Abstract
Background:
Despite evidence that formalized trauma systems enhance patient functional outcomes and decrease mortality rates, there remains a lack of such systems globally. Critical to trauma systems are the equipment, materials, and supplies needed to support care, which vary in availability regionally. The purpose of the present study was to identify essential resources for musculoskeletal trauma care across diverse resource settings worldwide.
Methods:
The modified Delphi method was utilized, with 3 rounds of electronic surveys. Respondents consisted of 1 surgeon with expertise in musculoskeletal trauma per country. Participants were identified with use of the AO Trauma, AO Alliance, Orthopaedic Trauma Association, and European Society for Trauma and Emergency Surgery networks. Respondents rated resources on a Likert scale from 1 (most important) to 9 (least important). The “most essential” resources were classified as those rated ≤2 by ≥75% of the sampled group.
Results:
One hundred and three of 111 invited surgeons completed the first survey and were included throughout the subsequent rounds (representing a 93% response rate). Most participants were fellowship-trained (78%) trauma and orthopaedic surgeons (90%) practicing in an academic setting (62%), and 46% had >20 years of experience. Respondents represented low-income and lower-middle-income countries (LMICs; 35%), upper-middle income countries (UMICs; 30%), and high-income countries (HICs; 35%). The initial survey identified 308 unique resources for pre-hospital, in-hospital, and post-hospital phases of care, of which 71 resources achieved consensus as the most essential. There was a significant difference (p < 0.0167) in ratings between income groups for 16 resources, all of which were related to general trauma care rather than musculoskeletal injury management.
Conclusions:
There was agreement on a core list of essential musculoskeletal trauma care resources by respondents from LMICs, UMICs, and HICs. All significant differences in resource ratings were related to general trauma management. This study represents a first step toward establishing international consensus and underscores the need to prioritize resources that are locally available. The information can be used to develop effective guidelines and policies, create best-practice treatment standards, and advocate for necessary resources worldwide.
Clinical Relevance:
This study utilized the Delphi method representing expert opinion; however, this work did not examine patient management and therefore does not have a clinical Level of Evidence.
Trauma is a leading cause of morbidity and mortality worldwide, with musculoskeletal injury representing a large proportion of this burden overall1,2. According to the World Health Organization (WHO), >4 million deaths are attributed to traumatic injuries annually3. While trauma impacts all populations, injury patterns vary widely by region, disproportionately affecting those in low-income and lower-middle-income countries (LMICs), where 90% of injury-related deaths occur1,4. Unsafe conditions, less access to resources, and lack of standardized treatment efforts contribute to this disparity5. Strategies to address this burden include trauma systems and established guidelines. Despite evidence that coordinated trauma systems enhance functional patient outcomes, decrease mortality rates among treated trauma patients by 15% to 20%, and provide support for improved allocation of resources1,5-7, there remains a lack of formalized systems globally8-10. A recent study indicated that only 29% of surgeons worldwide, and only 50% of those in high-income countries (HICs), reported that their country had a trauma system8. Critical to these systems are the equipment, materials, and supplies needed to deliver musculoskeletal care, which vary in availability regionally. Given the breadth of geographic and economic differences globally, recommendations for trauma care are not always generalizable from higher-income to lower-income countries. Understanding the most high-yield and locally available resources for musculoskeletal injury management across all income groups is necessary for the development of guidelines for trauma care in any given region. Thus, the purpose of the present study was to identify the most essential resources for musculoskeletal trauma care across diverse resource settings worldwide.
Materials and Methods
Modified Delphi Method
A 3-round electronic survey was administered in the English language to a panel of trauma and orthopaedic surgeons with use of the modified Delphi method. This iterative process seeks consensus opinion through a series of surveys among a group of experts. Over the last 2 decades, this method has become an increasingly valuable tool used to enhance decision-making processes in the field of health research11,12. The current study involved 3 survey rounds: (1) an initial survey to identify a list of essential musculoskeletal trauma care resources, (2) a second survey to rate the list of essential resources identified in the initial survey, and (3) a third survey to re-rate the list of the most essential resources identified in the second survey. Feedback on the panel’s aggregate rating was provided during each survey round to help the individual surgeons re-evaluate their own opinions against those of the group.
The group of experts were practicing surgeons in leadership roles (e.g., leaders of professional societies, academic orthopaedic departments, or clinical practices) who treated traumatic musculoskeletal injuries and had knowledge of the status of their country’s trauma systems. All surgeons self-identified as being capable of understanding and completing a survey in the English language. One hundred and eleven surgeon-experts from 111 different countries, representing varying income groups, were invited to participate in the study. These respondents were identified using the AO Trauma, AO Alliance, Orthopaedic Trauma Association (OTA), and European Society for Trauma and Emergency Surgery (ESTES) networks and were recognized as being surgeon-leaders within their countries. Each survey was open for completion for 6 weeks and was administered electronically through REDCap (Research Electronic Data Capture), a secure web-based application for online surveys and databases. The study was approved by the institutional review board at the University of California, San Francisco (UCSF), and participant consent was obtained at the time that the survey was administered.
Delphi Round 1
The purposes of the Round 1 survey were to collect the surgeons’ demographic information and to develop a comprehensive list of resources considered essential for pre-hospital, in-hospital, and post-hospital phases of care for musculoskeletal injury with use of a free-text response field. The panelists were encouraged to identify a minimum of 5 resources for each phase of hospital care.
Delphi Round 2
All free-text responses from the Round 1 survey were compiled and synthesized into appropriate categories and were reviewed by the steering committee, which included a total of 10 trauma and orthopaedic surgeons from Africa, Australasia, Europe, North America, and South America. These responses were subsequently distributed through an electronic survey in which the panelists were asked to review each resource and rate its perceived importance on a 9-point Likert scale (with scores of 1 to 3 being “most important,” 4 to 6 being “moderately important,” and 7 to 9 being “least important”). The steering committee defined “most important” as a resource that should be considered a standard for the surgeon’s national trauma system. In contrast, the steering committee defined “least important” as a resource that should not be included as a standard for the surgeon’s national trauma system. All participants were encouraged to submit any additional resources that were considered of importance and that were not already included after the Round 1 survey.
Delphi Round 3
The overall mean for each resource was scored and listed by category from most important to least important in the electronic survey. Each resource was accompanied by a histogram illustrating the panelists’ average rating. With the knowledge of the group’s responses, the surgeons were invited to reassess their opinions and re-rate each resource against those of the group.
Statistical Analysis and Ranking
The results in the Delphi Round 3 survey were summarized with an aggregate rating. The criterion for the achievement of consensus was initially defined as a rating of 1 to 3 on the Likert scale (“most important”) by ≥75% of panelists, based on a threshold commonly used to define consensus13. However, because of the large number of resources that qualified for inclusion, a post hoc modification was made by the steering committee to set the criterion to a rating of 1 or 2 on the Likert scale with ≥75% agreement among the group. This modification allowed for the identification of only the highest ranked, or most essential, resources.
In addition, a comparison analysis of the surgeons’ ratings was performed across income levels as defined by the 2021 World Bank and Lending Groups data14. Summary statistics were calculated with use of the Wilcoxon rank sum test and the Kruskal-Wallis test, with p < 0.0167 as the significance level (due to a Bonferroni adjustment for the 3 pairwise comparisons among income groups). Adjustments for multiple testing across variables were not performed, as each variable was independent. All analyses were conducted with use of Stata SE (version 17; StataCorp).
Source of Funding
This study was supported by funding from the Wyss Medical Foundation.
Results
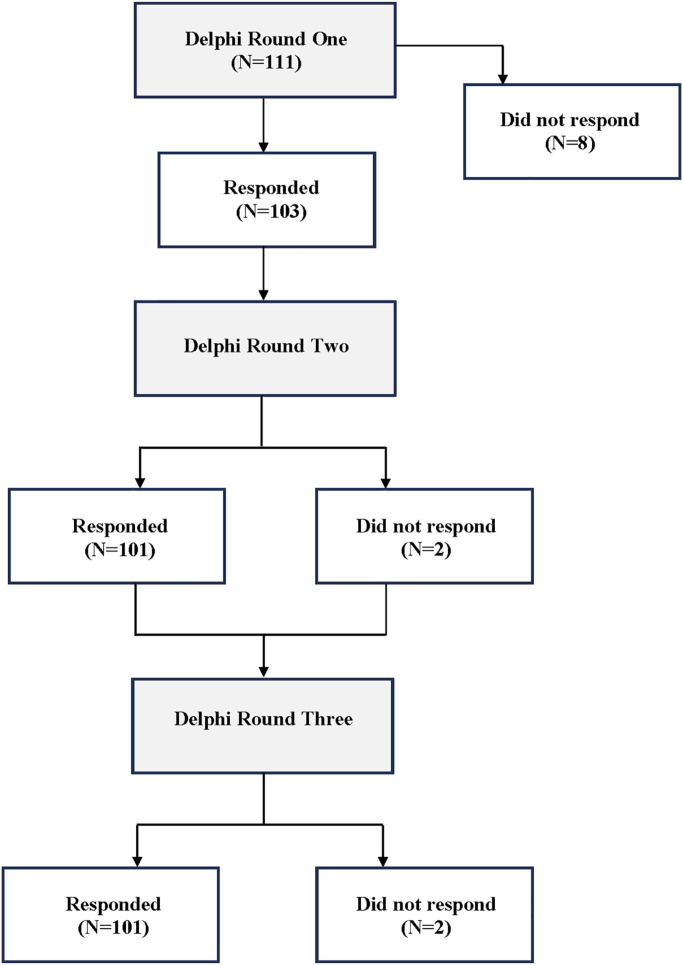
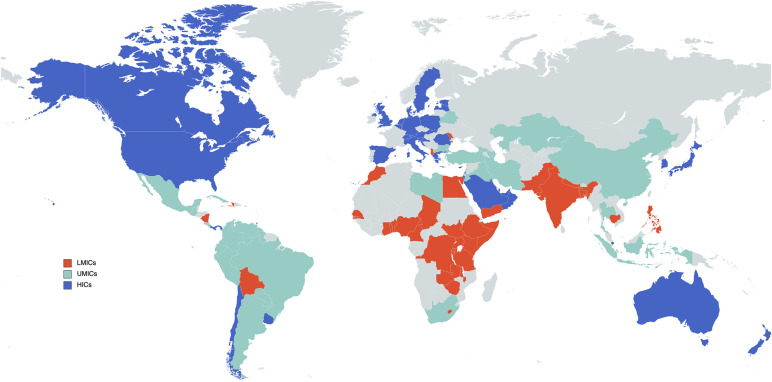
The initial survey was completed by 103 of 111 invited respondents, yielding an overall response rate of 93%. Of these 103 respondents, 101 completed the subsequent 2 survey rounds (Fig. 1). Participants represented countries across all income groups: low-income countries and LMICs (35%), upper-middle income countries (UMICs; 30%), and HICs (35%) (Fig. 2).
Fig. 1.
Flowchart of survey administration and respondents.
Fig. 2.
World map representing respondents’ countries of origin.
Most respondents were fellowship-trained (78%) orthopaedic surgeons (90%) practicing in an academic setting (62%), and 46% had >20 years of experience (Table I). Given the networks from which the participants were selected, few (3%) identified as a surgeon practicing in a specialty other than orthopaedic surgery (e.g., general surgeons who treated trauma and musculoskeletal injuries). The initial survey yielded a total of 308 unique resources for pre-hospital, in-hospital, and post-hospital phases of care (see Appendix). Seventy-one of these resources were identified as “most essential” and were associated with the following categories: pre-hospital care (ancillary services, personnel, and supplies), in-hospital care (training, education, personnel, policies, protocols, supplies, emergency department, operating room, and infrastructure), and post-hospital care (personnel and supplies) (Table II).
TABLE I.
Demographic Data of Surgeon Respondents
| Characteristic | No. of Respondents (N = 103) |
|---|---|
| Training | |
| Orthopaedic surgeon | 93 (90.3%) |
| Fellow (undergoing orthopaedic trauma specialty training) | 7 (6.8%) |
| Other | 3 (2.9%) |
| No. of years in practice | |
| 0-5 | 18 (17.5%) |
| 6-10 | 12 (11.6%) |
| 11-15 | 15 (14.6%) |
| 16-20 | 11 (10.7%) |
| >20 | 47 (45.6%) |
| Fellowship in orthopaedic trauma | |
| Yes | 80 (77.7%) |
| No | 23 (22.3%) |
| Practice setting* | |
| Academic | 64 (62.1%) |
| Private clinic | 47 (45.6%) |
| Public hospital | 31 (30.1%) |
| Other | 3 (2.9%) |
| Country income group | |
| Low-income & lower-middle-income (LMICs) | 36 (35%) |
| Upper-middle-income (UMICs) | 31 (30%) |
| High-income (HICs) | 36 (35%) |
Multiple responses were selected.
TABLE II.
Most Essential Resources Identified Across Income Groups (LMICs, UMICs, and HICs)*
| Overall Mean | LMIC Mean | UMIC Mean | HIC Mean | P Value | |
|---|---|---|---|---|---|
| Pre-hospital phase | |||||
| Ancillary services | |||||
| Ambulance services | 1.53 | 1.53 | 1.73 | 1.37 | 0.30 |
| Emergency medical response system | 1.71 | 1.80 | 1.53 | 1.77 | 0.35 |
| Personnel | |||||
| Quick response team | 1.97 | 2.00 | 2.23 | 1.71 | 0.28 |
| Supplies | |||||
| IV fluids | 1.47 | 1.51 | 1.47 | 1.43 | 0.96 |
| Surgical gloves | 1.49 | 1.69 | 1.50 | 1.29 | 0.25 |
| Cervical collar | 1.52 | 1.54 | 1.47 | 1.54 | 0.57 |
| Resuscitation kit/airway management | 1.53 | 1.77 | 1.73 | 1.20 | 0.05 |
| Pulse oximeter | 1.56 | 1.77 | 1.73 | 1.20 | 0.05 |
| Face mask | 1.61 | 1.66 | 1.77 | 1.42 | 0.69 |
| Life support equipment | 1.67 | 1.60 | 1.93 | 1.51 | 0.30 |
| Spine board | 1.75 | 1.83 | 1.90 | 1.54 | 0.73 |
| Basic dressings | 1.82 | 1.94 | 1.77 | 1.74 | 0.74 |
| Antiseptics/iodine | 1.89 | 1.80 | 1.97 | 1.91 | 0.90 |
| Basic immobilization systems | 1.95 | 1.80 | 2.13 | 1.94 | 0.88 |
| In-hospital phase | |||||
| Training | |||||
| Training OR trauma surgeon | 1.77 | 1.69 | 1.60 | 1.40 | 0.70 |
| Training OR orthopaedic surgeon | 1.83 | 1.61 | 1.60 | 1.48 | 0.48 |
| Training ER staff/nursing | 1.85 | 1.78 | 1.83 | 1.51 | 0.59 |
| Training ER physician | 1.86 | 1.67 | 1.80 | 1.54 | 0.61 |
| Training OR anesthesia | 1.93 | 1.78 | 1.90 | 1.42 | 0.14 |
| Education | |||||
| Advanced trauma life support (ATLS) | 1.76 | 1.63 | 1.77 | 1.34 | 0.35 |
| Continuing medical education (CME) | 1.85 | 1.64 | 2.13 | 1.54 | 0.12 |
| Personnel | |||||
| Anesthesiologist | 1.42 | 1.47 | 1.33 | 1.08 | 0.14 |
| Nursing | 1.75 | 1.96 | 1.67 | 1.54 | 0.50 |
| Radiologist | 1.85 | 1.91 | 1.83 | 1.63 | 0.66 |
| ER physician | 1.85 | 1.89 | 1.97 | 1.77 | 0.23 |
| Orthopaedic trauma surgeon | 1.88 | 1.50 | 1.83 | 1.43 | 0.23 |
| Neurosurgeon | 1.93 | 1.93 | 2.00 | 1.80 | 0.45 |
| Policies | |||||
| 24/7 in-house anesthesiologist | 1.80 | 1.72 | 1.37 | 1.11 | 0.03 |
| 24/7 in-house trauma surgeon | 1.98 | 1.97 | 2.03 | 1.63 | 0.43 |
| Protocols | |||||
| Trauma imaging protocol | 1.80 | 1.83 | 2.10 | 1.34 | 0.14 |
| Preoperative anesthesia assessment | 1.88 | 2.14 | 2.20 | 1.74 | 0.85 |
| Trauma management protocol | 1.90 | 1.75 | 2.07 | 1.43 | 0.43 |
| Trauma triage protocol | 1.95 | 1.64 | 2.20 | 1.37 | 0.15 |
| Musculoskeletal trauma management protocol | 1.98 | 1.80 | 2.10 | 1.60 | 0.64 |
| Pelvic trauma management protocol | 1.98 | 1.69 | 2.07 | 1.48 | 0.48 |
| Operating room surgery triage—urgent cases | 2.00 | 1.97 | 2.20 | 1.37 | 0.13 |
| Multidisciplinary team management | 2.00 | 1.86 | 2.13 | 1.51 | 0.43 |
| Supplies | |||||
| Radiographs | 1.31 | 1.69 | 1.23 | 1.08 | 0.02 |
| Intubation supplies | 1.45 | 1.47 | 1.47 | 1.0 | 0.006† |
| OR equipment | 1.45 | 1.56 | 1.53 | 1.03 | 0.02 |
| Autoclave sterilization | 1.46 | 1.53 | 1.53 | 1.14 | 0.15 |
| Surgical gloves | 1.46 | 1.44 | 1.37 | 1.08 | 0.06 |
| Antibiotics | 1.52 | 1.56 | 1.50 | 1.23 | 0.31 |
| Power equipment | 1.56 | 1.56 | 1.83 | 1.08 | 0.06 |
| Internal fixation—nails | 1.56 | 1.69 | 1.73 | 1.17 | 0.05 |
| CT | 1.58 | 2.03 | 1.40 | 1.08 | 0.003† |
| External fixators | 1.58 | 1.72 | 1.70 | 1.08 | 0.08 |
| Analgesia | 1.59 | 1.56 | 1.70 | 1.14 | 0.01† |
| Dressings | 1.60 | 1.53 | 1.57 | 1.17 | 0.02 |
| Ultrasound | 1.63 | 1.78 | 1.77 | 1.57 | 0.35 |
| Ventilator | 1.65 | 1.69 | 1.70 | 1.03 | 0.006† |
| Internal fixation—plates | 1.69 | 1.89 | 1.63 | 1.14 | 0.24 |
| Splint material | 1.77 | 1.53 | 1.77 | 1.34 | 0.14 |
| Anticoagulants | 1.82 | 2.08 | 1.80 | 1.48 | 0.13 |
| Traction table | 1.86 | 1.80 | 2.03 | 1.23 | 0.05 |
| Radiolucent fracture table | 1.95 | 1.78 | 2.17 | 1.23 | 0.04 |
| Emergency department | |||||
| Procedure room | 1.94 | 1.86 | 2.23 | 1.71 | 0.70 |
| Operating room | |||||
| 24/7 availability trauma | 1.71 | 1.78 | 2.10 | 1.40 | 0.26 |
| OR priority for emergency surgeries | 1.74 | 1.80 | 1.80 | 1.17 | 0.14 |
| Availability trauma | 1.85 | 1.78 | 2.00 | 1.49 | 0.63 |
| 24/7 dedicated availability for musculoskeletal trauma | 1.95 | 1.80 | 2.20 | 1.49 | 0.34 |
| Infrastructure | |||||
| Blood bank | 1.60 | 1.81 | 1.67 | 1.17 | 0.13 |
| Clinical laboratories | 1.66 | 1.81 | 1.87 | 1.40 | 0.35 |
| Reliable power supply | 1.68 | 1.67 | 1.83 | 1.23 | 0.16 |
| Intensive care unit—general | 1.80 | 1.75 | 1.78 | 1.08 | 0.01† |
| Intensive care unit—trauma/surgery | 1.90 | 1.94 | 1.87 | 1.83 | 0.87 |
| Post-hospital phase | |||||
| Personnel | |||||
| Orthopaedic surgeon | 1.77 | 1.69 | 1.93 | 1.54 | 0.39 |
| Supplies | |||||
| Radiographs | 1.44 | 1.50 | 1.53 | 1.14 | 0.05 |
| Analgesia | 1.77 | 1.61 | 1.97 | 1.26 | 0.07 |
| Antibiotics | 1.81 | 1.64 | 1.80 | 1.66 | 0.58 |
| Dressings | 1.89 | 1.80 | 2.07 | 1.34 | 0.05 |
Resources rated ≤2 with consensus by ≥75% of the group. IV = intravenous, OR = operating room, ER = emergency room, CT = computed tomography.
Significantly different between income groups (p < 0.0167).
Comparison Between Income Groups
Among the full list of 308 resources identified, there were significant differences (p < 0.0167) in ratings between income groups (LMICs, UMICs, and HICs) for 16 resources, which were designated under the following categories: pre-hospital care (ancillary services and infrastructure), in-hospital care (personnel, research, supplies, and infrastructure), and post-hospital care (community education). These resources included air medical access, general and psychiatric practitioners, advanced imaging, and anesthesia-related supplies and equipment (ventilator, intubation supplies, analgesia) (Table III).
TABLE III.
Significant Differences in Ratings Between Income Groups (LMICs, UMICs, HICs)*
| Resource | LMIC Mean | UMIC Mean | HIC Mean | P Value |
|---|---|---|---|---|
| Pre-hospital phase | ||||
| Ancillary services | ||||
| Air medical airplane/helicopter services | 5.33 | 3.83 | 3.09 | <0.001 |
| Infrastructure | ||||
| Internet access | 2.60 | 2.47 | 1.51 | 0.01 |
| In-hospital phase | ||||
| Personnel | ||||
| Research assistant | 3.05 | 4.13 | 4.34 | 0.01 |
| General practitioner | 3.22 | 3.70 | 4.60 | 0.008 |
| Psychiatrist | 3.61 | 4.67 | 4.77 | 0.01 |
| Psychologist | 3.44 | 4.93 | 4.83 | 0.001 |
| Research | ||||
| Basic research | 2.72 | 4.13 | 4.23 | 0.003 |
| Supplies | ||||
| Intubation supplies | 1.47 | 1.47 | 1.00 | 0.006 |
| CT | 2.03 | 1.40 | 1.08 | 0.003 |
| Analgesia | 1.56 | 1.70 | 1.14 | 0.01 |
| Ventilator | 1.69 | 1.70 | 1.03 | 0.006 |
| Skin grafting equipment | 2.0 | 3.07 | 1.91 | 0.004 |
| Infrastructure | ||||
| Intensive care unit—general | 1.75 | 1.78 | 1.08 | 0.01 |
| CT imaging proximity to ED | 2.40 | 2.27 | 1.37 | 0.01 |
| 24/7 angiography suite | 3.42 | 3.03 | 2.00 | 0.002 |
| Post-hospital phase | ||||
| Community education | ||||
| Short-term housing | 3.67 | 4.63 | 3.40 | 0.01 |
Out of the total of 308 resources identified. CT = computed tomography, ED = emergency department.
In all 3 phases of care, surgeons from lesser-resourced countries rated most of these resources as having significantly lower priority relative to those from higher-resourced countries. One exception was seen in the in-hospital personnel category; these personnel included research assistants, general practitioners, psychiatrists, and psychologists. Another exception was in the basic-research category.
Discussion
Trauma care is largely dependent on the organization of services as well as on highly resource-dependent variables, including the availability of specialists and access to essential supplies15. The number of orthopaedic and traumatology specialists per capita ranges substantially across income groups, with the number of surgeons providing care for musculoskeletal injuries being estimated at 2.6 per 1 million inhabitants in LMICs and 58.8 per 1 million inhabitants in HICs8. Similarly, there are disparities in the equipment, materials, and supplies needed to support musculoskeletal trauma care across different regional economies that further impact injury management, although the specific resources required for this care are not well documented16,17. Higashi et al. estimated that in LMICs, 21% of the morbidity and mortality due to injuries is potentially modifiable with the establishment of basic trauma care provisions18, underscoring the importance of identifying the most high-yield resources for musculoskeletal care.
In the present study, consensus was reached on 71 items that were considered to be “most essential” by the expert panel across all income groups, suggesting that these are widely regarded as the most basic of required resources. Significant differences were observed in 16 resources, all related to general trauma management and not musculoskeletal injury care, further demonstrating consensus on essential musculoskeletal resources across regions. The most essential resources that were identified should be considered for inclusion in guidelines. Many LMICs often do not have the supplies and equipment recommended in trauma care protocols. Therefore, many LMIC providers only refer to guidelines for needs assessments, advocacy, and policy development purposes, with a minority implementing these recommendations10,19. This suggests that the recommended use of locally available resources is critical for effective guidelines20-22. The differences in ratings by surgeons in the present study were likely reflective of the availability of the current resources in their respective countries. Resources such as air medical services and internet access, both ranked as highly important among surgeons in HICs and UMICs, were rated substantially lower by surgeons in LMICs. Similarly, more-advanced technological resources that are more accessible in resource-rich countries, such as computed tomography (CT) suites and 24/7 (always available) angiography suites, also were ranked differently by surgeons across income groups. Among the list of most essential resources, surgeons from HICs ranked specialized medical personnel higher than those from LMICs and UMICs. Notably, surgeons from LMICs and UMICs rated primary health-care personnel as being more important than did surgeons from HICs, perhaps indicating that primary-care providers play a more substantial role in resource-limited settings. These findings support the importance of prioritizing locally available equipment and services for the development of effective guidelines23,24.
In an effort to improve trauma care quality, the American College of Surgeons (ACS) Task Force of the Committee on Trauma developed a list of essential and desirable provisions considered to be important for trauma care (pre-hospital to post-hospital), with an emphasis on surgeons and patients in rural settings21. Subsequently, Mock et al., in collaboration with the World Health Organization, established the Essential Trauma Care (EsTC) Project in 2004, which recommended affordable supplies and equipment, specifically for LMICs6,22. The list of recommendations addressed general trauma surgical services, including basic resuscitation, airway management, and hemorrhage control. While the EsTC Project has made progress in implementing locally relevant recommendations across sites in LMICs6, it was focused on countries within a specific economic group and on general trauma care (rather than comprehensive musculoskeletal injury management). In 2018, Chan et al. conducted a Delphi study to develop recommendations for an essential list of trauma and orthopaedic equipment for nonoperative, specialist, and tertiary providers across LMICs in Africa24. The current study expands on that work and includes 3 phases of care, identifying additional resource categories (i.e., personnel, education, policies, protocols).
The present study had several potential limitations. Although >300 unique resources were reported by the expert panel, it is highly likely that there were additional items—particularly, more basic supplies, such as sutures—that were not identified in the study. In addition, for the purposes of identifying a list of resources that were considered to be “most important,” a post hoc modification was made with a more stringent set of criteria. By doing so, some key resources may not have been identified in the “most essential” category. These essential resources could be considered more prominently, but not exclusively, for recommended guidelines. Furthermore, as the survey was designed in the English language, this may have limited the participants’ responses. Additionally, while >70% of the respondents had >10 years of experience, the remainder had fewer years of experience and may not have had the same level of knowledge as their counterparts. Finally, although employing a larger sample size than most Delphi studies13, the present study sought to have sufficiently broad geographical and economical representation for comparison between income groups6. The selection of 1 surgeon-expert per country provided for this greater overview; however, a single surgeon would not be representative of an entire country or region, within which substantial variations in socioeconomic conditions may exist. Further investigation is therefore necessary to evaluate and validate resource criteria that are unique to specific regions; the findings from this study could be used as a basis for those investigations.
In summary, resource availability is critical for the successful development of trauma systems and the delivery of musculoskeletal trauma care. In the present study, survey respondents from LMICs, UMICs, and HICs achieved agreement on a core list of essential musculoskeletal trauma care resources. The results of this study underscore the need to prioritize resources that are locally available in any given setting rather than those that are not accessible. This study represents a first step toward establishing international consensus. The information can be used to develop effective guidelines and policies, create best-practice treatment standards, and advocate for necessary resources worldwide.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJS/H697).
Acknowledgments
Note: We would like to recognize our colleagues from the Delphi Study Group.
Members of the Delphi Study Group include Anani G. Abalo, MD; Ephrem Adem, MD; Dino Aguilar, MD; Waleed A. Al-Saadan, MD; Mohammed Alsaifi, MD; Rafael Amadei, MD; Theerachai Apivatthakakul, MD; Mapuor M. Mading Areu, MD; Federico Bove, MD; Rastislav Burda, MD; Alex M. Butera, MD; Linda C. Chokotho, MD; Alvaro Cordero, MD; Adel Ebrahimpour, MD; John Ekure, MD; Igor A. Escalante, MD; Osama Farouk, MD; Christos Garnavos, MD, PhD, FIOTA; Mario Garuz, MD; Florian Gebhard, MD, PhD; Andres Gelink, MD; Torsten G. Gerich, MD; Wojciech M. Glinkowski MD, PhD; Paata Gudushauri, MD, PhD; Enrique Guerado, MD; Billy T. Haonga, MD; Yazan J. Hattar, MD; Zekeriya Ugur Isiklar, MD; Rishi Jagdeo MD, MB, BS, MSc, MBA, LLM; Fareed H.Y. Kagda, MD, FRCS; Radko Komadina, MD; Arjun Lamichhane, MD, MS; Jean Pierre F. Leung, MD; Florent Anicet Lekina, MD; Esther M.M. Van Lieshout, PhD, MSc; Biser Makelov, MD, PhD; Kebba S. Marenah, MD; Konstantinos Michail, MD, MSc; Anna N. Miller, MD; Sayid Omar Mohamed, MD; Younes El Moudni, MD; Walid Mugla, MD; Josep Maria Muñoz-Vives, MD; James Munthali, MD; Thomas Nau, MD; Pierre Navarre, MD, FRACS; Horacio Tabares Neyra, MD; Reuben K.S. Ngissa, MD, MBChB(UG), FGCS(Ortho); Tomoyuki Noda, MD, PhD; Hermann Oberli, MD; Gerald Oguzie, MD; Elchin Orujov, MD; Luis G. Padilla, MD; Hans-Christoph Pape, MD; Col. Narayan Ramachandran, MD, MS, MSc, PCLC; Victor A. de Ridder, MD, PhD; Iván Salce, MD; Ulf Schmidt, MD; Emil H. Schemitsch, MD; Daniele Sciuto, MD; Julio Segovia, MD; Edvin Selmani MD, PhD; Fandebnet Siniki, MD; Alexandre Sitnik, MD, PhD; Andrey Smirnov, MD; Huot Socheat, MD; Darko Talevski, MD; Igors Terjajevs, MD; Kighoma K. Vuhaka, MD; Yoram A. Weil, MD; Olof Wolf, MD, PhD; and Pierre M. Woolley, MD.
Footnotes
A list of the Delphi Study Group members is included as a note at the end of this article.
Investigation performed at Zuckerberg San Francisco General Hospital, University of California San Francisco, San Francisco, California
Disclosure: The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJS/H696).
Contributor Information
Collaborators: Anani G. Abalo, Ephrem Adem, Dino Aguilar, Waleed A. Al-Saadan, Mohammed Alsaifi, Rafael Amadei, Theerachai Apivatthakakul, Mapuor M. Mading Areu, Federico Bove, Rastislav Burda, Alex M. Butera, Linda C. Chokotho, Alvaro Cordero, Adel Ebrahimpour, John Ekure, Igor A. Escalante, Osama Farouk, Christos Garnavos, Mario Garuz, Florian Gebhard, Andres Gelink, Torsten G. Gerich, Wojciech M. Glinkowski, Paata Gudushauri, Enrique Guerado, Billy T. Haonga, Yazan J. Hattar, Zekeriya Ugur Isiklar, Rishi Jagdeo, Fareed H.Y. Kagda, Radko Komadina, Arjun Lamichhane, Jean Pierre F. Leung, Florent Anicet Lekina, Esther M.M. Van Lieshout, Biser Makelov, Kebba S. Marenah, Konstantinos Michail, Anna N. Miller, Sayid Omar Mohamed, Younes El Moudni, Walid Mugla, Josep Maria Muñoz-Vives, James Munthali, Thomas Nau, Pierre Navarre, Horacio Tabares Neyra, Reuben K.S. Ngissa, Tomoyuki Noda, Hermann Oberli, Gerald Oguzie, Elchin Orujov, Luis G. Padilla, Hans-Christoph Pape, Col. Narayan Ramachandran, Victor A. de Ridder, Iván Salce, Ulf Schmidt, Emil H. Schemitsch, Daniele Sciuto, Julio Segovia, Edvin Selmani, Fandebnet Siniki, Alexandre Sitnik, Andrey Smirnov, Huot Socheat, Darko Talevski, Igors Terjajevs, Kighoma K. Vuhaka, Yoram A. Weil, Olof Wolf, and Pierre M. Woolley
References
- 1.Krug EG, Sharma GK, Lozano R. The global burden of injuries. Am J Public Health. 2000. Apr;90(4):523-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006. May 27;367(9524):1747-57. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Injuries and Violence: The Facts. 2014. Accessed 2023 Aug 9. https://apps.who.int/iris/bitstream/handle/10665/149798/9789241508018_eng.pdf. [Google Scholar]
- 4.Haagsma JA, Graetz N, Bolliger I, Naghavi M, Higashi H, Mullany EC, Abera SF, Abraham JP, Adofo K, Alsharif U, Ameh EA, Ammar W, Antonio CA, Barrero LH, Bekele T, Bose D, Brazinova A, Catalá-López F, Dandona L, Dandona R, Dargan PI, De Leo D, Degenhardt L, Derrett S, Dharmaratne SD, Driscoll TR, Duan L, Petrovich Ermakov S, Farzadfar F, Feigin VL, Franklin RC, Gabbe B, Gosselin RA, Hafezi-Nejad N, Hamadeh RR, Hijar M, Hu G, Jayaraman SP, Jiang G, Khader YS, Khan EA, Krishnaswami S, Kulkarni C, Lecky FE, Leung R, Lunevicius R, Lyons RA, Majdan M, Mason-Jones AJ, Matzopoulos R, Meaney PA, Mekonnen W, Miller TR, Mock CN, Norman RE, Orozco R, Polinder S, Pourmalek F, Rahimi-Movaghar V, Refaat A, Rojas-Rueda D, Roy N, Schwebel DC, Shaheen A, Shahraz S, Skirbekk V, Søreide K, Soshnikov S, Stein DJ, Sykes BL, Tabb KM, Temesgen AM, Tenkorang EY, Theadom AM, Tran BX, Vasankari TJ, Vavilala MS, Vlassov VV, Woldeyohannes SM, Yip P, Yonemoto N, Younis MZ, Yu C, Murray CJ, Vos T. The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Inj Prev. 2016. Feb;22(1):3-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mock C, Joshipura M, Goosen J, Lormand JD, Maier R. Strengthening trauma systems globally: the Essential Trauma Care Project. J Trauma. 2005. Nov;59(5):1243-6. [DOI] [PubMed] [Google Scholar]
- 6.Mock C, Nguyen S, Quansah R, Arreola-Risa C, Viradia R, Joshipura M. Evaluation of Trauma Care capabilities in four countries using the WHO-IATSIC Guidelines for Essential Trauma Care. World J Surg. 2006. Jun;30(6):946-56. [DOI] [PubMed] [Google Scholar]
- 7.Nathens AB, Jurkovich GJ, Rivara FP, Maier RV. Effectiveness of state trauma systems in reducing injury-related mortality: a national evaluation. J Trauma. 2000. Jan;48(1):25-30. [DOI] [PubMed] [Google Scholar]
- 8.Miclau T, Hoogervorst P, Shearer DW, El Naga AN, Working ZM, Martin C, Pesántez R, Hüttl T, Kojima KE, Schütz M; International Orthopaedic Trauma Study Consortium. Current Status of Musculoskeletal Trauma Care Systems Worldwide. J Orthop Trauma. 2018. Oct;32(10)(Suppl 7):S64-70. [DOI] [PubMed] [Google Scholar]
- 9.Dijkink S, Nederpelt CJ, Krijnen P, Velmahos GC, Schipper IB. Trauma systems around the world: A systematic overview. J Trauma Acute Care Surg. 2017. Nov;83(5):917-25. [DOI] [PubMed] [Google Scholar]
- 10.LaGrone L, Riggle K, Joshipura M, Quansah R, Reynolds T, Sherr K, Mock C. Uptake of the World Health Organization’s trauma care guidelines: a systematic review. Bull World Health Organ. 2016. Aug 1;94(8):585-598C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jones J, Hunter D. Consensus methods for medical and health services research. BMJ. 1995. Aug 5;311(7001):376-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. 2000. Oct;32(4):1008-15. [PubMed] [Google Scholar]
- 13.Diamond IR, Grant RC, Feldman BM, Pencharz PB, Ling SC, Moore AM, Wales PW. Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol. 2014. Apr;67(4):401-9. [DOI] [PubMed] [Google Scholar]
- 14.The World Bank. Data: World Bank Country and Lending Groups 2021. 2021. Accessed 2023 Aug 9. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
- 15.World Health Organization. Global Status Report on Noncommunicable Diseases 2010. 2011. Accessed 2023 Aug 9. https://apps.who.int/iris/bitstream/handle/10665/44579/9789240686458_eng.pdf.
- 16.Mock CN. The Global Burden of Musculoskeletal Injuries: Challenges and Solutions. Clin Orthop Relat Res. 2008;466(10):2306-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gosselin RA, Spiegel DA, Coughlin R, Zirkle LG. Injuries: the neglected burden in developing countries. Bull World Health Organ. 2009. Apr;87(4):246-246a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Higashi H, Barendregt JJ, Kassebaum NJ, Weiser TG, Bickler SW, Vos T. Burden of injuries avertable by a basic surgical package in low- and middle-income regions: a systematic analysis from the Global Burden of Disease 2010 Study. World J Surg. 2015. Jan;39(1):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Choi J, Carlos G, Nassar AK, Knowlton LM, Spain DA. The Impact of Trauma Systems on Patient Outcomes. Curr Probl Surg. 2021;58:1-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Turner J, Duffy S. Orthopaedic and trauma care in low-resource settings: the burden and its challenges. Int Orthop. 2022. Jan;46(1):143-52. [DOI] [PubMed] [Google Scholar]
- 21.Resources for optimal care of the injured patient: an update. Task Force of the Committee on Trauma, American College of Surgeons. Bull Am Coll Surg. 1990. Sep;75(9):20-9. [PubMed] [Google Scholar]
- 22.Mock C, Joshipura M, Goosen J, Maier R. Overview of the Essential Trauma Care Project. World J Surg. 2006. Jun;30(6):919-29. [DOI] [PubMed] [Google Scholar]
- 23.Mock C, Lormand JD, Goosen J, Joshipura M, Peden M. Guidelines for Essential Trauma Care. 2004. Accessed 2023 Aug 9. https://apps.who.int/iris/bitstream/handle/10665/42565/9241546409_eng.pdf;sequence=1.
- 24.Chan Y, Banza L, Martin C, Jr, Harrison WJ. Essential fracture and orthopaedic equipment lists in low resource settings: consensus derived by survey of experts in Africa. BMJ Open. 2018. Sep 17;8(9):e023473. [DOI] [PMC free article] [PubMed] [Google Scholar]