Abstract
Current and projected shortages in the US health workforce have prompted policymakers to propose reforms to Medicare Graduate Medical Education (GME) and nursing programs. However, researchers have historically faced challenges in accurately predicting workforce trends; physician and nurse supply and demand all grew faster than expected over the past 2 decades. These discrepancies highlight the need for scenario-based workforce planning and projection models that estimate how a policy intervention would affect the workforce outcome of interest. In addition, policy options modeled should address not only increasing provider-to-population ratios but also improving health outcomes through innovative payment and care models.
Keywords: health workforce projection, health workforce policy, physician shortages, nurse shortages, scenario-based modeling
Senate Finance Committee Chair Ron Wyden and a bipartisan group of Finance Committee members recently outlined Medicare Graduate Medical Education (GME) reforms to address current and projected physician shortages in rural and underserved areas and in certain specialties, including primary care and psychiatry.1 Similarly, Representatives Haley Stevens and David Joyce reintroduced the Stop Nurse Shortages Act in May 2024, proposing to spend $10 million annually from fiscal years 2024 through 2028 for accelerated nursing degree programs.2 These policymakers were spurred to action by reports of current shortages that are projected to persist. However, it is unclear whether these proposed policies would alleviate health workforce shortages or improve the distribution of medical professionals.3,4
What past projections said about the present
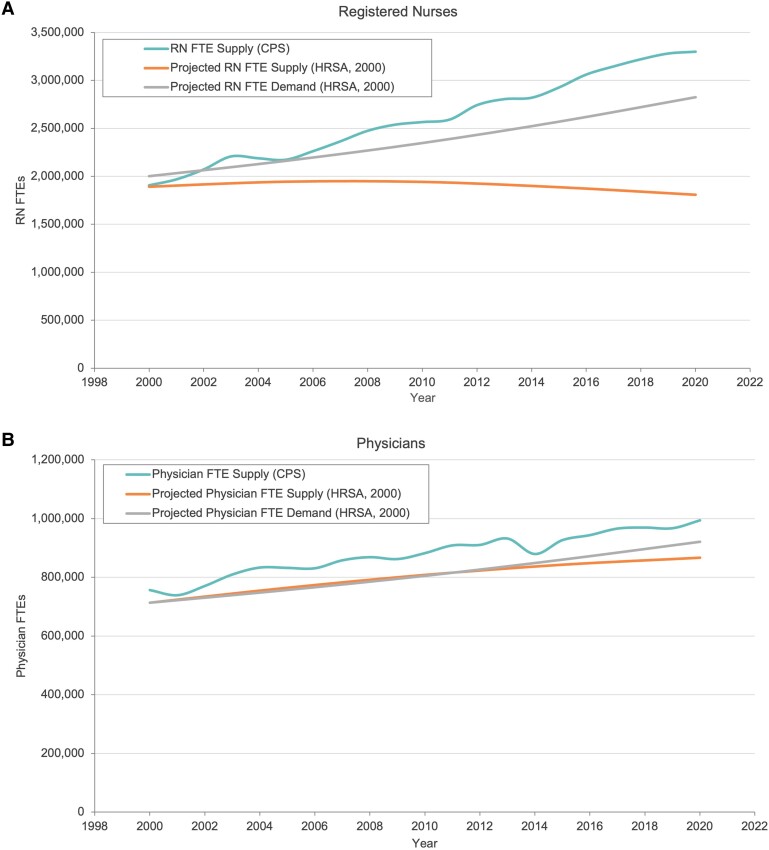
Predicting the size of the future workforce is difficult, even in the absence of policy change. Figure 1A displays a projection of supply and demand for registered nurses (RNs) made by the US Health Resources and Services Administration (HRSA) in 1996, compared with the actual supply of RNs from 2000 to 2020.5 The HRSA forecasted that the RN workforce would plateau at just under 2 million full-time equivalents (FTEs) in the late 2000s, and subsequently decline due to retiring baby boomer RNs and smaller incoming cohorts. Independent projections from that time also predicted a plateauing, and eventually declining RN workforce, albeit starting later—in the mid-2010s.6 Meanwhile, the 1996 HRSA forecast assumed that demand for RNs would grow from 2.0 to 2.8 million between 2000 and 2020, leading to a nursing shortage of over 1 million RN FTEs (35%) by 2020.
Figure 1.
Projection of supply and demand for registered nurses (A) and physicians (B) made by the US HRSA, compared with the actual supply of RNs and physicians from 2000 to 2020. Source: HRSA projections for US supply and demand of RNs (2000, projected to 2020) and physicians (2000, projected to 2020), and CPS (2000–2020). The actual supply of FTE RNs and physicians was calculated using employment data from the CPS. Abbreviations: CPS, Current Population Survey; FTE, full-time equivalent; HRSA, Health Resources and Services Administration; RN, registered nurse.
The projected shortages did not materialize. Instead of shrinking, total RN supply grew 73%, from 1.9 million in 2000 to nearly 3.3 million RN FTEs in 2020 (representing 16% growth in RNs per capita over this period). Similarly, for physicians, HRSA expected 866 400 physicians by 2020, far fewer than the 1 000 000 observed in 2020 (Figure 1B).7 These changes occurred even without major federal policy intervention, although there were state and philanthropic initiatives,8 and were likely also spurred by broader demographic and economic forces that influence the relative attractiveness of these key health care professions compared with other choices available to generations of students and workers seeking career changes.9
While nursing supply grew more quickly than expected, the demand forecast also missed the mark. Based mainly on population trends and 1990s utilization patterns, HRSA's projection of nursing demand for 2020 was far below the actual number of RNs that year, suggesting that we should have enjoyed a surplus of 600 000 RNs in 2020. Few observers would argue that was what occurred.
Takeaways from past health workforce projections
The mismatch between projections and reality demonstrates that there is a greater degree of change and flexibility in health care delivery than modelers and policymakers traditionally assume. For example, population aging in the United States was assumed to have predictable effects on demand for health care. Given that adults aged 65–84 years are far more likely to require inpatient hospital stays compared with children aged 1–17 years, a forecaster in 2000 might have reasonably anticipated a growing need for hospital beds due to population aging. Despite a nearly 55% increase in the US population aged 65 and above,10 the number of hospital stays in 2019 was only 0.3% higher than in 2000.11
There are also sustained differences in health care delivery at the regional and local level: South Dakota had nearly twice as many employed RNs per 1000 population as California in 2022,12 and Massachusetts had twice as many practicing physicians per 1000 population as Indiana (or Georgia) in 2020.13 Yet, the provision and experience of health care in these states are not as different as these numbers might suggest. As we have learned from decades of research published in the Dartmouth Atlas of Health Care, health care practice patterns adapt to the available resources, for better or worse.14
A call for scenario-based workforce planning
Forecasters are, of course, aware that their models are far from perfect. They generally rely on a limited set of forecastable factors and relationships, such as population trends by age and sex, while assuming past relationships, including care utilization patterns, technology in care delivery, and workforce participation, remain constant. Forecasting is an “all else equal” exercise, which is never the case in reality. But it still can be incredibly useful.
Forecasting can play out observed trends to their logical outcomes, alerting us to potential consequences. Even a basic understanding of whether a trend is likely to continue, increase, or decrease can provide valuable insights for policymakers and health workforce planners. Given the tremendous uncertainty in forecasts, we may be better off asking forecasters if supply will grow faster or more slowly than it has recently rather than estimating explicit shortages. We should also ask forecasters to evaluate how their projections bore out and what that says about how the models might be improved.
If the policy goal of shaping the future workforce is to improve health care delivery and, ultimately, health care outcomes, we should endeavor to refine our understanding of the impact of specific levers of policy or organizational change on the outcomes we are interested in. Past health workforce literature has revealed a need for more quantitative evidence regarding recommendations on workforce development, effectiveness, and policies.15 For example, how do payment rates, payment types (eg, fee-for-service vs capitation)m or the type and amount of risk for costs and outcomes influence physicians’ and nurses’ supply of services? How do salary levels and differentials among specialties affect the supply of nurses and specialty choices of physicians? How do workforce training programs and subsidies like those envisioned in the proposals before Congress affect patterns of the supply of clinicians and health care delivery? Having a sense that future supply of a clinician type might be 5% higher or 10% lower, all else equal, if we made a given payment change, is exactly the sort of estimates relied upon by policymakers when analyzing policy options and thus extremely helpful to the policy process. Forecasting combined with an improved understanding of the impact of key policy levers on the ultimate outcomes of interest can help support and drive decision making toward better policy and better outcomes for all.
Evaluating proposed workforce policies
The Senate Medicare GME Working Group proposed to address physician shortages by increasing the number of Medicare-supported residency slots from fiscal year 2027 through 2031, with 25% designated for primary care and 15% designated for psychiatry.1 The proposed policy provisions also included an updated allocation formula redefining rural hospitals to increase the number of slots in rural areas, as well as allowing Indirect Graduate Medical Education (IME) payments to support establishment of residency training programs in sole community hospitals (SCHs) and Medicare-dependent hospitals (MDHs), many of which serve the rural areas. In a parallel effort to address nurse shortages, the Stop Nurse Shortages Act proposed to support accelerated nursing programs through hiring and retaining faculty, expanding clinical training sites, and providing financial aid to students.2
These reforms may not address the root problems associated with the projected shortages. The current medical education payment structures—Direct Graduate Medical Education (DGME), based on Medicare patient loads and resident numbers, and IME, based on resident-to-bed ratios—do not ensure that residents are attracted to rural areas.16,17 Residency slots are disproportionately unfilled at smaller rural facilities.18 Without changes to the payment structure, the proposed policy may fall short of providing enough incentive for medical students to apply for these slots. Beyond that, physicians must be compensated at sufficient levels to stay in rural areas and choose less lucrative specialties such as primary care. Similarly, producing more nurses through accelerated training programs does not address the retention issue in the profession, or shortages in specialty areas that may require specialized training such as geriatric care.19,20
Furthermore, simply adding more professionals does not necessarily translate into better-quality care that meets population health needs. A recent review of health workforce projection models highlighted the importance of aligning projection models with population health needs, considering different health care delivery models (particularly shifts from profession-specific to team-oriented approaches), and incorporating budgetary analysis that factors in potential cost savings from improved health outcomes.21 Given the rapid changes in care delivery and existing unmet health needs, new types of professionals and care models may be required. It may be time to focus on policies targeted at improved health outcomes and quality of care over provider ratios. Policies that incentivize and mobilize the existing workforce, such as updated payment models for physicians and nurses, or promoting team-based care and community health workers, may offer more sustainable solutions.22 Projections of the effects of such policies on both numbers of health professionals and population health outcomes would provide more actionable information to policymakers than shortage forecasts alone.
Supplementary Material
Contributor Information
Melinda J B Buntin, Department of Health Policy and Management, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD 21205, United States; Carey Business School, Johns Hopkins University, Baltimore, MD 21202, United States.
Mingxin Chen, Department of Population, Family and Reproductive Health, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD 21205, United States.
David I Auerbach, Research and Cost Trends, Massachusetts Health Policy Commission, Boston, MA 02109, United States.
Supplementary material
Supplementary material is available at Health Affairs Scholar online.
Funding
None.
Data availability
All data are publicly available.
Notes
- 1. US Senate Committee on Finance . Wyden, Bipartisan finance members outline proposal to improve Medicare physician training to reduce workforce shortages. May 24, 2024. Accessed July 12, 2024. https://www.finance.senate.gov/chairmans-news/wyden-bipartisan-finance-members-outline-proposal-to-improve-medicare-physician-training-to-reduce-workforce-shortages
- 2. Stop Nurse Shortages Act . HR 8330, 118th Congress (2023-2024). 2024. Accessed September 7, 2024. https://www.congress.gov/bill/118th-congress/house-bill/8330/text
- 3. Leider JP, Yeager VA, Kirkland C, Krasna H, Hare Bork R, Resnick B. The state of the US public health workforce: ongoing challenges and future directions. Annu Rev Public Health. 2023;44(1):323–341. 10.1146/annurev-publhealth-071421-032830 [DOI] [PubMed] [Google Scholar]
- 4. US Government Accountability Office . Physician Workforce: Locations and Types of Graduate Training Were Largely Unchanged, and Federal Efforts May Not Be Sufficient to Meet Needs. 2017. Accessed September 7, 2024. https://www.gao.gov/assets/gao-17-411.pdf
- 5. Biviano MB, Tise S, Dall TM. What is behind HRSA's projected U.S. supply, demand, and shortages of registered nurses. In: Gupta A, Harding A, eds. Modelling Our Future: Population Ageing, Health and Aged Care. Vol 16. International Symposia in Economic Theory and Econometrics. Emerald Group Publishing Limited; 2007:343–374. [Google Scholar]
- 6. Buerhaus PI, Staiger DO, Auerbach DI. Implications of an aging registered nurse workforce. JAMA. 2000;283(22):2948. 10.1001/jama.283.22.2948 [DOI] [PubMed] [Google Scholar]
- 7. Dall T, Grover A, Roehrig C, et al. Physician supply and demand: projections to 2020. Bureau of Health Professions, Health Resources and Services Administration, U.S. Department of Health and Human Services; 2006. Accessed July 18, 2024. https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/data-research/physician-2020-projections.pdf [Google Scholar]
- 8. Johnson & Johnson Nursing . The Johnson & Johnson Campaign for Nursing's Future Celebrates Fourteen Years. February 23, 2016. Accessed October 29, 2024. https://nursing.jnj.com/the-johnson-johnson-i-campaign-for-nursings-future-i-celebrates-fourteen-years
- 9. Buerhaus PI, Staiger DO, Auerbach DI. New signs of a strengthening U.S. nurse labor market? Younger nurses and men entering nursing drove the rising numbers of hospital nurses in 2003, but the shortage is not necessarily a thing of the past. Health Aff (Millwood). 2004;23(Suppl 1):W4-526–W4-533. 10.1377/hlthaff.W4.526 [DOI] [PubMed] [Google Scholar]
- 10. Administration on Aging; Administration for Community Living; US Department of Health and Human Services . 2020 Profile of Older Americans. 2021. Accessed October 29, 2024. https://acl.gov/sites/default/files/Profile%20of%20OA/2020ProfileOlderAmericans_RevisedFinal.pdf
- 11. Healthcare Cost and Utilization Project (HCUPnet) . Rockville, MD: Agency for Healthcare Research and Quality; 2000-2020. Accessed July 14, 2024. https://datatools.ahrq.gov/hcupnet
- 12. Bureau of Labor Statistics, US Department of Labor, Occupational Employment and Wage Statistics. Registered nurses . Accessed July 18, 2024. https://www.bls.gov/oes/current/oes291141.htm
- 13. Association of American Medical Colleges (AAMC) . 2021 State Physician Workforce Data Report. 2022. Accessed June 7, 2024. https://store.aamc.org/downloadable/download/sample/sample_id/506/
- 14. Chandra A, Staiger DO. Productivity spillovers in health care: evidence from the treatment of heart attacks. J Polit Econ. 2007;115(1):103–140. 10.1086/512249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Beck AJ, Boulton ML. Building an effective workforce. Am J Prev Med. 2012;42(5):S6–S16. 10.1016/j.amepre.2012.01.020 [DOI] [PubMed] [Google Scholar]
- 16. Congressional Research Office . Medicare Graduate Medical Education payments: an overview. 2022. Accessed September 7, 2024. https://crsreports.congress.gov/product/pdf/IF/IF10960
- 17. He K, Whang E, Kristo G. Graduate medical education funding mechanisms, challenges, and solutions: a narrative review. Am J Surg. 2021;221(1):65–71. 10.1016/j.amjsurg.2020.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. US Government Accountability Office . Physician workforce: caps on Medicare-funded Graduate Medical Education at teaching hospitals. 2021. Accessed September 7, 2024. https://www.gao.gov/assets/gao-21-391.pdf
- 19. Buerhaus P, Fraher E, Frogner B, Buntin M, O’Reilly-Jacob M, Clarke S. Toward a stronger post-pandemic nursing workforce. N Engl J Med. 2023;389(3):200–202. 10.1056/NEJMp2303652 [DOI] [PubMed] [Google Scholar]
- 20. Spetz J. Changes in registered nurse employment and education capacity during the COVID-19 pandemic and the risk of future shortages. Health Serv Res. 2021;56(S2):47–47. 10.1111/1475-6773.13814 [DOI] [Google Scholar]
- 21. Lee JT, Crettenden I, Tran M, et al. Methods for health workforce projection model: systematic review and recommended good practice reporting guideline. Hum Resour Health. 2024;22(1):25. 10.1186/s12960-024-00895-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Auerbach DI, Levy DE, Maramaldi P, et al. Optimal staffing models to care for frail older adults in primary care and geriatrics practices in the US: study examines optimal staffing levels to care for frail older adults in primary care and geriatrics practices. Health Aff (Millwood). 2021;40(9):1368–1376. 10.1377/hlthaff.2021.00401 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data are publicly available.