75 | 1.3 | ||
Frequencies are raw values and percentages are weighted.
The results regarding the participants’ experiences of patient safety at medical institutions and their fear of infection are reported in table 2. Participants reported that HCPs failed to follow the patient identification process properly (n=115, 2.3%). With regard to injection safety, participants reported that HCPs failed to provide proper explanations prior to administering injections (n=327, 7.2%), HCPs failed to clean their hands prior to administering injections (n=527, 10.9%), HCPs did not open sealed syringes and vials in their presence (n=316, 7.4%) and HCPs neglected to disinfect injection sites (n=248, 5.9%). Furthermore, some participants reported experiencing adverse drug reactions while receiving care at a medical institution (n=584, 12.8%). Lastly, 786 outpatients (14.1%) reported having a fear of infection while using the medical institution’s outpatient services, whereas 3630 outpatients (83.9%) stated that they did not have a fear of infection.
Table 2. Experiences of patient safety in medical institutions and patients’ fear of infection*.
| Experience in patient safety | Yes | No | ||
| n | Weighted % | n | Weighted % | |
| Patient identification | ||||
| HCPs verified the patient’s identity | 4301 | 97.7 | 115 | 2.3 |
| Injection safety | ||||
| HCPs provided an explanation for administering the injection | 4089 | 92.8 | 327 | 7.2 |
| HCPs performed hand hygiene before the injection | 3889 | 89.1 | 527 | 10.9 |
| HCPs opened the sealed syringe and injection supplies in the patient’s presence | 4100 | 92.6 | 316 | 7.4 |
| HCPs disinfected the skin before administering the injection | 4168 | 94.1 | 248 | 5.9 |
| Medication safety | ||||
| Experience in adverse drug reactions at medical institution | 584 | 12.8 | 3832 | 87.2 |
| Fear of infection | 786 | 14.1 | 3630 | 83.9 |
Frequencies are raw values and percentages are weighted.
HCP, healthcare professional
The result of the cross-tabulation analysis between patient safety experiences and fear of infection revealed significant associations with several patient experiences of patient safety factors (see table 3): patient identification experience (F=9.38, p=0.002), experience of HCPs providing explanations when administering injections (F=6.11, p=0.014), patient experience with HCPs’ hand hygiene (F=76.72, p<0.001), experience regarding HCPs’ proper use of injection supplies (F=6.35, p=0.012) and experience of adverse drug reactions (F=429.81, p<0.001).
Table 3. Cross-tabulation analysis of patient safety experiences and fear of infection.
| Experience in patient safety | Fear of infection | F(p)* | |
| Yes (%)† | No (%)† | ||
| Patient identification | 9.38 (0.002) | ||
| Yes | 15.8 | 84.2 | |
| No | 28.3 | 71.7 | |
| Explanation | 6.11 (0.014) | ||
| Yes | 15.6 | 84.4 | |
| No | 2.2 | 7.8 | |
| Hand hygiene | 76.72 (<0.001) | ||
| Yes | 13.5 | 86.5 | |
| No | 37.6 | 62.4 | |
| Proper use of injection supplies | 6.35 (0.012) | ||
| Yes | 15.6 | 84.4 | |
| No | 22.3 | 77.7 | |
| Skin disinfection | 2.01 (0.157) | ||
| Yes | 15.9 | 84.1 | |
| No | 20.5 | 79.5 | |
| Experience of adverse drug reaction | 429.81 (<0.001) | ||
| Yes | 55.7 | 44.3 | |
| No | 10.3 | 89.7 | |
To account for the weights in the data, we used a design based on F-test statistics and the corresponding p -values.
Percentages are weighted.
In the unadjusted logistic regression model (table 4), all items but one in the patient safety experience questionnaire—disinfection before an injection—were found to influence participants’ fear of infection. Participants who interacted with HCPs who had overlooked the patient identification process were 2.10 times more likely to have a fear of infection (OR 2.10; 95% CI 1.34, 3.28). Participants who observed HCPs disregarding the injection safety process were also more likely to have a fear of infection. Those who reported not receiving an explanation for their injection were 1.54 times more likely to have a fear of infection (OR 1.54; 95% CI 1.13, 2.08), and those who reported that HCPs had omitted hand hygiene were 3.85 times more likely to have a fear of infection (OR 3.85; 95% CI 3.08, 4.80). Participants who reported that HCPs had not opened the sealed syringe or vials for injection in their presence were likewise 1.55 times more likely to have a fear of infection (OR 1.55; 95% CI 1.15, 2.09). After covariates were accounted for in the multivariate logistic regression model, experiencing an adverse drug reaction and poor hand hygiene by HCPs were found to be significantly related to participants’ fear of infection. Participants who experienced an adverse drug reaction were 13.96 times more likely to have a fear of infection (OR 13.96; 95% CI 10.94, 17.87), and those who reported that HCPs had omitted hand hygiene were 8.00 times more likely to have a fear of infection at the medical institution they visited (OR 8.00; 95% CI 5.64, 11.33). However, other safety experiences did not show significant results in the multivariate logistic regression analysis.
Table 4. Association between experience in patient safety and fear of infection.
| Variable | Unadjusted model | Adjusted model†‡ | ||
| OR | 95% CI | OR | 95% CI | |
| Patient identification (reference, yes) | 2.10** | (1.34, 3.28) | 0.76 | (0.45, 1.30) |
| Explanation (reference, yes) | 1.54** | (1.13, 2.08) | 0.62 | (0.32, 1.21) |
| Hand hygiene (reference, yes) | 3.85*** | (3.08, 4.80) | 8.00*** | (5.64, 11.33) |
| Proper use of injection supplies (reference, yes) | 1.55** | (1.15, 2.09) | 0.79 | (0.41, 1.54) |
| Skin disinfection (reference, yes) | 1.37 | (0.97, 1.91) | 0.78 | (0.38, 1.61) |
| Adverse drug reaction (reference, no) | 10.89*** | (8.77, 13.53) | 13.96*** | (10.94, 17.87) |
*p<0.01, ***p<0.001.
Likelihood ratio (LR) χ²(29) = 71.05, p < 0.001.
Effects of sex, age, educational level, insurance type, income, job status, underlying disease and perceived health status were controlled for in the regression analyses.
Discussion
Our study found that 14.1% of Korean outpatients experienced a significant degree of fear of infection. This finding may be generalised to the entire Korean population who have used outpatient services in the past year. Additionally, we found that outpatients’ experiences of HCPs’ hand hygiene and medication safety may play a significant role in influencing their fear of infection. The findings of our study are noteworthy for revealing the influence of patient safety experiences in hospitals on outpatients’ fear of infection. Previous studies have mainly emphasised the importance of patient safety activities such as hand hygiene and patient identification in reducing hospital-acquired infections.29 Our study builds on these findings by indicating that patient safety activities inside hospitals may have an impact not only on patients’ physical health but also on their psychological well-being.
Prior research on the general fear of infections within hospitals, not specific to any particular infectious disease, is limited. Therefore, this study compared a general fear of infection in hospitals to existing research on COVID-19 fear. Fear of COVID-19 in various cohorts ranged from 18.1% to 45.2%,21 whereas in our study, the fear of infection in hospitals amid the COVID-19 pandemic was relatively low. The difference in findings may be attributed to differences in how infection fear was measured. Previous studies focused on fear of COVID-19 infection using structured instruments, while our study measured a general fear of infection during the first year of the COVID-19 pandemic.
The analysis of participants’ experiences with patient safety revealed that HCPs had the highest compliance rate with patient identification activities and the lowest compliance rate with hand hygiene activities. Our result is in line with previous studies, which have identified hand hygiene as one of the most frequently omitted infection-control activities by nurses.30 Despite a significant improvement in the hand hygiene compliance rate after the COVID-19 pandemic began,31 our results suggest that additional solutions should be sought to improve compliance further. Additionally, the incidence rate of medication safety issues reported in our study was higher than the 8% rate among the Swiss public.32 However, compared with the medication error rate that may be extracted from electronic records, the rate of patient-reported medication safety incidents was relatively low.33 These discrepancies in rates across measurement methods may arise from a lack of patient awareness concerning the extent of medication safety. Patients may neglect to report adverse effects if they have limited knowledge of medication safety, or they may report only severe cases.
Our research indicates that two kinds of patient safety experiences affected outpatients’ fear of infection. First, outpatients who had positive experiences with proactive HCPs were less likely to develop a fear of infection. Our results provide evidence to support an earlier study, which suggested that patients’ fear of infection was influenced by HCPs’ proactivity in infection control.34 According to the previous study, patient experience, knowledge and hygiene sensitivity are related to a patient’s general awareness of safety issues.34 35 Therefore, both institutional and patient-level actions are needed to improve patient safety experiences in hospitals. Second, patients who experienced medication safety incidents had a higher level of fear of infection in healthcare facilities. Our research is consistent with the result of a systematic review which revealed that negative experiences related to patient safety incidents can lead to a negative perception of healthcare institutions.36 A systematic review of studies of patients’ experiences of adverse events in healthcare noted that patients may feel distressed by such experiences.37 Our study provides evidence for the importance of implementing effective patient safety activities to prevent and manage patient safety issues, not only to improve patient outcomes but also to enhance patients’ trust and assurance in healthcare institutions.
This study has important policy and practical implications. Our research highlights the need for both institutional and patient-level actions to enhance outpatient patient safety. Institutionally, it is crucial to strengthen infection-control education and improve infrastructure to prevent adverse drug reactions. South Korea has improved its infectious disease management, mandating dedicated infection-control staff for hospitals with over 100 beds.38 However, there is a gap in government agencies’ oversight of how medical institutions manage infection-control education and activities.39 There is also a need for tailored infection-control education to support outpatient services since current educational offerings focus primarily on inpatients. In addition, staff shortages, patient overcrowding and heavy workloads have been reported as barriers to patient-safety compliance.40 41 In fact, the consultation time per patient in Korea was only 6.2 min per patient, corresponding to half of the average Organization for Economic Co-operation and Development (OECD) outpatient consultation time, of 12.6 min.42 43 It has also been reported that outpatient nurses experience job stress due to insufficient staffing,44 which may lead to inadequate explanations and omission of patient safety behaviours, such as careful observation of infusion-related reactions or performing hand hygiene. To improve the quality of outpatient medical services, it is necessary to implement a reinforced staffing policy that expands personnel for outpatients.
The Institute of Medicine Committee on the Quality of Health Care in America noted in 2000 that ‘to err is human’.45 Thus, unintended errors are always possible simply because HCPs are human. To prevent patient safety incidents, multiple layers of mechanisms are required to avoid safety behaviour omissions resulting from human error. Patient participation in patient safety activities may also serve as part of the overall mechanism for preventing such incidents. Patients should actively engage in their safety by asking questions, seeking information and participating in their treatment.46 In a study on patient safety behaviours and patient willingness to participate, patients were reluctant to ask challenging questions to HCPs, such as ‘Have you washed your hands?’ or ‘Would you check that this is the correct medication for me?’.47 Based on the traditional relationship between HCPs and patients in which the latter are regarded as passive recipients of the former’s care,48 patients may hesitate to challenge an HCP’s authority fearing potential negative consequences for themselves. To reduce patient concerns about contracting infection at hospitals, it is necessary to cultivate a hospital culture where patients feel comfortable speaking openly about factors that contribute to their fears. Supportive and permissive attitudes of HCPs may encourage patients to ask challenging questions and voice their opinions on safety issues.49,51 Therefore, education programmes should be implemented for both patients and HCPs, with the goal of improving awareness and creating an environment that fosters open communication.
Strength and limitations
Our study explores the impact of patient experiences of patient safety on the fear of infection, extending existing research beyond physical health outcomes. This approach underscores the importance of psychological aspects in patient care, which have often been overlooked in traditional studies focused solely on infection rates and physical health outcomes. However, this study has several limitations. First, while data were collected during the COVID-19 pandemic, its direct external effects were not considered. Given COVID-19’s known influence on infection fear, future research should account for these effects. Second, relying on a single question for infection fear may not comprehensively capture all aspects of the psychological responses related to the fear of infection. Future studies should use validated tools to assess various dimensions of fear. Third, while participants were advised to respond based on their most recent experience within the past year of outpatient utilisation, for those with medical experiences in the more distant past not closely aligned with the data collection period, recall bias may have occurred. Also, it should be noted that the questionnaire used to evaluate patient safety experiences primarily provided binary response options. To improve research quality, adopting more refined methods like Likert scales and validated assessment tools is essential. Lastly, our study was a secondary analysis that only used existing data on patient safety experiences, which primarily focused on injection safety. This is a limitation because in reality, patient safety experiences encompass a broader range of phenomena, including patient participation and facility safety. Future research should consider a wider variety of patient safety experiences.
Conclusion
The findings of the current study suggest that the perceived fear of infection in medical institutions was significantly associated with patients’ experiences of safety in outpatient settings. Among the patients’ safety experiences, HCPs’ hand hygiene and patients’ prior experience of adverse drug reactions were found to have significant impacts. In our study, the most deficient service in patients’ experiences was HCPs’ hand hygiene. These results highlight the importance of HCPs’ proactive behaviour and the need to minimise adverse drug reactions to enhance outpatients’ psychological safety concerning infection.
Policy implications
Given the larger number of unidentified individuals encountered in outpatient settings, it is crucial to ensure that patients receive treatment safely from HCPs. To achieve this, training for HCPs should focus on patient safety practices to ensure that patients feel confident in their care. Particularly, there is a need to expand the dedicated infection control personnel in outpatient services to reinforce proactive behaviour monitoring and education. It is also necessary to minimise adverse treatment experiences, such as adverse drug reactions, as they are associated with higher levels of infection fear based on our findings. To minimise adverse drug reactions, a robust adverse drug reaction reporting system should be implemented, and this information should be shared interprofessionally. This approach will help prevent recurrence and improve patient safety. Additionally, to empower patients to actively participate in managing their health and infection risks, institutional measures that promote patient engagement should be developed and implemented.
Acknowledgements
We express our gratitude to the officials of the Ministry of Health and Welfare and Statistics Korea for providing valuable national survey statistics. We thank the generosity of participants of HSES in sharing their experiences and thoughts. Lastly, we would also like to thank Seonkyu LEE and Sangkyu LEE for their valuable feedback and statistical support.
Footnotes
Funding: None
Prepublication history for this paper is available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2024-083899).
Data availability free text: The data used in the study are available on the Microdata Integration Service at https://mdis.kostat.go.kr. To download the original data, interested parties must first register as a member and then submit a research proposal. We also acquired the HSES data after submitting a research proposal and downloaded after permission from the Microdata Integration Service.
Patient consent for publication: Not applicable.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Ethics approval: The original HSES study obtained ethical approval from the institutional review board of the Korea Institution of Health and Social Affairs. For this secondary analysis, ethical approval was exempted by the Seoul National University Institutional Review Board (IRB No. E2302/004-003).
Contributor Information
Hyunjeong Kwon, Email: opalight58@snu.ac.kr.
Miseon Lee, Email: mslee@pusan.ac.kr.
Data availability statement
Data are available in a public, open access repository.
References
- 1.Institute of Medicine . Crossing the quality chasm: a new healthsystem for the 21st century. National Academy Press; 2001. [Google Scholar]
- 2.Philpot LM, Khokhar BA, DeZutter MA, et al. Creation of a Patient-Centered Journey Map to Improve the Patient Experience: A Mixed Methods Approach. Mayo Clin Proc Innov Qual Outcomes. 2019;3:466–75. doi: 10.1016/j.mayocpiqo.2019.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization Global patient safety action plan 2021-2030: towards eliminating avoidable harm in health care. 2021.
- 4.Lee NJ, Ahn S, Lee M. The effects of a mobile application for patient participation to improve patient safety. Health Expect. 2022;25:1601–18. doi: 10.1111/hex.13503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moynihan R, Sanders S, Michaleff ZA, et al. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open. 2021;11:e045343. doi: 10.1136/bmjopen-2020-045343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Megawati D, Ratri DR, Erzi A. Causes of Decreasing Hospital Visit during the Covid-19 Pandemic. JKB . 2022;31:7–10. doi: 10.21776/ub.jkb.2021.031.02.2s. [DOI] [Google Scholar]
- 7.Raoofi A, Takian A, Haghighi H, et al. COVID-19 and Comparative Health Policy Learning; the Experience of 10 Countries. Arch Iran Med. 2021;24:260–72. doi: 10.34172/aim.2021.37. [DOI] [PubMed] [Google Scholar]
- 8.Almutairi NZ, Almutairi AM, Alduhayshi IS, et al. Impact of COVID-19 Pandemic on the Self-Reported Frequency of Hospital Visits and Pediatric Care Outcomes in the Kingdom of Saudi Arabia. Cureus. 2022;14:e20958. doi: 10.7759/cureus.20958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garrett Jr, JH A Review of the CDC Recommendations for Prevention of HAIs in Outpatient Settings. AORN J. 2015;101:519–28. doi: 10.1016/j.aorn.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 10.Korea Centers for Disease Control and Prevention (KDCA) Healthcare-Associated Infection Management. https://www.kdca.go.kr/contents.es?mid=a20301080100 Available.
- 11.Ministry of Welfare and Health As the COVID-19 spread, the utilization of medical services decreased, and the fear of infection increased. https://www.mohw.go.kr/synap/doc.html?fn=1645626336773_20220223232537.hwp&rs=/upload/result/202311/ Available.
- 12.Ajayi DM, Arigbede AO. Barriers to oral health care utilization in Ibadan, South West Nigeria. Afr Health Sci. 2012;12:507–13. doi: 10.4314/ahs.v12i4.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lau JTF, Yang X, Pang E, et al. SARS-related perceptions in Hong Kong. Emerg Infect Dis . 2005;11:417–24. doi: 10.3201/eid1103.040675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chatterji P, Li Y. Effects of the COVID-19 Pandemic on Outpatient Providers in the United States. Med Care. 2021;59:58–61. doi: 10.1097/MLR.0000000000001448. [DOI] [PubMed] [Google Scholar]
- 15.Zhang J. Hospital Avoidance and Unintended Deaths during the COVID-19 Pandemic. Am J Health Econ. 2021;7:405–26. doi: 10.1086/715158. [DOI] [Google Scholar]
- 16.Cho H, Kwon J. Pandemic and hospital avoidance: Evidence from the 2015 Middle East respiratory syndrome outbreak in South Korea. Econ Lett. 2021;203:109852. doi: 10.1016/j.econlet.2021.109852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lau D, McAlister FA. Implications of the COVID-19 Pandemic for Cardiovascular Disease and Risk-Factor Management. Can J Cardiol. 2021;37:722–32. doi: 10.1016/j.cjca.2020.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American Psychological Association Fear. APA Dictionary of Psychology. 2024. https://dictionary.apa.org/fear Available.
- 19.Loveday H. Fear, explanation and action – the psychosocial response to emerging infections. J Infect Prev. 2020;21:44–6. doi: 10.1177/1757177420911511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Quadros S, Garg S, Ranjan R, et al. Fear of COVID 19 Infection Across Different Cohorts: A Scoping Review. Front Psychiatry. 2021;12:708430. doi: 10.3389/fpsyt.2021.708430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wildavsky A, Dake K. The institutional dynamics of culture, volumes I and II. Routledge; 2018. Theories of risk perception: who fears what and why; pp. 243–62. [Google Scholar]
- 22.Cerda AA, García LY. Factors explaining the fear of being infected with COVID-19. Health Expect. 2022;25:506–12. doi: 10.1111/hex.13274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mertens G, Gerritsen L, Duijndam S, et al. Fear of the coronavirus (COVID-19): Predictors in an online study conducted in March 2020. J Anxiety Disord. 2020;74:S0887-6185(20)30072-4. doi: 10.1016/j.janxdis.2020.102258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ministry of Health and Welfare Data from: 2020 Health Service Experience Survey. MicroData Integrated Service. 2023. https://mdis.kostat.go.kr/ofrData/ Available.
- 25.Shin JW, Cho BH, Choi BR, et al. Health service experience survey. Korea Institute for Health and Social Affairs; 2020. [Google Scholar]
- 26.Kim HN, Choi YS, Moon SJ, et al. Review of Reliability and Validity of Medical Service Experience Survey: Focused on the Differences by Type of Medical Institutions. H P M. 2022;32:94–106. doi: 10.4332/KJHPA.2022.32.1.94. [DOI] [Google Scholar]
- 27.Park J, Im D, Lee D, et al. 2020 regular assessment report for HSES, Statistics Korea, 2020 Nov. Report No.: 11-1240000-001403-14. World Health Organization. Patient safety. 2020. https://www.who.int/news-room/fact-sheets/detail/patient-safety Available.
- 28.World Health Organization Patient safety. https://www.who.int/news-room/fact-sheets/detail/patient-safety n.d. Available.
- 29.Sickbert-Bennett EE, DiBiase LM, Willis TMS, et al. Reduction of Healthcare-Associated Infections by Exceeding High Compliance with Hand Hygiene Practices. Emerg Infect Dis . 2016;22:1628–30. doi: 10.3201/eid2209.151440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Henderson J, Willis E, Blackman I, et al. Comparing infection control and ward nurses’ views of the omission of infection control activities using the Missed Nursing Care Infection Prevention and Control (MNCIPC) Survey. J Nurs Manag. 2021;29:1228–38. doi: 10.1111/jonm.13261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang Y, Yang J, Qiao F, et al. Compared hand hygiene compliance among healthcare providers before and after the COVID-19 pandemic: A rapid review and meta-analysis. Am J Infect Control. 2022;50:563–71. doi: 10.1016/j.ajic.2021.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schwappach DL. Frequency of and predictors for patient-reported medical and medication errors in Switzerland. Swiss Med Wkly. 2011;141:w13262. doi: 10.4414/smw.2011.13262. [DOI] [PubMed] [Google Scholar]
- 33.Alqenae FA, Steinke D, Keers RN. Prevalence and Nature of Medication Errors and Medication-Related Harm Following Discharge from Hospital to Community Settings: A Systematic Review. Drug Saf. 2020;43:517–37. doi: 10.1007/s40264-020-00918-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bulmash B, Ben-Assuli O, Amar M. Fear of Hospital-Acquired Infections: The Combined Impact of Patient’s Hygiene Sensitivity and Perceived Staff Preventive Behavior. J Community Health. 2020;45:1211–9. doi: 10.1007/s10900-020-00857-1. [DOI] [PubMed] [Google Scholar]
- 35.Baek OJ, Shin SH. The Moderating Effect of Patient Safety Knowledge in the Relationship between Patient Experience and Patient Safety Perception for Patients in Primary Care Institutions. Korean J Adult Nurs . 2021;33:387. doi: 10.7475/kjan.2021.33.4.387. [DOI] [Google Scholar]
- 36.Batbaatar E, Dorjdagva J, Luvsannyam A, et al. Determinants of patient satisfaction: a systematic review. Perspect Public Health. 2017;137:89–101. doi: 10.1177/1757913916634136. [DOI] [PubMed] [Google Scholar]
- 37.Harrison R, Walton M, Manias E, et al. The missing evidence: a systematic review of patients’ experiences of adverse events in health care. Int J Qual Health Care. 2015;27:424–42. doi: 10.1093/intqhc/mzv075. [DOI] [PubMed] [Google Scholar]
- 38.Medical Service Act, 47. 2021. https://elaw.klri.re.kr/kor_service/lawView.do?hseq=60889&lang=ENG Available.
- 39.Lee J. The Present and Future of Infection Control Policy in Korea. Korean J Healthc Assoc Infect Control Prev . 2020;25:70–8. doi: 10.14192/kjicp.2020.25.2.70. [DOI] [Google Scholar]
- 40.Le CD, Lehman EB, Nguyen TH, et al. Hand Hygiene Compliance Study at a Large Central Hospital in Vietnam. Int J Environ Res Public Health. 2019;16:607. doi: 10.3390/ijerph16040607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sadule-Rios N, Aguilera G. Nurses’ perceptions of reasons for persistent low rates in hand hygiene compliance. Intensive Crit Care Nurs. 2017;42:17–21. doi: 10.1016/j.iccn.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 42.Irving G, Neves AL, Dambha-Miller H, et al. International variations in primary care physician consultation time: a systematic review of 67 countries. BMJ Open. 2017;7:e017902. doi: 10.1136/bmjopen-2017-017902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lee CH, Lim HS, Kim YN, et al. Analysis of New Patient's Willingness to Pay Additional Costs for Securing Satisfactory Consultation Time. H P M. 2017;27:39–46. doi: 10.432/KJHPA.2017.27.1.39. [DOI] [Google Scholar]
- 44.Kim JH, Jo HS. A Comparative Study on Job Stress and Satisfaction between Ward Nurses and Outpatient Nurses. Korean J Occup Health Nurs. 2013;22:83–92. doi: 10.5807/kjohn.2013.22.2.83. [DOI] [Google Scholar]
- 45.Institute of Medicine (US) Committee on Quality of Health Care in America To Err is Human: Building a Safer Health System. Edited by Linda T. Kohn et. al., National Academies Press (US) 2020. [DOI] [PubMed]
- 46.Lee N-J, Ahn S, Lee M. Mixed-method investigation of health consumers’ perception and experience of participation in patient safety activities. BMJ Open. 2020;10:e035831. doi: 10.1136/bmjopen-2019-035831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Davis RE, Sevdalis N, Vincent CA. Patient involvement in patient safety: How willing are patients to participate? BMJ Qual Saf. 2011;20:108–14. doi: 10.1136/bmjqs.2010.041871. [DOI] [PubMed] [Google Scholar]
- 48.Sharma M. “Can the patient speak?”: postcolonialism and patient involvement in undergraduate and postgraduate medical education. Med Educ. 2018;52:471–9. doi: 10.1111/medu.13501. [DOI] [PubMed] [Google Scholar]
- 49.Davis RE, Koutantji M, Vincent CA. How willing are patients to question healthcare staff on issues related to the quality and safety of their healthcare? An exploratory study. Qual Saf Health Care. 2008;17:90–6. doi: 10.1136/qshc.2007.023754. [DOI] [PubMed] [Google Scholar]
- 50.Leslie JL, Lonneman W. Promoting Trust in the Registered Nurse-Patient Relationship. Home Healthc Now. 2016;34:38–42. doi: 10.1097/NHH.0000000000000322. [DOI] [PubMed] [Google Scholar]
- 51.Oxelmark L, Ulin K, Chaboyer W, et al. Registered Nurses’ experiences of patient participation in hospital care: supporting and hindering factors patient participation in care. Scand J Caring Sci. 2018;32:612–21. doi: 10.1111/scs.12486. [DOI] [PubMed] [Google Scholar]