Abstract
Background:
A prospective cohort study was conducted to assess the predictors of failure of nonoperative treatment, defined as the patient undergoing surgery for symptomatic, atraumatic full-thickness rotator cuff tears. We present the 10-year follow-up data of this population to determine if predictors for surgery change over time, and secondarily we report the outcomes of the cohort.
Methods:
At the time of enrollment, demographic, symptom, rotator cuff anatomy, and patient-reported outcome data were collected in patients with symptomatic, atraumatic full-thickness rotator cuff tears. Patients underwent a standard physical therapy protocol for 6 to 12 weeks. Patient data were then collected at 1, 2, 5, 7, and 10 years. Failure of nonoperative treatment was defined as the patient electing to undergo surgery.
Results:
Of the 452 patients in the original cohort, 20 patients (5%) withdrew from the study, 37 (9%) died before 10 years, and 40 (9%) were otherwise lost to follow-up. A total of 115 patients (27.0%) underwent a surgical procedure at some point during the 10-year follow-up period. Of these patients, 56.5% underwent surgery within 6 months of enrollment and 43.5%, between 6 months and 10 years. Low patient expectations regarding the efficacy of physical therapy were found to be a predictor of early surgery. Workers’ Compensation status and activity level were more important predictors of later surgery. Patient-reported outcome measures all improved following physical therapy. For patients who did not undergo a surgical procedure, patient-reported outcome measures did not decline over the 10-year follow-up period.
Conclusions:
Low patient expectations regarding the efficacy of physical therapy were found to be a predictor of early surgery, whereas Workers’ Compensation status and activity level were predictors of later surgery. Physical therapy was successful in >70% of patients with symptomatic, atraumatic full-thickness rotator cuff tears at 10 years. Outcome measures improved with physical therapy and did not decline over the 10-year follow-up period.
Level of Evidence:
Prognostic Level I. See Instructions for Authors for a complete description of levels of evidence.
Rotator cuff tears (RCTs) are one of the leading causes of shoulder pain and disability, accounting for 272,148 surgical procedures in the U.S. in 20061,2. In the U.S., rotator cuff repair rates have been accelerating, with a 141% increase in procedures from 1996 to 20061. The likelihood of an RCT increases with age3-8. Because of an increasingly aging population and because more than two-thirds of patients undergoing rotator cuff surgery are of working age, these injuries represent a substantial economic burden to the U.S. health-care system9.
Historically, the presence of the condition served as the indication for rotator cuff repair surgery for many surgeons10. Surveys of the members of the American Academy of Orthopaedic Surgeons show little agreement in clinical decision making for RCTs11, which may contribute to the tremendous geographical variation noted for rotator cuff surgery in the U.S2,12,13. These data suggest there is uncertainty regarding the indications for surgery for patients with RCTs.
In order to gain insight into the indications for rotator cuff repair surgery, our Multicenter Orthopaedic Outcomes Network (MOON) Shoulder Group performed a prospective cohort study of 452 patients with nonoperatively treated symptomatic, atraumatic full-thickness RCTs14,15. We hypothesized that specific variables related to the medical history, physical examination, and imaging would serve as predictors for failure of nonoperative treatment. The primary aim of this study was to assess how the predictors of surgery change over the course of the 10-year follow-up period. Secondarily, we sought to determine if the effectiveness of nonoperative treatment is durable, and report on the types of surgery performed over the 10-year period.
Materials and Methods
Study Design
This multicenter prospective cohort study was designed to identify predictors of failure of nonoperative treatment for symptomatic, atraumatic full-thickness RCTs14,15. This study (ClinicalTrials.gov NCT00762580) was approved by the institutional review boards of each institution. Patients 18 to 100 years old with symptomatic, atraumatic full-thickness RCTs were invited to participate. Patients were excluded if they had a history of injury, pain related to the cervical spine, scapular pain, previous shoulder surgery, glenohumeral arthritis, inflammatory arthritis, adhesive capsulitis, previous proximal humeral fracture, known bilateral RCTs, or dementia.
At the initial visit, patients completed a questionnaire that detailed demographic data and included validated patient-reported outcome measures (PROMs)14,15. The following PROMs were collected: Short Form-12 (SF-12) score16, American Shoulder and Elbow Surgeons (ASES) score17, Western Ontario Rotator Cuff (WORC) index score18, Single Assessment Numeric Evaluation (SANE) score19, Self-Administered Comorbidity Questionnaire20, and the Shoulder Activity Scale21. Patient expectations were assessed by the Musculoskeletal Outcomes Data Evaluation and Management System (MODEMS) survey, which includes 6 items, each scored from 1 (lowest expectations) to 5 (highest expectations). Physical examination and magnetic resonance imaging (MRI) assessment was performed by the surgeons participating in the study according to the methods and cohort data detailed in previous reports14,15.
Outcome scores were collected at each follow-up point (6 weeks, 12 weeks, and 1, 2, 5, 7, and 10 years). Physical examination data were also collected at the 6 and 12-week visits.
Patients were given 2 instructive rehabilitation books, 1 for physical therapists and another for home-based physical therapy written at the eighth-grade level with an accompanying DVD (digital video disc). The specific exercises14,15 were derived from a systematic review of the literature22.
Patients returned after performing the therapy program for 6 weeks. At that point, patients were given 3 options. (1) If they considered themselves “cured,” no additional treatment or scheduled physician follow-up was prescribed. (2) If they considered themselves “improved,” patients continued the physical therapy program for another 6 weeks. (3) If they considered themselves “no better,” they could elect to undergo surgery. Patients could choose to have surgery at any time after enrollment in the study.
Patients were contacted by telephone at 1, 2, 5, 7, and 10 years, and data were collected regarding whether they had had surgery and the details of that surgery. Surgical reports were obtained when possible. Patients were mailed our PROMs form with instructions to complete and return it at each time point.
Statistical Analysis
Descriptive analyses of the PROMs were performed, including calculation of the median and interquartile range for each year of follow-up. Time-to-event analyses were performed to examine the durability of nonoperative treatment over time and to identify baseline predictors of failure of nonoperative treatment. Kaplan-Meier survivorship curves were utilized to visually display the proportion of patients who were free of surgery over time. Cox proportional hazards models were fit to determine predictors of failure of nonoperative treatment. The dependent variable was the number of days to surgery. The models sought to adjust for the following independent covariates: tear severity, patient demographics, psychosocial factors, and comorbidities, as well as other aspects of the patient’s medical history deemed pertinent at the time of enrollment. Age, body mass index (BMI), sex, occupation, Workers’ Compensation status, education, duration of symptoms, dominant arm, shoulder activity level, smoking status, comorbidity score, patient expectations, visual analogue scale (VAS) pain score, number of tendons torn, amount of RCT retraction, and forward elevation strength (FE) were all included as candidate predictors in the models. Three Cox models were fitted with the same covariate adjustment as described above. An overall model was fitted using 115 events (i.e., 115 surgical interventions). The Schoenfeld test was utilized to confirm that the proportional hazards assumption of the Cox models was not violated. Subgroup analyses were performed to explore potential differences in factors driving surgery early versus late during rehabilitation. Patients were categorized as undergoing early surgery if they required operative intervention within 180 days or as undergoing late surgery if they required operative intervention at >180 days. Statistical analysis was performed with use of R (R Project for Statistical Computing), and models were fitted with use of the rms package23. The STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines were utilized in producing this manuscript24.
Results
Population Demographics
A total of 2,233 patients with RCTs were identified during the enrollment period (January 17, 2007, to September 23, 2010). Of these, 1,280 were excluded for the following reasons: acute traumatic tears (38%), previous surgery (11%), bilateral disease (8%), neck disorders (6%), frozen shoulder (2%), dislocation (3%), rheumatoid disease (1%), and/or fracture (1%). Of the remaining 953 patients eligible to enroll in the study, 452 (47%) elected to do so. These 452 patients were followed as a prospective cohort, with rolling entry into the study. Of this group, 20 patients withdrew from the study soon after enrollment and did not contribute longitudinal follow-up, leaving a sample of 432 patients14,15.
Of the 432 patients available for analysis, 37 (9%) died before the end of the 10-year follow-up period and 40 others (9%) were lost to follow-up; thus, a total of 355 patients (82%) were included for the final analyses. Of these, 115 (27%) were known to have undergone surgery at some point during the 10-year follow-up period. Operative details were available for 105 of these patients.
Demographics of the cohort are detailed in previous reports14,15. The mean age of the study population was 62.6 years (range, 31 to 90 years), with 51% men and 49% women. The dominant arm was affected in 68% of patients. The right arm was affected in 70%. The population was predominantly White (86%), Black (8%), or Asian (3%). Many patients had comorbidities, with hypertension, back pain, and osteoarthritis being the most common14. Most patients (90%) were nonsmokers. Before enrolling in the study, 23% of patients had already undergone some physical therapy, 40% had received corticosteroid injections, and 80% had utilized nonsteroidal anti-inflammatory drugs14,15.
MRI14,15 showed superior humeral head migration in 15% of patients. Tears involving only the supraspinatus were observed in 70% of patients. RCT size was graded in the coronal plane on MRI according to the Patte classification25, with 48% of cases being classified as Stage 1 (i.e., tendon stump near the osseous insertion or minimal), 34% as Stage 2 (i.e., tendon stump retracted to the middle of the humeral head or midhumeral), and 19% as Stage 3 (i.e., tendon stump retracted to the glenoid or glenohumeral).
Predictors of Surgery Over Time
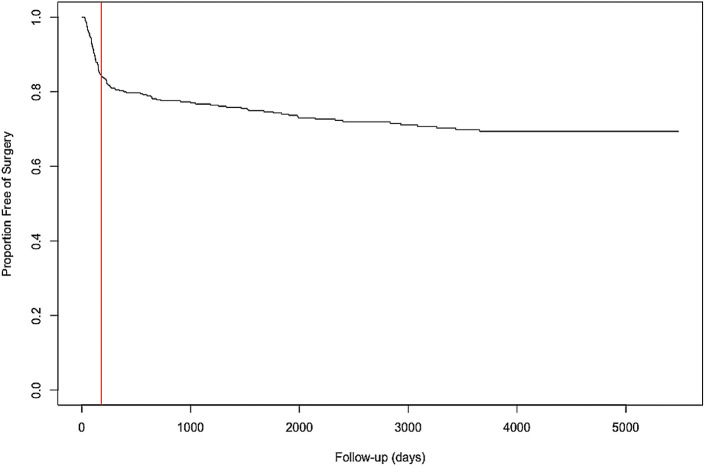
Figure 1 depicts a Kaplan-Meier survivorship curve for the cohort over the 10-year follow-up period. Of the 115 patients who underwent surgery, 65 (57%) did so within 6 months of enrollment. The other 50 patients (43%) underwent surgery between 6 months and 10 years after enrolling in the study, with a constant rate of approximately 5 patients/year. Overall, <30% of patients had undergone surgery at the end of the 10-year follow-up period.
Fig. 1.
Ten-year Kaplan-Meier curve showing survival free from operative treatment among patients with symptomatic, atraumatic full-thickness RCTs. Overall, <30% of patients had undergone surgery by the end of the 10-year follow-up period. Most patients who underwent surgery did so within 6 months (red line).
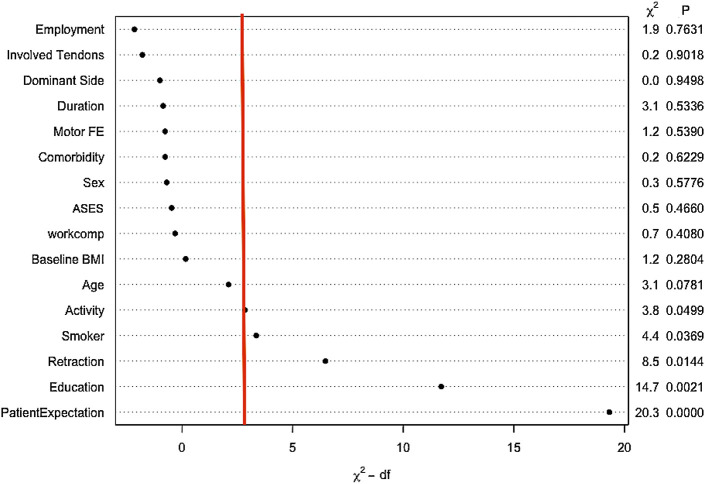
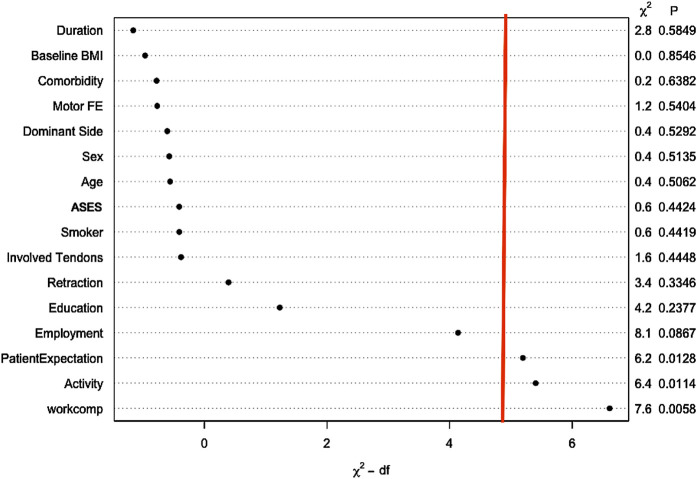
Low patient expectations regarding the efficacy of physical therapy were the most powerful predictor of early surgery (hazard ratio [HR], 16.86; 95% confidence interval [CI], 4.94 to 57.59 (Fig. 2; see also Appendix). Other less impactful predictors included patient education, the amount of rotator cuff tear retraction, smoking, and activity level. Among patients who underwent surgery between 6 months and 10 years, patient expectations were less important, whereas Workers’ Compensation status (HR, 3.51; 95% CI, 1.44 to 8.58) and activity level (HR, 1.79; 95% CI, 1.14 to 2.81) were more important (Fig. 3; see also Appendix 1).
Fig. 2.
Predictors of early surgery. This graph reflects the characteristics of patients who underwent surgery within 6 months of enrollment. The strength of each predictor is reflected by its position on the x axis. Predictors to the right of the vertical red line were significant (p < 0.05). Significant predictors of early surgery include smoking, Workers’ Compensation status, the amount of tear retraction (see Figure 4), activity level, and patient expectations. The strongest predictor in this group, by far, was the patient’s expectations regarding the effectiveness of physical therapy.
Fig. 3.
Predictors of later surgery (6 months to 10 years). This graph reflects the characteristics of patients who underwent surgery after 6 months of enrollment. The strength of each predictor is reflected by its position on the x axis. Predictors to the right of the vertical red line were significant (p < 0.05). Significant predictors of later surgery include patient expectations, activity level, and Workers’ Compensation status. Workers’ Compensation status and activity level were stronger predictors of later surgery than patient expectations regarding the effectiveness of physical therapy. df = degrees of freedom.
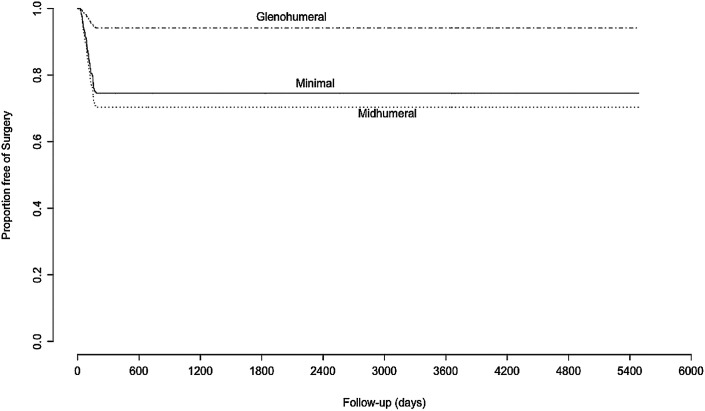
Although not nearly as impactful as patient expectations, the extent of RCT retraction was found to be a significant predictor for early surgery (HR for glenohumeral retraction versus minimal retraction, 0.20; 95% CI, 0.06 to 0.71), but not later surgery. Interestingly, patients with smaller tears were more likely to undergo surgery than those with larger tears (Fig. 4; see also Appdendix 1).
Fig. 4.
The influence of RCT retraction on predicting early surgery. RCT retraction was a significant predictor of early surgery. The effect of retraction is adjusted for all covariates in the model. Interestingly, larger tears were less likely to be operatively treated than smaller tears.
Types of Surgeries Performed
Surgery was performed in 115 (27%) of 432 patients over the 10-year follow-up period, with operative data available for 105 patients. Rotator cuff repair was performed in 103 patients (98%), including 1 partial repair and 1 repair augmented with use of a graft. Concomitant biceps surgery was performed in 37 patients (35%), including 23 tenodeses, 12 tenotomies, and 2 debridements of a ruptured tendon stump. Distal clavicular excisions were performed in 20 patients (19%). One patient had lysis of adhesions and underwent manipulation under anesthesia. Only 1 patient in the entire cohort (0.2%) underwent reverse total shoulder arthroplasty.
Indications for Surgery
Indications for surgery were listed in 89 of the 105 surgical reports. Indications listed for surgery included failure of nonoperative treatment (67), pain (42), weakness or functional loss (11), new trauma (10), biceps problems (3), adhesive capsulitis (2), and tear enlargement (2).
Durability of Physical Therapy as Assessed with PROMs
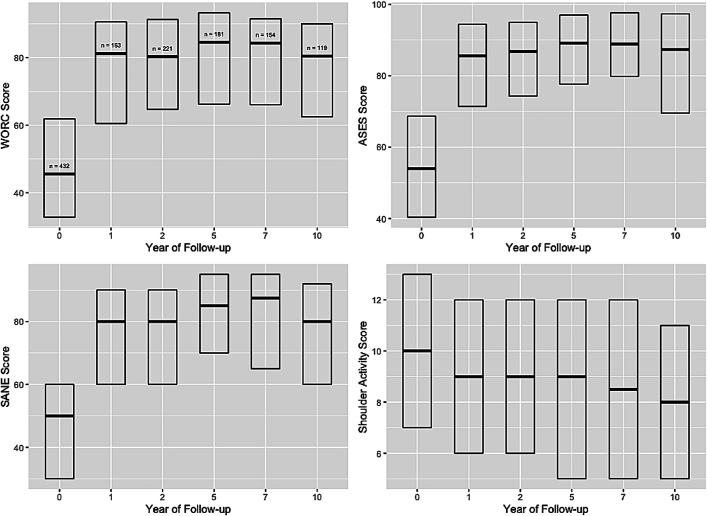
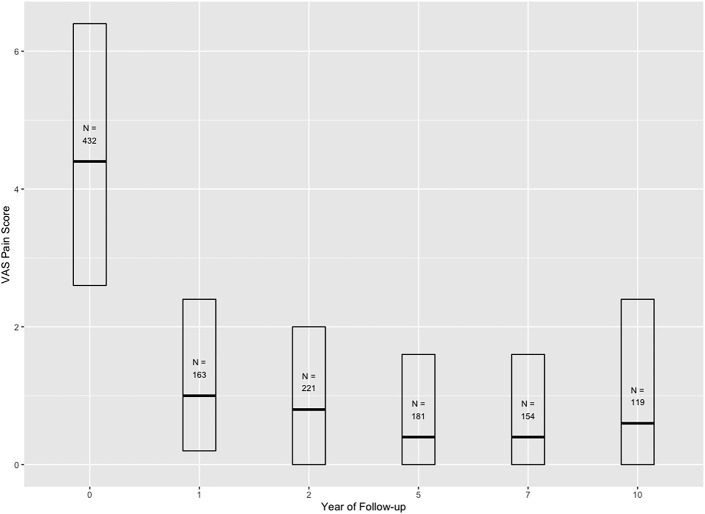
Figures 5-A and 5-B depict the effect of physical therapy and the measured PROMs over time. Initially, physical therapy produced significant improvements in PROMs from baseline to 1 year that exceeded the minimal clinically important difference for each PROM. After year 1, no meaningful changes were noted over the 10-year follow-up period for the WORC, ASES, SANE, and Shoulder Activity Scale (Fig. 5-A). Similarly, the VAS pain scores showed statistically significant improvement exceeding the minimal clinically important difference after the physical therapy program and this improvement did not change significantly over the 10-year follow-up period (Fig. 5-B).
Figs. 5-A and 5-B Changes in PROMs over time. The interquartile range is denoted by a box, and the median is denoted by a line within the box. PROMs improved with physical therapy, exceeding the minimal clinically important difference for the measures utilized. The Western Ontario Rotator Cuff score, American Shoulder and Elbow Surgeons score, Single Assessment Numeric Evaluation, and Shoulder Activity Score were stable over the 10-year follow-up period (Fig. 5-A). Similar findings occurred for VAS pain scores (Fig. 5-B). The sample sizes (N) show the group size available at each year of the follow-up, with zero on the x axis indicating baseline assessment at the time of enrollment. The N values are shown on only 1 plot in each figure but are the same for all plots.
Fig. 5-A.
Fig. 5-B.
Discussion
The primary aim of this study was to identify predictors of failure of nonoperative treatment for symptomatic, atraumatic full-thickness RCTs in order to help identify potential indications for surgery. Our data demonstrates that the predictors of failure change over time. Early surgery (within 6 months) is driven by low expectations regarding the efficacy of physical therapy. For patients who underwent surgery after 6 months, activity level and Workers’ Compensation status were strong predictors.
Patient Expectations
Modifying patient expectations through education has been shown to improve outcomes in total knee arthroplasty26,27, physical therapy for neck pain28, and the use of kinesiotape for shoulder pain29. It is not known whether expectations can be modified in patients with shoulder pain; however, there is currently a trial underway to study this question30. If low patient expectations regarding therapy could be modified, the overall rate of surgery might be similar to what we observed between 6 month and 10 years, and the effectiveness of physical therapy as a treatment would likely exceed 88%.
Activity Level and Workers’ Compensation Status
Activity level was found to be a significant predictor of both early and later surgery, whereas Workers’ Compensation status was a significant predictor of later surgery. These variables were more important than age, pain intensity, the number of tendons involved, and the duration of symptoms in predicting the likelihood of surgery. Physicians should strongly consider a patient’s activity level and Workers’ Compensation status when considering options for treatment of symptomatic, atraumatic full-thickness RCTs.
Secondary Aims
It is interesting to note that physical therapy was effective in treating >70% of patients with symptomatic, atraumatic full-thickness RCTs, with a durable effect lasting at least 10 years. It is also important to note that PROMs did not decline in patients undergoing nonoperative treatment over the 10-year follow-up period.
One potential indication for surgery is to prevent progression of RCTs. It is known that RCTs can progress over time; however, it is not known whether progression leads to symptoms substantial enough to warrant surgery. One recent systematic review designed to study RCT progression31 determined that progression of asymptomatic tears was observed in 40.6% of patients at 46.8 months and in 34% of asymptomatic patients at 36.8 months. Progression rates were not different when comparing symptomatic to asymptomatic patients, suggesting that progression and the presence of symptoms are not strongly related31.
Keener et al.32 found that only 28% of patients with asymptomatic tears who later developed symptoms underwent surgery. Variables that predicted surgery included greater pain intensity, early onset of pain, a decline in the ASES score, and a history of surgery for symptomatic rotator cuff tear on the contralateral side32. RCT progression was not found to be a predictor of surgery. Our data support these findings. Only 11.6% of our cohort had surgery between 6 months and 10 years, despite the expectation that RCT progression is expected in approximately 40% of patients31. Pain intensity and duration of symptoms—both of which may be associated with tear progression—were not found to be predictors of failure of nonoperative treatment in our covariate-adjusted models.
RCT progression in some patents will lead to substantial disability, which may ultimately require reverse shoulder arthroplasty. It would be helpful to know who is at risk for extensive progression of RCTs. Although the literature is limited, smoking33, age of >60 years34, larger tears34,35, and more fatty infiltration of the muscle34 have been associated with higher rates of RCT progression. Unfortunately, other studies have failed to show a relationship between age33 or tear size36 and RCT progression.
The present study suggests that severe or rapid progression may be relatively rare, in that only 1 patient (0.2%) required reverse shoulder arthroplasty over the 10-year follow-up period. At the time of enrollment, this patient had a tear that involved the supraspinatus only, with 25% atrophy and retraction to the middle of the humeral head. The rest of the rotator cuff was normal, and the patient had no arthritis. The patient underwent surgery at 9.5 years after enrollment. In the operative report, the treating surgeon described RCT arthropathy with pseudoparalysis as an indication for the intervention.
If we predict that tear progression occurs in 40% of the population31 and that the rate of progression in those patients is approximately 1 mm/year in the sagittal plane37, then we can assume that in most patients, progression either does not occur or occurs at a rate that would not produce symptoms severe enough to warrant surgery. This presumed rate of progression could explain why operative rates did not increase over time in the present study and why PROMs did not decline among patients with known symptomatic, atraumatic full-thickness RCTs treated nonoperatively.
Limitations
The present study had limitations. First, the findings do not apply to patients with a history of trauma. Second, because only 47% of the eligible patients enrolled in the study, there may have been selection bias as a result of including patients who did not want surgery and excluding patients with more severe symptoms who requested surgery. Third, 9% of the patients died and an additional 9% were lost to follow-up, which may introduce another source of selection bias. Fourth, MRI was not available for patients at later time points in the follow-up period, so we cannot know the true extent of RCT progression and how it may have influenced these findings. Finally, we recognize that in our statistical analysis, some data has relatively wide confidence intervals. This may be an artifact of restricted variation within certain subgroups—even though the overall sample size was large. This may have produced a condition in which the restricted clinical variation caused a limited capacity to assess secondary effects and interactions.
Summary
This large, prospective, multicenter cohort study has shown that the features that predict failure of nonoperative treatment for symptomatic, atraumatic full-thickness RCTs change over time, with low patient expectations regarding the efficacy of physical therapy being a predictor of early surgery (within 6 months) and activity level and Workers’ Compensation status being predictors of later surgery (6 months to 10 years). Physical therapy was an effective treatment for >70% of patients, and the effect was durable to at least 10 years. In patients treated nonoperatively, PROMs did not decline over 10 years. Finally, patients undergoing physical therapy were unlikely to require reverse shoulder arthroplasty over the course of the 10-year follow-up.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJS/I99).
Acknowledgments
Note: Members of the Multicenter Orthopaedic Outcomes Network (MOON) Shoulder Group include John E. Kuhn, MD, MS, Warren R. Dunn, MD, MPH, Rosemary Sanders, BA, Keith M. Baumgarten, MD, Julie Y. Bishop, MD, Robert H. Brophy, MD, James L. Carey, MD, MPH, Brian G. Holloway, MD, Grant L. Jones, MD, C. Benjamin Ma, MD, Robert G. Marx, MD, MS, Eric C. McCarty, MD, Sourav K. Poddar, MD, Matthew V. Smith, MD, Edwin E. Spencer, MD, Armando F. Vidal, MD, Brian R. Wolf, MD, MS, and Rick W. Wright, MD.
Footnotes
Disclosure: This work was funded by the following agencies: Arthrex (unrestricted research gift), NFL Charities (medical research grant); National Institutes of Health (grant 5K23-AR05392-05 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases), American Orthopaedic Society for Sports Medicine (Career Development Award), and Pfizer (Scholars Grant in Clinical Epidemiology). The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJS/I98).
Contributor Information
Warren R. Dunn, Email: dunnwr@me.con.
Rosemary Sanders, Email: rosemary.a.sanders@vumc.org.
Keith M. Baumgarten, Email: kbaumga@yahoo.com.
Julie Y. Bishop, Email: julie.bishop@osumc.edu.
Robert H. Brophy, Email: brophyrh@wustl.edu.
James L. Carey, Email: James.Carey@pennmedicine.upenn.edu.
Brian G. Holloway, Email: brian.holloway@orthotennessee.com.
Grant L. Jones, Email: Grant.Jones@osumc.edu.
C. Benjamin Ma, Email: maben@orthosurg.ucsf.edu.
Robert G. Marx, Email: MarxR@hss.edu.
Sourav K. Poddar, Email: sourav.poddar@ucdenver.edu.
Matthew V. Smith, Email: smithmv@wudosis.wustl.edu.
Edwin E. Spencer, Email: spencershoulder13@gmail.com.
Armando F. Vidal, Email: avidal@thesteadmanclinic.com.
Brian R. Wolf, Email: brian-wolf@uiowa.edu.
Rick W. Wright, Email: rick.w.wright@vumc.org.
Data Sharing
A data-sharing statement is provided with the online version of the article (http://links.lww.com/JBJS/I100).
References
- 1.Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL. National trends in rotator cuff repair. J Bone Joint Surg Am. 2012. Feb 1;94(3):227-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jain NB, Higgins LD, Losina E, Collins J, Blazar PE, Katz JN. Epidemiology of musculoskeletal upper extremity ambulatory surgery in the United States. BMC Musculoskelet Disord. 2014. Jan 8;15:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jeong J, Shin DC, Kim TH, Kim K. Prevalence of asymptomatic rotator cuff tear and their related factors in the Korean population. J Shoulder Elbow Surg. 2017. Jan;26(1):30-5. [DOI] [PubMed] [Google Scholar]
- 4.Minagawa H, Yamamoto N, Abe H, Fukuda M, Seki N, Kikuchi K, Kijima H, Itoi E. Prevalence of symptomatic and asymptomatic rotator cuff tears in the general population: From mass-screening in one village. J Orthop. 2013. Feb 26;10(1):8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tempelhof S, Rupp S, Seil R. Age-related prevalence of rotator cuff tears in asymptomatic shoulders. J Shoulder Elbow Surg. 1999. Jul-Aug;8(4):296-9. [DOI] [PubMed] [Google Scholar]
- 6.Teunis T, Lubberts B, Reilly BT, Ring D. A systematic review and pooled analysis of the prevalence of rotator cuff disease with increasing age. J Shoulder Elbow Surg. 2014. Dec;23(12):1913-21. [DOI] [PubMed] [Google Scholar]
- 7.Yamamoto A, Takagishi K, Kobayashi T, Shitara H, Osawa T. Factors involved in the presence of symptoms associated with rotator cuff tears: a comparison of asymptomatic and symptomatic rotator cuff tears in the general population. J Shoulder Elbow Surg. 2011. Oct;20(7):1133-7. [DOI] [PubMed] [Google Scholar]
- 8.Kuhn JE. Prevalence, Natural History, and Nonoperative Treatment of Rotator Cuff Disease. Oper Tech Sports Med. 2023;31(1):150978. [Google Scholar]
- 9.Parikh N, Martinez DJ, Winer I, Costa L, Dua D, Trueman P. Direct and indirect economic burden associated with rotator cuff tears and repairs in the US. Curr Med Res Opin. 2021. Jul;37(7):1199-211. [DOI] [PubMed] [Google Scholar]
- 10.Seltzer DG, Kechele P, Basmania C, Rockwood CA, Jr. Conservative Management of Rotator Cuff Tears. In: Burkhead WZ, editor. Rotator Cuff Disorders. Philadelphia: Williams & Wilkins; 1996. p 258-67. [Google Scholar]
- 11.Dunn WR, Schackman BR, Walsh C, Lyman S, Jones EC, Warren RF, Marx RG. Variation in orthopaedic surgeons’ perceptions about the indications for rotator cuff surgery. J Bone Joint Surg Am. 2005. Sep;87(9):1978-84. [DOI] [PubMed] [Google Scholar]
- 12.Austin DC, Torchia MT, Lurie JD, Jevsevar DS, Bell JE. Identifying regional characteristics influencing variation in the utilization of rotator cuff repair in the United States. J Shoulder Elbow Surg. 2019. Aug;28(8):1568-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vitale MG, Krant JJ, Gelijns AC, Heitjan DF, Arons RR, Bigliani LU, Flatow EL. Geographic variations in the rates of operative procedures involving the shoulder, including total shoulder replacement, humeral head replacement, and rotator cuff repair. J Bone Joint Surg Am. 1999. Jun;81(6):763-72. [DOI] [PubMed] [Google Scholar]
- 14.Dunn WR, Kuhn JE, Sanders R, An Q, Baumgarten KM, Bishop JY, Brophy RH, Carey JL, Harrell F, Holloway BG, Jones GL, Ma CB, Marx RG, McCarty EC, Poddar SK, Smith MV, Spencer EE, Vidal AF, Wolf BR, Wright RW; MOON Shoulder Group. 2013 Neer Award: predictors of failure of nonoperative treatment of chronic, symptomatic, full-thickness rotator cuff tears. J Shoulder Elbow Surg. 2016. Aug;25(8):1303-11. [DOI] [PubMed] [Google Scholar]
- 15.Kuhn JE, Dunn WR, Sanders R, An Q, Baumgarten KM, Bishop JY, Brophy RH, Carey JL, Holloway BG, Jones GL, Ma CB, Marx RG, McCarty EC, Poddar SK, Smith MV, Spencer EE, Vidal AF, Wolf BR, Wright RW; MOON Shoulder Group. Effectiveness of physical therapy in treating atraumatic full-thickness rotator cuff tears: a multicenter prospective cohort study. J Shoulder Elbow Surg. 2013. Oct;22(10):1371-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ware J, Kosinski M, Keller SDAA. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996. Mar;34(3):220-33. [DOI] [PubMed] [Google Scholar]
- 17.Richards RR, An KN, Bigliani LU, Friedman RJ, Gartsman GM, Gristina AG, Iannotti JP, Mow VC, Sidles JA, Zuckerman JD. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994. Nov;3(6):347-52. [DOI] [PubMed] [Google Scholar]
- 18.Kirkley A, Alvarez C, Griffin S. The development and evaluation of a disease-specific quality-of-life questionnaire for disorders of the rotator cuff: The Western Ontario Rotator Cuff Index. Clin J Sport Med. 2003. Mar;13(2):84-92. [DOI] [PubMed] [Google Scholar]
- 19.Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC. Comparison of the Single Assessment Numeric Evaluation method and two shoulder rating scales. Outcomes measures after shoulder surgery. Am J Sports Med. 1999. Mar-Apr;27(2):214-21. [DOI] [PubMed] [Google Scholar]
- 20.Sangha O, Stucki G, Liang MH, Fossel AH, Katz JN. The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003. Apr 15;49(2):156-63. [DOI] [PubMed] [Google Scholar]
- 21.Brophy RH, Beauvais RL, Jones EC, Cordasco FA, Marx RG. Measurement of shoulder activity level. Clin Orthop Relat Res. 2005. Oct;439(439):101-8. [DOI] [PubMed] [Google Scholar]
- 22.Kuhn JE. Exercise in the treatment of rotator cuff impingement: a systematic review and a synthesized evidence-based rehabilitation protocol. J Shoulder Elbow Surg. 2009. Jan-Feb;18(1):138-60. [DOI] [PubMed] [Google Scholar]
- 23.R Core Team. R: A language and environment for statistical computing. 2023. Accessed 2024 Feb 21. https://www.R-project.org/. [Google Scholar]
- 24.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007. Oct 16;4(10):e296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patte D. Classification of rotator cuff lesions. Clin Orthop Relat Res. 1990. May;(254):81-6. [PubMed] [Google Scholar]
- 26.Furney S, Montez N. The Effects of Pre-Surgical Education on Patient Expectations in Total Knee Arthroplasties. Open J Prev Med. 2015;5:449-55. [Google Scholar]
- 27.Tolk JJ, Janssen RPA, Haanstra TM, van der Steen MC, Bierma-Zeinstra SMA, Reijman M. The influence of expectation modification in knee arthroplasty on satisfaction of patients: a randomized controlled trial. Bone Joint J. 2021. Apr;103-B(4):619-26. [DOI] [PubMed] [Google Scholar]
- 28.Malfliet A, Lluch Girbés E, Pecos-Martin D, Gallego-Izquierdo T, Valera-Calero A. The Influence of Treatment Expectations on Clinical Outcomes and Cortisol Levels in Patients With Chronic Neck Pain: An Experimental Study. Pain Pract. 2019. Apr;19(4):370-81. [DOI] [PubMed] [Google Scholar]
- 29.Analay AY, Kaya Mutlu E, Altun S, Celik D. Does the patients’ expectations on kinesiotape affect the outcomes of patients with a rotator cuff tear? A randomized controlled clinical trial. Clin Rehabil. 2018. Nov;32(11):1509-19. [DOI] [PubMed] [Google Scholar]
- 30.Myers H, Keefe F, George SZ, Kennedy J, Lake AD, Martinez C, Cook C. The influence of a cognitive behavioural approach on changing patient expectations for conservative care in shoulder pain treatment: a protocol for a pragmatic randomized controlled trial. BMC Musculoskelet Disord. 2021. Aug 24;22(1):727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kwong CA, Ono Y, Carroll MJ, Fruson LW, More KD, Thornton GM, Lo IKY. Full-Thickness Rotator Cuff Tears: What Is the Rate of Tear Progression? A Systematic Review. Arthroscopy. 2019. Jan;35(1):228-34. [DOI] [PubMed] [Google Scholar]
- 32.Keener JD, Aleem AW, Chamberlain AM, Sefko J, Steger-May K. Factors associated with choice for surgery in newly symptomatic degenerative rotator cuff tears: a prospective cohort evaluation. J Shoulder Elbow Surg. 2020. Jan;29(1):12-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yamamoto N, Mineta M, Kawakami J, Sano H, Itoi E. Risk Factors for Tear Progression in Symptomatic Rotator Cuff Tears: A Prospective Study of 174 Shoulders. Am J Sports Med. 2017. Sep;45(11):2524-31. [DOI] [PubMed] [Google Scholar]
- 34.Maman E, Harris C, White L, Tomlinson G, Shashank M, Boynton E. Outcome of nonoperative treatment of symptomatic rotator cuff tears monitored by magnetic resonance imaging. J Bone Joint Surg Am. 2009. Aug;91(8):1898-906. [DOI] [PubMed] [Google Scholar]
- 35.Mall NA, Kim HM, Keener JD, Steger-May K, Teefey SA, Middleton WD, Stobbs G, Yamaguchi K. Symptomatic progression of asymptomatic rotator cuff tears: a prospective study of clinical and sonographic variables. J Bone Joint Surg Am. 2010. Nov 17;92(16):2623-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Safran O, Schroeder J, Bloom R, Weil Y, Milgrom C. Natural history of nonoperatively treated symptomatic rotator cuff tears in patients 60 years old or younger. Am J Sports Med. 2011. Apr;39(4):710-4. [DOI] [PubMed] [Google Scholar]
- 37.Moosmayer S, Gärtner AV, Tariq R. The natural course of nonoperatively treated rotator cuff tears: an 8.8-year follow-up of tear anatomy and clinical outcome in 49 patients. J Shoulder Elbow Surg. 2017. Apr;26(4):627-34. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
A data-sharing statement is provided with the online version of the article (http://links.lww.com/JBJS/I100).