Abstract
Background
The long-term health effects of assisted reproductive technologies, including in vitro fertilization (IVF) and hormonal therapies, remain poorly understood. This highlights the need to investigate potential chronic conditions that may arise following treatment.
Objective
The objective of this study was to investigate the long-term effects of fertility treatments on maternal health, with a focus on the incidence of chronic conditions and overall health outcomes in women who have undergone such treatments.
Methodology
This cross-sectional study included 180 women, aged 20-45, who had received fertility treatments and successfully delivered a live child. The research was conducted at Rehman Medical Institute and Hayatabad Medical Complex in Peshawar, Pakistan, from January to December 2023. Data were collected through medical record reviews and structured interviews to assess long-term health outcomes, including cancer, metabolic disorders, and cardiovascular diseases. Descriptive statistics and logistic regression were applied using IBM SPSS Statistics for Windows, Version 25.0 (Released 2017; IBM Corp., Armonk, NY, USA), with a significance threshold set at p < 0.05.
Results
The study included 180 participants with an average age of 34.5 years. Among them, 73 (40.56%) underwent hormone therapy, 81 (45.00%) used IVF, and 26 (14.44%) used intracytoplasmic sperm injection. All participants delivered live births, with 21 (11.67%) experiencing premature deliveries and 33 (18.33%) having multiple pregnancies. Key findings showed that nine (5.00%) developed cancer, 31 (17.22%) had metabolic disorders, and 24 (13.33%) developed cardiovascular disease. Overall, 146 (81.11%) participants reported excellent long-term health, while 34 (18.89%) had new diagnoses, including 12 (6.67%) with cardiovascular disease, 18 (10.00%) with metabolic disorders, and four (2.22%) with cancer. Additionally, 36 (20.00%) had preeclampsia, 21 (12.00%) experienced OHSS, and 12 (7.00%) developed gestational diabetes.
Conclusions
Despite most participants reporting excellent overall health, the study underscores the need for ongoing monitoring and management, as it reveals significant long-term health risks associated with fertility treatments.
Keywords: assisted reproductive technologies, cancer, cardiovascular disease, chronic conditions, fertility treatment, hormonal therapies, ivf, long-term health effects, maternal health, metabolic disorders
Introduction
Due to the increasing number of couples facing difficulties conceiving naturally, fertility treatments are becoming more common [1]. These treatments, ranging from modern assisted reproductive technologies (ARTs) such as in vitro fertilization (IVF) to hormone therapies like gonadotropins and other medications that stimulate ovarian function and ovulation, have given hope to many individuals and couples wishing to start a family [2]. The popularity and success of these procedures have led to significant advances in reproductive medicine, enhancing accessibility and success rates [3]. However, the potential long-term health consequences for mothers undergoing these treatments are often overshadowed by the immediate focus on pregnancy outcomes [4].
Given the complex hormonal and physiological changes induced by fertility treatments, maternal health has become a critical area of research [5]. Most reproductive treatments involve hormonal therapies, which are associated with several short-term side effects, including weight gain, mood swings, and ovarian hyperstimulation syndrome (OHSS) [6]. While the acute effects are well-documented and generally manageable, there is growing concern over potential long-term health issues, such as metabolic disorders, increased cancer risk, and cardiovascular complications [7]. These concerns highlight the need for a comprehensive understanding of the long-term impact of fertility treatments on maternal health [8].
Current research predominantly focuses on the safety and efficacy of fertility treatments in achieving successful pregnancies, with less attention given to the long-term health effects on mothers [9]. Studies have indicated that health trajectories in women using ART may differ from those in women conceiving naturally [10]. For instance, some evidence suggests a higher prevalence of gestational diabetes, preeclampsia, and other pregnancy-related complications among women undergoing ART [11,12]. However, the long-term effects on chronic conditions, such as metabolic syndromes and cardiovascular diseases, remain insufficiently explored, necessitating more in-depth longitudinal studies [13,14].
Despite advances in fertility treatment and short-term success rates, a clear gap exists in research concerning the long-term effects of these therapies on maternal health. Many studies lack comprehensive health assessments and extended follow-up periods, limiting our understanding of the potential risks and outcomes that may arise years after treatment.
Objective
The objective of this study was to investigate the long-term effects of fertility treatments on maternal health, with a focus on the incidence of chronic conditions and overall health outcomes in women who have undergone these treatments.
Materials and methods
Study design and settings
This cross-sectional study was conducted at Rehman Medical Institute and Hayatabad Medical Complex in Peshawar, Pakistan, over a one-year period from January to December 2023.
Inclusion and exclusion criteria
The study included women aged 20-45 who had received fertility treatments between 2018 and 2022 and successfully conceived a live child. Exclusion criteria included women with prior chronic diseases before undergoing fertility treatments, those who had received repeated reproductive treatments at various institutions, or those who had not provided informed consent.
Sample size
The study involved 180 women who met the inclusion criteria. The sample size was determined based on the availability of eligible volunteers and the scope of the study.
Data collection
Data were collected through two methods: reviewing medical records and conducting structured interviews. Medical records provided details on the type of fertility treatment received, the duration of treatment, and the outcomes of the first pregnancy. Structured interviews were conducted to assess long-term health outcomes, including the prevalence of chronic conditions such as cancer, metabolic disorders, and cardiovascular diseases. Participants were also asked about their general health and any new diagnoses following fertility treatment.
Statistical analysis
Data analysis was conducted using IBM SPSS Statistics for Windows, Version 25.0 (Released 2017; IBM Corp., Armonk, NY, USA). Descriptive statistics, including means, medians, and standard deviations, were calculated for continuous variables. Categorical variables were represented using frequencies and percentages. Logistic regression analysis was employed to identify potential risk factors associated with long-term health outcomes, with a significance threshold set at p < 0.05.
Ethical approval
Ethical approval for the research was granted by the Ethical Review Board of Rehman Medical Institute. All participants provided written informed consent before being included in the study. They were assured of their right to withdraw from the study at any time without facing any repercussions, and measures were taken to ensure the confidentiality and privacy of their data.
Results
Table 1 presents the demographic profile of the 180 participants in the study. The participants had a mean age of 34.5 years (SD ± 5.6), with the age distribution as follows: 46 participants (25.56%) were aged 20-29 years, 81 participants (45.00%) were aged 30-39 years, and 53 participants (29.44%) were aged 40-45 years. All participants were married. Regarding educational attainment, 89 participants (49.44%) held a bachelor’s degree, 57 participants (31.67%) had a master’s degree, 13 participants (7.22%) possessed a PhD, and 21 participants (11.67%) had completed high school.
Table 1. Demographic characteristics of study participants.
| Characteristic | Number of patients (n) | Percentage (%) | |
| Age (years) | 20-29 | 46 | 25.56 |
| 30-39 | 81 | 45 | |
| 40-45 | 53 | 29.44 | |
| Mean ± SD | 34.5 ± 5.6 | ||
| Marital status | Married | 180 | 100 |
| Educational level | High school | 21 | 11.67 |
| Bachelor’s degree | 89 | 49.44 | |
| Master’s degree | 57 | 31.67 | |
| Doctorate | 13 | 7.22 | |
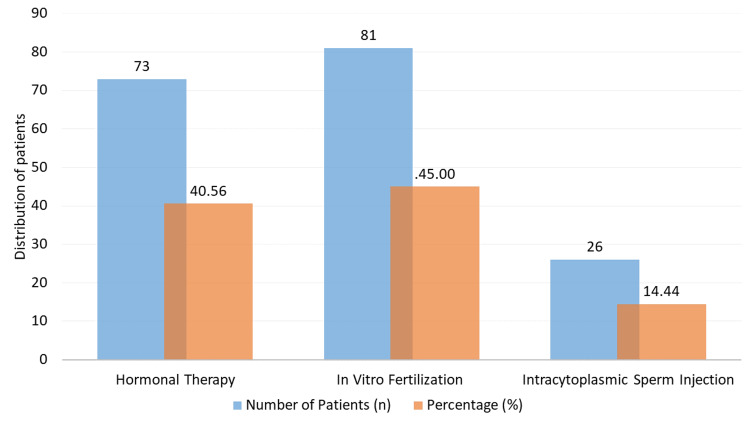
Figure 1 illustrates the distribution of fertility treatment modalities among the 180 participants. Among the sample, 40.56% (73 patients) underwent hormonal therapy, while IVF was the most commonly used treatment, accounting for 45.00% (81 individuals) of the total. Additionally, 14.44% of the participants (26 individuals) received intracytoplasmic sperm injection (ICSI).
Figure 1. Distribution of fertility treatment types.
Out of the 180 patients, 33 (18.33%) experienced multiple pregnancies, indicating the presence of more than one fetus, representing 100% of the sample. Notably, all 180 patients achieved a live birth (Figure 2). Additionally, 21 patients (11.67%) delivered before 37 weeks of gestation, which is classified as preterm birth.
Figure 2. Immediate pregnancy outcomes following fertility treatments.
Table 2 presents the incidence of chronic diseases among the 180 patients following therapy. Among the sample, 24 individuals (13.33%) reported having cardiovascular disease. Additionally, 31 patients (17.22%) were diagnosed with metabolic disorders. Cancer was reported in nine patients (5.00%), including cases of breast, prostate, and colorectal cancers. Furthermore, 116 individuals (64.44%) reported having no ongoing medical issues.
Table 2. Post-treatment incidence of chronic conditions.
| Condition | Number of patients (n) | Percentage (%) |
| Cardiovascular disease | 24 | 13.33 |
| Metabolic disorder | 31 | 17.22 |
| Cancer | 9 | 5 |
| No chronic condition | 116 | 64.44 |
The prevalence of pregnancy-related complications among the 180 patients is detailed as follows: 36 individuals (20.00%) reported experiencing gestational diabetes. Additionally, 21 patients (12.00%) were diagnosed with preeclampsia, while 12 individuals (7.00%) had OHSS. Furthermore, 111 individuals (61.00%) reported having no complications related to pregnancy (Figure 3).
Figure 3. Prevalence of pregnancy-related complications.
Table 3 compares the frequency of chronic diseases across different reproductive therapies. Among the 73 individuals receiving hormone therapy, 10 (13.70%) had metabolic disorders, 12 (16.44%) had cardiovascular disease, five (6.85%) had cancer, and 46 (63.01%) reported no chronic illnesses. In the group undergoing IVF (n = 81), 52 patients (64.20%) had no chronic illnesses, while 11 patients (13.58%) had cardiovascular disease, 15 (18.52%) had metabolic disorders, and three (3.70%) had cancer. Among the 26 patients who underwent ICSI, 18 (69.23%) reported no chronic illnesses, while three (11.54%) had cardiovascular disease, four (15.38%) had metabolic disorders, and one (3.85%) had cancer.
Table 3. Comparison of chronic conditions by type of fertility treatment.
| Condition | Hormonal therapy (n = 73) | IVF (n = 81) | ICSI (n = 26) | p-value |
| Cardiovascular disease | 10 (13.70%) | 11 (13.58%) | 3 (11.54%) | 0.918 |
| Metabolic disorder | 12 (16.44%) | 15 (18.52%) | 4 (15.38%) | 0.731 |
| Cancer | 5 (6.85%) | 3 (3.70%) | 1 (3.85%) | 0.558 |
| No chronic condition | 46 (63.01%) | 52 (64.20%) | 18 (69.23%) | 0.408 |
Table 4 presents the new diagnoses and long-term health status of the 180 patients. A total of 146 patients (81.11%) reported being in overall good health, while 34 patients (18.89%) received a new diagnosis. Among these new diagnoses, 12 patients (6.67%) were identified with metabolic disorders, 18 patients (10.00%) with cardiovascular disease, and four patients (2.22%) with cancer.
Table 4. Long-term health status and new diagnoses.
| Variable | Number of patients (n) | Percentage (%) | |
| Health status | Overall good health | 146 | 81.11 |
| New diagnosis | 34 | 18.89 | |
| Types of new diagnosis | Cardiovascular disease | 12 | 6.67 |
| Metabolic disorders | 18 | 10 | |
| Cancer | 4 | 2.22 | |
Discussion
The long-term health outcomes of fertility treatments have garnered increasing attention as more individuals and couples seek these interventions to achieve pregnancy. This research examined several aspects of post-treatment maternal health, yielding both anticipated and unexpected results.
According to our findings, 64.44% of patients reported no chronic diseases, while 13.33% had cardiovascular disease, 17.22% had metabolic disorders, and 5.00% had cancer. These results are consistent with several other studies indicating a higher risk of metabolic and cardiovascular disorders following reproductive treatments [15]. For instance, research by Rossberg et al. [16] found that women who underwent ART had an elevated cardiovascular risk, underscoring the need for long-term monitoring. Additionally, the incidence of metabolic diseases aligns with a study conducted by Udell et al. [15], which revealed that women who underwent reproductive treatments had a higher likelihood of developing metabolic syndrome.
In terms of pregnancy-related complications, 20.00% of patients experienced gestational diabetes, 12.00% had preeclampsia, and 7.00% had OHSS. These rates are somewhat similar to those reported by Wang et al. [11], who noted a significant prevalence of preeclampsia and gestational diabetes among patients receiving antiretroviral therapy. However, the incidence of OHSS in our study was lower than that observed in the study by Sun et al. [17], which could be attributed to variations in patient management techniques or treatment regimens.
When comparing the incidence of cardiovascular disease across different reproductive treatments, it was found to be 13.70% for hormonal therapy, 13.58% for IVF, and 11.54% for ICSI. No significant differences were noted among these groups. This finding is consistent with the research of Dumanski and Ahmed [18], which reported comparable incidences of chronic illnesses across various ART regimens. However, other studies, such as those conducted by Bunting et al. [1], have shown potential variations in long-term outcomes based on specific treatment modalities, despite our data indicating no discernible differences among treatment types.
In terms of long-term health, 81.11% of patients reported being in excellent overall health, while 18.89% received a new diagnosis. Among these new diagnoses, 6.67% were related to cardiovascular disease, 10% to metabolic disorders, and 2.22% to cancer. Although a substantial proportion of patients are in good health, these findings underscore the importance of ongoing surveillance for chronic conditions, as highlighted by Talaulikar and Arulkumaran [19], who emphasized the necessity of long-term health monitoring in ART patients to address emerging health concerns.
In summary, this research contributes to the growing body of knowledge regarding the long-term health effects of reproductive therapies. The observed patterns and comparisons with existing literature, even in the absence of statistically significant differences in certain areas, underscore the need for further investigation and improved patient management strategies to mitigate potential long-term risks associated with reproductive treatments.
Conclusions
This research underscores the importance of assessing the long-term health effects of reproductive treatments on mothers. While immediate outcomes often receive the most attention, our findings reveal that women who undergo these therapies experience significant rates of cancer, metabolic disorders, and cardiovascular disease. Although a majority of patients maintain excellent health - 64.44% reporting no chronic diseases - our data highlight that a notable minority face long-term health challenges. This emphasizes the necessity for ongoing surveillance and long-term health monitoring for individuals receiving reproductive treatments. Future research should focus on extending follow-up periods and investigating the relationship between specific reproductive treatments and long-term health outcomes to enhance patient care and management strategies.
Disclosures
Human subjects: Consent for treatment and open access publication was obtained or waived by all participants in this study. Rehman Medical Institute Research Ethics Committee issued approval RMI/RMI-REC/Article Approval/76, September 07, 2022.
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: Nabila Shams, Faiza Rahman
Acquisition, analysis, or interpretation of data: Nabila Shams, Faiza Rahman, Laraib Fatima, Laiba Asad, Kashmal Khattak, Ayesha Khan, Hina Khan
Drafting of the manuscript: Nabila Shams, Faiza Rahman, Laraib Fatima, Laiba Asad, Kashmal Khattak, Ayesha Khan, Hina Khan
Critical review of the manuscript for important intellectual content: Nabila Shams, Faiza Rahman, Laraib Fatima, Laiba Asad, Kashmal Khattak, Ayesha Khan, Hina Khan
Supervision: Nabila Shams, Faiza Rahman
References
- 1.Fertility knowledge and beliefs about fertility treatment: findings from the International Fertility Decision-making Study. Bunting L, Tsibulsky I, Boivin J. Hum Reprod. 2013;28:385–397. doi: 10.1093/humrep/des402. [DOI] [PubMed] [Google Scholar]
- 2.Assisted reproductive technology - IVF treatment in Ireland: a study of couples with successful outcomes. Mahon E, Cotter N. Hum Fertil (Camb) 2014;17:165–169. doi: 10.3109/14647273.2014.948498. [DOI] [PubMed] [Google Scholar]
- 3.Expected advances in human fertility treatments and their likely translational consequences. Gleicher N. J Transl Med. 2018;16:149. doi: 10.1186/s12967-018-1525-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maternal and fetal risk associated with assisted reproductive technology. Kawwass JF, Badell ML. Obstet Gynecol. 2018;132:763–772. doi: 10.1097/AOG.0000000000002786. [DOI] [PubMed] [Google Scholar]
- 5.Fertility practitioners’ experience of the psychological sequelae of unmet parental goals after unsuccessful fertility treatment: a Delphi Consensus Study. Moore SE. https://www.semanticscholar.org/paper/Fertility-practitioners'-experience-of-the-sequelae-Moore/c9249afd49a08008aca9749cee3f0396f4584353 2018 [Google Scholar]
- 6.Fertility preservation in women: indications and options for therapy. Hussein RS, Khan Z, Zhao Y. Mayo Clin Proc. 2020;95:770–783. doi: 10.1016/j.mayocp.2019.10.009. [DOI] [PubMed] [Google Scholar]
- 7.Impact of contraception and IVF hormones on metabolic, endocrine, and inflammatory status. Coussa A, Hasan HA, Barber TM. J Assist Reprod Genet. 2020;37:1267–1272. doi: 10.1007/s10815-020-01756-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.The longer-term health outcomes for children born as a result of IVF treatment: part I-general health outcomes. Hart R, Norman RJ. Hum Reprod Update. 2013;19:232–243. doi: 10.1093/humupd/dms062. [DOI] [PubMed] [Google Scholar]
- 9.Obstetric and perinatal outcomes in subfertile patients who conceived following low technology interventions for fertility enhancement: a comprehensive review. Palomba S, Santagni S, Daolio J, Gibbins K, Battaglia FA, La Sala GB, Silver RM. Arch Gynecol Obstet. 2018;297:33–47. doi: 10.1007/s00404-017-4572-9. [DOI] [PubMed] [Google Scholar]
- 10.The health outcomes of human offspring conceived by assisted reproductive technologies (ART) Chen M, Heilbronn LK. J Dev Orig Health Dis. 2017;8:388–402. doi: 10.1017/S2040174417000228. [DOI] [PubMed] [Google Scholar]
- 11.Increased incidence of gestational hypertension and preeclampsia after assisted reproductive technology treatment. Wang YA, Chughtai AA, Farquhar CM, Pollock W, Lui K, Sullivan EA. Fertil Steril. 2016;105:920–926. doi: 10.1016/j.fertnstert.2015.12.024. [DOI] [PubMed] [Google Scholar]
- 12.Assisted reproductive technology and the risk of pregnancy-related complications and adverse pregnancy outcomes in singleton pregnancies: a meta-analysis of cohort studies. Qin J, Liu X, Sheng X, Wang H, Gao S. Fertil Steril. 2016;105:73–6. doi: 10.1016/j.fertnstert.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 13.Cardiovascular and metabolic profiles of offspring conceived by assisted reproductive technologies: a systematic review and meta-analysis. Guo XY, Liu XM, Jin L, Wang TT, Ullah K, Sheng JZ, Huang HF. Fertil Steril. 2017;107:622–631. doi: 10.1016/j.fertnstert.2016.12.007. [DOI] [PubMed] [Google Scholar]
- 14.Infertility etiologies are genetically and clinically linked with other diseases in single meta-diseases. Tarín JJ, García-Pérez MA, Hamatani T, Cano A. Reprod Biol Endocrinol. 2015;13:31. doi: 10.1186/s12958-015-0029-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Long-term cardiovascular risk in women prescribed fertility therapy. Udell JA, Lu H, Redelmeier DA. https://www.jacc.org/doi/epdf/10.1016/j.jacc.2013.05.085. J Am Coll Cardiol. 2013;62:1704–1712. doi: 10.1016/j.jacc.2013.05.085. [DOI] [PubMed] [Google Scholar]
- 16.Pregnancy and cardiovascular risk: a review focused on women with heart disease undergoing fertility treatment. Rossberg N, Stangl K, Stangl V. Eur J Prev Cardiol. 2016;23:1953–1961. doi: 10.1177/2047487316673143. [DOI] [PubMed] [Google Scholar]
- 17.Factors associated with ovarian hyperstimulation syndrome (OHSS) severity in women with polycystic ovary syndrome undergoing IVF/ICSI. Sun B, Ma Y, Li L, et al. Front Endocrinol (Lausanne) 2020;11:615957. doi: 10.3389/fendo.2020.615957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fertility and reproductive care in chronic kidney disease. Dumanski SM, Ahmed SB. J Nephrol. 2019;32:39–50. doi: 10.1007/s40620-018-00569-9. [DOI] [PubMed] [Google Scholar]
- 19.Maternal, perinatal and long-term outcomes after assisted reproductive techniques (ART): implications for clinical practice. Talaulikar VS, Arulkumaran S. Eur J Obstet Gynecol Reprod Biol. 2013;170:13–19. doi: 10.1016/j.ejogrb.2013.04.014. [DOI] [PubMed] [Google Scholar]