Abstract
Background/Objectives: Acne is the most prevalent dermatological condition among humans, affecting approximately 80% of adolescents during puberty. To date, numerous compounds have been used for acne treatment, including erythromycin ointments and antiseptics, with varying degrees of success. The emergence of erythromycin-resistant C. acnes strains has spurred the search for new antimicrobial agents, particularly from natural sources. Methods: Propolis collected in Rwanda was extracted and fractionated by flash chromatography and tested against C. acnes growth by using NCLSI recommendations. Results: In our research, we identified a molecule, 2,4-Di-tert-butylphenol (2,4-DTBP) which inhivbited the C. acnes growth at a concentration of 16 µg/mL. Based on these results, we formulated an ointment (1%) using OFAP18 and petroleum jelly for the potential treatment of acne using a mouse model. Conclusions: In vitro and in vivo evidence suggests that 2,4-DTBP has anti-inflammatory properties and could effectively manage the overgrowth of C. acnes as well as serve as a potent alternative for the formulation of an active propolis ointment for acne treatment.
Keywords: acne; antibacterial activity; Cutibacterium acnes; 2,4-Di-tert-butylphenol; ointment; propolis
1. Introduction
Acne stands out as the prevailing dermatological condition among humans, primarily affecting approximately 80% of adolescents during the onset of puberty, a period marked by hormonal fluctuations that are uniform across genders. While acne typically diminishes as individuals enter their twenties, it persists in 54% of women and 40% of men in adulthood. The development of acne is closely linked to the distribution of sebaceous glands, primarily appearing on the face, jawline (especially in adults), neck, chest, and back [1]. It presents in various forms, including whiteheads, blackheads, and differing levels of inflamed lesions [2]. Antibiotics play a pivotal role in restraining bacterial growth, with oral antibiotics serving as the primary treatment for moderate acne or instances where topical combinations prove intolerable or ineffective. Notably, systemic erythromycin and various generations of tetracyclines have demonstrated efficacy in addressing inflammatory acne. However, the prolonged use of topical and oral antibiotics against C. acnes has led to a prevalent emergence of resistance, particularly in European Union countries [3,4,5]. Spanish researchers, for instance, reported resistance rates of 91% and 92.4% for both kinds of antibiotics in Spain, while Greece and Italy recorded resistance rates of 75.3% and 59.5%, respectively [6]. The escalating prevalence of drug-resistant C. acnes strains globally has prompted widespread concern about the diminishing arsenal of antibiotics available for treating this common ailment [7,8,9].
Propolis, a resinous substance crafted by honeybees, boasts a rich history in traditional medicine spanning millennia. Etymologically rooted in ancient Greek, the term “propolis” combines ‘pro’ (in front of) and ‘polis’ (city), literally translating to ‘defense of the city’ [10]. This aptly reflects how bees utilize propolis to safeguard their hive from diseases caused by fungi, bacteria, and predators [11]. Derived from tree buds and bark, propolis, with its sticky and gummy consistency, results from the collection of resins by foraging bees, creating a blend with pollen, waxes, and enzymes [12,13]. The exact composition varies based on honeybee species, plant source, harvesting seasons, and climate changes. Propolis has demonstrated a spectrum of clinical applications, including antioxidant, anticancer, anti-inflammatory, and antimicrobial effects [14,15,16,17,18,19,20,21]. Notably, recent findings highlight propolis as a natural remedy for skin issues, thanks to its soothing and healing properties [22].
Nonetheless, it is crucial to recognize that propolis is not a singular entity; rather, its variations depend on the surrounding flora, and not all types will necessarily exhibit the same efficacy in addressing a particular pathology.
In the pursuit of discovering potent antimicrobial molecules, our studies have delved into exploring the potentialities of different propolis samples collected in Rwanda, a region marked by the presence of one of the last remaining primary forests in the world. Our aim is to identify novel molecules of interest to advance antimicrobial research, specifically for developing a potent alternative for formulating an active propolis-based ointment for acne treatment.
2. Materials and Methods
2.1. Reagents
All solvents and reagents used were commercially available. Dichloromethane, methanol, ethyl acetate, and petroleum ether were purchased from VWR and used without further purification. Column chromatography was performed on Macherey Nagel silica gel (70–230 mesh) using a COMBIFLASH device. The 1H and 13C NMR spectra were recorded in CDCl3 on a 300 and 75 MHz Bruker AC 300 spectrometer, respectively (the usual abbreviations are used: s: singlet, d: doublet, t: triplet, q: quadruplet, m: multiplet). All chemical displacements are indicated in ppm. The analysis by mass spectroscopy was carried out by the laboratory of analysis of the faculty of pharmacy (University of Aix-Marseille).
2.2. Preparation of the Hydroalcoholic Extract of OFAP18
OFAP18 was collected in Rwanda at a precise place located at the GPS coordinates 2°26′53.0″ S 29°04′07.0″ E, in the form of a black gum. Briefly, 9.0 g of propolis OFAP18 was extracted with 15 mL of ethanol (water–ethanol (30:70, v/v)) by using a Biotage initiator microwave apparatus operating for 10 min at 100 °C and 2 bars. After centrifugation and filtration, this led to an ethanol extract of which the propolis concentration was determined to be 120 mg/mL and was subsequently used for biological tests and flash chromatography (from non-polar to polar, namely petroleum ether, ethyl acetate, and methanol).
2.3. Fractionation of Propolis OFAP18
Briefly, 9.0 g of propolis OFAP18 was extracted with ethanol (water–ethanol (30:70, v/v) leading to an ethanol extract which was concentrated under vacuum to a crude powder (1.8 g) and subsequently submitted for flash chromatography (from non-polar to polar namely petroleum ether, ethyl acetate, and methanol) yielding 73 fractions of 20 mL which were grouped into 11 fractions titled F1 to F11
2.4. Bacterial Strains
The bacterial strains tested were E. coli ATCC25922, B. cereus ATCC11778, S. aureus ATCC25923, S. epidermidis CIP81.55, and C. acnes DSM1897, CIP110516, CIP110517, CIP110528, and CIPA179. All bacterial experiments were performed according to CLSI M11 Methods for Antimicrobial Susceptibility Testing of Anaerobic Bacteria, 9th Edition and CLSI M07_Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically, 12th Edition.
2.5. General Procedure for Measuring Antimicrobial Activities
The antibacterial activity of the compounds was measured using a standard microdilution test based on Clinical and Laboratory Standards Institute (CLSI) guidelines. This method was slightly modified to improve reproducibility. The final volume remains 200 µL, now consisting of 190 µL of bacterial suspension and 10 µL of the test molecule solution.
The bacteria were handled under a hood in the L2 laboratory. The chemical compounds (2,4-Di-tert-butylphenol, 3,5-Di-tert-butylphenol, 2,6-Di-tert-butylphenol) and propolis extracts to be tested were prepared in 70% ethanol at a concentration of 10 mg/mL.
2.5.1. Culture Preparation
An inoculum was prepared by resuspending a grown colony (1 to 7 days) of each strain in a culture tube containing 5 mL of Brain Heart Infusion (BHI) medium then incubated at 37 °C for 16 to 18 h under agitation at 100 rpm. Similar experimental conditions are involved for C. acnes but under an anaerobic atmosphere (GENbag anaer—Biomérieux®, Paris, France) and during a 30 to 36 h incubation.
2.5.2. Preparation of Precultures
Each laboratory strain has an established OD-to-CFU ratio. To determine this ratio, all strains were cultured until reaching the exponential growth phase. The optical density (OD) of each bacterial suspension was measured, followed by bacterial enumeration on solid media. This ratio enables the precise calculation of the required dilution, ensuring the appropriate bacterial concentration for Minimum Inhibitory Concentration (MIC) tests. All the experiments were performed according to CLSI guidelines. Typically, the precultures were prepared by adding 20 µL of overnight E. coli ATCC25922 culture, 50 µL of B. cereus ATCC11778, or 100 µL of S. aureus ATCC25923 and S. epidermidis CIP81.55, each into 3 mL of fresh BHI. The tubes were then incubated at 37 °C for 3–4 h at 100 rpm. Due to the slower growth rate of C. acnes, a previously prepared culture was used directly for microplate preparation.
2.5.3. Preparation of Test Solutions
The diluted molecules (2,4-DTBP, 2,6-DTPB, and 3,5-DTPB) (in 70% ethanol) or the hydroalcoholic extract of propolis samples (OFAP2-21) underwent a two-fold serial dilution, beginning with 70% ethanol for the first two dilutions, followed by dilution in water. Working solutions with concentrations ranging from 5000 to 80 µg/mL (corresponding to ethanol percentages of 70% to 2.2%) were prepared, resulting in final concentrations in the microplate wells from 250 to 4 µg/mL (3.5% to 0.1% ethanol).
2.5.4. Preparation of Microplate for Determination of MIC
The optical density at 600 nm (OD600) of each bacterial suspension was measured and then diluted to achieve a target OD600 (0.0009 for E. coli, 0.001 for B. cereus, 0.0012 for S. aureus and S. epidermidis, and 0.0013 for C. acnes), corresponding to a bacterial density of 5 × 105 CFU/mL as previously determined in our laboratory. For example, an OD600 of 0.5 corresponds to a concentration of 2.1 × 108 CFU/mL for S. aureus. Therefore, if this suspension is diluted 417-fold to an equivalent OD of 0.0012 (used solely for calculation purposes and not directly measured), a final bacterial concentration of 5 × 105 CFU/mL is obtained. In a flat-bottom, translucent 96-well plate, 10 µL of each working solution—within the dilution range of propolis extract or tested molecules (2,4-DTBP, 2,6-DTPB, and 3,5-DTPB)—was added to 190 µL of the bacterial suspension, adjusted to 5 × 105 CFU/mL. This resulted in final concentration ranges of 250 to 4 µg/mL, with final ethanol concentrations ranging from 3.2% to 0.1%
The control wells were carried out with the following parameters:
-
-
Growth control containing 200 µL bacterial suspension at 5.105 CFU/mL.
-
-
Contamination control containing 200 µL of medium BHI.
-
-
Control growth in the presence of ethanol, corresponding to a range of ethanol between 3.2 and 0.1% final in the presence of bacterial suspension at 5.105 CFU/mL.
2.5.5. Reading the Plates
After an 18-hour incubation at 37 °C for E. coli ATCC25922, B. cereus ATCC11778, S. aureus ATCC25923, and S. epidermidis CIP81.55, or a 40-hour anaerobic incubation at 37 °C for C. acnes strains DSM1897, DSM30753, CIP110516, CIP110517, CIP110528, and CIP.A179, 50 µL of a 2 mg/mL nitrophenyl-tetrazolium iodide (INT) solution was added to each test well. In the presence of live bacteria, the INT is reduced, producing a detectable red compound.
Growth and ethanol control wells must indicate bacterial growth, while contamination control wells must show no growth. Once these conditions are confirmed, the test wells can be interpreted.
For each product tested, the minimum inhibitory concentration (MIC) is defined as the lowest concentration of the test product that does not result in a visible red color change, indicating bacterial inhibition.
2.6. Growth Curves
The solutions of the compounds at the tested concentrations of 2, 4, 16, and 32 μg/mL were each tested in triplicate against B. cereus ATCC11778. In a 96-well plate, 10 μL of 40, 80, 320, and 640 μg/mL fresh stock solutions of 2,4-DTBP, 2,6-DTPB, and 3,5-DTPB compounds were placed, as well as 190 μL of 5 × 105 CFU/mL of the selected bacterial suspension in brain heart infusion (BHI) broth.
Positive controls containing only 200 μL of 5 × 105 CFU/mL of the bacterial suspension in BHI and negative controls containing only 200 μL of BHI broth were added. The plate was incubated at 37 °C in a TECAN Spark Reader (Roche Diagnostic, Meylan, France) and the bacterial growth was followed by OD590 nm measurements every 20 min for 18 h.
2.7. Measurement of the ATP Efflux
Fresh stock solutions of 2,4-DTBP, 2,6-DTPB, and 3,5-DTPB were prepared in Phosphate-Buffer Saline (PBS) at concentration of 10 mg/mL then 10-fold diluted in BHI.
The B. cereus ATCC11778 suspensions were prepared in BHI and were incubated at 37 °C until reaching the growth exponential phase. Then, 90 μL of bacterial suspension was added to 10 μL of the compound solution in a Corning® 96-well white flat-bottom cell culture plate and shaken for 5s in the incubator at 37 °C. Subsequently, after 3 min of contact, 50 μL of Luceferin–Luciferase reagent (Yelen, Marseille, France) was added to the mixture, and the luminescent signal was quantified with TECAN Spark Reader (Roche Diagnostic, Meylan, France) (Tecan, Männedorf, Switzerland) for 6 readings spaced 30 s apart. Squalamine (100 μg/mL) was used as the positive control to quantify the maximum level of ATP efflux with BHI as the negative control. This assay was performed in three independent experiments.
2.8. OFAP18 and Erythromycin Ointments Preparation
The propolis OFAP18-based ointment (1%) was prepared by mixing 95 g petroleum jelly (Cooper, cooperation pharmaceutique française, Paris, France) and 5 mL of a glycerol solution containing 1 g of pure extract of OFAP 18. Thus, petroleum jelly was added gradually, and the contents were mixed for 10 min until obtaining a homogeneous ointment. The ointment was then stored in a sterile tube at 4 °C. A similar protocol was followed to prepare a 1% erythromycin ointment by dissolving 1 g of erythromycin in 4 g of glycerol, then mixing it with 95 g of petroleum jelly. The sterility of the different ointments was then verified by suspending them in sterile distilled water and depositing 100 µL of these suspensions on TSA agar plates and incubating them at 37 °C for 24 h.
2.9. Mouse Model of C. acnes Induced Inflammation (APAFIS Project Authorization No. 40597-2023020110385822 v2)
Propolis solutions at 1% (OFAP 18) and erythromycin at 1% in petroleum jelly are used for treatments. Pure petroleum jelly was used as a negative control. Erythromycin (Sigma, Saint Quentin Fallavier, France, ref E7904-10G), the predominant antibiotic used to treat acne, will serve as the reference treatment in this trial.
After a 12-day acclimatization period, the mice received the following cream applications:
Cohort 1 “test”: 10 mice (5 males and 5 females) received a daily application of petroleum jelly on their left flank and petroleum jelly + 1% propolis on their right flank for 8 days.
Cohort 2 “reference”: 10 mice (5 males and 5 females) received a daily application of petroleum jelly on their left flank and petroleum jelly + 1% erythromycin on their right flank for 8 days.
On the 9th day, a bacterial suspension of C. acnes DSM 1897 at 109 CFU/mL was prepared from overnight cultures in an anaerobic atmosphere following this protocol:
For 24 tubes:
Centrifuge 1.5 mL of culture at 4000 RPM for 10 min.
Repeat centrifugation twice, removing the supernatant and adding 1 mL of sterile PBS each time, followed by another centrifugation at 4000 RPM for 10 min.
Remove the supernatant and add 1 mL of sterile PBS.
Mix and transfer the suspension sequentially from tube 1 to tube 24, each time adding 1 mL of sterile PBS.
Perform a final centrifugation at 4000 RPM for 10 min and remove the supernatant, then add 1 mL of sterile PBS.
The OD600 of the sample was measured at 2.6. Due to the saturation limit of the device, a 5-fold dilution was prepared for measurement to confirm the bacterial concentration range (1.5 × 109 CFU/mL). Two bacterial counts were conducted on this suspension: the first before starting the injections (1.1 × 109 CFU/mL) and the second 2 h after the injections (1.4 × 109 CFU/mL). These results indicate no significant difference in the quantity of bacteria injected between the first and last treated mice.
The 20 mice were infected by subcutaneous injections of 20 µL of this bacterial suspension. Each mouse received one injection in the right flank and one in the left flank. Following the injection and in the subsequent days, the mice received cream applications according to the previous protocol.
One day after the appearance of pimples, the mice were sacrificed. A 5 mm skin sample from each flank was taken using a punch. Each sample was divided into two portions: one for bacterial enumeration and the other for histological analysis.
2.10. Histological Analysis
For each mouse, skin biopsy obtained from the acne pimples treated with petroleum jelly, erythromycin or OFAP18 was fixed in 4% phosphate-buffered neutral formaldehyde and processed for paraffin embedding. Paraffin sections (3–4 μm) were stained with routine hematoxylin–eosin–saffron. The examination was performed by a pathologist blinded to the group identity (H. L.) to determine the level of inflammation of the different skin samples.
3. Results and Discussion
In the extraction process, it is noteworthy that propolis exhibits a hard and crumbly consistency initially. However, upon handling and slight heating, it undergoes a transformation, becoming viscous and sticky, with a melting point at temperatures around 70 °C [8]. Among all the propolis tested and collected from various parts of Rwanda, even close in terms of distance, only one, namely OFAP18, demonstrated a potent interesting antimicrobial activity against C. acnes, as illustrated in Table 1. Based on these findings, we decided to identify the molecule or molecules responsible for such antibacterial activities.
Table 1.
Antimicrobial activities of Rwandan propolis extracts against various both Gram-positive and negative bacteria.
| Sample | MIC (µg/mL) | ||||||
|---|---|---|---|---|---|---|---|
|
E. coli ATCC 25922 |
S. aureus ATCC 25923 |
S. epidermidis CIP 81.55 |
B. cereus ATCC 11778 |
C. acnes DSM 1897 |
C. acnes DSM 30753 |
C. acnes CIP 110516 |
|
| OFAP 2 | >256 | >256 | 256 | 16 | 8 | 16 | 32 |
| OFAP 6 | >256 | >256 | >256 | 125 | 125 | 64 | 256 |
| OFAP 7 | >256 | >256 | >256 | 64 | 64 | 32 | 32 |
| OFAP 9 | >256 | >256 | 256 | 32 | 32 | 16 | ND |
| OFAP 10 | >256 | >256 | 32 | 64 | 16 | 32 | ND |
| OFAP 11 | >256 | >256 | >256 | 64 | 64 | 64 | ND |
| OFAP 15 | >256 | 64 | 32 | 16 | 16 | ND | ND |
| OFAP 16 | >256 | >256 | >256 | 32 | 32 | ND | ND |
| OFAP 18 | >256 | 64 | 16 | 16 | 16 | 16 | 16 |
| OFAP 20 | >256 | >256 | >256 | 64 | 16 | 32 | >256 |
| OFAP 21 | >256 | 64 | 64 | 32 | 32 | 32 | >256 |
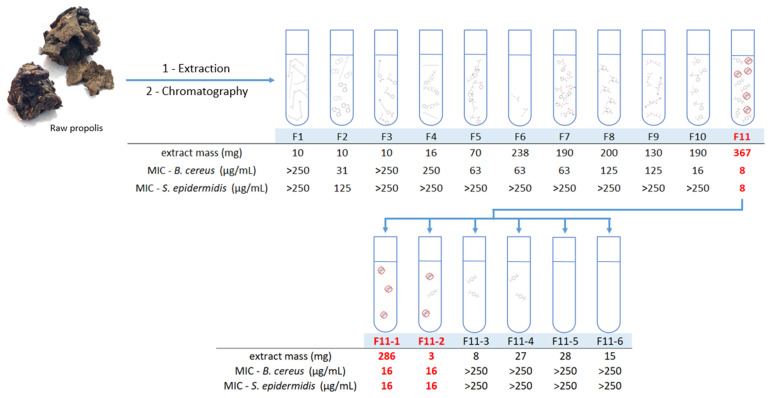
Briefly, 9.0 g of propolis OFAP18 was extracted with ethanol (water–ethanol (30:70, v/v), leading to an ethanol extract which is concentrated under vacuum as a crude powder and subsequently submitted to flash chromatography (from non-polar to polar, namely petroleum ether, ethyl acetate, and methanol) yielding 11 fractions titled F1 to F11 (Figure 1).
Figure 1.
Summary of the fractionation of OFAP18.
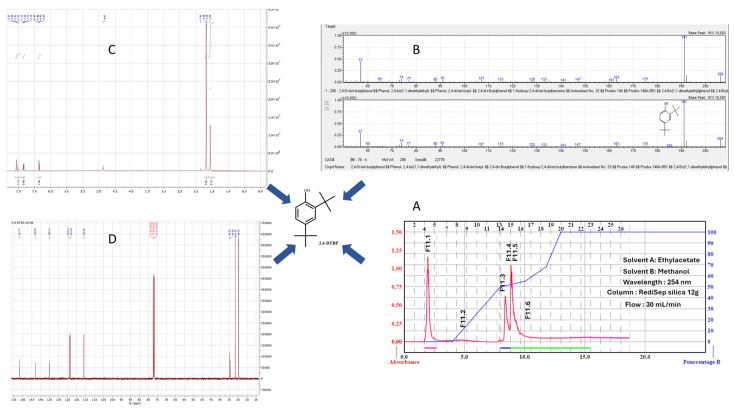
All the fractions were tested for antimicrobial activities and only fraction F11 led to an interesting MIC against both B. cereus and C. acnes strains. Thus, the F11 fraction was used for a second purification via flash chromatography carried out from 367 mg of crude residue which allowed us to obtain 35 fractions of 20 mL; these were grouped into six fractions coded from F11.1 to F11.6. These fractions are summarized in Table 2, and their respective antibacterial activities are highlighted. Pure fraction F11.1 was identified as the most active against both B. cereus and C. acnes, prompting an investigation into the compound responsible for this activity. The nature of the molecule was clearly determined by GC-MS as 2,4-Di-tert-butylphenol (2,4-DTBP) and its structure was unambiguously confirmed by 1H and 13C NMR spectrometry (Figure 2 and Figures S1 and S2).
Table 2.
Antimicrobial activities of OFAP18, 2,4-DTBP, 3,5-DTBP, and 2,6-DTBP against a wide range of bacterial strains.
| Sample | MIC (µg/mL) | ||||
|---|---|---|---|---|---|
| E. coli 25922 | S. aureus 25923 | S. epidermidis 81.55 | B. cereus 11778 | C. acnes 1897 | |
| OFAP18 | >256 | 64 | 16 | 16 | 16 |
| 2,4-DTBP | >256 | 16 | 16 | 8 | 16 |
| 2,6-DTBP | >256 | >256 | 125 | 256 | >256 |
| 3,5-DTBP | >256 | 32 | 32 | 16 | 64 |
Figure 2.
(A–D) Determination of the identity of 2,4-Di-tert-butylphenol (2,4-DTBP) in the studied fraction.
Notably, we also detected the presence of 3,5-Di-tert-butylphenol (3,5-DTBP), an isomer of 2,4-DTPB in a 1:10 ratio relative to 2,4-Di-tert-butylphenol, in the analyzed propolis sample via GC-MS analysis.
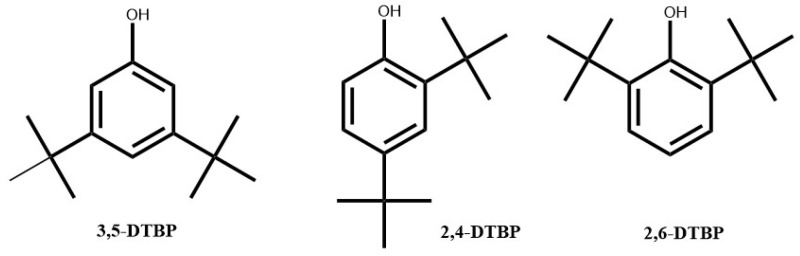
All these compounds as well as their 2,6-DTBP isomer (Figure 3) were tested for their intrinsic antimicrobial activities against a wide range of bacterial strains, including E. coli ATCC 25922, B. cereus ATCC 11778, S. aureus ATCC 25923, S. epidermidis CIP81.55, and C. acnes ATCC 1897.
Figure 3.
Structure of Di-tert-butyl phenol isomers (2,4-DTBP, 3,5-DTBP, and 2,6-DTBP).
The antimicrobial activity tests of the commercial molecules 2,4-DTBP and 3,5-DTBP demonstrated strong antimicrobial activity against B. cereus and C. acnes, particularly with 2,4-DTBP, whereas no activity was encountered by using isomer 2,6-DTBP. Thus, there is a strong correlation between the antimicrobial activity of the OFAP18 extract against the pathogen responsible for acne and the presence of 2,4-DTBP, a property that has not been previously reported in the literature (Table 2).
Subsequently, we were able to extend the spectrum of action of 2,4-DTBP on a larger panel of C. acnes strains, confirming the great activity of the latter towards this pathogen with a MIC of 16 µg/mL even against an erythromycin-resistant strain (Table 3).
Table 3.
Antimicrobial activities of 2,4-DTBP against a large panel of C. acnes bacterial strains.
| Sample | CMI (µg/mL) | |||||
|---|---|---|---|---|---|---|
| C. acnes DSM1897 | C. acnes CIPDSM110512 |
C. acnes CIP 110516 (ERY-R) |
C. acnes CIP110517 | C. acnes CIP110528 |
C. acnes CIP A179 |
|
| 2,4-DTBP | 16 | 16 | 16 | 16–32 | 16 | 16 |
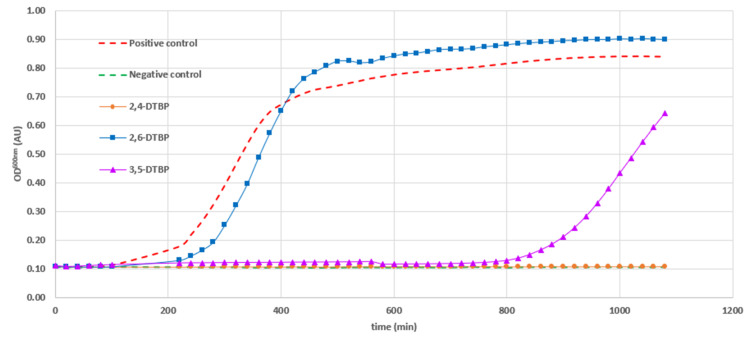
The growth inhibition profiles of the three Di-tert-butylphenol (DTBP) isomers against Bacillus cereus ATCC 11778 were determined to evaluate the dynamics of their antibacterial activity. No inhibition of bacterial growth was observed in the presence of 2,6-DTBP at a concentration of 16 µg/mL. In contrast, the growth response to 2,5-DTBP was more nuanced; inhibition was observed during the first 13 h, followed by a subsequent escape from the action of the compound. Finally, significant growth inhibition was only observed with the 2,4-DTBP isomer used at a 16 µg/mL concentration (Figure 4).
Figure 4.
Bacterial growth inhibition against B. cereus ATCC 11778 exhibited by Di-tert-butyl phenol isomers (2,4-DTBP, 3,5-DTBP, and 2,6-DTBP) used at a 16 µg/mL concentration. Positive control was bacteria only and negative control was media only.
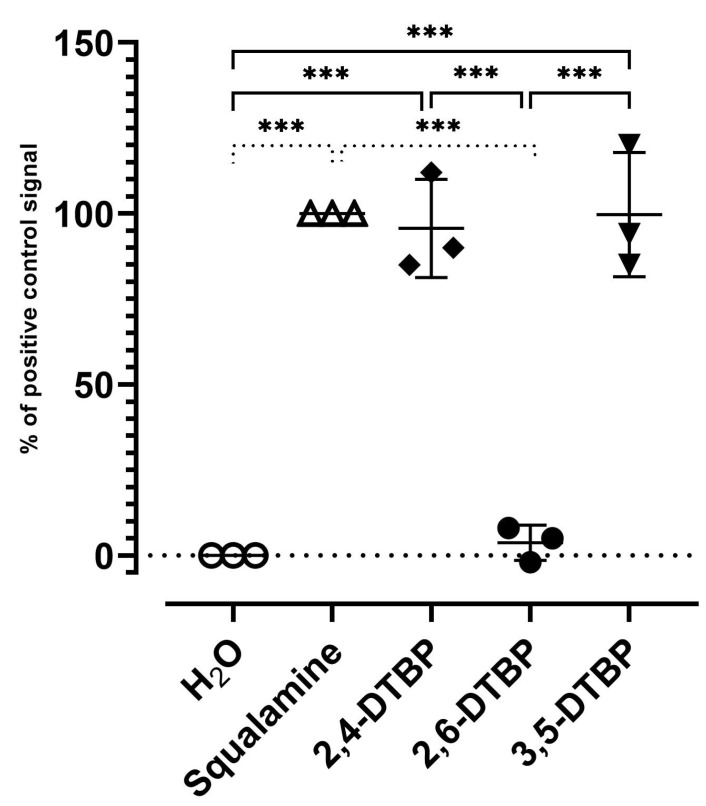
On the other hand, we attempted to elucidate more precisely the mechanism of action of 2,4-DTBP by investigating its potent permeabilizing and disrupting behavior of the outer membrane of Gram-positive B. cereus. A bioluminescence method was then developed involving the detection of the external concentration of ATP, which was used as a reporter reflecting the permeabilizing effect of 2,4-DTBP and 3,5-DTBP. Thus, these derivatives dramatically disrupted the B. cereus membrane after 2 min, as observed by intracellular ATP release kinetics, which was like the positive control squalamine (Figure 5). Nevertheless, we must keep in mind that the concentration used for these compounds was very high, whereas only 2,4-DTBP was active at around 16 µg/mL, suggesting that LPS damage induced by this latter is clearly greater and faster than that caused by 2,6-DTBP. Conversely, no significant effect was found by using water as a negative control as well as 2,6-DTBP during the test time, with only a 0 and 10% ATP efflux release relative to the squalamine positive control, respectively.
Figure 5.
ATP release in B. cereus ATCC11778 exhibited by Di-tert-butyl phenol isomers (2,4-DTBP, 3,5-DTBP and 2,6-DTBP) as determined using ATP efflux assay. Squalamine (100 µg/mL) was the positive control and water was the negative control. Compounds were tested at a final concentration of 100 µg/mL, and the results are reported as a percentage (%) relative to positive control. *** shows significant differences.
Based on these results, we formulated an ointment using OFAP18 and petroleum jelly (1% OFAP18 or erythromycin) for the treatment of acne in a mouse model. In the first set of experiments, we injected 20 µL of a bacterial suspension (109 CFU/mL) under the skin to induce acne pimples over 2 days, followed by applying the ointment for 7 days. We mainly observed a decrease in pimples for each test parameter. No bacteria were enumerated, and all mice exhibited inflammation; the immune response of mice masked any potential effect of the formulated ointment.
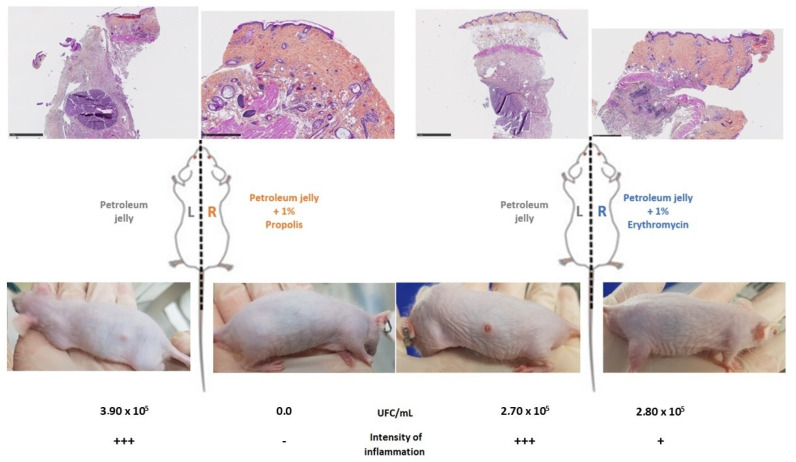
In the second set of experiments, we applied OFAP18 and erythromycin ointments daily for 8 days before injecting the bacterial suspension. We then evaluated the efficacy of both ointments against C. acnes colonization over the course of 2 days (Figure 6). The histological analysis of mouse skin biopsies showed inflammatory infiltrates in the dermis composed predominantly of neutrophils often associated with cutaneous necrosis. OFAP18 and erythromycin-treated mice exhibited lower dermal inflammation than control ones treated with excipient 2 days after injection with 109 CFU/mL of C. acnes DSM1897 suspension.
Figure 6.
OFAP18 (orange)- and erythromycin (blue)-treated mice exhibited lower epidermal inflammation than control ones treated with excipient 2 days after injection with 109 CFU/mL of C. acnes DSM1897 suspension.
Moreover, due to the lower observed concentration of bacteria in the petroleum sample from the cohort 1 mice compared to cohort 2, pre-treatment with the 1% OFAP18 ointment appears to diffuse throughout the entire body of the mouse, effectively limiting the growth of C. acnes bacteria compared to pre-treatment with the petroleum jelly of cohort 2 (Figure 7).
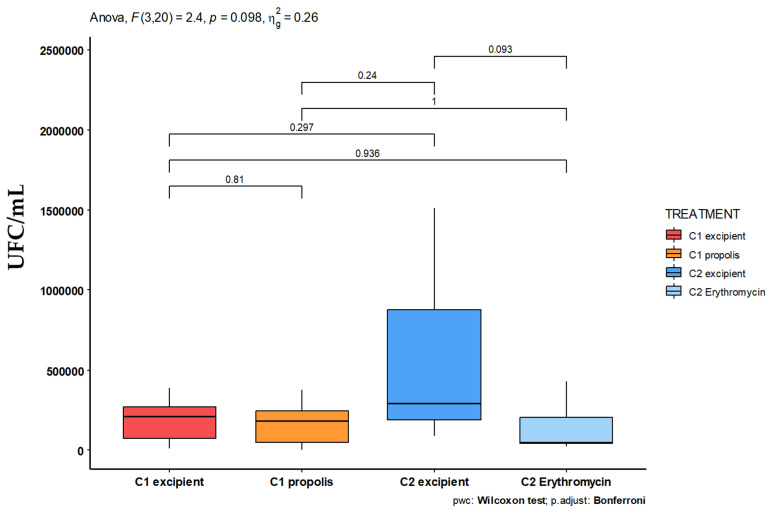
Figure 7.
Graphical representation of bacterial counts of C. acnes based on the treatments performed on the two cohorts of mice with OFAP18 (C1 orange) or erythromycin (C2 pale blue) ointments.
Therefore, due to significant variations in the number of bacteria counted within the mouse categories, we did not achieve statistically significant results regarding the reduction in the bacterial population. However, the comparison between pimples treated with OFAP18 (cohort 1) and those treated with petroleum jelly alone (cohort 2, without propolis diffusion) reveals a significant decrease in C. acnes concentration.
Finally, mice treated with OFAP18 and erythromycin exhibited significantly lower epidermal inflammation compared to those treated with petroleum jelly (Figure 7). Notably, more prominent inflammation was observed in mice pre-treated with petroleum jelly than in those pre-treated with OFAP18. We observe a statistically significant difference in bacterial counts between the petroleum jelly and erythromycin treatments in cohort 2 mice (p = 0.093). However, no such difference is seen between the OFAP18 treatment and petroleum jelly alone. Notably, there is a significant difference in the bacterial counts of pimples treated with petroleum jelly between cohorts 1 and 2. Furthermore, the pimples in cohort 2 appear more pronounced than those in cohort 1, suggesting that the active compound in propolis may have diffused during the 7-day pre-treatment period. When comparing the bacterial counts of pimples treated with OFAP18 in cohort 1 to those treated with petroleum jelly alone in cohort 2, we observe a marked difference, highlighting the antibacterial effect of the propolis OFAP18 treatment. These data support the effectiveness of the propolis-based cream OFAP18 and, more broadly, the molecule 2,4-DTPB responsible for its antibacterial activity. On the other hand, 2,4-DTPB appears as a metabolite produced by various plants and, even if the biosources and bioactivities have been well investigated, the phenol has not been systematically reported. Thus, it can be, for example, encountered in Pinus kesiya as the major component in the water extracts of fresh needles (16%) [23,24,25]. Based on the GPS coordinates (2°26′53.0″ S 29°04′07.0″ E), we were able to determine that two main species could constitute the source of 2,4-DTBP. Indeed, the hives from which the propolis OFAP18 is extracted from are found in a forest of Eucalyptus globulus bordered by a green tea field but also by the primary forest of Nyungwe which holds many endemic species of Rwanda.
4. Conclusions
In summary, we identified the molecule 2,4-Di-tert-butylphenol (2,4-DTBP) from propolis OFAP18 collected in Rwanda, which demonstrated the inhibition of C. acnes growth at a concentration of 16 µg/mL. A 1% ointment formulation was successfully prepared and tested in a mouse model, suggesting that 2,4-DTBP could effectively manage C. acnes overgrowth and serve as a potent alternative for acne treatment. Studies are now under current investigation to more precisely identify the most suitable propolis collection site and estimate the quality of the propolis harvested from the seasonality.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/antibiotics13111080/s1: Figure S1: 1H NMR and 13C NMR spectrum of 2,4-DTBP; Figure S2: 1H NMR and 13C NMR spectrum of 3,5-DTBP.
Author Contributions
Conceptualization, F.R. and J.M.B.; formal analysis, J.M.B.; investigation, F.R., L.A., E.W., P.A., J.C., M.-M.K., C.N., H.L. and J.M.B.; methodology, F.R. and J.M.B.; project administration, J.M.B.; supervision, J.M.B.; writing—original draft, F.R. and J.M.B. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The animal study protocol was approved by Direction générale de la recherche et de l’innovation (APAFIS #40597-2023020110385822 v2).
Informed Consent Statement
Not applicable.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This research received external funding from OFA (Observatoire Français d’Apidologie).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Dessinioti C., Katsambas A. The Microbiome and Acne: Perspectives for Treatment. Dermatol. Ther. 2024;14:31–44. doi: 10.1007/s13555-023-01079-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mayslich C., Grange P.A., Dupin N. Cutibacterium acnes as an Opportunistic Pathogen: An Update of Its Virulence-Associated Factors. Microorganisms. 2021;9:303. doi: 10.3390/microorganisms9020303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Antimicrobial Resistance Collaborators Global Burden of Bacterial Antimicrobial Resistance in 2019: A Systematic Analysis. Lancet Lond. Engl. 2022;399:629–655. doi: 10.1016/S0140-6736(21)02724-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rozas M., Hart de Ruijter A., Fabrega M.J., Zorgani A., Guell M., Paetzold B., Brillet F. From Dysbiosis to Healthy Skin: Major Contributions of Cutibacterium acnes to Skin Homeostasis. Microorganisms. 2021;9:628. doi: 10.3390/microorganisms9030628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gurung A., Badola A. An updated review on acne. World J. Biol. Pharm. Health Sci. 2023;14:300–317. doi: 10.30574/wjbphs.2023.14.3.0266. [DOI] [Google Scholar]
- 6.Abdel Fattah N.S., Darwish Y.W. In vitro antibiotic susceptibility patterns of Propionibacterium acnes isolated from acne patients: An Egyptian university hospital-based study. J. Eur. Acad. Dermatol. Venereol. 2013;27:1546–1551. doi: 10.1111/jdv.12057. [DOI] [PubMed] [Google Scholar]
- 7.Walsh T.R., Efthimiou J., Dréno B. Systematic review of antibiotic resistance in acne: An increasing topical and oral threat. Lancet Infect Dis. 2016;16:e23–e33. doi: 10.1016/S1473-3099(15)00527-7. [DOI] [PubMed] [Google Scholar]
- 8.Jappe U. Pathological mechanisms of acne with special emphasis on Propionibacterium acnes and related therapy. Acta Derm. Venereol. 2003;83:241–248. doi: 10.1080/00015550310016463. [DOI] [PubMed] [Google Scholar]
- 9.Fanelli M., Kupperman E., Lautenbach E., Edelstein P.H., Margolis D.J. Antibiotics, acne, and Staphylococcus aureus colonization. Arch. Dermatol. 2011;147:917–921. doi: 10.1001/archdermatol.2011.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Makashvili Z. From the History of Propolis. APIMONDIA Standing Commission on Bee Keeping Technology and Equipment; Bucharest, Romania: 1978. Remarkable hive product: Propolis. Scientific data and suggestions concerning its composition, properties and possible use in therapeutics.249p [Google Scholar]
- 11.Bankova V. Recent trends and important developments in propolis research. Evid. Based Complement. Alternat. Med. 2005;2:29–32. doi: 10.1093/ecam/neh059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sforcin J.M. Biological properties and therapeutic applications of propolis. Phytother. Res. 2016;30:894–905. doi: 10.1002/ptr.5605. [DOI] [PubMed] [Google Scholar]
- 13.Anjum S.I., Ullah A., Khan K.A., Attaullah M., Khan H., Ali H., Bashir M.A., Tahir M., Ansari M.J., Ghramh H.A., et al. Composition and functional properties of propolis (bee glue): A review. Saudi J. Biol. Sci. 2019;26:1695–1703. doi: 10.1016/j.sjbs.2018.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang K., Ping S., Huang S., Hu L., Xuan H., Zhang C., Hu F. Molecular mechanisms underlying the in vitro anti-inflammatory effects of a flavonoid-rich ethanol extract from chinese propolis (poplar type) Evid. Based Complement. Alternat. Med. 2013;2013:127672. doi: 10.1155/2013/127672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bankova V.S., de Castro S.L., Marcucci M.C. Propolis: Recent advances in chemistry and plant origin. Apidologie. 2000;31:3–15. doi: 10.1051/apido:2000102. [DOI] [Google Scholar]
- 16.Sforcin J.M. Propolis and the immune system: A review. J. Ethnopharmacol. 2007;113:1–14. doi: 10.1016/j.jep.2007.05.012. [DOI] [PubMed] [Google Scholar]
- 17.de Groot A.C. Propolis: A review of properties, applications, chemical composition, contact allergy, and other adverse effects. Dermatitis. 2013;24:263–282. doi: 10.1097/DER.0000000000000011. [DOI] [PubMed] [Google Scholar]
- 18.Huang S., Zhang C.P., Wang K., Li G.Q., Hu F.L. Recent advances in the chemical composition of propolis. Molecules. 2014;19:19610–19632. doi: 10.3390/molecules191219610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Silva-Carvalho R., Baltazar F., Almeida-Aguiar C. Propolis: A complex natural product with a plethora of biological activities that can be explored for drug development. Evid. Based Complement. Alternat. Med. 2015;2015:206439. doi: 10.1155/2015/206439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sforcin J.M., Bankova V. Propolis: Is there a potential for the development of new drugs? J. Ethnopharmacol. 2011;133:253–260. doi: 10.1016/j.jep.2010.10.032. [DOI] [PubMed] [Google Scholar]
- 21.Stojanović S., Najman S.J., Bogdanova-Popov B., Najman S.S. Propolis: Chemical composition, biological and pharmacological activity—A review. Acta Medica Median. 2020;59:108–113. doi: 10.5633/amm.2020.0215. [DOI] [Google Scholar]
- 22.McLoone P., Tabys D., Fyfe L. Honey combination therapies for skin and wound infections: A systematic review of the literature. Clin. Cosmet. Investig. Dermatol. 2020;13:875–888. doi: 10.2147/CCID.S282143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhao F., Wang P., Lucardi R.M., Su Z., Li S. Natural Sources and Bioactivities of 2,4-Di-Tert-Butylphenol and Its Analogs. Toxins. 2020;12:35. doi: 10.3390/toxins12010035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Celeiro M., Lamas J.P., Arcas R., Lores M. Antioxidants Profiling of By-Products from Eucalyptus Greenboards Manufacture. Antioxidants. 2019;8:263. doi: 10.3390/antiox8080263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lu M. Is aromatic plants environmental health engineering (APEHE) a leverage point of the earth system? Heliyon. 2024;10:e30322. doi: 10.1016/j.heliyon.2024.e30322. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.