Abstract
Purpose
Health-related quality of life (HRQoL) impacts of insomnia and depression (as separated entities) have been well investigated in previous studies. However, little is known about the effect of comorbid insomnia and depression on HRQoL. This study aimed to assess the impacts of insomnia and depression, in combination or alone, on HRQoL in Australian adults.
Methods
Data used in this study were obtained from the large-scale longitudinal Household, Income and Labour Dynamics in Australia (HILDA) survey. Insomnia was defined using key insomnia criteria of DSM-V. Depression was based on validated cut-off points of the Mental Health Inventory-5 (MHI-5) (scores ≤ 62) in the base case analysis. HRQoL expressed as utility scores (ranging from 0 to 1) were measured using the Short-Form 6-Dimension (SF-6D) converted from the SF-36 and valued using an Australian scoring algorithm. Multi-level modelling was applied to assess the effect of insomnia and/or depression on utility scores.
Results
The study analysed 30,972 observations from 10,324 individuals (age [mean ± SD]: 45.7 ± 16.5, female: 54.6%). The proportion of individuals with insomnia only, depression only, and comorbid insomnia and depression was 11.3%, 11.6%, and 8.2%, respectively. The interaction effect suggested the combined impact of insomnia and depression on health-related quality of life beyond the sum of their individual effects. Marginal mean difference in utility scores for insomnia only, depression only, and the comorbidity relative to no insomnia or depression was -0.058 (SE: 0.003, Cohen’s d: 0.420, small effect), -0.210 (SE: 0.003, Cohen’s d: 1.530, large effect), and -0.291 (SE: 0.004, Cohen’s d: 2.120, large effect), respectively.
Conclusion
Comorbid depression and insomnia appear to have very large quality-of-life impacts. Furthermore, this is the first study that has estimated the magnitude of the impact of comorbid insomnia and depression on utility scores which can be utilised in future clinical or economic studies.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11136-024-03793-y.
Keywords: Comorbidity, Depression, Health-related quality of life, Insomnia, Utility score
Plain language summary
Insomnia and depression often occur together and have an evidence-based bidirectional relationship. The impairment of health-related quality of life (HRQoL) associated with insomnia or depression, as an individual effect, has been previously examined by several studies. However, the reduction in HRQoL associated with comorbid insomnia and depression has been understudied. With the use of representative longitudinal data containing a large sample size of 10,324 Australian adults, we found that insomnia and depression were associated with statistically significant reductions in health-related quality of life, whether occurring individually or concurrently. The effect of comorbid insomnia and depression on quality of life was significantly larger than the summative effect of insomnia and depression. This study provides new insights into the quality-of-life burden of insomnia and/or depression and emphasises the importance of addressing insomnia in adults with depression.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11136-024-03793-y.
Introduction
Depression is one of the 25 leading causes contributing to the global health-related burden with a dramatic upward trend of prevalence and incidence rates in the last ten years [1]. Insomnia and depression often occur concurrently [2], with 41% of those with depression experiencing insomnia [3]. Moreover, depression and insomnia have a bidirectional relationship that has been investigated by several studies, especially in adult populations [4–6]. Insomnia has been found to be a risk factor that impairs depression treatments and predicts subsequent depression [4, 7–11]. Additionally, increasing evidence has shown that insomnia treatment may alleviate depressive symptoms in individuals with comorbid insomnia and depression [12–14]. Conversely, depression is also considered a risk factor for future insomnia [15].
Health-related quality of life (HRQoL) is a multidimensional concept that is widely used to capture the health status of individuals. The two main dimensions of HRQoL are usually physical and mental health [16]. Measuring HRQoL can provide new insights into the burden of preventable diseases, injuries, and disabilities [16]. HRQoL can be measured by different questionnaires such as the World Health Organization Quality-of-Life (WHO-Qol) [17] or the Short Form (SF)-36 [18]. HRQoL is usually expressed as utility scores commonly derived from HRQoL questionnaires that have preference-based scoring algorithms (commonly referred to as multi-attribute utility instruments - MAUIs). The scoring algorithms convert scores on the questionnaires to a scale of 0 to 1. A score of 1 denotes perfect health as measured by the questionnaire and 0 denotes death [19]. There can be health states measured on the questionnaires that have values that are less than 0 – these health states have been judged to be worse than death [20]. Commonly used MAUIs include the EQ-5D [21], the SF-6D – derived from the SF-12 or SF-36 [22], Health Utilities Index (HUI) [23], and the suite of Assessment of Quality of Life (AQoL) [24] questionnaires. Utility scores are also used to determine quality-adjusted life years (QALYs), a generic health outcome measure recommended in several guidelines for economic evaluations [25–27].
Impairment of HRQoL associated with insomnia or depression has been examined by previous studies. The mean utility scores for those with major depressive disorder (MDD) have been found to be significantly lower than the scores for those without mental disorders/symptoms (0.65 ± 0.28 versus 0.88 ± 0.17, effect size: -1.32, p-value < 0.001) (assessed with AQoL-4D) [28]. Individuals with chronic insomnia have been similarly found to have significantly lower utility scores compared to those without insomnia (0.63 versus 0.72 in the US, p-value < 0.001, 0.57 versus 0.67 in France, p-value < 0.001, and 0.67 versus 0.77 in Japan, p-values < 0.001) (all measured by SF-6D) [29]. However, these scores are not directly compared given that utilities derived from different MAUIs will result in different scores [30]. Furthermore, little is known about the interaction effect of both insomnia and depression on utility scores. This study aimed to assess the impact of insomnia and depression, in combination or alone, on HRQoL measured as utility scores in a representative sample of Australian adults.
Methods
Study sample
The Household, Income, and Labour Dynamics in Australia (HILDA) survey is an ongoing longitudinal study that commenced in 2001. HILDA gathers comprehensive data on various aspects of family life, income, employment, and the health of over 17,000 Australians aged 15 years or above annually. The survey consists of two parts: an interview and a self-completed questionnaire (SCQ). Sleep, depression and HRQoL were collected in the SCQ part. SCQ response rates among those who completed the interview of these waves were approximately 90% [31]. A full description of sample selection and data collection was published elsewhere [31].
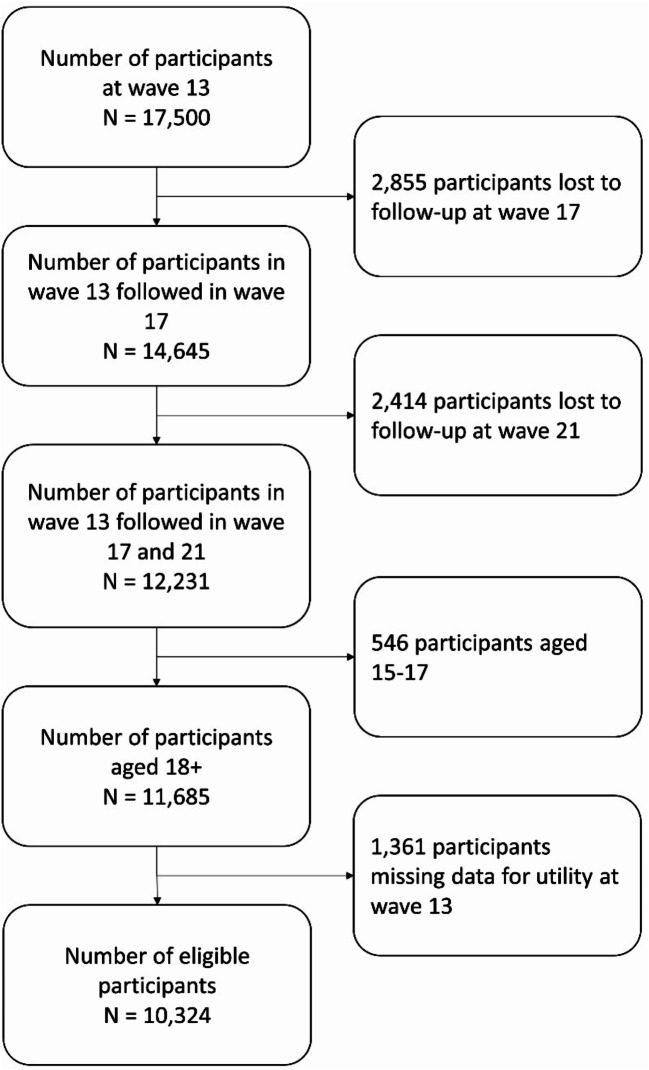
Data from waves 13 (baseline), 17 (follow-up T1), and 21 (follow-up T2) (collected in 2013, 2017, and 2021, respectively) were used for this study since sleep items were only available in these waves [31, 32]. A total of 11,685 individuals aged 18 years or above participated in all these three waves. After excluding 1,361 participants (11.6%) due to missing data on utility scores at baseline (wave 13), the remaining 10,324 participants (30,972 observations) comprised the analytical sample (Fig. 1).
Fig. 1.
Study subject flowchart
Measures
Exposures
Depression was defined using a Mental Health Inventory-5 (MHI-5) [33] cut-off point of 62 or less (sensitivity: 0.74, specificity: 0.91 to define major depression and dysthymia according to DSM-III-R criteria) [34]. The MHI-5 is a brief and valid tool that contains five six-point-scale questions focusing on measuring depression and anxiety symptoms and psychological well-being (higher scores indicate better mental health) [35].
Key features of insomnia disorder according to the DSM-V are “dissatisfaction with sleep quantity or quality with complaints of difficulty initiating or maintaining sleep” [36]. In the HILDA survey, participants were asked to self-report how often during the past month they had trouble sleeping because of (i) difficulty getting to sleep within 30 min; (ii) wake-up in the middle of the night or early in the morning on a five-level scale. Sleep quality was also self-reported by the participants on a four-level scale. In this study, insomnia was defined as subjective complaints with sleep initiation or maintenance at least 3 times per week combined with fairly or very bad self-rated sleep quality.
Outcomes
Utility scores were estimated using the SF-6D, a widely used MAUI and can be derived from the SF-36 which was measured in all waves of the HILDA [22]. The validity of HILDA data for the SF-36 has been tested and published elsewhere [37]. Australian algorithm developed by Norman et al. [38] was used to value health states in this study.
Covariates
Potential covariates are factors previously examined that are thought to be associated with the exposure and/or outcome variables in other studies [10, 11, 29, 39–51]. These covariates for the current study comprised demographics and socio-economic status (i.e., age, sex, education, marital status, English as not first language learnt to speak as a child, employment status, regular income, and major life events), self-reported physical conditions (i.e., serious physical illnesses, obesity, and pain), behaviours and lifestyle (i.e., diet quality, physical activity, smoking, and alcohol use), and Covid-19 impact.
Definitions and values of all measures are described in Table S1 in the supplementary materials.
Statistical analyses
We employed descriptive statistics to summarise characteristics of the analytical sample and subgroups classified based on the presence of insomnia and/or depression. Univariate tests, including t-tests of means, analysis of variance (ANOVA), and chi-square test, were used to assess the association between potential confounders and the exposures/outcomes and between insomnia and depression using data from wave 13. The association between insomnia and depression was also tested using a chi-squared test.
Data on both insomnia and depression were exclusively gathered in three waves of the HILDA survey, with a substantial four-year gap between two waves, during which no information regarding the remission and relapse of depression and insomnia was collected. Given that previous studies have highlighted the dynamic nature of depression and insomnia [52–54], a repeated measures design was employed instead of using growth models. The associations between insomnia and/or depression and utility scores were tested using linear multi-level modelling with observations nested within individuals. The null model which included random-effects only was first derived. Insomnia, depression, and the interaction between them were added to the fixed-effects model. The covariates were subsequently incorporated into the model in the following order: age and sex (Model 2), physical conditions (Model 3), the remaining variables of demographics and socio-economic status (Model 4), behaviours and lifestyle (Model 5), and Covid-19 impact (Model 6).
The final model (Model 6) was used to derive marginal mean utility scores for four groups: insomnia only, depression only, comorbid insomnia and depression, and no insomnia and depression. Tukey’s honest significant difference (HSD) was used for post-hoc pairwise comparisons to examine differences in marginal means between those with insomnia only, depression only, and comorbid insomnia and depression compared to no insomnia and depression. We also compared comorbid insomnia and depression to depression only. The pairwise differences were also expressed as standardised effect sizes using Cohen’s d (SES) with their standard errors (SE). SES was classified into small (d = 0.2), medium (d = 0.4), and large (d = 0.8) effects [55].
Residual diagnostic plots (Q-Q plots and scatter plots of residuals versus fitted values) were used to test the assumptions of normal distribution and homogeneity of variance for univariate analyses and multi-level modelling [56–58].
Statistical significance was considered when a 2-sided p-value was less than 0.05. However, for selecting confounders to be incorporated in the modelling using univariate tests, a cut-off of p-value < 0.25 was used. This is a conservative cut-off point used to minimise the risk of excluding variables that were not found to be statistically significant but might impact the modelling results [59, 60]. All analyses were performed using R version 4.3.0. The tidyverse package was used for descriptive statistics. For conducting multilevel modelling and calculating marginal means and effect sizes for insomnia and/or depression on utility scores, we utilised the lme4, emmeans, and ggplot2 packages.
The mean utility scores were calculated both with and without the use of weights in the current study. If the difference between the marginal means of utility scores, with and without the utilisation of weights, was negligible, we did not apply weights for the rest of the analyses.
The missing rates for most variables were less than 7% (Refer to Table S3 in the supplementary materials); therefore, no imputations were performed. To handle missing values, pairwise deletion was applied for descriptive statistics and univariate analyses, and full information maximum likelihood (FIML) was used instead of restricted maximum likelihood (REML) for multilevel modelling.
Sensitivity and subgroup analyses
Two other cut-off points of MHI-5 scores with different sensitivity and specificity levels were used to define depression: MHI-5 scores ≤ 54 (sensitivity: 0.63, specificity: 0.96) (Sensitivity analysis 1: SA1); and MHI-5 scores ≤ 74 (sensitivity: 0.90, specificity: 0.80) (Sensitivity analysis 2: SA2) [34].
Moreover, we used the Kessler Psychological Distress Scale (K10) to characterise depression in the subsequent analysis (Sensitivity analysis 3: SA3). The K10 is a well-validated global tool to measure psychological distress over the past four weeks in adult populations [61]. The total score was calculated as the sum of each item score, yielding a score range from 10 to 50 [62]. The choice of the cut-off point of ≥ 20 was based on validation studies and its widespread application in general practice and previous studies [62–65]. Sensitivity and specificity of K10 scores ≥ 20 to define anxiety or affective disorders were 0.66 and 0.92, respectively [63].
In line with previous studies showing a greater reduction in HRQoL associated with more severe depression, this study also investigated the effect of insomnia in people with varying depression severity levels. Given that there were no validated MHI-5 cut-off points to define depression severity, we used K10 to classify the severity of depression into three severity categories, including mild (K10 scores of 20–24), moderate (K10 scores of 25–29), and severe (K10 scores of 30–50) [63, 64] in subgroup analyses.
Results
Base case analysis
At baseline, the one-month prevalence of insomnia or depression was nearly 20%; and 41.3% of individuals with depression had insomnia. Table 1 summarises characteristics for the whole study sample and subgroups stratified by insomnia and depression: no insomnia or depression, insomnia only, depression only, and comorbid insomnia and depression. At baseline (wave 13), approximately 11% of individuals had insomnia only, and a similar proportion had depression only, while 8.2% had both insomnia and depression. The proportions for depression only and comorbid insomnia and depression at T2 were slightly higher, at 15% and 11%, respectively. The mean age of the sample at the baseline was 45.7 ± 16.5, with females accounting for 54.6%.
Table 1.
Characteristics of the study subjects by subgroups of depression and insomnia in the base case analysis
| Variables | Wave 13, N (%) | Wave 17, N (%) | Wave 21, N (%) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ALL | NONE | INS | DEP | BOTH | ALL | NONE | INS | DEP | BOTH | ALL | NONE | INS | DEP | BOTH | ||
| N (%) |
10,324 (100.0) |
6,998 (68.8) |
1,151 (11.3) |
1,184 (11.6) |
833 (8.2) |
10,324 (100.0) |
6,537 (66.7) |
1,170 (11.9) |
1,206 (12.3) |
887 (9.1) |
10,324 (100.0) |
5,987 (61.9) |
1,156 (12.0) |
1,475 (15.3) |
1,054 (10.9) |
|
|
Utility scores Mean (SD) |
0.662 (0.236) |
0.740 (0.174) |
0.642 (0.210) |
0.458 (0.228) |
0.338 (0.256) |
0.641 (0.246) |
0.729 (0.182) |
0.612 (0.216) |
0.445 (0.235) |
0.309 (0.256) |
0.612 (0.253) |
0.711 (0.186) |
0.613 (0.212) |
0.441 (0.237) |
0.299 (0.248) |
|
|
Age Mean (SD) |
45.7 (16.5) |
46.1 (16.8) |
47.1 (15.8) |
42.7 (16.0) |
44.8 (15.2) |
49.7 (16.5) |
50.5 (16.6) |
51.4 (15.7) |
46.5 (16.4) |
47.1 (14.9) |
53.7 (16.5) |
55.1 (16.4) |
54.8 (15.6) |
50.1 (16.4) |
50.9 (15.3) |
|
| Sex | Male |
4,691 (45.4) |
3,354 (47.9) |
451 (39.2) |
512 (43.2) |
306 (36.7) |
4,691 (45.4) |
3,113 (47.6) |
463 (39.6) |
538 (44.6) |
335 (37.8) |
4,691 (45.4) |
2,870 (47.9) |
472 (40.8) |
636 (43.1) |
391 (37.1) |
| Female |
5,633 (54.6) |
36,44 (52.1) |
700 (60.8) |
672 (56.8) |
527 (63.3) |
5,633 (54.6) |
3,424 (52.4) |
707 (60.4) |
668 (55.4) |
552 (62.2) |
5,633 (54.6) |
3,117 (52.1) |
684 (59.2) |
839 (56.9) |
663 (62.9) |
|
| Education level | High |
2,947 (28.6) |
2,168 (31.0) |
291 (25.3) |
294 (24.8) |
170 (20.4) |
3,280 (31.8) |
2,250 (34.4) |
337 (28.8) |
376 (31.2) |
189 (21.3) |
3,416 (33.1) |
2,130 (35.6) |
354 (30.6) |
478 (32.4) |
281 (26.7) |
| Middle |
5,027 (48.7) |
3,394 (48.5) |
566 (49.2) |
605 (51.1) |
397 (47.7) |
4,877 (47.3) |
3,013 (46.1) |
573 (49.0) |
568 (47.1) |
454 (51.2) |
4,810 (46.6) |
2,738 (45.8) |
561 (48.5) |
694 (47.1) |
510 (48.4) |
|
| Low |
2,345 (22.7) |
1,432 (20.5) |
293 (25.5) |
285 (24.1) |
266 (31.9) |
2,162 (21.0) |
1,270 (19.4) |
259 (22.2) |
262 (21.7) |
244 (27.5) |
2,093 (20.3) |
1,114 (18.6) |
241 (20.8) |
303 (20.5) |
263 (25.0) |
|
| Marital status | Partnered |
7,210 (69.8) |
5,095 (72.8) |
813 (70.6) |
705 (59.5) |
494 (59.3) |
7,340 (71.1) |
4,835 (74.0) |
869 (74.3) |
752 (62.4) |
552 (62.2) |
7,294 (70.7) |
4,465 (74.6) |
853 (73.9) |
969 (65.7) |
630 (59.8) |
| Non-partnered |
3,114 (30.2) |
1,903 (27.2) |
338 (29.4) |
479 (40.5) |
339 (40.7) |
2,983 (28.9) |
1,701 (26.0) |
301 (25.7) |
454 (37.6) |
335 (37.8) |
3,027 (29.3) |
1,521 (25.4) |
302 (26.1) |
506 (34.3) |
423 (40.2) |
|
| English as 2nd language | Yes |
9,279 (89.9) |
6,280 (89.8) |
1,066 (92.6) |
1,037 (87.6) |
758 (91.0) |
9,279 (89.9) |
5,869 (89.8) |
1,086 (92.8) |
1051 (87.2) |
823 (92.8) |
9,279 (89.9) |
5,357 (89.5) |
5,357 (89.5) |
1,307 (88.6) |
970 (92.0) |
| No |
1,044 (10.1) |
717 (10.2) |
85 (7.4) |
147 (12.4) |
75 (9.0) |
1,044 (10.1) |
668 (10.2) |
84 (7.2) |
154 (12.8) |
64 (7.2) |
1,044 (10.1) |
630 (10.5) |
630 (10.5) |
168 (11.4) |
84 (8.0) |
|
| Employment status | Employed |
6,974 (67.6) |
4956 (70.8) |
755 (65.6) |
736 (62.2) |
444 (53.3) |
6,769 (65.6) |
4,477 (68.5) |
733 (62.6) |
770 (63.8) |
471 (53.1) |
6,319 (61.2) |
3,766 (62.9) |
684 (59.2) |
888 (60.2) |
592 (56.2) |
|
Unemployed/ Not in the labour force |
3,350 (32.4) |
2042 (29.2) |
396 (34.4) |
448 (37.8) |
389 (46.7) |
3,555 (34.4) |
2,060 (31.5) |
437 (37.4) |
436 (36.2) |
416 (46.9) |
4,005 (38.8) |
2,221 (37.1) |
472 (40.8) |
587 (39.8) |
462 (43.8) |
|
|
Household income Mean (SD) (per A$10,000) |
11.6 (10.2) |
12.2 (10.5) |
11.4 (10.6) |
10.3 (9.3) |
9.5 (8.1) |
12.4 (12.6) |
13.2 (13.6) |
12.0 (11.7) |
11.1 (10.6) |
10.2 (9.9) |
13.5 (12.6) |
14.2 (13.6) |
13.0 (10.5) |
12.4 (9.2) |
11.9 (11.1) |
|
| Social support | Medium-High |
6,721 (66.2) |
5,270 (76.3) |
751 (66.5) |
396 (34.1) |
219 (26.7) |
6,448 (65.9) |
4,959 (77.4) |
775 (67.2) |
393 (33.5) |
225 (26.0) |
6,048 (62.3) |
4,412 (74.4) |
725 (63.4) |
534 (36.8) |
318 (30.4) |
| Low |
3,436 (33.8) |
1,633 (23.7) |
378 (33.5) |
764 (65.9) |
602 (73.3) |
3,341 (34.1) |
1,451 (22.6) |
378 (32.8) |
780 (66.5) |
640 (74.0) |
3,660 (37.7) |
1,517 (25.6) |
418 (36.6) |
919 (63.2) |
728 (69.6) |
|
| Major life events | No |
3,958 (39.4) |
2,848 (41.6) |
404 (36.0) |
416 (36.3) |
239 (29.8) |
4,141 (42.4) |
2,898 (45.2) |
445 (39.0) |
417 (35.6) |
285 (33.1) |
4,341 (44.8) |
2,823 (47.6) |
503 (44.0) |
594 (41.0) |
352 (34.2) |
| Yes |
6,100 (60.6) |
3,995 (58.4) |
718 (64.0) |
730 (63.7) |
564 (70.2) |
5,637 (57.6) |
3,510 (54.8) |
696 (61.0) |
755 (64.4) |
576 (66.9) |
5,359 (55.2) |
3,112 (52.4) |
639 (56.0) |
856 (59.0) |
676 (65.8) |
|
| Sleep medication | No |
9,400 (91.6) |
6,681 (95.8) |
954 (83.0) |
1,045 (88.7) |
606 (73.1) |
9,045 (91.0) |
6,208 (95.3) |
980 (84.3) |
1,049 (87.6) |
652 (74.0) |
8,663 (88.8) |
5,623 (94.2) |
929 (80.4) |
1,242 (85.1) |
768 (73.0) |
| Yes |
867 (8.4) |
294 (4.2) |
196 (17.0) |
133 (11.3) |
223 (26.9) |
897 (9.0) |
303 (4.7) |
183 (15.7) |
149 (12.4) |
229 (26.0) |
1,094 (11.2) |
344 (5.8) |
227 (19.6) |
218 (14.9) |
284 (27.0) |
|
| Depression medication | No |
9,811 (95.0) |
6,840 (97.7) |
1,106 (96.1) |
1,052 (88.9) |
667 (80.1) |
9,525 (92.3) |
6,320 (96.7) |
1,106 (94.5) |
994 (82.4) |
644 (72.6) |
9,317 (90.2) |
5,731 (95.7) |
1,080 (93.4) |
1,181 (80.1) |
756 (71.7) |
| Yes |
513 (5.0) |
158 (2.3) |
45 (3.9) |
132 (11.1) |
166 (19.9) |
799 (7.7) |
217 (3.3) |
64 (5.5) |
212 (17.6) |
243 (27.4) |
1,007 (9.8) |
256 (4.3) |
76 (6.6) |
294 (19.9) |
298 (28.3) |
|
| Chronic pain | No |
9,527 (92.3) |
6,663 (95.2) |
1,018 (88.4) |
1,062 (89.7) |
646 (77.6) |
9,326 (90.3) |
6,155 (94.2) |
996 (85.1) |
1,052 (87.2) |
663 (74.7) |
9,197 (89.1) |
5,575 (93.1) |
997 (86.2) |
1,270 (86.1) |
790 (75.0) |
| Yes |
797 (7.7) |
335 (4.8) |
133 (11.6) |
122 (10.3) |
187 (22.4) |
998 (9.7) |
382 (5.8) |
174 (14.9) |
154 (12.8) |
224 (25.3) |
1,127 (10.9) |
412 (6.9) |
159 (13.8) |
205 (13.9) |
264 (25.0) |
|
| Serious physical illnesses | No |
6,253 (60.6) |
4,449 (63.6) |
609 (52.9) |
700 (59.1) |
406 (48.7) |
5,845 (56.6) |
3,891 (59.5) |
556 (47.5) |
685 (56.8) |
407 (45.9) |
5,275 (51.1) |
3,192 (53.3) |
511 (44.2) |
788 (53.4) |
427 (40.5) |
| Yes |
4,071 (39.4) |
2,549 (36.4) |
542 (47.1) |
484 (40.9) |
427 (51.3) |
4,479 (43.4) |
2,646 (40.5) |
614 (52.5) |
521 (43.2) |
480 (54.1) |
5,049 (48.9) |
2,795 (46.7) |
645 (55.8) |
687 (46.6) |
627 (59.5) |
|
| Obesity | No |
7,540 (75.3) |
5,297 (77.9) |
795 (70.5) |
838 (73.6) |
507 (63.5) |
7,027 (72.3) |
4,765 (74.9) |
786 (68.7) |
820 (70.8) |
500 (59.4) |
6,688 (69.0) |
4,293 (72.7) |
746 (65.2) |
964 (66.6) |
580 (56.0) |
| Yes |
2,474 (24.7) |
1,507 (22.1) |
332 (29.5) |
300 (26.4) |
291 (36.5) |
2,698 (27.7) |
1,600 (25.1) |
358 (31.3) |
339 (29.2) |
342 (40.6) |
3,010 (31.0) |
1,610 (27.3) |
398 (34.8) |
483 (33.4) |
456 (44.0) |
|
| Diet quality | Good |
3,267 (34.1) |
2,408 (37.0) |
351 (32.3) |
273 (24.9) |
199 (25.9) |
2,958 (32) |
2,066 (34.5) |
360 (32.6) |
276 (24.7) |
197 (23.6) |
2,501 (27.7) |
1,681 (30.7) |
289 (27.0) |
308 (22.9) |
184 (18.6) |
| Poor |
6,319 (65.9) |
4,101 (63.0) |
737 (67.7) |
823 (75.1) |
568 (74.1) |
6,285 (68) |
3,928 (65.5) |
743 (67.4) |
841 (75.3) |
639 (76.4) |
6,523 (72.3) |
3,803 (69.3) |
783 (73.0) |
1,035 (77.1) |
804 (81.4) |
|
| Physical activity | High frequency |
3,617 (35.1) |
2,709 (38.8) |
349 (30.4) |
319 (27.0) |
181 (21.8) |
3,231 (32.5) |
2,374 (36.4) |
342 (29.3) |
307 (25.5) |
160 (18.1) |
3,345 (34) |
2,344 (39.2) |
355 (30.7) |
389 (26.4) |
208 (19.7) |
| Low frequency |
6,688 (64.9) |
4,280 (61.2) |
798 (69.6) |
861 (73.0) |
650 (78.2) |
6,722 (67.5) |
4,156 (63.6) |
825 (70.7) |
897 (74.5) |
726 (81.9) |
6,506 (66) |
3,638 (60.8) |
800 (69.3) |
1,086 (73.6) |
846 (80.3) |
|
| Alcohol use | Low risk |
8,736 (85.1) |
5,896 (84.8) |
954 (83.1) |
,1032 (87.6) |
721 (87.1) |
8,381 (84.6) |
5,435 (83.7) |
974 (83.7) |
1,057 (88.2) |
771 (87.3) |
8,201 (83.4) |
4,918 (82.3) |
955 (82.8) |
1,266 (86.1) |
904 (85.8) |
| High risk |
1,526 (14.9) |
1,056 (15.2) |
194 (16.9) |
146 (12.4) |
107 (12.9) |
1,527 (15.4) |
1,062 (16.3) |
190 (16.3) |
141 (11.8) |
112 (12.7) |
1,636 (16.6) |
1,059 (17.7) |
198 (17.2) |
205 (13.9) |
149 (14.2) |
|
| Smoking | Never/Former smoker |
8,567 (83.3) |
6,027 (86.4) |
923 (80.5) |
923 (78.3) |
582 (70.1) |
8,470 (85.3) |
5,753 (88.4) |
965 (82.8) |
964 (80.3) |
657 (74.3) |
85,55 (87.1) |
53,30 (89.3) |
1,002 (86.9) |
1,236 (83.9) |
837 (79.7) |
| Smoker |
1,717 (16.7) |
945 (13.6) |
224 (19.5) |
256 (21.7) |
248 (29.9) |
1,454 (14.7) |
757 (11.6) |
201 (17.2) |
237 (19.7) |
227 (25.7) |
12,71 (12.9) |
637 (10.7) |
151 (13.1) |
238 (16.1) |
213 (20.3) |
|
| Life changed by Covid | Not impacted |
955 (27.6) |
621 (8.9) |
102 (8.9) |
121 (10.2) |
86 (10.3) |
||||||||||
| Impacted with a great extent |
2,505 (72.4) |
1,614 (23.1) |
301 (26.2) |
307 (26.0) |
246 (29.5) |
|||||||||||
| Impacted with a moderate extent |
3,651 (51.3) |
2,527 (36.1) |
394 (34.3) |
414 (35.0) |
260 (31.2) |
|||||||||||
| Impacted with a great extent |
3,207 (34.3) |
2,234 (31.9) |
353 (30.7) |
340 (28.8) |
241 (28.9) |
|||||||||||
NONE: No insomnia and depression, INS: Insomnia, DEP: Depression, BOTH: Comorbid insomnia and depression
Missing rates for all variables were presented Table S3 in the supplementary material
The mean utility scores, whether weighted or unweighted, were nearly equal, as presented in Table S2 in the supplementary materials. The weighted and unweighted mean utility scores of the study sample were 0.636 ± 0.247 and 0.639 ± 0.246, respectively.
Table 2 presents the results of multilevel modelling for the base case analysis. The intraclass correlation coefficient (ICC) for the null model was 0.599. As shown in Table 2, insomnia, depression, and the interaction term between insomnia and depression presented significant associations with the decrement of utility scores in both unadjusted (Model 1) and adjusted models (Model 2–6). In model 6, which included all covariates, the main effect showed that insomnia or depression independently decreased utility scores by 0.058 (95% CI: 0.064 to 0.051) and 0.210 (95% CI: 0.216 to 0.203), respectively. The interaction term between insomnia and depression suggested that the combined effect of insomnia and depression on utility scores was synergistic, meaning comorbid insomnia and depression led to an additional decrease of 0.023 (95% CI: -0.034 to -0.013) in utility score beyond the sum of their individual effects alone.
Table 2.
Association of Insomnia and depression with utility scores (β, 95% CI)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |
|---|---|---|---|---|---|---|
| Fixed effects | ||||||
| Intercept | 0.709 (0.706–0.713)*** | 0.835 (0.828–0.843)*** | 0.837 (0.830–0.844)*** | 0.865 (0.856–0.874)*** | 0.903 (0.893–0.913)*** | 0.902 (0.888–0.916)*** |
| Insomnia | -0.078 (-0.084 – -0.071)*** | -0.077 (-0.083 – -0.070)*** | -0.066 (-0.073 – -0.060)*** | -0.061 (-0.067 – -0.055)*** | -0.058 (-0.064 – -0.051)*** | -0.058 (-0.064 – -0.051)*** |
| Depression | -0.231 (-0.237 – -0.225)*** | -0.238 (-0.244 – -0.231)*** | -0.233 (-0.239 – -0.227)*** | -0.213 (-0.219 – -0.207)*** | -0.21 (-0.217 – -0.204)*** | -0.210 (-0.216 – -0.203)*** |
| Insomnia*depression | -0.029 (-0.040 – -0.018)*** | -0.029 (-0.040 – -0.019)*** | -0.022 (-0.033 – -0.012)*** | -0.023 (-0.033 – -0.013)*** | -0.024 (-0.034 – -0.013)*** | -0.023 (-0.034 – -0.013)*** |
| Age (centring at 18) | -0.003 (-0.004 – -0.003)*** | -0.002 (-0.002 – -0.002)*** | -0.002 (-0.002 – -0.001)*** | -0.002 (-0.002 – -0.002)*** | -0.002 (-0.002 – -0.002)*** | |
| Sex (Female) | -0.031 (-0.037 – -0.025)*** | -0.024 (-0.029 – -0.019)*** | -0.024 (-0.029 – -0.018)*** | -0.022 (-0.027 – -0.016)*** | -0.021 (-0.027 – -0.016)*** | |
| Serious physical illnesses | -0.051 (-0.056 – -0.046)*** | -0.045 (-0.050 – -0.040)*** | -0.045 (-0.050 – -0.040)*** | -0.045 (-0.050 – -0.040)*** | ||
| Obesity | -0.041 (-0.046 – -0.035)*** | -0.037 (-0.042 – -0.032)*** | -0.032 (-0.037 – -0.027)*** | -0.032 (-0.037 – -0.027)*** | ||
| Chronic pain | -0.177 (-0.184 – -0.170)*** | -0.172 (-0.180 – -0.165)*** | -0.169 (-0.177 – -0.162)*** | -0.169 (-0.177 – -0.162)*** | ||
| Education (Medium) | -0.01 (-0.016 – -0.004)*** | -0.007 (-0.013 – -0.001)* | -0.008 (-0.014 – -0.002)* | |||
| Education (Low) | -0.015 (-0.022 – -0.007)*** | -0.006 (-0.014–0.002) | -0.007 (-0.014–0.001) | |||
| Non-partnered | -0.011 (-0.016 – -0.005)*** | -0.010 (-0.016 – -0.005)*** | -0.010 (-0.015 – -0.005)*** | |||
| English as 2nd language | -0.012 (-0.021 – -0.003)* | -0.006 (-0.015–0.003) | -0.005 (-0.014–0.004) | |||
| Unemployed or not in the labour force | -0.038 (-0.043 – -0.033)*** | -0.04 (-0.046 – -0.035)*** | -0.04 (-0.046 – -0.035)*** | |||
| Income (A$10,000) | 0.001 (0.000–0.001)*** | 0.000 (0.000–0.001)*** | 0.000 (0.000–0.001)*** | |||
| Low social support | -0.052 (-0.057 – -0.047)*** | -0.050 (-0.055 – -0.045)*** | -0.050 (-0.055 – -0.045)*** | |||
| Major life events | -0.024 (-0.028 – -0.020)*** | -0.024 (-0.028 – -0.020)*** | -0.024 (-0.028 – -0.020)*** | |||
| Low diet quality | -0.012 (-0.017 – -0.007)*** | -0.012 (-0.017 – -0.007)*** | ||||
| Low frequency of physical activity | -0.045 (-0.049 – -0.040)*** | -0.045 (-0.049 – -0.040)*** | ||||
| Smoking | -0.017 (-0.024 – -0.010)*** | -0.017 (-0.024 – -0.010)*** | ||||
| High-risk alcohol use | 0.013 (0.007–0.020)*** | 0.013 (0.007–0.020)*** | ||||
|
Life changed by Covid (Great extent) |
-0.009 (-0.020–0.001) | |||||
| Life changed by Covid (Moderate extent) | 0.004 (-0.006–0.014) | |||||
|
Life changed by Covid (Little extent) |
0.004 (-0.006–0.014) | |||||
| Random effect | ||||||
| Level-2 variance | 0.020 | 0.020 | 0.019 | 0.019 | 0.019 | 0.019 |
| Level-1 variance | 0.021 | 0.018 | 0.012 | 0.010 | 0.010 | 0.010 |
| Summary | ||||||
| No. participants | 10,315 | 10,315 | 10,281 | 10,228 | 10,043 | 10,038 |
| No. observations | 29,163 | 29,163 | 28,462 | 27,549 | 25,399 | 25,390 |
| Marginal R-squared | 0.246 | 0.307 | 0.418 | 0.455 | 0.471 | 0.472 |
| Conditional R-squared | 0.630 | 0.634 | 0.638 | 0.648 | 0.654 | 0.655 |
P < 0.05, **P < 0.01, ***P < 0.001
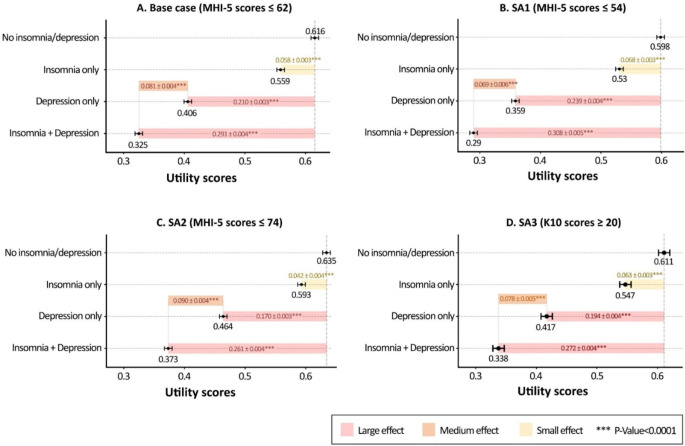
After adjusting for all covariates and the interaction effect of insomnia and depression, marginal mean utility scores for individuals with insomnia only, depression only, and comorbid insomnia and depression were calculated to be 0.559 (95% CI: 0.550–0.568), 0.406 (95% CI: 0.398–0.415) and 0.325 (95% CI: 0.316–0.335), respectively. These scores were significantly lower than those without insomnia and depression (0.616, 95% CI: 0.609–0.624). Figure 2 and Table S6 in the supplementary materials present differences in marginal mean utility scores and effect sizes across the pairwise comparisons. The standardised effect sizes for insomnia only, depression only and comorbid insomnia and depression were 0.420 (small), 1.530 (large), and 2.120 (large), respectively. For individuals with depression, the marginal mean utility score of those experiencing insomnia was 0.081 (SE:0.004, t-ratio: 18.157, P < 0.0001) lower than those not experiencing it (SES: 0.591, moderate effect).
Fig. 2.
Marginal mean utility scores and standard error of depression and/or insomnia. Adjusted for age, sex, mental and physical health, demographics, lifestyle, and Covid impact. (The error bars present marginal mean utility scores and their standard errors for each subgroup defined by insomnia and depression. The figures in coloured bars are marginal mean differences in utility scores between the two subgroups, along with their standard errors: insomnia only, depression only, and comorbid insomnia and depression compared to no insomnia and depression, and comorbid insomnia and depression compared to depression only)
Sensitivity and subgroup analyses
A comparison between the prevalence of depression and insomnia as well as mean utility scores in base case and sensitivity analyses is shown in Table SS in the supplementary materials. The prevalence values and the mean utility scores for subgroups using a cut-off point of K10 scores ≥ 20 to define depression (SA3) were nearly the same as the base case analysis.
All sensitivity analyses indicated that both insomnia and depression were significantly associated with the decreased utility scores (Table S5 in the supplementary materials). The regression coefficients of insomnia, depression, and the interaction term between the base case and SA3 were nearly similar. For SA1, the decrement of utility scores associated with insomnia or depression was slightly larger than the base case analysis, and the interaction term was not statistically significant (β: -0.001, 95% CI: -0.013 to 0.011). For SA2, while the coefficient for either insomnia or depression was slightly smaller, the coefficient for the interaction effect doubled compared to the base case analysis (β: -0.005, 95% CI: -0.060 to -0.039). Marginal mean utility scores of all subgroups and their pairwise differences, along with effect sizes, derived from all SAs are shown in Fig. 2B-D and Table S6 in the supplementary materials.
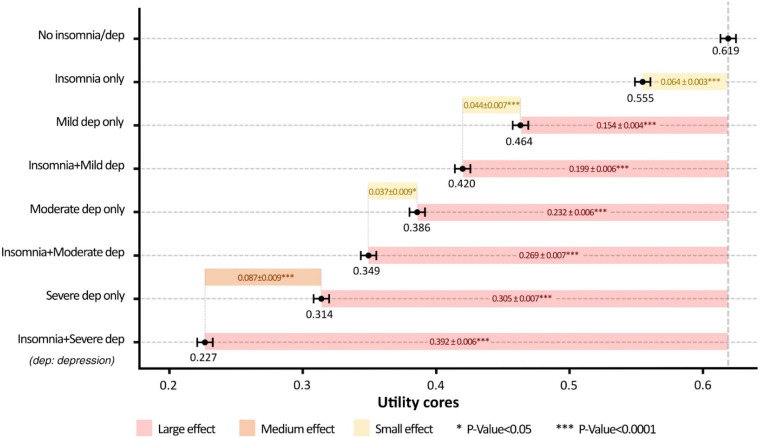
The subgroup analyses using K10 cut-off points found that higher levels of depression severity led to greater utility decrements. This is demonstrated by the regression coefficients from the multilevel model (Table S7 in the supplementary materials), as well as marginal mean utility scores for each subgroup defined by insomnia and depression (Fig. 3). In cases of mild/moderate depression, the interaction effect between insomnia and depression expressed the overlapping effect of insomnia and depression on utility scores (β: 0.019, 95% CI: 0.005 to 0.033 for mild; β: 0.027, 95% CI: 0.009 to 0.045 for moderate). However, for severe depression, the interaction effect indicated an additional decrement of utility scores attributed to the co-occurrence of insomnia and depression (β: -0.023, 95% CI: -0.042 to -0.005). Figure 3 and Table S8 in the supplementary materials present marginal mean utility scores for each subgroup defined by insomnia and depression and the mean differences in utility scores with effect sizes of insomnia and/or depression relative to no insomnia and depression and of comorbid insomnia and depression relative to depression only. Marginal mean scores were lower when depression severity was more severe. For people with mild depression, the marginal mean score was 0.464 ± 0.005 for those without insomnia and 0.420 ± 0.006 for those with insomnia. For people with moderate depression, the marginal mean score was 0.386 ± 0.007 for those without insomnia and 0.349 ± 0.007 for those with insomnia. For people with severe depression, the marginal mean score was 0.314 ± 0.008 for those without insomnia and 0.227 ± 0.007 for those with insomnia. The effect size of insomnia impact on utility scores was small for individuals with mild/moderate depression (SES: 0.322 for mild depression and 0.267 for moderate depression) but medium for individuals with severe depression (SES: 0.631).
Fig. 3.
Marginal mean utility scores and standard error of different depression severity with/without insomnia. Adjusted by age, sex, mental and physical health, demographics, lifestyle, and Covid impact. (The error bars present marginal mean utility scores and their standard errors for each subgroup defined by insomnia and depression. The figures in coloured bars are marginal mean differences in utility scores between the two subgroups, along with their standard errors: insomnia only, depression only, and comorbid insomnia and depression compared to no insomnia and depression, and comorbid insomnia and depression compared to depression only.)
Discussion
Our study found that insomnia and depression had substantive impacts on HRQoL as measured by SF-6D utility scores. The impairment of utility scores associated with comorbid insomnia and depression was, overall, significantly larger than the sum of their individual effects. To the best of our knowledge, this is the first study that has examined the reduction in utility scores associated with insomnia and depression, with the explicit consideration of the impacts of their interaction.
The subgroup analysis showed that increasing depression severity was associated with decreased levels of utility scores. The results of sensitivity analyses were also in line with this. The difference in utility scores between individuals with and without depression (regardless of the presence of insomnia) was found to be higher when using MHI-5 ≤ 54 (SA1) to define depression than when using MHI-5 ≤ 62 (base case) or MHI-5 ≤ 74 (SA2). This may be due to MHI-5 ≤ 54 capturing individuals with more severe depression. Previous studies have also observed similar findings [28, 66–68]. Moreover, depression severity also affected the combined effect between insomnia and depression on HRQoL. For mild-to-moderate depression, the interaction term in the model suggested the effects of insomnia and depression overlapped. For severe depression, the comorbidity of insomnia and depression incurred an additional negative effect greater than the overlapping effect. Further studies are required to strengthen this result.
Our study has revealed the burden of insomnia in those with depression. We observed a high prevalence of insomnia in this group (32–46%), which aligns with previous epidemiological studies [3, 69]. Insomnia significantly decreased HRQoL after adjusting for the effect of depression and other covariates. These findings are in line with another study that observed significant associations between higher severity levels of insomnia and lower utility scores in American adults with major depressive disorder [70]. Our study findings also underscored the bidirectional associations between insomnia and depression found in prior research [4–6]. The impairment of HRQoL associated with insomnia in adults with depression was found to have a medium effect size, while insomnia resulted in a small effect size on the reduction of HRQoL in those without depression. However, in practice, little effort is made to directly address insomnia when insomnia and depression concurrently occur [2, 71–73], and management of depression is expected to address both depression and insomnia symptoms [2, 71]. Indeed, chronic insomnia is 1.8 to 3.5 times more likely to perpetuate depression [8], and residual insomnia symptoms may increase the risk of depression relapse [74]. Current studies have shown that adding interventions targeting insomnia (including cognitive behavioural therapy and sedative-hypnotics) to depression treatments results in better HRQoL and more QALYs gained compared to depression treatment alone [75–77]. Our study findings suggest targeting the management of insomnia may improve the HRQoL of individuals with depression.
Comparing the utility scores measured in this study with previous research is limited. We were unable to compare the utility scores in the current study to population norms because there have been no publications on Australian population norms for the SF-6D. Moreover, the variety of MAUIs and methods applied to value health states also makes comparisons across studies difficult [78]. In this study, the utility scores were derived from the Australian algorithm developed by Norman et al. [38] who used the methods of discrete choice experiments (DCE) for the valuation of SF-6D health states. Other studies that have used the SF-6D have used the algorithm published by J. Brazier et al. [22] that used standard gamble (SG) instead [29, 66, 70]. The mean utility scores of individuals with insomnia or depression estimated in this current study were generally lower than the other studies. Norman et al. [38] explained that whereas J. Brazier et al. [22] valued no health states measured by the SF-6D as being below zero, there were 5% of health states in the Australian valuation study that were assigned a negative value.
Strengths and limitations
Our study estimated utility scores associated with insomnia and/or depression using data from a national survey with a large study sample size of 10,324 adults and an Australian algorithm [38]. Apart from showing that depression and insomnia are associated with substantive losses in utility, the utility scores derived from this study can be used in future clinical and economic studies on insomnia and depression. However, since we only used the Australian algorithm to value SF-6D health states, the generalisability of utility values estimated in this study to other countries is unclear. The preference-based scoring algorithm of the Australian population may not reflect the preferences of people in other countries. Although this study utilised validated cut-off points of MHI-5 or K10 [34, 63, 79, 80], the absence of formal diagnostic questions of depression is a study limitation. The measure of insomnia did not include the DSM-V diagnostic duration criteria, which require sleep difficulties to last for at least three months. As a result, our study findings are likely to be conservative since insomnia may also include cases of acute and short-term sleep disturbances. Nevertheless, the estimated prevalence was consistent with other large epidemiological studies [3, 69]. The application of multi-level mixed-effect models with three-wave panel data nested within individuals might offer more insights when working with a dataset containing a larger number of observations. This approach also allowed us to control individual time-constant unobserved factors as well as time effects and dynamics [81]. However, the repeated measures design with lengthy intervals between the HILDA waves restricted causal inferences between insomnia/depression and decreased utility scores. Finally, the impact of depression severity on utility scores was analysed in this study, but the effect of different insomnia severity levels on the outcomes was not examined.
Conclusions
This study has provided new insights into the burden associated with insomnia and depression in adult populations. The impact of insomnia and depression on utility scores, either individually or in combination, was significant. The co-occurrence of insomnia and depression was associated with an additional reduction in utility scores beyond the sum of their individual effects. Alleviating insomnia symptoms is suggested to be important for improving the HRQoL of adults with depression. The utility scores estimated in this study can be utilised in future clinical or economic studies.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
This study used data derived from the Household, Income and Labour Dynamics in Australia Survey (HILDA) which is funded and owned by the Australian Government [32]. Study findings were presented at the poster session of the 2023 HILDA Survey Research Conference on 27th, September 2023. We would like to thank Dr. Tim Powers for providing statistical analysis consulting.
Author contributions
Concept and design: All authors. Acquisition and analysis of data: PHL, LKDL. Interpretation of data: All authors. Statistical analysis: PHL. Drafting of the manuscript: PHL. Critical revision of the manuscript for important intellectual content: LKDL, SMWR, CM. Administrative, technical, or material support: All authors. Supervision: LKDL, SMWR, CM.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. The study is a part of a PhD project. Phuong Hong Le has received a scholarship and sponsorship from Monash University Health Economics Group and School of Public Health and Preventative Medicine for this project.
Data availability
The HILDA unit data can be accessed upon request via the Dataverse platform (https://dataverse.ada.edu.au/dataverse.xhtml?alias=hilda).
Declarations
Ethical approval
The HILDA survey was granted ethics approval by the Human Research Ethics Committee of the University of Melbourne (ID: 1647030). Consent was implied when participants agreed to be interviewed. Using secondary de-identified data, this study received low-risk ethics approval from the Human Research Ethics Committee (Project ID: 36681, date: 27th Feb 2023).
Competing interests
There is no conflict of interest to declare.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.The Institute for Health Metrics and Evaluation (IHME) (2020). Global Burden of Disease Study 2019 (GBD 2019) Data Resources. Retrieved May 2, 2021, from http://ghdx.healthdata.org/gbd-2019
- 2.Staner, L. (2010). Comorbidity of insomnia and depression. Sleep Medicine Reviews, 14(1), 35–46. 10.1016/j.smrv.2009.09.003 [DOI] [PubMed] [Google Scholar]
- 3.Stewart, R., Besset, A., Bebbington, P., Brugha, T., Lindesay, J., Jenkins, R., Singleton, N., & Meltzer, H. (2006). Insomnia comorbidity and impact and hypnotic use by age group in a national survey population aged 16 to 74 years. Sleep, 29(11), 1391–1397. 10.1093/sleep/29.11.1391 [DOI] [PubMed] [Google Scholar]
- 4.Zhang, M. M., Ma, Y., Du, L. T., Wang, K., Li, Z., Zhu, W., Sun, Y. H., Lu, L., Bao, Y. P., & Li, S. X. (2022). Sleep disorders and non-sleep circadian disorders predict depression: A systematic review and meta-analysis of longitudinal studies. Neuroscience and Biobehavioral Reviews, 134, 104532. 10.1016/j.neubiorev.2022.104532 [DOI] [PubMed] [Google Scholar]
- 5.Bao, Y. P., Han, Y., Ma, J., Wang, R. J., Shi, L., Wang, T. Y., He, J., Yue, J. L., Shi, J., Tang, X. D., & Lu, L. (2017). Cooccurrence and bidirectional prediction of sleep disturbances and depression in older adults: Meta-analysis and systematic review. Neuroscience & Biobehavioral Reviews, 75, 257–273. 10.1016/j.neubiorev.2017.01.032 [DOI] [PubMed] [Google Scholar]
- 6.Hertenstein, E., Feige, B., Gmeiner, T., Kienzler, C., Spiegelhalder, K., Johann, A., Jansson-Fröjmark, M., Palagini, L., Rücker, G., Riemann, D., & Baglioni, C. (2019). Insomnia as a predictor of mental disorders: A systematic review and meta-analysis. Sleep Medicine Reviews, 43, 96–105. 10.1016/j.smrv.2018.10.006 [DOI] [PubMed] [Google Scholar]
- 7.Hill Almeida, L. M., Flicker, L., Hankey, G. J., Golledge, J., Yeap, B. B., & Almeida, O. P. (2022). Disrupted sleep and risk of depression in later life: A prospective cohort study with extended follow up and a systematic review and meta-analysis. Journal of Affective Disorders, 309, 314–323. 10.1016/j.jad.2022.04.133 [DOI] [PubMed] [Google Scholar]
- 8.Pigeon, W. R., Hegel, M., Unützer, J., Fan, M. Y., Sateia, M. J., Lyness, J. M., Phillips, C., & Perlis, M. L. (2008). Is insomnia a perpetuating factor for late-life depression in the IMPACT cohort? Sleep, 31(4), 481–488. 10.1093/sleep/31.4.481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Biddle, D. J., Kelly, P. J., Hermens, D. F., & Glozier, N. (2018). The association of insomnia with future mental illness: Is it just residual symptoms? Sleep Health, 4(4), 352–359. 10.1016/j.sleh.2018.05.008 [DOI] [PubMed] [Google Scholar]
- 10.Dragioti, E., Radua, J., Solmi, M., Arango, C., Oliver, D., Cortese, S., Jones, P. B., Shin, I., Correll, J., C. U., & Fusar-Poli, P. (2022). Global population attributable fraction of potentially modifiable risk factors for mental disorders: A meta-umbrella systematic review. Molecular Psychiatry. 10.1038/s41380-022-01586-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Firth, J., Solmi, M., Wootton, R. E., Vancampfort, D., Schuch, F. B., Hoare, E., Gilbody, S., Torous, J., Teasdale, S. B., Jackson, S. E., Smith, L., Eaton, M., Jacka, F. N., Veronese, N., Marx, W., Ashdown-Franks, G., Siskind, D., Sarris, J., Rosenbaum, S., Carvalho, A. F., & Stubbs, B. (2020). A meta-review of lifestyle psychiatry: The role of exercise, smoking, diet and sleep in the prevention and treatment of mental disorders. World Psychiatry, 19(3), 360–380. 10.1002/wps.20773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hertenstein, E., Trinca, E., Wunderlin, M., Schneider, C. L., Züst, M. A., Fehér, K. D., Su, T., Straten, A., Berger, T., Baglioni, C., Johann, A., Spiegelhalder, K., Riemann, D., Feige, B., & Nissen, C. (2022). Cognitive behavioral therapy for insomnia in patients with mental disorders and comorbid insomnia: A systematic review and meta-analysis. Sleep Medicine Reviews, 62, 101597. 10.1016/j.smrv.2022.101597 [DOI] [PubMed] [Google Scholar]
- 13.Canadian Agency for Drugs and Technologies in Health (CADTH). (2018). Sep). Clinical evaluation of interventions for the management of Insomnia: A review of reviews. CADTH.
- 14.Rios, P., Cardoso, R., Morra, D., Nincic, V., Goodarzi, Z., Farah, B., Harricharan, S., Morin, C. M., Leech, J., Straus, S. E., & Tricco, A. C. (2019). Comparative effectiveness and safety of pharmacological and non-pharmacological interventions for insomnia: An overview of reviews. Systematic Reviews, 8(1), 281. 10.1186/s13643-019-1163-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morphy, H., Dunn, K. M., Lewis, M., Boardman, H. F., & Croft, P. R. (2007). Epidemiology of insomnia: A longitudinal study in a UK population. Sleep, 30(3), 274–280. [PubMed] [Google Scholar]
- 16.Yin, S., Njai, R., Barker, L., Siegel, P. Z., & Liao, Y. (2016). Summarizing health-related quality of life (HRQOL): Development and testing of a one-factor model. Popul Health Metr, 14, 22. 10.1186/s12963-016-0091-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization (WHO) (2012). WHOQOL: Measuring Quality of Life. from https://www.who.int/tools/whoqol
- 18.Hays, R. D., Sherbourne, C. D., & Mazel, R. (1995). User’s Manual for the Medical Outcomes Study (MOS) Core Measures of Health-Related Quality of Life. RAND Corporation.
- 19.Richardson, J., McKie, J., & Bariola, E. (2014). Multiattribute utility instruments and their use. Encyclopedia of Health Economics, 341–357.
- 20.Brazier, J., Ratcliffe, J., Saloman, J., & Tsuchiya, A. (2017). Measuring and valuing health benefits for economic evaluation. Oxford University Press.
- 21.EuroQoL (2023). EQ-5D - User guides. Retrieved Oct 2023, from https://euroqol.org/information-and-support/documentation/user-guides/
- 22.Brazier, J., Roberts, J., & Deverill, M. (2002). The estimation of a preference-based measure of health from the SF-36. Journal of Health Economics, 21(2), 271–292. 10.1016/s0167-6296(01)00130-8 [DOI] [PubMed] [Google Scholar]
- 23.Horsman, J., Furlong, W., Feeny, D., & Torrance, G. (2003). The Health utilities Index (HUI): Concepts, measurement properties and applications. Health and Quality of Life Outcomes, 1, 54. 10.1186/1477-7525-1-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Richardson, J., Iezzi, A., Khan, M. A., & Maxwell, A. (2014). Validity and reliability of the Assessment of Quality of Life (AQoL)-8D multi-attribute utility instrument. Patient, 7(1), 85–96. 10.1007/s40271-013-0036-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Institute for Health and Care Excellence (NICE) (2022). NICE health technology evaluations: the manual. March 2023, from www.nice.org.uk/process/pmg36
- 26.Canadian Agency for Drugs and Technologies in Health (CADTH) (2021). Guidelines for the Economic Evaluation of Health Technologies: Canada. March 2023, from https://www.cadth.ca/guidelines-economic-evaluation-health-technologies-canada-0
- 27.The Pharmaceutical Benefits Advisory Committee (PBAC) (2016). Guidelines for preparing submissions to the Pharmaceutical Benefits Advisory Committee (PBAC) version 5.0. from https://pbac.pbs.gov.au/
- 28.Mihalopoulos, C., Engel, L., Le, L. K. D., Magnus, A., Harris, M., & Chatterton, M. L. (2018). Health state utility values of high prevalence mental disorders in Australia: Results from the National Survey of Mental Health and Wellbeing. Quality of Life Research, 27(7), 1815–1825. 10.1007/s11136-018-1843-2 [DOI] [PubMed] [Google Scholar]
- 29.Léger, D., Morin, C. M., Uchiyama, M., Hakimi, Z., Cure, S., & Walsh, J. K. (2012). Chronic insomnia, quality-of-life, and utility scores: Comparison with good sleepers in a cross-sectional international survey. Sleep Medicine, 13(1), 43–51. 10.1016/j.sleep.2011.03.020 [DOI] [PubMed] [Google Scholar]
- 30.Mihalopoulos, C., Chen, G., Iezzi, A., Khan, M. A., & Richardson, J. (2014). Assessing outcomes for cost-utility analysis in depression: Comparison of five multi-attribute utility instruments with two depression-specific outcome measures. British Journal of Psychiatry, 205(5), 390–397. 10.1192/bjp.bp.113.136036 [DOI] [PubMed] [Google Scholar]
- 31.Summerfield, M., Garrard, B., Nesa, M. K., Kamath, R., Macalalad, N., Watson, N., Wilkins, R., & Wooden, M. (2021). HILDA user manual – release 21: Melbourne Institute. Applied Economic and Social Research, University of Melbourne.
- 32.Department of Social Services, & Melbourne Institute of Applied Economic Social Research. (2022). The Household, Income and Labour Dynamics in Australia (HILDA) Survey, GENERAL RELEASE 21 (waves 1–21). ed.): ADA Dataverse. (V4Department of Social Services.
- 33.Rumpf, H. J., Meyer, C., Hapke, U., & John, U. (2001). Screening for mental health: Validity of the MHI-5 using DSM-IV Axis I psychiatric disorders as gold standard. Psychiatry Research, 105(3), 243–253. 10.1016/s0165-1781(01)00329-8 [DOI] [PubMed] [Google Scholar]
- 34.Cuijpers, P., Smits, N., Donker, T., ten Have, M., & de Graaf, R. (2009). Screening for mood and anxiety disorders with the five-item, the three-item, and the two-item Mental Health Inventory. Psychiatry Research, 168(3), 250–255. 10.1016/j.psychres.2008.05.012 [DOI] [PubMed] [Google Scholar]
- 35.Theunissen, M. J., Jansen, M., & van Gestel, A. (2011). Are mental health and binge drinking associated in Dutch adolescents? Cross-sectional public health study. BMC Research Notes, 4(1), 100. 10.1186/1756-0500-4-100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (5th ed.). ed.). American Psychiatric Association.
- 37.Butterworth, P., & Crosier, T. (2004). The validity of the SF-36 in an Australian National Household Survey: Demonstrating the applicability of the Household Income and Labour Dynamics in Australia (HILDA) Survey to examination of health inequalities. Bmc Public Health, 4(1), 44. 10.1186/1471-2458-4-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Norman, R., Viney, R., Brazier, J., Burgess, L., Cronin, P., King, M., Ratcliffe, J., & Street, D. (2014). Valuing SF-6D Health States using a Discrete Choice Experiment. Medical Decision Making, 34(6), 773–786. 10.1177/0272989x13503499 [DOI] [PubMed] [Google Scholar]
- 39.Hölzel, L., Härter, M., Reese, C., & Kriston, L. (2011). Risk factors for chronic depression–a systematic review. Journal of Affective Disorders, 129(1–3), 1–13. 10.1016/j.jad.2010.03.025 [DOI] [PubMed] [Google Scholar]
- 40.Lallukka, T., Sares-Jäske, L., Kronholm, E., Sääksjärvi, K., Lundqvist, A., Partonen, T., Rahkonen, O., & Knekt, P. (2012). Sociodemographic and socioeconomic differences in sleep duration and insomnia-related symptoms in Finnish adults. Bmc Public Health, 12(1), 565. 10.1186/1471-2458-12-565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sivertsen, B., Krokstad, S., Øverland, S., & Mykletun, A. (2009). The epidemiology of insomnia: Associations with physical and mental health. The HUNT-2 study. Journal of Psychosomatic Research, 67(2), 109–116. 10.1016/j.jpsychores.2009.05.001 [DOI] [PubMed] [Google Scholar]
- 42.Haario, P., Rahkonen, O., Laaksonen, M., Lahelma, E., & Lallukka, T. (2013). Bidirectional associations between insomnia symptoms and unhealthy behaviours. Journal of Sleep Research, 22(1), 89–95. 10.1111/j.1365-2869.2012.01043.x [DOI] [PubMed] [Google Scholar]
- 43.Roy, T., & Lloyd, C. E. (2012). Epidemiology of depression and diabetes: a systematic review. J Affect Disord, 142 Suppl, S8-21. 10.1016/s0165-0327(12)70004-6 [DOI] [PubMed]
- 44.Norman, R., Church, J., van den Berg, B., & Goodall, S. (2013). Australian health-related quality of life population norms derived from the SF-6D. Australian and New Zealand Journal of Public Health, 37(1), 17–23. 10.1111/1753-6405.12005 [DOI] [PubMed] [Google Scholar]
- 45.Hare, D. L., Toukhsati, S. R., Johansson, P., & Jaarsma, T. (2014). Depression and cardiovascular disease: A clinical review. European Heart Journal, 35(21), 1365–1372. 10.1093/eurheartj/eht462 [DOI] [PubMed] [Google Scholar]
- 46.Baxter, S., Sanderson, K., Venn, A., Otahal, P., & Palmer, A. J. (2015). Construct validity of SF-6D health state utility values in an employed population. Quality of Life Research, 24(4), 851–870. 10.1007/s11136-014-0823-4 [DOI] [PubMed] [Google Scholar]
- 47.Metlaine, A., Sauvet, F., Gomez-Merino, D., Elbaz, M., Delafosse, J. Y., Leger, D., & Chennaoui, M. (2017). Association between Insomnia symptoms, job strain and burnout syndrome: A cross-sectional survey of 1300 financial workers. British Medical Journal Open, 7(1). 10.1136/bmjopen-2016-012816. e012816. [DOI] [PMC free article] [PubMed]
- 48.Yang, B., Wang, Y., Cui, F., Huang, T., Sheng, P., Shi, T., Huang, C., Lan, Y., & Huang, Y. N. (2018). Association between Insomnia and job stress: A meta-analysis. Sleep & Breathing = Schlaf & Atmung, 22(4), 1221–1231. 10.1007/s11325-018-1682-y [DOI] [PubMed] [Google Scholar]
- 49.Godos, J., Grosso, G., Castellano, S., Galvano, F., Caraci, F., & Ferri, R. (2021). Association between diet and sleep quality: A systematic review. Sleep Medicine Reviews, 57, 101430. 10.1016/j.smrv.2021.101430 [DOI] [PubMed] [Google Scholar]
- 50.Sweetman, A., Lack, L., McEvoy, R. D., Smith, S., Eckert, D. J., Osman, A., Carberry, J. C., Wallace, D., Nguyen, P. D., & Catcheside, P. (2021). Bi-directional relationships between co-morbid insomnia and sleep apnea (COMISA). Sleep Medicine Reviews, 60, 101519. 10.1016/j.smrv.2021.101519 [DOI] [PubMed] [Google Scholar]
- 51.Lerner, D. J., Levine, S., Malspeis, S., & D’Agostino, R. B. (1994). Job strain and health-related quality of life in a national sample. American Journal of Public Health, 84(10), 1580–1585. 10.2105/AJPH.84.10.1580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Paykel, E. S. (2008). Partial remission, residual symptoms, and relapse in depression. Dialogues Clin Neurosci, 10(4), 431–437. 10.31887/DCNS.2008.10.4/espaykel [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ji, X., Ivers, H., Savard, J., LeBlanc, M., & Morin, C. M. (2019). Residual symptoms after natural remission of insomnia: Associations with relapse over 4 years. Sleep, 42(8). 10.1093/sleep/zsz122 [DOI] [PMC free article] [PubMed]
- 54.Morin, C. M., Jarrin, D. C., Ivers, H., Mérette, C., LeBlanc, M., & Savard, J. (2020). Incidence, persistence, and Remission Rates of Insomnia over 5 years. JAMA Netw Open, 3(11), e2018782. 10.1001/jamanetworkopen.2020.18782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cohen, J. (1988). Statistical Power Analysis for the behavioral sciences. United Kingdom: Routledge.
- 56.Gałecki, A., & Burzykowski, T. (2013). Linear mixed-effects models using R. In. Springer.
- 57.Clarke, B. R. (2008). Linear models the theory and application of analysis of variance. Wiley.
- 58.Toprak, T. E. (2019). Analysis of differences between groups: The t-test and the analysis of variance (ANOVA) in language assessment (1 ed., pp. 179–197). Routledge.
- 59.Tong, S., & Lu, Y. (2001). Identification of confounders in the Assessment of the relationship between lead exposure and child development. Annals of Epidemiology, 11(1), 38–45. 10.1016/S1047-2797(00)00176-9 [DOI] [PubMed] [Google Scholar]
- 60.Oftedal, S., Glozier, N., Holliday, E. G., & Duncan, M. J. (2020). Diet quality and depressive symptoms. Assessing the direction of the association in a population-based cohort study. Journal of Affective Disorders, 274, 347–353. 10.1016/j.jad.2020.05.046 [DOI] [PubMed] [Google Scholar]
- 61.Kessler, R. C., Andrews, G., Colpe, L. J., Hiripi, E., Mroczek, D. K., Normand, S. L. T., Walters, E. E., & Zaslavsky, A. M. (2002). Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine, 32(6), 959–976. 10.1017/S0033291702006074 [DOI] [PubMed] [Google Scholar]
- 62.Australian Bureau of Statistics (2012). Use of the Kessler Psychological Distress Scale in ABS Health Surveys, Australia, 2007-08 Retrieved Mar, 2023, from https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4817.0.55.001Chapter92007-08
- 63.Andrews, G., & Slade, T. (2001). Interpreting scores on the Kessler Psychological Distress Scale (K10). Australian and New Zealand Journal of Public Health, 25(6), 494–497. 10.1111/j.1467-842x.2001.tb00310.x [DOI] [PubMed] [Google Scholar]
- 64.Victorian Government Department of Human Services. (2002). Victorian Population Health Survey 2001: Selected findings. The Rural and Regional Health and Aged Care Services Division.
- 65.Stallman, H. M., & Shochet, I. (2009). Prevalence of mental health problems in Australian university health services. Australian Psychologist, 44(2), 122–127. 10.1080/00050060902733727 [Google Scholar]
- 66.Kolovos, S., Bosmans, J. E., van Dongen, J. M., van Esveld, B., Magai, D., van Straten, A., van der Feltz-Cornelis, C., van Steenbergen-Weijenburg, K. M., Huijbregts, K. M., van Marwijk, H., Riper, H., & van Tulder, M. W. (2017). Utility scores for different health states related to depression: Individual participant data analysis. Quality of Life Research, 26(7), 1649–1658. 10.1007/s11136-017-1536-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lamers, L. M., Bouwmans, C. A., van Straten, A., Donker, M. C., & Hakkaart, L. (2006). Comparison of EQ-5D and SF-6D utilities in mental health patients. Health Economics, 15(11), 1229–1236. 10.1002/hec.1125 [DOI] [PubMed] [Google Scholar]
- 68.Revicki, D. A., & Wood, M. (1998). Patient-assigned health state utilities for depression-related outcomes: Differences by depression severity and antidepressant medications. Journal of Affective Disorders, 48(1), 25–36. 10.1016/s0165-0327(97)00117-1 [DOI] [PubMed] [Google Scholar]
- 69.Buysse, D. J., Angst, J., Gamma, A., Ajdacic, V., Eich, D., & Rössler, W. (2008). Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep, 31(4), 473–480. 10.1093/sleep/31.4.473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Joshi, K., Cambron-Mellott, M. J., Costantino, H., Pfau, A., & Jha, M. K. (2023). The clinical, economic, and patient-centric burden of insomnia symptom severity in adults with major depressive disorder in the United States. Brain and Behavior, 13(8), e3143. 10.1002/brb3.3143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Sweetman, A., Lack, L., Van Ryswyk, E., Vakulin, A., Reed, R. L., Battersby, M. W., Lovato, N., & Adams, R. J. (2021). Co-occurring depression and insomnia in Australian primary care: Recent scientific evidence. Medical Journal of Australia, 215(5), 230–236. 10.5694/mja2.51200 [DOI] [PubMed] [Google Scholar]
- 72.Ohayon, M. M., Shapiro, C. M., & Kennedy, S. H. (2000). Differentiating DSM-IV anxiety and depressive disorders in the general population: Comorbidity and treatment consequences. Canadian Journal of Psychiatry, 45(2), 166–172. 10.1177/070674370004500207 [DOI] [PubMed] [Google Scholar]
- 73.Matteson-Rusby, S. E., Pigeon, W. R., Gehrman, P., & Perlis, M. L. (2010). Why treat insomnia? Prim Care Companion J Clin Psychiatry, 12(1), PCC.08r00743. 10.4088/PCC.08r00743bro [DOI] [PMC free article] [PubMed]
- 74.Dombrovski, A. Y., Cyranowski, J. M., Mulsant, B. H., Houck, P. R., Buysse, D. J., Andreescu, C., Thase, M. E., Mallinger, A. G., & Frank, E. (2008). Which symptoms predict recurrence of depression in women treated with maintenance interpersonal psychotherapy? Depression and Anxiety, 25(12), 1060–1066. 10.1002/da.20467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Snedecor, S. J., Botteman, M. F., Schaefer, K., Sarocco, P., Barry, N., & Pickard, A. S. (2010). Economic outcomes of eszopiclone treatment in insomnia and comorbid major depressive disorder. The Journal of Mental Health Policy and Economics, 13(1), 27–35. [PubMed] [Google Scholar]
- 76.Watanabe, N., Furukawa, T. A., Shimodera, S., Katsuki, F., Fujita, H., Sasaki, M., Sado, M., & Perlis, M. L. (2015). Cost-effectiveness of cognitive behavioral therapy for insomnia comorbid with depression: Analysis of a randomized controlled trial. Psychiatry and Clinical Neurosciences, 69(6), 335–343. 10.1111/pcn.12237 [DOI] [PubMed] [Google Scholar]
- 77.McCall, W. V., Blocker, J. N., D’Agostino, R. Jr., Kimball, J., Boggs, N., Lasater, B., Haskett, R., Krystal, A., McDonald, W. M., & Rosenquist, P. B. (2010). Treatment of insomnia in depressed insomniacs: Effects on health-related quality of life, objective and self-reported sleep, and depression. Journal of Clinical Sleep Medicine, 6(4), 322–329. [PMC free article] [PubMed] [Google Scholar]
- 78.Peasgood, T., & Brazier, J. (2015). Is Meta-analysis for utility values appropriate given the potential impact different elicitation methods have on values? Pharmacoeconomics, 33(11), 1101–1105. 10.1007/s40273-015-0310-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rumpf, H. J., Meyer, C., Hapke, U., & John, U. (2001). Screening for mental health: Validity of the MHI-5 using DSM-IV Axis I psychiatric disorders as gold standard. Psychiatry Research, 105(3), 243–253. 10.1016/S0165-1781(01)00329-8 [DOI] [PubMed] [Google Scholar]
- 80.Yamazaki, S., Fukuhara, S., & Green, J. (2005). Usefulness of five-item and three-item Mental Health inventories to screen for depressive symptoms in the general population of Japan. Health and Quality of Life Outcomes, 3(1), 48. 10.1186/1477-7525-3-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hsiao, C. (2007). Panel data analysis—advantages and challenges. TEST, 16(1), 1–22. 10.1007/s11749-007-0046-x [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The HILDA unit data can be accessed upon request via the Dataverse platform (https://dataverse.ada.edu.au/dataverse.xhtml?alias=hilda).