Abstract
ABSTRACT
Objectives
The widespread adoption of self-testing for SARS-CoV-2 has proven effective in curbing the virus’ spread, particularly in Western countries. However, significant knowledge gaps persist regarding the feasibility, acceptance and factors influencing the uptake of self-testing in low-resource areas, notably rural Africa. Our aim was to assess the willingness and capability of rural Zimbabwean participants to self-diagnose COVID-19 using rapid lateral flow tests (LFTs) and adhere to post-positive test guidelines. Additionally, we aimed to identify barriers to self-testing uptake and reasons for non-compliance with follow-up actions.
Design and setting
We conducted a cross-sectional survey in Shamva District, Zimbabwe.
Participants
A total of 120 villagers aged 18 years and above participated. We employed a questionnaire to gather data on participants' attitudes towards self-testing for SARS-CoV-2 using LFTs, along with their knowledge, attitudes and practices regarding COVID-19. Primary outcomes included the likelihood of self-testing, the ability and accuracy of self-testing, adherence to post-test guidelines and socio-demographic factors influencing these responses.
Results
Among the 120 participants, 108 (90%) expressed willingness to use LFTs for self-testing. The subset unwilling to self-test belonged to a religious sect historically opposed to Western medicine. All self-tests yielded valid results, as confirmed by the appearance of control lines on the LFT. Participants demonstrated the ability to interpret their results accurately without assistance and expressed willingness to adhere to post-test guidelines. Questionnaire responses indicated a preference for self-testing due to its ease, lack of pain, convenience and confidentiality. Moreover, participants exhibited a high level of knowledge about COVID-19.
Conclusion
This study underscores the acceptability and feasibility of SARS-CoV-2 LFT self-testing in rural settings, suggesting its potential as an additional public health measure for epidemics and pandemics in low-resource areas.
Keywords: COVID-19, PUBLIC HEALTH, SARS-CoV-2 Infection
Strengths and limitations of this study.
The study provides comprehensive insights into rural Zimbabwe self-testing feasibility by examining sociodemographic factors alongside COVID-19 self-diagnosis using lateral flow tests.
Social desirability bias may have influenced the reporting of attitudes and practices regarding COVID-19 among survey respondents.
At the time of the study, a considerable portion of the population had already received three doses of the COVID-19 vaccine, which may have impacted their attitudes and behaviours related to testing.
Convenience sampling was used, potentially limiting the generalisability of findings beyond rural Zimbabwe.
Introduction
The COVID-19 pandemic resulted in unprecedented national responses of social distancing and movement restrictions through national lockdowns. In Africa, these restrictions impacted livelihoods,1,4 food security,5,11 access to health services and healthcare12,16 and schooling17,21 derailing progress towards the sustainable development goals.22 The effect of successive lockdowns on Zimbabweans' lives and healthcare has been significant and wide-ranging, including de-prioritisation of non-COVID-19-related healthcare, disrupted education and reduction in household income since a high proportion of Zimbabwe’s workforce is employed in the informal sector.23,26 Due to economic factors, many people were unable to fully comply with the guidelines, which undermined the effects of implemented interventions, resulting in elevated transmission. One possible approach for easing the detrimental impact of lockdowns was 'object-driven'27 COVID-19 testing, which focused on enabling specific actions or goals such as travel or work by requiring individuals to test negative for the virus before participating. This approach helped mitigate the impact of the infection on vulnerable populations and healthcare systems while ensuring that societies and economies could continue to function. Nonetheless, this was not implemented in several countries in Africa, including Zimbabwe in the early stages of the pandemic with the most stringent lockdowns, partly due to lack of evidence on its feasibility.
Object-driven testing was adopted globally, for example, people testing negative for SARS-CoV-2 virus via PCR could travel.28 29 As rapid lateral flow tests (LFTs) became available, these also became useful and acceptable for indicating SARS-CoV-2 status, and these tests are still used today in several countries, for instance, by health workers to protect their patients.30 31
To date, self-testing for various diseases has been successful globally, including in Africa,32,37 with most patients being able to easily perform these tests, obtain accurate results and correctly interpret them.38,41 Thus, self-testing is not a novel concept in low-resource settings, and arguably, SARS-CoV-2 self-testing would have been a useful intervention to reduce the impact of the lockdown responses. The use of LFTs for self-testing allowed the decentralisation of SARS-CoV-2 testing,42 thus relieving the overburdened healthcare centres. The self-tests prevented unnecessary exposure between patients and healthcare staff during sample collection and improved diagnosis access for communities in remote areas.42 Additionally, as LFT results were observed within 30 min after testing, this decreased turnaround times to support improved surveillance.42,44
As indicated earlier, one reason for not implementing SARS-CoV-2 self-testing widely in Africa was the lack of evidence on its feasibility and acceptability. Scientific evidence from several African countries on how home-based SARS-CoV-2 self-testing could be achieved3645,48 is growing. In this study, we aim to add to this evidence base by generating evidence from rural Zimbabwe whose sociocultural factors and dynamics may differ from other African countries.
At the centre of any health intervention using self-testing, is the individual’s willingness and ability to correctly perform the self-test, interpret the result and follow through with appropriate action in the event of a positive result. Hence, in the context of future pandemics, it is important to determine the acceptability and feasibility of lateral flow self-testing and factors affecting these. Therefore, we sought to determine whether participants were willing and able to self-diagnose COVID-19 using LFTs, as well as to follow through with the self-isolation guidelines that were prescribed at the time.
Methodology
Study design, population and site
In July 2022, we conducted a cross-sectional survey of villagers aged >18 years in Mupfure village, Shamva District, Zimbabwe. At this time, a significant portion of the population had already received three courses of the COVID-19 vaccination. Residents in the village were all invited to participate in the study and were enrolled into the study after the aims and procedures of the study were explained to them. A convenient sampling approach was used to select participants.
120 participants were enrolled. The majority of the study participants were affiliated with an Apostolic Faith Christian sect that traditionally shies away from allopathic medical intervention, owing to a belief that illness has a spiritual dimension and that healing is a function of faith.49 This religious affiliation is important to note as it may influence participants' health behaviours and attitudes towards medical interventions, potentially impacting the study’s findings and their interpretation.
The study was conducted in two stages: a questionnaire-based study with 39 questions incorporating knowledge attitudes and practice (KAP) aspect and an observational aspect assessing how participants self-tested. The study was conducted at the local health facility.
Questionnaire on practices pertaining to COVID-19
The study questionnaire was developed in English and translated into Shona, the local language. The initial questionnaire was validated and pre-tested through a preliminary study carried out in Bulawayo, Zimbabwe, with 635 participants. A final version of the questionnaire was developed based on the revisions made from the pre-testing stage.
Quantitative and qualitative information was obtained using fixed-choice and open-ended responses, respectively. Details of the full questionnaire are included in online supplemental material S1. Participants were given the choice to complete the questionnaire in their preferred language, either English or Shona. The questionnaire included participants’ demographics, experiences with COVID-19 and insights into COVID-19-associated behaviours. In addition, acceptability of COVID-19 self-tests and possible actions to be taken after using a COVID-19 self-test were also captured.
Self-testing study design
The self-testing aspect was designed to simulate how lateral flow testing would have been deployed within the existing health structures during the height of the pandemic to reach the largest number of villagers with minimal exposure of health workers to infection. Zimbabwe’s health service delivery is established at four levels: primary, secondary, tertiary and quaternary.50 51 The primary healthcare (PHC) is the main vehicle through which healthcare programmes are implemented in the community in Zimbabwe. It is the first point of contact between the community and the health system. Community health workers including village health workers (VHWs) are an important link between the clinical staff (nurses at the local clinic) and the community. Thus, this study was designed to function at the PHC level involving the local nurse and VHWs.
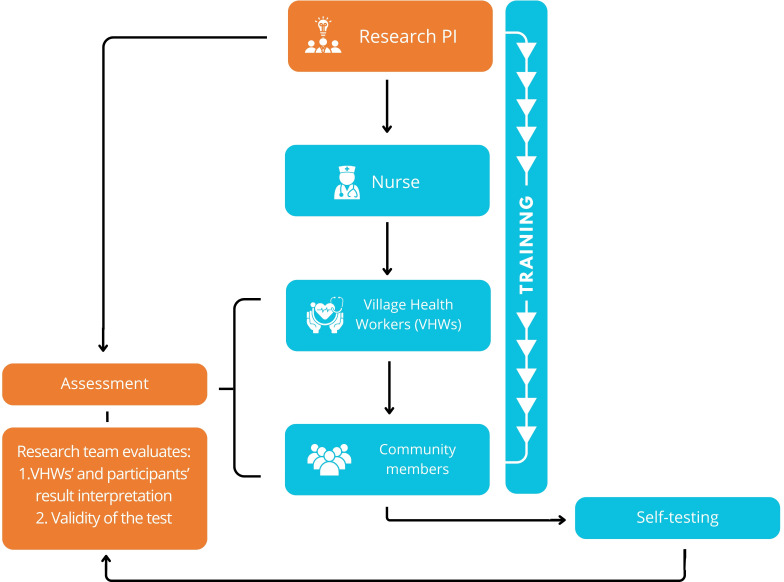
First, the nurse in charge received training from the research team leader on the use of the UNscience SARS-CoV-2 Antigen Rapid Test Kit (Wuhan UNscience Biotechnology Co., Ltd) for self-testing SARS-CoV-2. Subsequently, the trained nurse provided a demonstration to nine VHWs, who in turn demonstrated to the community members. Instructions for the test were conveyed in the local language, Shona, in accordance with the method described in the test’s attached leaflet. Emphasis was placed on promoting good health and safety practices, including the appropriate disposal of the nasopharyngeal swab. The test was observed after developing for 10–15 min, and the significance of both the control and test lines was explained. Following the demonstration, community members independently conducted self-tests in accordance with the provided guidelines. Finally, we conducted an assessment to evaluate VHWs' and participants' interpretation of results as well as the validity of the test. Figure 1 summarises the study design.
Figure 1. Self-testing workflow. The figure summarises the self-testing investigation workflow. Aspects in blue are the current components of the primary healthcare pathway in Zimbabwe’s health system, which were integrated into the study, while aspects related to the research team are highlighted in orange.
To investigate the feasibility and attitudes towards self-testing for COVID-19 using LFTs, we determined the proportion of villagers willing to self-test and follow post-test guidelines. We further investigated the sociodemographic factors affecting these responses using descriptive statistical methods.
Patient and public involvement statement
Our research did not include the participation of patients or the public in its design, conduct, reporting or dissemination plans.
Data analysis
The outcome measures used included categorical data, which were summarised as frequencies and percentages and used in graphic representations or hypothesis testing. Free-text responses from participants were analysed using content analysis. This involved systematically coding and grouping responses into predefined categories based on common themes, which facilitated the identification and categorisation of recurring patterns. This approach ensured that the qualitative data could be quantified and summarised effectively. The sociodemographic characteristics of respondents, responses to survey questions and testing assessment were summarised using routine descriptive statistical methods or analysed through Fisher’s exact test as appropriate conducted with SPSS v. 27. Figures were produced using GraphPad Prism v. 8.2.0.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Results
Participants’ characteristics
There were 120 respondents, comprising 99 (82.5%) females, and 82 (68.3%) of the respondents were subsistence farmers. The mean age of the participants was 42.4 years with an SD of 15.6. In terms of religious affiliation, the Apostolic faith group was the most represented. The characteristics of the participants are shown in table 1.
Table 1. Respondents' sociodemographic characteristics (n=120).
| Demographic characteristics | Category | Frequency | Percentage (%) |
| Sex | Female | 99 | 82.5 |
| Male | 21 | 17.5 | |
| Age | ≤ 20 years | 9 | 7.5 |
| 21–40 years | 52 | 43.3 | |
| 40+ years | 59 | 49.2 | |
| Marital status | Single | 9 | 7.5 |
| Married | 84 | 70 | |
| Divorced | 2 | 1.7 | |
| Widowed | 16 | 13.3 | |
| Declined to respond | 9 | 7.5 | |
| Employment | Subsistence farmer | 82 | 68.3 |
| Healthcare professional | 4 | 3.3 | |
| Home maker | 9 | 7.5 | |
| Student | 5 | 4.2 | |
| Vendor | 6 | 5 | |
| Paid employment | 13 | 10.8 | |
| Unemployed | 1 | 0.8 | |
| Religion | Apostolic | 92 | 76.7 |
| Non-Apostolic | 26 | 21.7 | |
| Non-religious | 2 | 1.7 | |
| Total | 120 | 100 |
Willingness to self-test
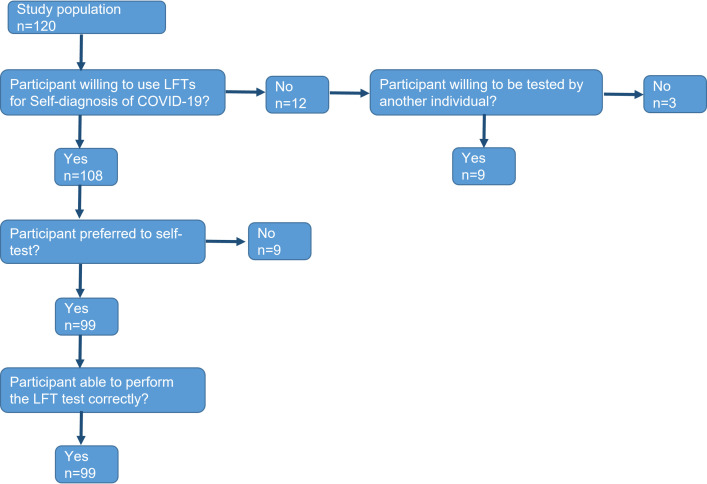
The majority of the participants (90%; n = 108) reported willingness to use LFTs for self-test, and the remaining individuals reported no (10%; n = 12). However, nine of these 12 were willing to be tested by another individual, as summarised in the flow chart in figure 2.
Figure 2. Flowchart depicting willingness and preferences for self-testing.
Factors associated with COVID-19 self-testing willingness
A Fisher’s exact test was employed to ascertain if there was any association between any of the recorded attributes of the study participants and their willingness to self-test (table 2). Among the attributes tested, it was observed that participants with no history of self-testing for other medical conditions were more likely to embrace COVID-19 self-testing compared with those who had previous experience of self-testing for other conditions (p=0.003).
Table 2. Association between participant attributes and willingness to self-test for COVID-19.
| Variable | Total population (n=120) | Willingness to Self-Test | P value | |
| Willing (n=108) | Unwilling (n=12) | |||
| Sex | ||||
| Male | 21 | 17 | 4 | 0.22 |
| Female | 99 | 91 | 8 | |
| Religion | ||||
| Apostolic | 92 | 80 | 12 | 0.066 |
| Other* | 28 | 28 | 0 | |
| Occupation | ||||
| Subsistence Farmer | 82 | 72 | 10 | 0.335 |
| Other† | 38 | 36 | 2 | |
| Tested for COVID-19 | ||||
| Yes | 96 | 88 | 8 | 0.255 |
| No | 24 | 20 | 4 | |
| COVID-19 vaccinated | ||||
| Yes | 116 | 104 | 12 | 1.000 |
| No | 4 | 4 | 0 | |
| Self-tested for other conditions | ||||
| Yes | 33 | 25 | 8 | 0.003 |
| No | 87 | 83 | 4 | |
Other- non-religious and non-Apostolic.
Other- Student, Hhealthcare worker, vendor, homemaker, unemployed.
Self-testing awareness and acceptability
The respondents were asked if they had used rapid tests for any condition prior to this study. About 33% of the study participants mentioned they had conducted rapid tests for one or more of the following conditions: HIV, malaria, hypertension or diabetes. The remaining (67.3%) participants had never self-tested (see online supplemental figure 1) but were aware of available self-tests.
Desirable features of the self-tests
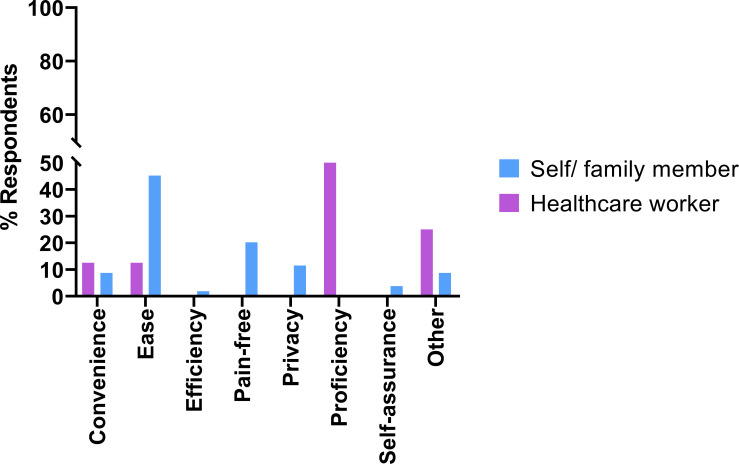
Individual preferences for COVID-19 self-testing and reasons given are presented in figure 3. The majority of the individuals who preferred to self-test stated diverse reasons for their preference. The most common response was on the ease of the test. Most participants also indicated that conducting the test themselves was painless compared with tests performed by others. The few individuals who preferred to be tested by a healthcare professional indicated that their preference for healthcare workers was related to their competence and expertise.
Figure 3. Preferred person to perform COVID-19 test and reasons given.
Barriers to self-testing
The results showed that, despite the availability of free self-test kits, indirect costs, such as transportation to obtain the kits and potential income loss due to isolation after testing positive, were significant barriers to widespread adoption. Additionally, many participants reported attributing common COVID-19 symptoms (eg, fever, sore throat) to other familiar illnesses, which often led to reluctance or a decision not to test.
Cultural and religious factors were also identified as barriers. Some individuals expressed beliefs that illness is spiritually rooted, with healing viewed as a matter of faith, which resulted in a reluctance to engage with Western medical practices, including self-testing.
Correct use of LFT
The correct use of LFTs was assessed by VHWs using a structured approach. Verification included observing proper nasopharyngeal swab technique, ensuring correct timing for reading the test results, appropriate handling of the test device (eg, correct application of the sample onto the test strip) and proper disposal of materials after use.
Overall, among the 108 participants who accepted the use of the SARS-CoV-2 self-tests, all of them (100%) correctly used the LFT as verified by the VHWs and research team, and each test result showed the presence of the control band-verifying the results. Furthermore, they were all able to accurately interpret the results. The one respondent confirmed as SARS-CoV-2 positive was further confirmed as positive by carrying out an additional LFT.
Adherence to post-positive test guidelines
In the case of the one participant who tested positive, the VHW responsible for that participant’s area was promptly notified of the result. The VHW provided instructions for the individual to adhere to the post-positive test guidelines in effect at that time, which included a 5 day isolation period, followed by wearing a mask around others for an additional 5 days. Close contacts, particularly household members, were advised to get tested. However, no formal follow-up was conducted to assess the participant’s compliance with these guidelines.
Discussion
This study sought to understand the acceptability and feasibility of LFTs for self-diagnosing COVID-19 in a low-resource setting in rural Zimbabwe and the KAP around self-testing. Of the 120 participants, 72 (60%) reported that they had experienced several COVID-19-associated symptoms in the previous month and on the day of the survey. Although many participants had carried out measures to mitigate the effects of their symptoms during the previous month either at the clinic or at home, none had undergone SARS-CoV-2 testing. This could be due to multiple reasons, including a lack of testing service or a lack of rapid tests.52 However, a more nuanced explanation may be the reason why someone would test or the motivation for testing. Participants were familiar with testing to diagnose or monitor a disease following the onset of symptoms, for example, fever in malaria. In the context of SAR-CoV-2, LTFs served dual purposes: confirming suspected COVID-19 cases and providing reassurance for asymptomatic individuals who might not be infected by SARS-CoV-2.53 In the case of testing for confirmation infection, barriers to testing were lack of trust in the healthcare system and stigma. In the case of the latter, studies in Africa have indicated that during the early phase of the pandemic, for example, in 2020 people believed a diagnosis was a 'death sentence' and did not want neighbours to know they were infected, ’so they avoided being tested' in Nigeria.54 In the case of the former, a study from Malawi55 reported a higher uptake of testing in the community when the international health organisation offered the test rather than a public clinic, an effect attributed to higher trust in the organisation and/or perceptions of greater capacity to ensure procedural integrity. By the time we conducted this study (July 2022), public opinion had shifted in Zimbabwe with fear subsiding and most people trusting the health system after the roll out of vaccines. This shift may account for the high level of uptake of self-testing we report here.
Beyond these two, barriers to testing uptake is the fact that COVID-19 shares symptoms with other diseases that were endemic to the area. Thus, affected people were inclined to attribute general symptoms such as high temperature and sore throat to other infections. This would likely be the case in this community where, like most of Africa, COVID-19 pathology presented with low severity.56 57 This has been previously observed in other settings, where members of the public were only inclined to request testing for more distinguishable COVID-19 symptoms, such as loss of taste and smell.58 59 This is exacerbated by poor knowledge of COVID-19 symptoms.60
Nonetheless, similar to other previous studies,61 62 most participants reported that they were willing to self-test and expressed enthusiasm about the introduction of LFTs for personal use for various reasons, including that they were straightforward, pain-free, confidential and convenient. They also reported that the teaching of the testing process and knowing one’s status promoted awareness of COVID-19 emphasising the importance of health education and health messaging. These findings are supported by previous studies highlighting some of the drivers of self-testing for other diseases, such as HIV.63 64
Many study participants preferred self-testing because it was relatively painless compared with previously taken COVID-19 tests. Convenience was an important factor in the willingness to accept self-testing, with some participants citing the time-saving aspect as a major influence for personal uptake. This addresses a current limitation where test-seeking members of the community are compelled to spend extended periods of time travelling to a clinic, testing and, in some cases, returning later for results. This factor has a causal relationship to affordability, where patients may have to forgo employment to access these services when available. This has been previously demonstrated with HIV testing in Zimbabwe, where real-time income loss and inconvenient location were prohibitive to testing uptake.65
The importance of confidentiality was apparent in individuals who favoured self-testing. Studies on attitudes to HIV testing have reflected that individuals attending testing units or medical centres feared stigmatisation as they are seen as at risk of the disease.65 As self-testing can be conducted in the privacy of one’s home, patients avoid the necessity of interfacing with these facilities, eliminating the effect of stigma in seeking diagnosis.
A minority of participants did not favour self-testing with rapid COVID-19 diagnostics. Notably, these individuals were all affiliated with an Apostolic Faith Christian sect which, as mentioned earlier, traditionally avoids allopathic medical intervention.49 However, this might have been a subgroup since most of the participants in this study belonged to that sect and were happy to self-test. Although they were unwilling to self-test, this group was shown to be largely receptive to testing in general, with a significant number expressing satisfaction with testing carried out by healthcare workers. Pre-established trust of healthcare personnel was revealed to be important as some individuals were still concerned with the result accuracy when conducting self-testing. These community members were reassured when offered the choice to have a healthcare worker perform the test, thereby increasing the overall number of participants willing to either carry out their personal LFTs or be subjected to the test by a professional.
By integrating the self-testing into already existent health systems structures such as training of the participants by the VHWs who were themselves trained by the nurse we were able to demonstrate that it is feasible to integrate LFT for SARS-CoV-2 within the health system. Furthermore, we confirmed that this approach resulted in the participants testing themselves and interpreting the results correctly and the following through with the appropriate action.
Self-testing has been demonstrated to be not only possible, as shown by one’s ability to complete a rapid test, but also preferred by the study community, even increasing the likelihood and frequency of testing. This provides a promising adjunct to centralised testing, potentially enabling prompt and effective management of life-threatening infectious outbreaks66 among those living in remote segregated areas. Moreover, the high acceptability of self-testing in this study population suggests that facilitating its easy access to the general public, including those in remote areas, may help increase the country’s testing rates.
Limitations
This study had some limitations introduced likely by social desirability bias, which is the inclination of survey participants to respond with answers that would be observed positively by the study investigators.67 This may have affected questions about COVID-19-associated behaviours, where respondents may answer questions following the stated health advice and previously enforced laws. This likely impacted questions such as mouth-covering while coughing and hand-washing practices. In addition, it may have influenced the reported responses to COVID-19 symptoms, driving individuals to relay increased frequency interfacing with the health system. Moreover, the use of convenience sampling may have introduced the selection bias, as participants who voluntarily enrolled in the study may have been more inclined towards testing or already more health conscious, making them less representative of the general population. Additionally, this study was conducted during a period of relatively low SARS-CoV-2 prevalence. The low number of positive cases made it difficult to comprehensively assess adherence to post-positive test guidelines.
Strengths
Despite using an opportunistic sample from a singular village, the study village is similar to other villages within the Mashonaland provinces of Zimbabwe, rendering it broadly representative of the rural populations in these areas. The study’s focus on a rural, resource-limited area, demonstrates the feasibility of implementing self-testing in environments where healthcare infrastructure is often inadequate. The successful adoption of self-testing in this context contributes to broader public health strategies, empowering communities to play an active role in managing infectious diseases. This could alleviate the burden on overstrained healthcare systems in similar regions. Additionally, this study lays important groundwork for future studies, providing valuable data that can help refine self-testing protocols and assess their long-term sustainability and effectiveness, both for COVID-19 and other health conditions requiring rapid diagnostics.
Conclusion
Our study findings mirror those of previous studies from other African countries, revealing that self-testing using lateral-flow methods is not only logistically feasible but also widely preferred by individuals over centralised testing conducted by healthcare professionals. Moreover, our study results indicate that most participants could perform the tests and correctly interpret the results independently of healthcare personnel. These findings underscore the value of lateral flow self-tests as a widely accepted public health tool that can be deployed for future epidemics and pandemics in low-resource settings. This diagnostic approach should be considered more widely to enhance diagnostic accessibility in low-resource settings, circumventing healthcare bottlenecks and improving diagnostic access in low-resource settings.
supplementary material
Acknowledgements
We thank the village health workers for their help with the fieldwork. Special thanks are due to the study participants. We also thank members all the members of the Parasite Immuno-epidemiology Group (at the University of Edinburgh for their helpful comments in shaping this manuscript. We would also like to thank Grace Zdesenko and Ciara Sawey for their help during the fieldwork for data collection.
Footnotes
Funding: FM, TM and LTP are funded by a Royal Society Grant (Ica/R1/201399). The funders had no role in the conception, study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2024-085391).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Ethics approval: This study involves human participants and was approved by Medical Research Council of Zimbabwe (MRCZ/A/2770) Participants gave informed consent to participate in the study before taking part.
Permission to conduct the study in the area (Shamva District) was sought from the Provincial Medical Director. The study aims and procedures were fully explained to village heads and all participants in their local language (Shona) before obtaining their verbal consent. Participation was voluntary, and participants were free to withdraw from the study at any stage.
Patient and public involvement: Patients and/or the public were not involved in the design, conduct, reporting or dissemination plans of this research.
Contributor Information
Lorraine Tsitsi Pfavayi, Email: lpfavayi@ed.ac.uk.
Emilia Choto, Email: emiliachoto@gmail.com.
Paradzayi Tagwireyi, Email: tagwireyip@gmail.com.
Takafira Mduluza, Email: taka.mduluza@gmail.com.
Francisca Mutapi, Email: f.mutapi@ed.ac.uk.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1.Paci P. How livelihoods deteriorated in Sub-Saharan Africa due to covid-19. World Bank: Africa Can End Poverty. 2021. https://blogs.worldbank.org/africacan/how-livelihoods-deteriorated-sub-saharan-africa-due-covid-19 Available.
- 2.Asegie AM, Adisalem ST, Eshetu AA. The effects of COVID-19 on livelihoods of rural households: South Wollo and Oromia Zones, Ethiopia. Heliyon. 2021;7:e08550. doi: 10.1016/j.heliyon.2021.e08550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Braam DH, Srinivasan S, Church L, et al. Lockdowns, lives and livelihoods: the impact of COVID-19 and public health responses to conflict affected populations - a remote qualitative study in Baidoa and Mogadishu, Somalia. Confl Health. 2021;15:47. doi: 10.1186/s13031-021-00382-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schotte S, Zizzamia R. The livelihood impacts of COVID-19 in urban South Africa: a view from below. Soc Indic Res. 2023;165:1–30. doi: 10.1007/s11205-022-02978-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Groot J, Lemanski C. COVID-19 responses: infrastructure inequality and privileged capacity to transform everyday life in South Africa. Environ Urban. 2021;33:255–72. doi: 10.1177/0956247820970094. [DOI] [Google Scholar]
- 6.Amusan L, Agunyai SC. The COVID-19 pandemic and the crisis of lockdowns in Nigeria: The household food security perspective. Afr Public Serv Deliv Perform Rev. 2021;9:10. doi: 10.4102/apsdpr.v9i1.484. [DOI] [Google Scholar]
- 7.Ngarava S. Empirical analysis on the impact of the COVID-19 pandemic on food insecurity in South Africa. Phys Chem Earth, Parts A/B/C. 2022;127:103180. doi: 10.1016/j.pce.2022.103180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Economics Observatory How is coronavirus affecting food security in sub-saharan Africa. 2020
- 9.Balana BB, Ogunniyi A, Oyeyemi M, et al. COVID-19, food insecurity and dietary diversity of households: Survey evidence from Nigeria. Food Secur. 2023;15:219–41. doi: 10.1007/s12571-022-01312-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abdul IM. COVID-19, LOCKDOWN AND TRANSITORY FOOD INSECURITY IN NIGERIA. Foodagrmanag. 2020;1:26–30. doi: 10.26480/fabm.01.2020.26.30. [DOI] [Google Scholar]
- 11.Ayanlade A, Radeny M. COVID-19 and food security in Sub-Saharan Africa: implications of lockdown during agricultural planting seasons. NPJ Sci Food. 2020;4:13. doi: 10.1038/s41538-020-00073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fayehun F, Harris B, Griffiths F, et al. COVID-19: how lockdowns affected health access in African and Asian slums. 2020. https://theconversation.com/covid-19-how-lockdowns-affected-health-access-in-african-and-asian-slums-147600 Available.
- 13.Tessema GA, Kinfu Y, Dachew BA, et al. The COVID-19 pandemic and healthcare systems in Africa: a scoping review of preparedness, impact and response. BMJ Glob Health. 2021;6:e007179. doi: 10.1136/bmjgh-2021-007179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Musoke D, Nalinya S, Lubega GB, et al. The effects of COVID-19 lockdown measures on health and healthcare services in Uganda. PLOS Glob Public Health . 2023;3:e0001494. doi: 10.1371/journal.pgph.0001494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van Staden Q, Laurenzi CA, Toska E. Two years after lockdown: reviewing the effects of COVID-19 on health services and support for adolescents living with HIV in South Africa. J Int AIDS Soc. 2022;25:e25904. doi: 10.1002/jia2.25904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arsenault C, Gage A, Kim MK, et al. COVID-19 and resilience of healthcare systems in ten countries. Nat Med. 2022;28:1314–24. doi: 10.1038/s41591-022-01750-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Okebukola PA, Suwadu B, Oladejo A, et al. Delivering High School Chemistry During COVID-19 Lockdown: Voices from Africa. J Chem Educ. 2020;97:3285–9. doi: 10.1021/acs.jchemed.0c00725. [DOI] [Google Scholar]
- 18.Zar HJ, Dawa J, Fischer GB, et al. Challenges of COVID-19 in children in low- and middle-income countries. Paediatr Respir Rev. 2020;35:70–4. doi: 10.1016/j.prrv.2020.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Duby Z, Jonas K, Bunce B, et al. Navigating Education in the Context of COVID-19 Lockdowns and School Closures: Challenges and Resilience Among Adolescent Girls and Young Women in South Africa. Front Educ. 2022;7 doi: 10.3389/feduc.2022.856610. [DOI] [Google Scholar]
- 20.Spaull N, Van der Berg S. Counting the cost: COVID-19 school closures in South Africa and its impact on children. SAJCE . 2020;10 doi: 10.4102/sajce.v10i1.924. [DOI] [Google Scholar]
- 21.Oppong Asante K, Quarshie E-B, Andoh-Arthur J. COVID-19 school closure and adolescent mental health in sub-Saharan Africa. Int J Soc Psychiatry. 2021;67:958–60. doi: 10.1177/0020764020973684. [DOI] [PubMed] [Google Scholar]
- 22.Min Y. How COVID-19 has impacted the SDGs in Africa. 2021. [23-May-2023]. https://www.un.org/africarenewal/magazine/august-2021/how-covid-19-has-impacted-sdgs-africa Available. Accessed.
- 23.Matsungo TM, Chopera P. Effect of the COVID-19-induced lockdown on nutrition, health and lifestyle patterns among adults in Zimbabwe. BMJ Nutr Prev Health . 2020;3:205–12. doi: 10.1136/bmjnph-2020-000124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hunter J, Chitsiku S, Shand W, et al. Learning on Harare’s streets under COVID-19 lockdown: making a story map with street youth. Environ Urban. 2021;33:31–42. doi: 10.1177/0956247820979440. [DOI] [Google Scholar]
- 25.Mavhandu-Mudzusi AH, Moyo I. How do you expect us to survive? Lamentation of female sex workers in Zimbabwe during COVID-19 lockdown. Afr J Reprod Health. 2022;26:104–13. doi: 10.29063/ajrh2022/v26i3.12. [DOI] [PubMed] [Google Scholar]
- 26.Price R. Impacts of COVID-19 regulatory measures on small-scale and informal trade in Zimbabwe. 2020
- 27.European Centre for Disease Prevention and Control . Stockholm:: European Centre for Disease Prevention and Control; 2020. COVID-19 testing strategies and objectives; p. 22. [Google Scholar]
- 28.Chung S-C, Marlow S, Tobias N, et al. Lessons from countries implementing find, test, trace, isolation and support policies in the rapid response of the COVID-19 pandemic: a systematic review. BMJ Open. 2021;11:e047832. doi: 10.1136/bmjopen-2020-047832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.European Centre for Disease Prevention and Control and European Union Aviation Safety Agency Addendum to the Aviation Health Safety Protocol. Guidelines for COVID-19 testing and quarantine of air travellers. 2020. [25-May-2023]. https://www.ecdc.europa.eu/sites/default/files/documents/Guidelines_for_COVID-19_testing_and_quarantine_of_air_travellers-12-2020.pdf Available. Accessed.
- 30.UK Health Security Agency Coronavirus (COVID-19) testing for anyone working in adult social care who is not part of regular testing at work United Kingdom. [25-May-2023]. https://www.gov.uk/guidance/coronavirus-covid-19-testing-for-personal-assistants Available. Accessed.
- 31.Remoe V. Community health workers: the unsung heroes in Africa’s COVID-19 response. 2021. [25-May-2023]. https://www.un.org/africarenewal/magazine/january-2021/unsung-heroes-africa%E2%80%99s-covid-19-response Available. Accessed.
- 32.Dallera G, Alaa A, El-Osta A, et al. Evaluating the feasibility and acceptability of a safety protocol to mitigate SARS-CoV-2 transmission risks when participating in full-capacity live mass events: a cross-sectional survey and interview-based study. BMJ Open. 2022;12:e063838. doi: 10.1136/bmjopen-2022-063838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.O’Farrell B. Evolution in lateral flow–based immunoassay systems. Lat flow immunoassay. 2009:1–33. doi: 10.1007/978-1-59745-240-3_1. [DOI] [Google Scholar]
- 34.Hoehl S, Schenk B, Rudych O, et al. High-Frequency Self-Testing by Schoolteachers for Sars-Cov-2 Using a Rapid Antigen Test–Results of the Safe School Hesse study. Dtsch Arztebl Int. 2021;118:252–3. doi: 10.3238/arztebl.m2021.0187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lindner AK, Nikolai O, Rohardt C, et al. Diagnostic accuracy and feasibility of patient self-testing with a SARS-CoV-2 antigen-detecting rapid test. J Clin Virol. 2021;141:104874. doi: 10.1016/j.jcv.2021.104874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Folayan M, Shilton S, Undelikwo V, et al. People’s willingness to use COVID-19 self-testing in Nigeria: a cross-sectional survey. BMJ Open. 2023;13:e063323. doi: 10.1136/bmjopen-2022-063323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Janssen R, Engel N, Esmail A, et al. Alone But Supported: A Qualitative Study of an HIV Self-testing App in an Observational Cohort Study in South Africa. AIDS Behav. 2020;24:467–74. doi: 10.1007/s10461-019-02516-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ibitoye M, Frasca T, Giguere R, et al. Home Testing Past, Present and Future: Lessons Learned and Implications for HIV Home Tests. AIDS Behav. 2014;18:933–49. doi: 10.1007/s10461-013-0668-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Figueroa C, Johnson C, Ford N, et al. Reliability of HIV rapid diagnostic tests for self-testing compared with testing by health-care workers: a systematic review and meta-analysis. Lancet HIV. 2018;5:e277–90. doi: 10.1016/S2352-3018(18)30044-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tidy EJ, Shine B, Oke J, et al. Home self-testing kits: helpful or harmful? Br J Gen Pract. 2018;68:360–1. doi: 10.3399/bjgp18X698021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Atchison C, Pristerà P, Cooper E, et al. Usability and Acceptability of Home-based Self-testing for Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Antibodies for Population Surveillance. Clin Infect Dis. 2021;72:e384–93. doi: 10.1093/cid/ciaa1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mackworth-Young CR, Chingono R, Mavodza C, et al. Community perspectives on the COVID-19 response, Zimbabwe. Bull World Health Organ. 2021;99:85–91. doi: 10.2471/BLT.20.260224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mina MJ, Parker R, Larremore DB. Rethinking Covid-19 Test Sensitivity - A Strategy for Containment. N Engl J Med. 2020;383:e120. doi: 10.1056/NEJMp2025631. [DOI] [PubMed] [Google Scholar]
- 44.Alemany A, Baró B, Ouchi D, et al. Analytical and clinical performance of the panbio COVID-19 antigen-detecting rapid diagnostic test. J Infect. 2021;82:186–230. doi: 10.1016/j.jinf.2020.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brumwell AN, Babatunde GB, Shilton S, et al. Self-testing for COVID-19 in Durban and Eastern Cape, South Africa: a qualitative inquiry targeting decision-takers. Contemp Soc Sci. 2022;17:450–67. doi: 10.1080/21582041.2022.2147986. [DOI] [Google Scholar]
- 46.Nwaozuru U, Obiezu-Umeh C, Diallo H, et al. Perceptions of COVID-19 self-testing and recommendations for implementation and scale-up among Black/African Americans: implications for the COVID-19 STEP project. BMC Public Health. 2022;22:1220. doi: 10.1186/s12889-022-13619-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brumwell AN, Babatunde GB, Wilson MW, et al. Values of COVID-19 Self-Testing among Urban and Rural South Africans: A Cross-Sectional Survey. Prev Med Rep. 2023;32:102114. doi: 10.1016/j.pmedr.2023.102114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Manguro G, Shilton S, Omenda S, et al. Are Kenyans Likely to Use COVID-19 Self-Testing Kits? Results From a Cross-Sectional Survey. Int J Public Health. 2022;67:1604918. doi: 10.3389/ijph.2022.1604918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mpofu E, Dune TM, Hallfors DD, et al. Apostolic faith church organization contexts for health and wellbeing in women and children. Ethn Health. 2011;16:551–66. doi: 10.1080/13557858.2011.583639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Matsena Zingoni Z, Chirwa T, Todd J, et al. Competing risk of mortality on loss to follow-up outcome among patients with HIV on ART: a retrospective cohort study from the Zimbabwe national ART programme. BMJ Open. 2020;10:e036136. doi: 10.1136/bmjopen-2019-036136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mugabe VA, Ali S, Chelene I, et al. Evidence for chikungunya and dengue transmission in Quelimane, Mozambique: Results from an investigation of a potential outbreak of chikungunya virus. PLoS One. 2018;13:e0192110. doi: 10.1371/journal.pone.0192110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Embrett M, Sim SM, Caldwell HAT, et al. Barriers to and strategies to address COVID-19 testing hesitancy: a rapid scoping review. BMC Public Health. 2022;22:750. doi: 10.1186/s12889-022-13127-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mathers J, Poyner C, Thompson D, et al. Exploration of the uptake of asymptomatic COVID-19 lateral flow testing in Birmingham, UK: survey and qualitative research. BMJ Open. 2022;12:e056606. doi: 10.1136/bmjopen-2021-056606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Maclean R. Covid-19 outbreak in Nigeria is just one of Africa’s alarming hot spots. The New York Times. 2020. https://www.nytimes.com/2020/05/17/world/africa/coronavirus-kano-nigeria-hotspot.html Available.
- 55.Ferree KE, Harris AS, Dulani B, et al. Stigma, Trust, and procedural integrity: Covid-19 testing in Malawi. World Dev. 2021;141:105351. doi: 10.1016/j.worlddev.2020.105351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fonte L, Acosta A, Sarmiento ME, et al. COVID-19 lethality in Sub-Saharan Africa and helminth immune modulation. Front Immunol. 2020;11:574910. doi: 10.3389/fimmu.2020.574910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Osei SA, Biney RP, Anning AS, et al. Low incidence of COVID-19 case severity and mortality in Africa; Could malaria co-infection provide the missing link? BMC Infect Dis. 2022;22:78. doi: 10.1186/s12879-022-07064-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fabella FE. Factors Affecting Willingness to be Tested for COVID-19. SSRN J. 2020 doi: 10.2139/ssrn.3670514. [DOI] [Google Scholar]
- 59.Khalifa AM, Alshammari AF, Alrimali AM, et al. Willingness to Test for COVID-19: A Cross-Sectional Study on the Population in the Ha’il Region, KSA. JPRI. 2021;33:44–53. doi: 10.9734/jpri/2021/v33i1331265. [DOI] [Google Scholar]
- 60.Smith LE, Potts HWW, Amlôt R, et al. Adherence to the test, trace, and isolate system in the UK: results from 37 nationally representative surveys. BMJ. 2021;372:n608. doi: 10.1136/bmj.n608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wanat M, Logan M, Hirst JA, et al. Perceptions on undertaking regular asymptomatic self-testing for COVID-19 using lateral flow tests: a qualitative study of university students and staff. BMJ Open. 2021;11:e053850. doi: 10.1136/bmjopen-2021-053850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nguyen N, Lane B, Lee S, et al. A mixed methods study evaluating acceptability of a daily COVID-19 testing regimen with a mobile-app connected, at-home, rapid antigen test: Implications for current and future pandemics. PLoS ONE. 2022;17:e0267766. doi: 10.1371/journal.pone.0267766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mathews A, Farley S, Conserve DF, et al. “Meet people where they are”: a qualitative study of community barriers and facilitators to HIV testing and HIV self-testing among African Americans in urban and rural areas in North Carolina. BMC Public Health. 2020;20:1–10. doi: 10.1186/s12889-020-08582-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Steehler K, Siegler AJ. Bringing HIV Self-Testing to Scale in the United States: a Review of Challenges, Potential Solutions, and Future Opportunities. J Clin Microbiol. 2019;57:e00257-19. doi: 10.1128/JCM.00257-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Morin SF, Khumalo-Sakutukwa G, Charlebois ED, et al. Removing barriers to knowing HIV status: same-day mobile HIV testing in Zimbabwe. J Acquir Immune Defic Syndr. 2006;41:218–24. doi: 10.1097/01.qai.0000179455.01068.ab. [DOI] [PubMed] [Google Scholar]
- 66.Sievers BL, Klotzle J, Khan TV. Evaluation of feasibility and user acceptance of lateral-flow self-testing for viral illness in a residential treatment rehabilitation facility. Health Justice . 2022;10:10. doi: 10.1186/s40352-022-00173-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zerbe WJ, Paulhus DL. Socially Desirable Responding in Organizational Behavior: A Reconception. Acad Manag Rev. 1987;12:250. doi: 10.2307/258533. [DOI] [Google Scholar]