Abstract
Introduction
The private sector plays a substantial role in delivering and financing healthcare in low- and middle-income countries (LMICs). Supporting governments to govern the private sector effectively, and so improve outcomes across the health system, requires an understanding of the evidence base on private health sector governance. This paper reports on a scoping review, which synthesised evidence on the approaches used to govern private sector delivery and financing of healthcare in LMICs, the effectiveness of these approaches and the key enablers and barriers to strengthening governance.
Methods
We undertook a systematic search of databases of published articles and grey literature to identify eligible papers published since 2010, drawing on WHO’s governance definition. Data were extracted into a pretested matrix and analysed using narrative synthesis, structured by WHO’s six governance behaviours and an additional cross-cutting theme on capacities.
Results
107 studies were selected as relevant, covering 101 LMICs. Qualitative methods and document/literature review were predominant. The findings demonstrate the relevance of the WHO governance behaviours, but the lack of robust evidence for approaches to implementing them. Valuable insights from the literature include the need for a clear vision around governance aims; the importance of ensuring that policy dialogue processes are inclusive and transparent, avoiding interest group capture; the benefits of exploiting synergies between governance mechanisms; and the need to develop capacity to enact governance among both public and private actors.
Conclusion
Governance choices shape not just the current health system, but also its future development. Common barriers to effective governance must be addressed in policy design, stakeholder engagement, public and private sector accountability, monitoring and capacity. Achieving this will require in-depth explorations of governance mechanisms and more rigorous documentation of implementation and outcomes in diverse contexts.
Keywords: Global health, Health policies and all other topics, Health policy, Health systems, Public health
WHAT IS ALREADY KNOWN ON THIS TOPIC
The private sector plays a substantial and expanding role in delivering and financing healthcare in most low- and middle-income countries (LMICs).
The private healthcare sector in many LMICs is argued to be undergoverned, detrimentally impacting on patients’ rights and safety and national health policy goals.
There is increasing interest in the governance of private healthcare, and a growing literature in this area, covering experiences across diverse settings.
WHAT THIS STUDY ADDS
This is the first comprehensive review of governance of the private healthcare sector in LMICs.
It describes the approaches used for private sector governance, structured by WHO’s six governance behaviours, and synthesises the evidence on their effectiveness and enablers/barriers.
The review emphasises the importance of private sector governance in shaping the current health system and its future development.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Insights include the need for a clear vision for the private sector’s role, inclusive and transparent policy processes, effective management of conflicts of interest and development of key capacities and institutions in public and private sectors.
More robust empirical studies are needed on governance interventions, with particular gaps including private health insurance regulation, public accountability mechanisms, digital health, medical tourism and governance strategies in fragile and conflict-affected settings.
The findings have informed the development of a ‘Progression Pathway for the Governance of Mixed Health Systems’ to support countries in strengthening governance.
Introduction
The private sector plays a substantial role in delivering and financing healthcare in most low- and middle-income countries (LMICs).1 2 Defined as all individuals and organisations involved in provision of health services that are neither owned nor directly controlled by government,3 the private sector encompasses both for-profit and not-for-profit entities, including private hospitals and clinics, laboratories, blood banks, pharmacy retailers and wholesalers, equipment providers, private insurers and health maintenance organisations (HMO). The role and scope of private sector involvement in healthcare has expanded rapidly in recent decades, driven by income growth, urbanisation and dissatisfaction with the coverage and quality of public provision.1 4 Private providers play a substantial role in the delivery of both ambulatory and inpatient care, including for maternal and child health services, and infectious and non-communicable diseases, with different segments of the private sector serving different income groups.5,7
Historically, LMIC governments perceived their main role to be the finance and delivery of healthcare through public facilities, with engagement with the private sector restricted to fairly minimal regulation of private providers and, in some contexts, partnerships with faith-based organisation (FBO) facilities. In recent years, greater interest has emerged in the government’s role in governing private healthcare more broadly,8 reflecting both the growth in this sector, and recognition that achieving universal health coverage (UHC) in a context of ageing populations, evolving disease burden and fiscal pressures will require states to harness the infrastructure, resources and skills of both the public and private sectors.9 However, currently the private sector is arguably undergoverned in many LMIC settings, with the government’s efforts to incentivise and control private behaviour seen as inadequate in terms of safeguarding patients and achieving health policy goals.4
Multiple definitions of health system governance have been proposed.10 It is defined by the WHO as ‘ensuring strategic policy frameworks exist and are combined with effective oversight, coalition-building, regulation, attention to system design and accountability’.11 WHO’s own focus on the private sector has evolved over the past 25 years. In 2010, the World Health Assembly called for enhanced engagement, oversight and regulation of private healthcare providers.12 In 2019, a WHO call to action emphasised the importance of private sector engagement in advancing the Sustainable Development Goals agenda.9 In response, WHO established a Technical Advisory Group on the Governance of the Private Sector for UHC, which developed a strategy entitled ‘Engaging the private health service delivery sector through governance in mixed health systems’.13 This strategy drew on work by Travis et al14 on health system stewardship functions to articulate six governance behaviours required for the effective governance of mixed health systems (table 1).15
Table 1. The six governance behaviours15.
| Governance behaviour | Definition |
| Deliver strategy | Government articulates clear strategic objectives for the health system and the role of the private sector. |
| Enable stakeholders | Government influences private sector operation and performance through financing and regulatory policies. |
| Foster relations | Inclusive policy processes involve a broad range of stakeholders, including the private sector. |
| Build understanding | Government ensures access to comprehensive and high-quality data on the private sector’s operation and performance. |
| Align structures | Actions are taken to coordinate and align private and public sectors in service delivery. |
| Nurture trust | Measures are implemented to safeguard patient rights and financial welfare in private sector interactions. |
Supporting LMIC governments to effectively implement these behaviours requires a detailed understanding of the evidence base on private healthcare governance in these settings. While existing literature reviews cover various aspects of health system governance more broadly, or in specific settings, for specific purposes or through specific mechanisms,1016,32 a comprehensive review on the governance of the private health sector is lacking. A scoping review was therefore commissioned by WHO to synthesise the existing literature on the six governance behaviours in LMICs. The review explored three research questions for each of the governance behaviours:
How do various entities approach the governance of the private health sector in LMICs?
To what extent are these approaches effective in governing the private health sector?
What are the key enablers and barriers to the adoption of governance approaches, and what potential avenues have been identified to strengthen governance?
Given the exploratory nature of the review, the broad scope of the research questions, and their application to an extremely diverse set of governance approaches, using a wide range of qualitative and quantitative evidence types, it was not appropriate to apply systematic review methods.33 We therefore used a scoping review methodology to both summarise the nature and coverage of the literature and provide a descriptive synthesis of the findings.33 34
Methods
Eligibility criteria, screening and article selection
We adopted WHO’s definition of health system governance provided above of ‘ensuring strategic policy frameworks exist and are combined with effective oversight, coalition-building, regulation, attention to system design and accountability’11 and further drew on the conceptualisation of the governance behaviours13 15 to identify eligible papers. We included papers concerning governance of any for-profit and not-for-profit, formal and informal private actors having a role in health financing and service delivery in any low- or middle-income country, but excluded other private actors such as manufacturers, social care, training institutions and producers of unhealthy commodities. We included papers concerning governance at national or subnational level but excluded papers on global/multilateral governance. We took a broad approach to eligibility by publication type, including published and grey literature, and quantitative and qualitative methods, literature reviews and evidence syntheses, in all languages (we did not include original policy, regulatory or legislative documents). We restricted the search to papers published from January 2010 to ensure relevance of the health systems context to the present day (while allowing rare exceptions for earlier seminal pieces). Full details on the inclusion criteria are provided in online supplemental table S1.
Systematic searches were conducted in Medline OVID, Scopus and Web of Science in January 2023 using free text and MeSH terms related to the domains of ‘private sector’ and ‘governance’ and ‘health’ (for full search strategies see online supplemental materials 2). Grey literature was identified through expert consultations and by searching the publication repositories of a range of websites of large international non-governmental organisations (INGOs), donor bodies, grant organisations and universities (eg, Results for Development, WHO, World Bank e-Library, Institute of Development Studies, University of Sydney, Lee Kuan Yew School of Public Policy) using a shorter set of search terms. Three reviewers (SS, SN, AB) piloted the screening process on a common set of articles, and then each screened a tranche of the remaining articles independently, with support from all other authors to discuss articles for which inclusion was uncertain, with final decisions reached through consensus.
Given the very large number of items identified through database searches, title and abstract screening was conducted using the ASReview machine learning tool to prioritise papers for screening. In line with previous practice, the reviewers screened at least 10% of their individual tranches and then continued to screen until they had identified 50 irrelevant articles in a row (the stopping rule).35,37 Full-text review was conducted for all articles screened as potentially eligible and of grey literature.
Data extraction and analysis
Data extraction was performed using a pretested matrix in Microsoft Excel independently by four reviewers (SS, SN, AB, DB), with support from all authors. Data extraction focused on the three research questions. We extracted information from the literature reviews using the same approach that we used for empirical papers; we did not go back to the original sources or try to distinguish between evidence synthesised from pre-2010 and post-2010 papers. A narrative synthesis was conducted, with findings organised around the three research questions for each of the six governance behaviours, and an additional cross-cutting theme on capacities for governance.
Patient and public involvement
No patients or members of the public were involved in this study.
Results
Summary of the literature included
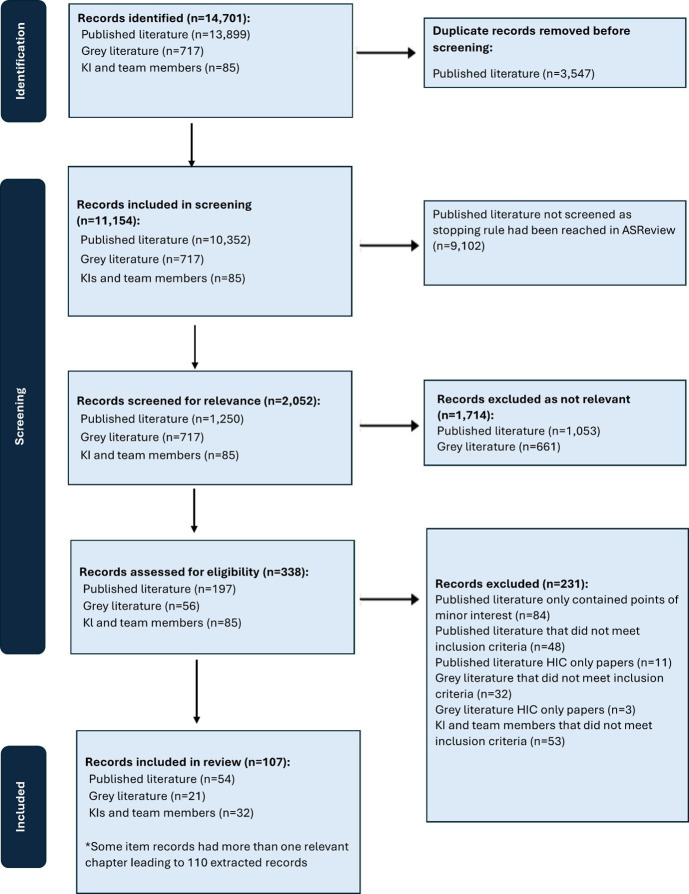
Our initial searches identified 13 899 records from databases, 717 reports identified through the web search and 85 papers from experts before deduplication. Following deduplication and screening, 338 records were selected for full-text review, of which 107 were selected for inclusion, or 110 items (some documents were books with more than one relevant chapter) (figure 1). We included three papers published pre-2010 that were considered highly significant in the development of the study of private sector governance.38,40
Figure 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram. KI, Key informants; HIC, High income country.
The characteristics of the included papers are shown in table 2 (more detail on each individual study is provided in online supplemental materials 1). The largest category of private actors studied was private facilities, followed by private health insurers and non-governmental organisations (NGOs). Regulation and contracting were the most common governance mechanisms discussed. Papers were identified covering 101 LMICs, including some from all six WHO regions. We found the highest concentration of papers covering LMICs in the African Region, followed by the South-East Asian Region and Eastern Mediterranean Region. Concerning the research methods used, qualitative methods and document/literature review were predominant.
Table 2. Characteristics of included studies.
| Paper characteristics* | Total papers extracted: 110 |
| Number of papers | 110 |
| Types of private sector actors covered | |
| Private healthcare facilities (hospitals, health centres, clinics, etc) | 92 |
| Private insurance companies or HMOs | 30 |
| Non-governmental organisations (NGOs) (national and international)/civil society organisations (CSOs) | 24 |
| Pharmacies and other retailers | 21 |
| Laboratories | 7 |
| Governance tools discussed | |
| Regulation/legislation | 62 |
| Contracting/purchasing | 47 |
| Support/collaboration/guidance | 22 |
| Accreditation | 8 |
| Taxation | 1 |
| Public accountability mechanisms | 5 |
| Level of governance covered | |
| National | 88 |
| Subnational | 30 |
| WHO regions of LMICs covered | |
| African Region (AFR) | 63 |
| Region of the Americas (AMR) | 24 |
| South-East Asian Region (SEAR) | 43 |
| European Region (EUR) | 16 |
| Eastern Mediterranean Region (EMR) | 29 |
| Western Pacific Region (WPR) | 27 |
| Journal/publication type | |
| Health and health systems journals | 62 |
| Social policy and development journals | 11 |
| Reports | 27 |
| Other† | 9 |
| Data collection methods | |
| Qualitative study | 45 |
| Quantitative study | 3 |
| Mixed methods | 19 |
| Reviews (document/literature) | 38 |
| N/A‡ | 5 |
Many publications include more than one category of private sector actor, governance tool, WHO region, or data collection method.
Other publications include book chapters, policy briefs, and academic theses.
These are papers which do not employ any data collection method and which are conceptual in nature.
HMOshealth maintenance organisationsLMICslow- and middle-income countries
We present the findings, organised by governance behaviour.
Deliver strategy
Deliver strategy is about articulating clear strategic goals and objectives for the health system and a clear definition of roles for the private health sector in achieving these. To assess whether the government had defined clear roles for the private sector, we considered evidence on the existence of up-to-date policies (eg, legal documents or policy statements) that define clear objectives for the private sector, in line with health system goals, and an articulation of how specific policy mechanisms will be used to influence the operation and performance of the private sector in line with these objectives.15
The literature indicates widespread inclusion of the private sector in national health sector strategies, policies and plans. A 2011 assessment found that over 85% of African countries mentioned the private sector in national policies, though the content varied from just recognising its role to giving it a prominent position in achieving strategic aims.41 A more recent 2020 assessment of 17 LMICs reported that all countries included the private sector in policies or strategic plans, though only a few had established a formal partnership framework.2 Specific private health sector or public–private partnership policies were observed in a minority of LMICs,241,44 and in some settings vertical programmes had their own private sector strategies.28 45,47
There is consensus across the literature on the importance of strong strategic policy direction for private sector governance.241 45 48,51 However, there is limited evidence on the specific impact of including the private sector in policy on subsequent governance arrangements, perhaps reflecting that it is challenging to separate this impact from other drivers for enhanced governance. There is evidence that in many settings inclusion in policy documents has not translated into a clear vision for the private sector’s role, and that implementation is limited.2 8 41 46 51 52
In earlier years, a barrier to the inclusion of the private sector in policy was that its governance was not seen as a priority for Ministries of Health (MoHs). Other barriers included a lack of relevant skills and funding in the public sector, an absence of private provider organisations to interface with and mutual mistrust.43 53 54 In some settings, such as India, this was reinforced by resistance from private actors to greater regulation.54 More recently, there has been increased focus on private sector inclusion in health policy, facilitated by better information on its growing size and complexity.46 Other factors stimulating greater inclusion of the private sector in policy have included the influence of external donors and technical advisors, and perceived positive results from private sector engagement in priority health programmes such as family planning and tuberculosis (TB).43 44 46 51 54
Enable stakeholders
Enable stakeholders covers the government’s use of regulatory and financing policy mechanisms to influence the private sector, with the principal financing mechanism being purchasing/contracting. We summarise the literature on these two broad areas in turn.
Regulation
Regulation of the private health sector spans diverse legal frameworks, covering public health, professional standards, legal redress, oversight of facilities, pharmacies and private insurers, and broader economic regulations.42 43 48 55 56 Core components include licensing facilities and practitioners, setting quality and safety standards, and compliance monitoring.57,59 While most regulation focuses on quality and safety standards, occasionally it extends to geographical location, for example, requiring Certificates of Need for new facilities,50 or stipulating minimum distances between pharmacies.4 60 Other requirements may include mandatory reporting of data, ensuring access to emergency services and restricting advertising.38 61 62 Some countries regulate prices,2 22 54 57 58 with concern about profiteering during the COVID-19 pandemic leading to additional price caps in some countries.63 64 Voluntary or mandatory facility accreditation also forms a key component of the regulatory system in some settings.8 20 54 65 Registration of healthcare insurers generally focuses on financial soundness, though some countries also regulate enrolment, benefits and risk rating.22
There is considerable evidence of poor regulatory compliance across multiple LMICs and provider types. Studies, particularly from the earlier period of the review, highlighted high numbers of unlicensed providers in many settings,38 41 66 though some countries have made substantial progress in this area.52 61 Other widespread forms of non-compliance included poor adherence to minimum standards, clinicians or pharmacists operating more establishments than legally allowed, public sector staff also working in the private sector even where such dual practice was outlawed, provision of unnecessary services, and breaches in pharmacy practices, notably provision of prescription-only medicines without a prescription.20 22 27 48 50 56 60 67 68
There is limited rigorous evidence on interventions to enhance regulation.24 25 27 An exception was a randomised controlled trial (RCT) of facility regulation reforms in Kenya, which led to a substantial increase in inspection scores,68 at an annualised economic cost of US$311 per inspection.69 A Cochrane review also reported positive effects from RCTs of enhanced pharmacy regulation in Thailand, Vietnam and Laos but these were published in the early 2000s, before our review period.25 Turning to voluntary accreditation or certification, an RCT of private sector certification in Tanzania found a small increase in compliance with certification standards, but no improvement in clinical quality.70 A Cochrane review reported similar results from one 2003 South African study, again outside our review period.24 A review with less restrictive inclusion criteria found multiple studies showing positive effects of accreditation on quality, though a minority found no impact.20
The few papers addressing the effectiveness of health insurance regulation emphasised its importance for the development of equitable, efficient and high-quality health systems.71,74 In South Africa, 1990s deregulation was said to have led to ‘dramatic unintended consequences’ in terms of private sector growth, increased costs and exclusion of high-risk patients.22 73 In Thailand, progress towards UHC was argued to be facilitated by strict underwriting requirements that constrained insurance market development; in contrast, in Brazil, limited regulation, and tax breaks for insurers, empowered private actors, negatively affecting UHC progress,71 and leading to poor-quality and inefficient provision.75 Similar themes were raised in the literature on medical tourism, with concerns that regulatory neglect could distort health systems by attracting scarce personnel from the public sector, prioritising tertiary services and worsening inequalities.71 76 77
Multiple barriers to effective regulation were raised in the literature. First, the complex legal environment, compounded by rapidly changing health technologies, leads to gaps, overlaps and inconsistencies between laws.43 48 50 56 78 Duplicative mechanisms included requirements to register with multiple bodies,22 65 while gaps include the ‘informal’ sector, often ignored by regulators because it is considered illegal.56 79
Second, there is considerable evidence, particularly in lower income settings, that regulation is poorly implemented: there is limited follow-up post registration, with inspections rare or sporadic, and sanctions often not applied.2 4 22 41 48 50 54 56 57 66 68 78 80 81 Implementation is complicated by overlapping mandates of multiple bodies, inadequate incentives for inspectors, their imperfect access to information and under-resourcing.2 4 22 41 56 66 82 83
For regulation to be effective, private actors must be able to comply within their economic constraints.4 57 High licensing and accreditation fees can be a barrier to compliance.4 38 43 56 65 82 Moreover, some providers argue that requirements to locate in rural areas, adhere to price caps or refrain from selling prescription medicines are financially unviable,52 60 64 84 with regulators sometimes accepting that enforcing standards could reduce access for poor communities.4 The resulting divergence between regulations and common practice provides extensive opportunities for corruption.4 50 56 60 81 82 85
Several authors stress that regulation is inherently a political process, with vested interests influencing outcomes.22 57 86 Powerful stakeholders, such as the Indian Medical Association, have opposed legislation affecting their commercial interests53 54 66; in contrast, some relatively qualified providers campaign for tighter regulation to constrain the operation of their less qualified counterparts.22 53 60 Politicians or officials with investments in the private sector may also undermine regulations.54 80
Despite these challenges, several enablers have been identified to strengthen regulatory outcomes. These include getting buy-in across multiple regulatory agencies, ensuring regulation is perceived as fair and transparent, digitising processes, strengthening logistics, and supporting and incentivising providers to comply.22 41 60 65 85 There is also interest in the potential of ‘decentered regulation’, involving multiple bodies such as accreditation agencies, insurers and even online marketplaces, though this can be disjointed.54 57 Finally, successful regulation requires detailed stakeholder analysis, alliance building and political mechanisms to prevent undue influence by lobby groups.22 57
Contracting and purchasing
Governments’ use of public funds to purchase or contract services from private providers has been justified by the need to expand coverage quality, efficiency and responsiveness.4 In the past 20 years, the growth of social health insurance programmes in LMICs has led to a substantial increase in public purchasing agencies contracting both private and public facilities to provide services for enrolled members.87 Other common forms have included contracting networks of FBO facilities in Africa,88 NGOs to manage primary care in crisis-affected settings,4 38 89 private facilities to provide specialised services such as dialysis,4 52 ‘management contracts’ for private organisations to provide services within government facilities62 89 and a surge in contracts for testing and treatment during the COVID-19 pandemic.63 Longer term ‘Private Financing Initiative’ contracts have also been used to leverage private funds for health facility construction or refurbishment.449 90,92 Contracting provides potentially powerful governance opportunities to influence private provider behaviour, but historically payments have often been based on past expenditure or norms, with little consideration of performance or regulatory compliance.50 93 94 In recent decades, a strong emphasis has emerged on ‘strategic purchasing’, which includes selecting facilities meeting specified quality standards, using payment methods to incentivise efficiency and quality, and enhanced performance monitoring.2 48 50 87 93 95 96
Evidence on the effectiveness of contracting compared with government provision in LMICs is mixed. A 2018 Cochrane review included only two studies: a 2015 controlled before-after study in Guatemala of contracting mobile clinic services to NGOs which found no impact on utilisation or service delivery, and a 2006 RCT in Cambodia of contracting district health services to INGOs, from before our review period.30 A more recent difference-in-difference study found contracting primary care services to NGOs in Brazil increased utilisation and reduced hospitalisation for preventable disease (Greve and Coelho 2017, cited in ref 97). Reviews with less restrictive inclusion criteria have generally identified evidence that contracting improved utilisation, input availability and patient satisfaction, but lacked evidence on clinical quality.29 62 97 However, Rao et al report mixed evidence on utilisation, finding that private providers faced many of the same service delivery challenges as their public sector counterparts.89
The key question for many governments may be how best to contract, rather than whether to contract, given that gaps in public provision and political realities may make contracting inevitable.29 89 There is little quantitative evidence on the relative effectiveness of alternative contracting mechanisms (an exception is the literature on the effectiveness of pay for performance98 99 but this primarily concerns public facilities). However, substantive insights are available from qualitative data and expert opinion, with several recent papers synthesising this evidence across multiple LMICs.32 89 93 94 They find that a first step to effective contracting is contract design, which should include appropriate and balanced incentives for facility enrolment, quality of care, efficiency and equity, plus referral and gatekeeping guidelines, and mechanisms for redress, all transparently published online.32 87 93 Care should be taken to reduce perverse incentives for overprovision or underprovision, unnecessary admissions and referrals, selecting out high-risk cases, and additional patient charges.52 74 87 However, in practice, reimbursement tariffs below cost and late disbursements were an important constraint on provider performance,3264 89 93 100,103 distorting provider incentives, increasing user charges and negatively affecting public–private relationships.32 93 101 103 In some countries, donors played an important role in addressing funding gaps, though this also risked sustainability challenges and low government ownership.29 32 89 93
Contract governance was often hampered by challenges in monitoring performance and applying sanctions.29 78 89 90 In some cases, third-party monitoring by NGOs or accreditation agencies has been used to strengthen oversight,89 90 93 and investment in digitised and automated processes has also been recommended to enhance monitoring and transparency.32 104 105 However, authors note the value of ‘relational contracts’ in some contexts, where specific contract stipulations are subordinated to building a trusting partnership, examples being contracts with African FBO facilities, though this may risk weak accountability.88 89
Fragmentation among purchasers was argued to be a key barrier to effective contracting, with contracting by multiple social and private insurance programmes and other schemes creating uncoordinated provider incentives and increasing administrative costs.87 93 94 Greater purchaser consolidation, or failing that, coordination, has been recommended to strengthen incentives and accountability.93 High fragmentation on the provider side (ie, a very high number of small facilities) can also increase the costs and complexity of enrolling facilities and monitoring contracts,2 100 105 with suggestions that greater provider organisation or consolidation would be beneficial, perhaps through intermediaries such as NGOs, HMOs or provider associations.2 88 93 100 105 106
Finally, it is argued that effective governance of purchasing systems requires a strong ‘task network’ of organisations, with clearly delineated responsibilities across purchasers, social health insurers, accreditation bodies, regulators and MoH departments.94 However, in practice, capacity was limited (see the Capacities for governance section), agency roles were often unclear and delays in development of quality standards and information systems hampered purchaser performance.32 94 103 The way in which purchasing agencies themselves are governed was also argued to be important.32 93 Although there was debate over the optimal degree of autonomy the purchaser should have from the MoH, there was consensus that the purchaser be subject to a clear accountability framework, specifying the strategic goals, governing laws and regulations, financial controls and transparency requirements.32 However, in practice, concern was expressed about political interference and the influence of vested interests in purchasing mechanisms (see the Foster relations section).32 72 89
Foster relations
Foster relations covers the establishment of inclusive policy processes that involve a broad range of stakeholders including the private health sector.15
The literature covers a variety of approaches to including the private sector in policy processes. Some studies focus on donor-driven public–private dialogue platforms—often established to support the delivery of specific programmatic objectives.45 48 107 Others focus on policy processes related to specific reforms—for example, contracting arrangements,51 78 93 101 104 public–private partnerships for capital investments42 44 108 and regulatory change.50 55 81 In general, inclusion of the private sector in policy processes is considered to be a positive component of governance—generating benefits in terms of information exchange, trust building and balancing of interests.8 However, the literature also points to the threats posed by private sector influence activities in relation to governments’ policy goals,8 59 72 81 109 including in relation to equity of access and financial protection.59
It can be considered desirable for governments to engage with private sector associations, rather than individual private actors.41 However, the extent to which the insights, perspectives and interests of diverse stakeholders—and not only the most powerful—are represented by such entities can vary.54 81
A key message emphasised in parts of the literature is the importance of ensuring that policy processes are open, inclusive and transparent. Where public–private dialogue takes place ‘behind closed doors’, this is observed to create risks of state capture, bias and corruption.42 72 90 101 Non-transparent influence from powerful producer interests (eg, by the owners of investor-owned hospitals or private insurance companies) is observed to result in undue influence on policy making, to the potential detriment of UHC.59 To mitigate such risks, it has been argued that governments need to develop mechanisms for engaging with a broader range of stakeholders—including inter alia patients, social insurance recipients, civil society organisations (CSOs), etc, alongside private sector interests.54
Build understanding
Build understanding concerns the government’s access to and use of data on the private sector.15
The literature records multiple efforts by governments and other stakeholders (notably donors) to improve governments’ access to data, alongside some of the challenges faced in doing so. Studies from multiple countries document a range of regulations that oblige private providers to collect and share data with state authorities.41 45 56 81 104 For example, facility licensing criteria may include a requirement for the private sector to provide data.103 This can include data on matters of public health importance, including reportable diseases such as HIV, malaria and TB; and public health programmes such as family planning and immunisation.110 In relation to service delivery more generally, access to data may be lacking even in service domains in which the private sector accounts for a significant proportion of provision (such as maternity care in Uttar Pradesh, India).111 The literature indicates that where information sharing is voluntary rather than mandatory, compliance can be limited61 81 104 112—though there is some evidence that the situation is improving, in part due to technological developments in DHIS2 modules or other health management information system (although reporting into DHIS2 often remains paper based).8 Financial incentives can encourage reporting—for example, if information provision is necessary for reimbursement under state purchasing arrangements.59
Data collection challenges may be driven by a number of factors, including a lack of trained personnel, high staff turnover rates, the burden of paper-based reporting (which remains common in LMICs), and uncertainty and/or misunderstanding about the purpose or value of reporting.46 61 113 Studies also point to the lack of interoperability between data systems as a key challenge.114 However, Gautham et al suggest that, while private facilities sometimes feared information disclosure, they were willing to share data if asked officially, if the process was simple, and if they were assured of confidentiality.111
Align structures
Align structures focuses on government action to ensure alignment and coordination between the private and public sectors in service delivery.15 Approaches include engaging the private sector in quality of care initiatives, priority health programmes and referral networks. Use of and adherence to clinical and quality of care guidelines may be required for participation in national health insurance programmes,93 and licensing, as well as being incentivised through public training programmes, sometimes linked to programmes focusing on specific issues, such as combating antimicrobial resistance.115 Other examples include involvement in disease control,2 immunisation116 and family planning programmes,47 where private providers receive benefits such as training, equipment and supplies in exchange for compliance with notification and referral requirements, as well as meeting quality standards.117 There is also a growing literature on COVID-19 that looked at the contribution of the private sector during the pandemic, which is seen as one factor supporting effective responses in some settings.63 84
The literature provides limited evaluative evidence, especially on inclusion in referral networks. Private sector contributions to immunisation programmes vary, with mixed service quality reported in different countries.118 There is some evidence that private providers can fill gaps in service provision—for example, for immunisation in conflict-affected settings,116 and that they can offer advantages in reaching groups facing stigma, such as adolescents seeking reproductive care.47 However, quality criteria relating to general healthcare processes are noted to be commonly absent or not monitored, though some countries, such as South Africa, have introduced comprehensive quality criteria applicable to both public and private facilities.22 If there is no routine process of inspection or monitoring, the incentive to comply with evidence-based guidelines and referral regulations is limited.59 81
Enabling factors for ensuring effective alignment include mutual trust63; collaborative partnerships with clear roles and expectations; engagement of relevant professional and training bodies115; clear incentive structures favouring alignment for all actors; inclusion of the private sector in planning, supervision and reporting systems116; regular monitoring of quality metrics tied to provision of goods, such as vaccines118; and addressing barriers faced by private providers, including access to training and regulatory information.47 Alignment requires resourcing and leadership support,115 and deficits or delays in support and lack of recognition of the private sector’s contribution are demotivating.119
Nurture trust
Nurture trust requires governments to safeguard the rights and financial welfare of the public through mechanisms to strengthen the public voice in health system governance, address patient complaints and provide legal redress, with many of these mechanisms covering both public and private providers.15
These mechanisms may be underpinned by patients’ rights charters or laws,50 81 102 such as the Indian Charter of Patients’ Rights.54 Opportunities for patient voice may occur through annual general meetings of social health insurance agencies, hospital boards, public consultations, feedback surveys and review apps.2 62 71 93 95 Complaint mechanisms include telephone hotlines and online portals,57 94 120 or ombuds offices,2 81 102 and patients or their advocates may also sue providers.4 57 62
Examples of well-functioning voice and compliant mechanisms were rare, with those identified often ad hoc, ineffective, distrusted or having low public awareness or participation.50 56 75 94 102 121 However, there were some positive exceptions. Indonesia’s LAPOR! (REPORT!) platform had reportedly been widely used to voice citizens’ views and submit complaints about health services,65 and Thailand’s National Health Assembly was said to provide a mechanism for the public to constrain private sector influence on policy.71 Thailand was also said to have robust systems for involving patient interest groups on particular diseases, and a well-functioning telephone helpline for social health insurance members,94 though the literature lacked information on why these had worked well.
An underlying barrier to effective public accountability is that patients often lack good information about quality of care, and on their rights and accountability mechanisms, with poorer and more vulnerable consumers particularly disadvantaged.56 57 94 It is argued that efforts to address this could include display of patient rights at facilities, facility scorecards and development of online mechanisms.2 4 65 81 CSOs, NGOs and patient groups may also facilitate interaction, and in some cases have official monitoring roles.2 93 However, there is considerable variation in how well different communities are represented, and capture of such mechanisms by local elites is possible.57
In some contexts, such as India and Thailand, consumer litigation had become a prominent regulatory tool, though fear of being sued was argued to lead to increasingly precautionary and ‘defensive’ medical practices, pushing up costs.54 62 66 Legal redress also requires citizens to have sufficient resources to pursue claims, and accessible court services, but this is not always the case in practice.57 For example, India’s district-level consumer courts were expected to facilitate quick and local resolution, but in practice the process could be lengthy and costly, with perceptions of a bias in favour of clinicians.4 62 66 In the absence of effective redress mechanisms, some disgruntled users were sharing grievances through social or press media, and, worryingly, violent attacks on healthcare workers had become a concern in some settings.54 56
Capacities for governance
Across the governance behaviours, capacity to operationalise governance mechanisms was described as inadequate. In some areas, clear skills deficits were highlighted. For example, skills gaps for contracting included legal, clinical and financial risk management, claims data analysis, clinical coding and pricing, and performance monitoring and enforcement,8 38 39 41 42 48 51 62 75 81 94 101 102 104 122 while regulation and accreditation required skills in facility registration, inspection, and enforcement,41 50 81 95 102 123 and quality improvement/assurance.42 48 95 123 In addition to these technical skills, management and leadership skills were also noted as important enablers for governance, such as the ability to make good-quality decisions, innovate and manage change.32 59 However, challenges to skills development included high staff turnover, inadequate succession planning and loss of institutional memory.81 102
Inadequate capacity was also reported in the organisational processes and systems required for governance,8 41 42 48 51 102 104 122 meaning that, even where governance policies existed, most countries lacked capacity for implementation and enforcement.41 However, there was stronger capacity to govern the private sector within some vertical disease programmes, supported by external funding.2 8
Public actors reportedly faced particular challenges when operationalising governance in decentralised contexts. Local regulatory entities almost always reported insufficient human and financial resources for monitoring and enforcing regulation,2 42 51 66 77 81 101 102 122 and local actors were not involved in policy development, and sometimes did not clearly understand policy objectives.2 This may render local actors vulnerable to undue influence from local relationships, which are far more ‘present’, resulting in power imbalances during contracting and compliance (see Foster relations and Enable stakeholders sections).48 51 81 82 122 An evaluation of regulatory failures recommended the separation of the public health and regulatory functions at the local level, as they require distinct skill sets, and fundamentally different relationships with providers.66 90
Capacity constraints on the part of private providers also affect their ability to engage in governance mechanisms, particularly for small, individual or rural providers, who lack the resources for regulatory compliance.8 43 46 48 51 90 123 These providers report not receiving training on government reporting systems and processes, and lack the capacity to collect, maintain and share mandatory data with regulators.2 46 48 In some countries, donor-funded initiatives have worked with private providers to address these gaps.43 45 46 107 A lack of ‘collaborative capacity’ also emerged within and between the public and private sectors,29 42 66 81 101 with the observation that cultural, relational and institutional ‘software’ are crucial for legitimacy, feasibility and enforceability of governance mechanisms.85 Effective governance was reported as requiring trust, cooperation and collaboration capacity, both across the sectors and between agencies, networks, civil society and communities.23 65
Efforts to enhance governance capacity generally involved donor-supported technical assistance programmes providing human resources, operational processes, training, and stakeholder forums and engagement,43 45 46 107 sometimes including the establishment of specific public–private partnership units.8 43 44 46 48 108 124 While improvements in governance were reported, concerns were raised about sustaining this engagement at scale when external funding ceased,43 46 and the degree of public ownership in governance strategies that have had strong external input.4 22 57
Discussion and conclusion
This review synthesises the literature relevant to the governance of the private healthcare sector in LMICs, organised according to WHO’s six governance behaviours. The findings have informed the development of a ‘Progression Pathway for the Governance of Mixed Health Systems’, which aims to enable countries to assess their governance arrangements, prioritise future actions and track progress.109
A strength of the review was the inclusion of a wide range of literature in terms of study design, data collection methods and publication type, reflecting the valuable evidence that can be identified on this topic from not only rigorous research studies, but also from descriptions of policy and practice, and reflections of actors directly engaged in governance. Given this variability in methodological approach, we chose not to base inclusion on a formal quality assessment which could have led to exclusion of certain forms of valid evidence. We also took a broad approach to the definition of ‘governance’, guided by the WHO governance behaviours. The nature of the topic precluded a tightly targeted search strategy, with our initial searches identifying over 11 000 articles. We therefore used machine learning technology to order the screening of the papers, in practice screening about a fifth of the search results. It is possible that relevant articles were not screened before our stopping rule was reached. However, we supplemented database searches with articles identified by experts on the literature, leading to some degree of confidence that the most significant articles were included. The breadth of the governance topic also presented some challenges at the synthesis stage, particularly for the enable stakeholders literature on regulation and contracting, as these are two extremely broad areas of literature in themselves. To maintain feasibility, we drew where possible on existing literature reviews or evidence syntheses on these topics, while also including individual empirical papers to elaborate key issues.
The literature had considerable geographical breadth, covering a high number of LMICs, though with very little on fragile and conflict-affected settings. There was also breadth in terms of governance topic, though some neglected areas included private health insurance regulation, taxation, public accountability mechanisms and governance of recent market developments, such as digital health, medical tourism, hospital and pharmacy chains and private equity investors.57 125 126
The literature drew primarily on qualitative methods and document review, typically including interviews with high-level stakeholders on their perceptions, with few in-depth qualitative studies of the operation of governance mechanisms on the ground.54 85 127 Data on stakeholder perceptions may be subject to social desirability bias with, for example, government staff wanting to be seen as effective regulators, and private providers having strategic interests in arguing for less regulation. In a number of cases, government staff and their advisors were authors, which could be a further source of bias. However, this literature did include extensive coverage of perceived problems with governance approaches. There was limited detail on the intensity of implementation of governance mechanisms (eg, number of meetings, frequency of inspections, sanctions implemented, etc), and only one rigorous costing study.69 There was a particular lack of quantitative evidence on the impact on governance outcomes (no quantitative measures of governance were presented), provider behaviour or UHC indicators, with only a couple of exceptions.68 70 This may reflect the challenges of studying governance; it is difficult to measure, and legal changes or health system reforms cannot be easily piloted or withheld from control groups. In sum, care is needed in interpreting the literature to identify credible evidence of ‘what works well’, as opposed to the claims of those involved in implementation or the many opinions on offer of what could be improved. Given the patchy nature and varied quality of the evidence base, identifying firm conclusions about patterns of findings across geographical regions or income levels is challenging. Future research should include more in-depth qualitative explorations of governance mechanisms and more rigorous documentation of context, implementation and outcomes.
A number of important lessons emerged from the review. First, effective performance of each governance behaviour requires a clear vision for the private sector’s role in the delivery of health system goals, together with specific mechanisms to enable this. Second, synergies can be exploited between governance mechanisms, such as linking contracting with regulatory compliance, or including data submission as a licensing requirement. Inadequate capacity, at the individual and organisation levels, was one of the most prominent themes, reflecting a persistent failure to see private sector governance as core to the government’s role. The skills required are well documented, but greater evidence is needed on how these can be developed, especially in devolved contexts and without donor support. Greater emphasis is also needed on developing strong (and ideally independent) institutions for regulation, purchasing and quality assurance. Another clear lesson is the importance of inclusive and transparent policy processes. Public–private dialogue ‘behind closed doors’ creates risks of state capture, bias and corruption. To balance legitimate stakeholder interests, the focus should be on purposeful deliberation in multistakeholder platforms, including patients, social insurance recipients and CSOs. The public sector also needs to be held accountable in its governance actions, including adherence to contract terms, transparency in tender and regulatory practices, and control of favouritism and other corrupt practices, an area which merits much greater innovation.128 129 A final lesson is that governance choices shape not just current private sector behaviour, but also the future development of the health system. Once a large and powerful constituency of private facilities or health insurers has developed, it can be particularly challenging to make progress towards UHC. Conversely, sustained effective governance has the potential to shape market development in line with health system goals, with the literature highlighting the many priority areas where further action is required to achieve this outcome.
supplementary material
Acknowledgements
The authors acknowledge librarians Bohee Lee, University of Edinburgh, and Kate Perris, LSHTM, for their support in designing the search strategy. We also extend our gratitude to Agrima Sahore and Munmun Biswas for their support in the search process.
Footnotes
Funding: This review was funded by the World Health Organization.
Provenance and peer review: Not commissioned; externally peer reviewed.
Handling editor: Lei Si
Patient consent for publication: Not applicable.
Ethics approval: Not applicable.
Data availability free text: Additional details will be available in the full review report and appendices prepared for the World Health Organization.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Contributor Information
Catherine Goodman, Email: catherine.goodman@lshtm.ac.uk.
Sophie Witter, Email: switter@qmu.ac.uk.
Mark Hellowell, Email: mark.hellowell@ed.ac.uk.
Louise Allen, Email: louise.allen@opml.co.uk.
Shuchi Srinivasan, Email: shuchi.srinivasan@opml.co.uk.
Swapna Nixon, Email: swapna.nixon@opml.co.uk.
Ayesha Burney, Email: ayesha.burney@opml.co.uk.
Debrupa Bhattacharjee, Email: debrupa1901@gmail.com.
Anna Cocozza, Email: anna.cocozza8@gmail.com.
Gabrielle Appleford, Email: gabrielle.aline@gmail.com.
Aya Thabet, Email: thabetay@who.int.
David Clarke, Email: Clarked@who.int.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1.Mackintosh M, Channon A, Karan A, et al. What is the private sector? Understanding private provision in the health systems of low-income and middle-income countries. Lancet. 2016;388:596–605. doi: 10.1016/S0140-6736(16)00342-1. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization . Private Sector Landscape in Mixed Health Systems. Geneva: World Health Organization; 2020. [Google Scholar]
- 3.World Health Organization . Geneva:: World Health Organization; 2023. The private sector in health service delivery: an operational definition.https://www.ccpsh.org/research/private-sector-health-service-delivery-operational-definition Available. [Google Scholar]
- 4.Montagu D, Goodman C. Prohibit, constrain, encourage, or purchase: how should we engage with the private health-care sector? Lancet. 2016;388:613–21. doi: 10.1016/S0140-6736(16)30242-2. [DOI] [PubMed] [Google Scholar]
- 5.Coveney L, Musoke D, Russo G. Do private health providers help achieve Universal Health Coverage? A scoping review of the evidence from low-income countries. Health Policy Plan. 2023;38:1050–63. doi: 10.1093/heapol/czad075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bradley SEK, Rosapep L, Shiras T. Where Do Caregivers Take Their Sick Children for Care? An Analysis of Care Seeking and Equity in 24 USAID Priority Countries. Glob Health Sci Pract. 2020;8:518–33. doi: 10.9745/GHSP-D-20-00115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Campbell OMR, Benova L, MacLeod D, et al. Family planning, antenatal and delivery care: cross‐sectional survey evidence on levels of coverage and inequalities by public and private sector in 57 low‐ and middle‐income countries. Tropical Med Int Health . 2016;21:486–503. doi: 10.1111/tmi.12681. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization . Geneva: World Health Organization; 2022. [13-Dec-2023]. Towards better engagement of the private sector in health service delivery.https://www.who.int/publications-detail-redirect/9789240047273 Available. accessed. [Google Scholar]
- 9.Clarke D, Doerr S, Hunter M, et al. The private sector and universal health coverage. Bull World Health Organ. 2019;97:434–5. doi: 10.2471/BLT.18.225540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barbazza E, Tello JE. A review of health governance: definitions, dimensions and tools to govern. Health Policy. 2014;116:1–11. doi: 10.1016/j.healthpol.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization . Geneva: World Health Organization; 2007. Everybody’s business -- strengthening health systems to improve health outcomes: WHO’s framework for action; p. 44.https://www.who.int/publications/i/item/everybody-s-business----strengthening-health-systems-to-improve-health-outcomes Available. [Google Scholar]
- 12.World Health Assembly Strengthening the capacity of governments to constructively engage the private sector in providing essential health-care services. [06-Jan-2023];2010 :63. https://apps.who.int/iris/handle/10665/3101 Available. accessed.
- 13.World Health Organization . Geneva: World Health Organization; 2020. Engaging the private health service delivery sector through governance in mixed health systems: strategy report of the who advisory group on the governance of the private sector for universal health coverage.https://www.who.int/publications/i/item/9789240018327 Available. [Google Scholar]
- 14.Travis P, Egger D, Davies P, et al. Geneva:: World Health Organization; 2002. Towards better stewardship: concepts and critical issues.https://iris.who.int/handle/10665/339291 Available. [Google Scholar]
- 15.Clarke D, Appleford G, Cocozza A, et al. The governance behaviours: a proposed approach for the alignment of the public and private sectors for better health outcomes. BMJ Glob Health. 2023;8:e012528. doi: 10.1136/bmjgh-2023-012528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Naher N, Hoque R, Hassan MS, et al. The influence of corruption and governance in the delivery of frontline health care services in the public sector: a scoping review of current and future prospects in low and middle-income countries of south and south-east Asia. BMC Public Health. 2020;20:880. doi: 10.1186/s12889-020-08975-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lokot M, Bou-Orm I, Zreik T, et al. Health system governance in settings with conflict-affected populations: a systematic review. Health Policy Plan. 2022;37:655–74. doi: 10.1093/heapol/czac027. [DOI] [PubMed] [Google Scholar]
- 18.George J, Jack S, Gauld R, et al. Impact of health system governance on healthcare quality in low-income and middle-income countries: a scoping review. BMJ Open. 2023;13:e073669. doi: 10.1136/bmjopen-2023-073669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ayanore MA, Amuna N, Aviisah M, et al. Towards Resilient Health Systems in Sub-Saharan Africa: A Systematic Review of the English Language Literature on Health Workforce, Surveillance, and Health Governance Issues for Health Systems Strengthening. Ann Glob Health. 2019;85:113. doi: 10.5334/aogh.2514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Montagu D, Goodman C, Berman P, et al. Recent trends in working with the private sector to improve basic healthcare: a review of evidence and interventions. Health Policy Plan. 2016;31:1117–32. doi: 10.1093/heapol/czw018. [DOI] [PubMed] [Google Scholar]
- 21.Whyle EB, Olivier J. Models of public-private engagement for health services delivery and financing in Southern Africa: a systematic review. Health Policy Plan. 2016;31:1515–29. doi: 10.1093/heapol/czw075. [DOI] [PubMed] [Google Scholar]
- 22.Doherty JE. Regulating the for-profit private health sector: lessons from East and Southern Africa. Health Policy Plan. 2015;30 Suppl 1:i93–102. doi: 10.1093/heapol/czu111. [DOI] [PubMed] [Google Scholar]
- 23.Ensor T, Weinzierl S. Regulating health care in low- and middle-income countries: Broadening the policy response in resource constrained environments. Soc Sci Med. 2007;65:355–66. doi: 10.1016/j.socscimed.2007.03.021. [DOI] [PubMed] [Google Scholar]
- 24.Flodgren G, Gonçalves-Bradley DC, Pomey MP. External inspection of compliance with standards for improved healthcare outcomes. Cochrane Database Syst Rev. 2016;12:CD008992. doi: 10.1002/14651858.CD008992.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wiysonge CS, Abdullahi LH, Ndze VN, et al. Public stewardship of private for-profit healthcare providers in low- and middle-income countries. Cochrane Database Syst Rev. 2016;2016:CD009855. doi: 10.1002/14651858.CD009855.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Greenfield D, Pawsey M, Hinchcliff R, et al. The standard of healthcare accreditation standards: a review of empirical research underpinning their development and impact. BMC Health Serv Res. 2012;12:329. doi: 10.1186/1472-6963-12-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miller R, Goodman C. Performance of retail pharmacies in low- and middle-income Asian settings: a systematic review. Health Policy Plan. 2016;31:940–53.:czw007. doi: 10.1093/heapol/czw007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wafula FN, Goodman CA. Are interventions for improving the quality of services provided by specialized drug shops effective in sub-Saharan Africa? A systematic review of the literature. Int J Qual Health Care. 2010;22:316–23. doi: 10.1093/intqhc/mzq022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nachtnebel M, O’Mahony A, Pillai N, et al. Effectively engaging the private sector through vouchers and contracting - A case for analysing health governance and context. Soc Sci Med. 2015;145:193–200. doi: 10.1016/j.socscimed.2015.05.021. [DOI] [PubMed] [Google Scholar]
- 30.Odendaal WA, Ward K, Uneke J, et al. Contracting out to improve the use of clinical health services and health outcomes in low- and middle-income countries. Cochrane Database Syst Rev. 2018;4:CD008133. doi: 10.1002/14651858.CD008133.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sanderson J, Lonsdale C, Mannion R. What’s Needed to Develop Strategic Purchasing in Healthcare? Policy Lessons from a Realist Review. Int J Health Policy Manag. 2018;8:4–17. doi: 10.15171/ijhpm.2018.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.World Health Organization, Regional Office for Europe . Copenhagen: 2023. [13-Dec-2023]. Reimagining governance for strategic purchasing: evidence from 10 countries in eastern Europe and central Asia.https://www.who.int/europe/publications/i/item/9789289060127 Available. accessed. [Google Scholar]
- 33.Munn Z, Peters MDJ, Stern C, et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:143. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tricco AC, Lillie E, Zarin W, et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Methodol. 2016;16:15. doi: 10.1186/s12874-016-0116-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Boetje J, de Schoot R van. The safe procedure: a practical stopping heuristic for active learning-based screening in systematic reviews and meta-analyses. In Review. 2023 doi: 10.21203/rs.3.rs-2856011/v1. https://www.researchsquare.com/article/rs-2856011/v1 Preprint. Available. [DOI] [PMC free article] [PubMed]
- 36.van de Schoot R, de Bruin J, Schram R, et al. An open source machine learning framework for efficient and transparent systematic reviews. Nat Mach Intell. 2021;3:125–33. doi: 10.1038/s42256-020-00287-7. [DOI] [Google Scholar]
- 37.Ros R, Bjarnason E, Runeson P. A machine learning approach for semi-automated search and selection in literature studies. Proceedings of the 21st International Conference on Evaluation and Assessment in Software Engineering; New York, NY, USA: Association for Computing Machinery. 2017. pp. 118–27. [DOI] [Google Scholar]
- 38.Lagomarsino G, Nachuk S, Kundra SS. Results for Development Institute. Available from. Washington, DC: 2009. Public stewardship of private providers in mixed health systems.https://staging.r4d.org/wp-content/uploads/Public-Stewardship-of-Private-Providers-in-Mixed-Health-Systems.pdf Available. [Google Scholar]
- 39.Harding A, Preker AS, editors. Private Participation in Health Services. (Health, Nutrition, and Population Series) World Bank; 2003. p. 349. [Google Scholar]
- 40.Balabanova D, Oliveira-Cruz V, Hanson K. Health sector governance and implications for the private sector. R4D. 2009. https://r4d.org/resources/health-sector-governance-implications-private-sector/ Available.
- 41.World Bank, International Finance Corporation . Washington, DC: World Bank; 2011. [12-Jan-2023]. Healthy partnerships: how governments can engage the private sector to improve health in Africa.https://openknowledge.worldbank.org/handle/10986/2304 Available. accessed. [Google Scholar]
- 42.Nuhu S, Mpambije CJ, Ngussa K. Challenges in health service delivery under public-private partnership in Tanzania: stakeholders’ views from Dar es Salaam region. BMC Health Serv Res. 2020;20:765. doi: 10.1186/s12913-020-05638-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cross HE, Sayedi O, Irani L, et al. Government stewardship of the for-profit private health sector in Afghanistan. Health Policy Plan. 2017;32:338–48. doi: 10.1093/heapol/czw130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dugle G, Kpinpuo SD, Ghartey BB. From paper to practice: an exploratory study of policy making and implementation in alternative forms of healthcare public-private partnership in Ghana. Int J Health Plann Manage. 2021;36:866–84. doi: 10.1002/hpm.3123. [DOI] [PubMed] [Google Scholar]
- 45.Cisek CR, Klein K, Koseki S, et al. Strengthening family planning stewardship with a total market approach: Mali, Uganda, and Kenya experiences. Pub Admin Dev. 2019;39:47–56. doi: 10.1002/pad.1840. [DOI] [Google Scholar]
- 46.Ali D, Woldegiorgis AG-Y, Tilaye M, et al. Integrating private health facilities in government-led health systems: a case study of the public-private mix approach in Ethiopia. BMC Health Serv Res. 2022;22:1477. doi: 10.1186/s12913-022-08769-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Azzopardi PS, Hennegan J, Prabhu SM, et al. Key recommendations to strengthen public-private partnership for adolescent health in resource constrained settings: Formative qualitative inquiry in Mongolia, Myanmar and the Philippines. Lancet Reg Health West Pac . 2021;15:100242. doi: 10.1016/j.lanwpc.2021.100242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Iqbal M, Feroz AS, Siddeeg K, et al. Engagement of private healthcare sector in reproductive, maternal, newborn, child and adolescent health in selected Eastern Mediterranean countries. East Mediterr Health J . 2022;28:638–48. doi: 10.26719/emhj.22.057. [DOI] [PubMed] [Google Scholar]
- 49.Kula N, Fryatt RJ. Public-private interactions on health in South Africa: opportunities for scaling up. Health Policy Plan. 2014;29:560–9. doi: 10.1093/heapol/czt042. [DOI] [PubMed] [Google Scholar]
- 50.Tsevelvaanchig U, Narula IS, Gouda H, et al. Regulating the for-profit private healthcare providers towards universal health coverage: A qualitative study of legal and organizational framework in Mongolia. Int J Health Plann Manage. 2018;33:185–201. doi: 10.1002/hpm.2417. [DOI] [PubMed] [Google Scholar]
- 51.Zaidi S, Mayhew SH, Cleland J, et al. Context matters in NGO-government contracting for health service delivery: a case study from Pakistan. Health Policy Plan. 2012;27:570–81. doi: 10.1093/heapol/czr081. [DOI] [PubMed] [Google Scholar]
- 52.Tsevelvaanchig U, Gouda H, Baker P, et al. Role of emerging private hospitals in a post-Soviet mixed health system: a mixed methods comparative study of private and public hospital inpatient care in Mongolia. Health Policy Plan. 2017;32:476–86. doi: 10.1093/heapol/czw157. [DOI] [PubMed] [Google Scholar]
- 53.De Costa A, Johannson E. By “default or design”? The expansion of the private health care sector in Madhya Pradesh, India. Health Policy. 2011;103:283–9. doi: 10.1016/j.healthpol.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 54.Hunter BM, Murray SF, Marathe S, et al. Decentred regulation: The case of private healthcare in India. World Dev. 2022;155:105889. doi: 10.1016/j.worlddev.2022.105889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lee KH, Ariffin RNR, Abdullah NRW. The implications of legislative controls on private hospitals in Malaysia. Inst Econ. 2018;10:62–94. [Google Scholar]
- 56.World Health Organization Assessing the regulation of the private health sector in the Eastern Mediterranean region: Yemen. World Health Organization. Regional Office for the Eastern Mediterranean. 2014. https://iris.who.int/handle/10665/250542 Available.
- 57.Bloom G, Henson S, Peters DH. Innovation in regulation of rapidly changing health markets. Global Health . 2014;10:53. doi: 10.1186/1744-8603-10-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Riley P, Callahan S, Dalious M. Regulation of drug shops and pharmacies relevant to family planning: a scan of 32 developing countries. SHOPS Plus (Abt Associates) 2017. https://shopsplusproject.org/sites/default/files/resources/Regulation%20of%20Drug%20Shops%20and%20Pharmacies%20Relevant%20to%20Family%20Planning%20-%20A%20Scan%20of%2032%20Developing%20Countries_0.pdf Available.
- 59.World Health Organization . Copenhagen: World Health Organization. Regional Office for Europe; 2023. [13-Dec-2023]. Private provision of services in Ukraine: current challenges, future directions. Health policy papers series.https://www.who.int/europe/publications/i/item/WHO-EURO-2023-7625-47392-69619 Available. accessed. [Google Scholar]
- 60.Hutchinson E, Mundua S, Ochero L, et al. Life in the buffer zone: Social relations and surplus health workers in Uganda’s medicines retail sector. Soc Sci Med. 2022;300:113941. doi: 10.1016/j.socscimed.2021.113941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Appleford G, Mumbia D, Emmart P. Incentives and disincentives to private sector reporting on family planning in Kenya: why these matter, and how they may change over time. 2023. https://gatesopenresearch.org/articles/6-124 Available. [DOI] [PMC free article] [PubMed]
- 62.Zaidi S, Riaz A, Thaver A, et al. World Health Organ Reg Off East Mediterr; 2016. Role and contribution of private sector in moving towards universal health coverage in the Eastern Mediterranean region. [Google Scholar]
- 63.Gadsden T, Ford B, Angell B, et al. Health financing policy responses to the COVID-19 pandemic: a review of the first stages in the WHO South-East Asia Region. Health Policy Plan. 2022;37:1317–27. doi: 10.1093/heapol/czac071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Williams OD, Yung KC, Grépin KA. The failure of private health services: COVID-19 induced crises in low- and middle-income country (LMIC) health systems. Glob Public Health. 2021;16:1320–33. doi: 10.1080/17441692.2021.1874470. [DOI] [PubMed] [Google Scholar]
- 65.Joint Learning Network Regulation of private primary health care: a country assessment guide. 2018. [13-Dec-2023]. https://jointlearningnetwork.org/resources/regulation-of-private-primary-health-care-a-country-assessment-guide/ Available. Accessed.
- 66.Sheikh K, Saligram PS, Hort K. What explains regulatory failure? Analysing the architecture of health care regulation in two Indian states. Health Policy Plan. 2015;30:39–55. doi: 10.1093/heapol/czt095. [DOI] [PubMed] [Google Scholar]
- 67.McPake B, Russo G, Hipgrave D, et al. Implications of dual practice for universal health coverage. Bull World Health Organ. 2016;94:142–6. doi: 10.2471/BLT.14.151894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bedoya G, Das J, Dolinger A. Randomized regulation: the impact of minimum quality standards on health markets. 2023. [19-Jul-2023]. https://openknowledge.worldbank.org/handle/10986/39630 Available. Accessed.
- 69.Chege T, Wafula F, Tama E, et al. How much does effective health facility inspection cost? An analysis of the economic costs of Kenya’s Joint Health Inspection innovations. BMC Health Serv Res. 2022;22:1351. doi: 10.1186/s12913-022-08727-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.King JJC, Powell-Jackson T, Makungu C, et al. Effect of a multifaceted intervention to improve clinical quality of care through stepwise certification (SafeCare) in health-care facilities in Tanzania: a cluster-randomised controlled trial. Lancet Glob Health. 2021;9:e1262–72. doi: 10.1016/S2214-109X(21)00228-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Harris J, Libardi Maia J. Universal healthcare does not look the same everywhere: Divergent experiences with the private sector in Brazil and Thailand. Glob Public Health. 2022;17:1809–26. doi: 10.1080/17441692.2021.1981973. [DOI] [PubMed] [Google Scholar]
- 72.Onoka CA, Hanson K, Hanefeld J. Towards universal coverage: a policy analysis of the development of the National Health Insurance Scheme in Nigeria. Health Policy Plan. 2015;30:1105–17. doi: 10.1093/heapol/czu116. [DOI] [PubMed] [Google Scholar]
- 73.van den Heever AM. The role of insurance in the achievement of universal coverage within a developing country context: South Africa as a case study. BMC Public Health. 2012;12 Suppl 1:S5. doi: 10.1186/1471-2458-12-S1-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Vargas I, Vázquez ML, Mogollón-Pérez AS, et al. Barriers of access to care in a managed competition model: lessons from Colombia. BMC Health Serv Res. 2010;10:297. doi: 10.1186/1472-6963-10-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lobato L de VC, Ribeiro JM, Vaitsman J. Public/Private Mix in the Brazilian Health System and the Quest for Equity. Glob Soc Welf. 2016;3:213–21. doi: 10.1007/s40609-016-0069-x. [DOI] [Google Scholar]
- 76.Cerón A, Crooks VA, Labonté R, et al. Medical Tourism in Guatemala: Qualitatively Exploring How Existing Health System Inequities Facilitate Sector Development. Int J Health Serv . 2019;49:754–72. doi: 10.1177/0020731419866085. [DOI] [PubMed] [Google Scholar]
- 77.Labonté R, Crooks VA, Valdés AC, et al. Government roles in regulating medical tourism: evidence from Guatemala. Int J Equity Health. 2018;17:150. doi: 10.1186/s12939-018-0866-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Khetrapal S, Acharya A, Mills A. Assessment of the public-private-partnerships model of a national health insurance scheme in India. Soc Sci Med. 2019;243:112634. doi: 10.1016/j.socscimed.2019.112634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.World Health Organization Assessing the regulation of the private health sector in the Eastern Mediterranean region: Egypt. World Health Organization. Regional Office for the Eastern Mediterranean. 2014. [11-Dec-2023]. https://iris.who.int/handle/10665/250541 Available. Accessed.
- 80.Khan M, Rahman-Shepherd A, Bory S, et al. How conflicts of interest hinder effective regulation of healthcare: an analysis of antimicrobial use regulation in Cambodia, Indonesia and Pakistan. BMJ Glob Health. 2022;7:e008596. doi: 10.1136/bmjgh-2022-008596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Putturaj M, Bhojani U, Rao NV, et al. Decoding the black box of health policy implementation: A case of regulating private healthcare establishments in southern India. Natl Med J India. 2021;34:100–6. doi: 10.4103/0970-258X.326754. [DOI] [PubMed] [Google Scholar]
- 82.Bork T, Kraas F, Yuan Y. Governance challenges in China’s urban health care system – the role of stakeholders. ERDKUNDE. 2011;65:121–35. doi: 10.3112/erdkunde.2011.02.02. [DOI] [Google Scholar]
- 83.Van Belle S, Mayhew SH. Public accountability needs to be enforced -a case study of the governance arrangements and accountability practices in a rural health district in Ghana. BMC Health Serv Res. 2016;16:568. doi: 10.1186/s12913-016-1836-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.World Health Organization . Geneva:: World Health Organization; 2022. Equitable access to covid-19 tools: aligning the private sector with national response efforts.https://www.who.int/publications-detail-redirect/9789240046481 Available. [Google Scholar]
- 85.Tama E, Khayoni I, Goodman C, et al. What Lies Behind Successful Regulation? A Qualitative Evaluation of Pilot Implementation of Kenya’s Health Facility Inspection Reforms. Int J Health Policy Manag. 2022;11:1852–62. doi: 10.34172/ijhpm.2021.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Machado CV, Silva GA e. Political struggles for a universal health system in Brazil: successes and limits in the reduction of inequalities. Global Health . 2019;15 doi: 10.1186/s12992-019-0523-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Honda A, Obse A. Payment Arrangements for Private Healthcare Purchasing Under Publicly Funded Systems in Low- and Middle-Income Countries: Issues and Implications. Appl Health Econ Health Policy. 2020;18:811–23. doi: 10.1007/s40258-019-00550-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Whyle E, Olivier J. Models of engagement between the state and the faith sector in sub-Saharan Africa – a systematic review. Dev Pract. 2017;27:684–97. doi: 10.1080/09614524.2017.1327030. [DOI] [Google Scholar]
- 89.Rao KD, Paina L, Ingabire MG, et al. Contracting non-state providers for universal health coverage: learnings from Africa, Asia, and Eastern Europe. Int J Equity Health. 2018;17:127. doi: 10.1186/s12939-018-0846-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hellowell M. Are public-private partnerships the future of healthcare delivery in sub-Saharan Africa? Lessons from Lesotho. BMJ Glob Health. 2019;4:e001217. doi: 10.1136/bmjgh-2018-001217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Cortez R, Quinlan-Davidson M. Washington, DC:: World Bank; 2022. Private sector engagement in public health systems.https://hdl.handle.net/10986/38231 Available. [Google Scholar]
- 92.Independent Evaluation Group . Washington, DC: World Bank; 2016. Public-private partnerships in health: World Bank group engagement in health PPPs.https://openknowledge.worldbank.org/handle/10986/25383 Available. [Google Scholar]
- 93.Gatome-Munyua A, Sieleunou I, Barasa E, et al. Applying the Strategic Health Purchasing Progress Tracking Framework: Lessons from Nine African Countries. Health Syst Reform . 2022;8:e2051796. doi: 10.1080/23288604.2022.2051796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hanson K, Barasa E, Honda A, et al. Strategic Purchasing: The Neglected Health Financing Function for Pursuing Universal Health Coverage in Low- and Middle-Income Countries. Int J Health Policy Manag. 2019;8:501–4. doi: 10.15171/ijhpm.2019.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Mbachu C, Okeke C, Obayi C, et al. Supporting strategic health purchasing: a case study of annual health budgets from general tax revenue and social health insurance in Abia state, Nigeria. Health Econ Rev. 2021;11:47. doi: 10.1186/s13561-021-00346-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.McPake B, Hanson K. Managing the public-private mix to achieve universal health coverage. Lancet. 2016;388:622–30. doi: 10.1016/S0140-6736(16)00344-5. [DOI] [PubMed] [Google Scholar]
- 97.Thomas C, Lanzas C, Tolmei C, et al. Washington, D.C:: R4D; 2021. [12-Dec-2023]. Strengthening mixed health systems evidence review.https://r4d.org/resources/strengthening-mixed-health-systems-evidence-review/ Available. accessed. [Google Scholar]
- 98.de Walque D, Kandpal E, Wagstaff A. Improving effective coverage in health: do financial incentives work? The World Bank. 2022. [15-Dec-2023]. https://hdl.handle.net/10986/37326 Available. Accessed.
- 99.Diaconu K, Falconer J, Verbel A, et al. Paying for performance to improve the delivery of health interventions in low- and middle-income countries. Cochrane Database Syst Rev. 2021;5:CD007899. doi: 10.1002/14651858.CD007899.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Boddam-Whetham L. Leveraging private health providers to achieve universal health coverage lessons from the African health markets for equity project. 2019. https://ccpsh.org/content/intro-clearing-house Available.
- 101.Maluka S, Chitama D, Dungumaro E, et al. Contracting-out primary health care services in Tanzania towards UHC: how policy processes and context influence policy design and implementation. Int J Equity Health. 2018;17:118. doi: 10.1186/s12939-018-0835-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Masefield SC, Msosa A, Grugel J. Challenges to effective governance in a low income healthcare system: a qualitative study of stakeholder perceptions in Malawi. BMC Health Serv Res. 2020;20:1142. doi: 10.1186/s12913-020-06002-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Chirwa ML, Kazanga I, Faedo G, et al. Promoting universal financial protection: contracting faith-based health facilities to expand access--lessons learned from Malawi. Health Res Policy Syst. 2013;11:27. doi: 10.1186/1478-4505-11-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Khalife J, Rafeh N, Makouk J, et al. Hospital Contracting Reforms: The Lebanese Ministry of Public Health Experience. Health Syst Reform . 2017;3:34–41. doi: 10.1080/23288604.2016.1272979. [DOI] [PubMed] [Google Scholar]
- 105.Suchman L, Owino E, Montagu D. Recognizing and mediating bureaucratic barriers: increasing access to care through small and medium-sized private providers in Kenya. Gates Open Res . 2021;5:95. doi: 10.12688/gatesopenres.13313.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Aiyenigba E, Arias J, Bolender T, et al. Intermediaries: the missing link in improving mixed market health systems? results for development (r4d) and the center for health market innovations (chmi) 2016. [13-Dec-2023]. https://r4d.org/resources/intermediaries-missing-link-improving-mixed-market-health-systems/ Available. Accessed.
- 107.Tolmie C, Lanzara C, Thomas C, et al. Supporting public-private engagement in Kakamega county (Kenya) case study. Results for Development. 2021. [21-Jul-2023]. https://r4d.org/resources/supporting-public-private-engagement-in-kakamega-county-kenya-case-study/ Available. Accessed.
- 108.Kamugumya D, Olivier J. Health system’s barriers hindering implementation of public-private partnership at the district level: a case study of partnership for improved reproductive and child health services provision in Tanzania. BMC Health Serv Res. 2016;16:596. doi: 10.1186/s12913-016-1831-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.World Health Organisation Advancing country’s capacity to govern the private sector in health. 2023. [15-Dec-2023]. https://ccpsh.org/research/advancing-countrys-capacity-govern-private-sector-health Available. Accessed.
- 110.Bhattacharyya S, Berhanu D, Taddesse N, et al. District decision-making for health in low-income settings: a case study of the potential of public and private sector data in India and Ethiopia. Health Policy Plan. 2016;31 Suppl 2:ii25–34. doi: 10.1093/heapol/czw017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Gautham M, Spicer N, Subharwal M, et al. District decision-making for health in low-income settings: a qualitative study in Uttar Pradesh, India, on engaging the private health sector in sharing health-related data. Health Policy Plan. 2016;31 Suppl 2:ii35–46. doi: 10.1093/heapol/czv117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Avan BI, Berhanu D, Umar N, et al. District decision-making for health in low-income settings: a feasibility study of a data-informed platform for health in India, Nigeria and Ethiopia. Health Policy Plan . 2016;31:ii3–11. doi: 10.1093/heapol/czw082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Mangone E, Romorini S. Private sector engagement in national health management information systems: barriers, strategies, and global case studies. SHOPS Plus (Abt Associates) 2021. https://www.marketlinks.org/resources/private-sector-engagement-national-health-management-information-systems-barriers Available.
- 114.Wu J, Qiao J, Nicholas S, et al. The challenge of healthcare big data to China’s commercial health insurance industry: evaluation and recommendations. BMC Health Serv Res. 2022;22 doi: 10.1186/s12913-022-08574-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Singh S, Charani E, Devi S, et al. A road-map for addressing antimicrobial resistance in low- and middle-income countries: lessons learnt from the public private participation and co-designed antimicrobial stewardship programme in the State of Kerala, India. Antimicrob Resist Infect Control. 2021;10 doi: 10.1186/s13756-020-00873-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Ahmed N, DeRoeck D, Sadr-Azodi N. Private sector engagement and contributions to immunisation service delivery and coverage in Sudan. BMJ Glob Health. 2019;4:e001414. doi: 10.1136/bmjgh-2019-001414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.World Health Organization . Copenhagen: WHO Regional Office for Europe; 2022. Monitoring the implementation of digital health: an overview of selected national and international methodologies.https://www.who.int/europe/publications/i/item/WHO-EURO-2022-5985-45750-65816 Available. [Google Scholar]
- 118.Levin A, Munthali S, Vodungbo V, et al. Scope and magnitude of private sector financing and provision of immunization in Benin, Malawi and Georgia. Vaccine (Auckl) 2019;37:3568–75. doi: 10.1016/j.vaccine.2019.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Salve S, Harris K, Sheikh K, et al. Understanding the complex relationships among actors involved in the implementation of public-private mix (PPM) for TB control in India, using social theory. Int J Equity Health. 2018;17:73. doi: 10.1186/s12939-018-0785-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Campos IA. Berlin, Heidelberg:: Springer; 2013. Health-care system regulation in Brazil and in Great Britain; pp. 223–43. Available. [DOI] [Google Scholar]
- 121.Patullo MPF, Aith FMA. Unequal participation of consumers and private health plans in the Brazilian Regulatory Agency for Private Health Insurance and Plans. Rev Direito Sanit. 2022;22:e0006. doi: 10.11606/issn.2316-9044.rdisan.2022.187345. [DOI] [Google Scholar]
- 122.Silva J, Carvalho BG, Domingos CM. Health governance and the public-private in small municipalities. Ciênc Saúde Colet. 2018;23:3179–88. doi: 10.1590/1413-812320182310.13952018. [DOI] [PubMed] [Google Scholar]
- 123.Spieker N. In: Improving Health Care in Low- and Middle-Income Countries: A Case Book. Marquez LR, editor. Cham: Springer International Publishing; 2020. The business case for quality in health care; pp. 89–104. [Google Scholar]
- 124.Arur A, Sulzbach S, Barnes J, et al. Strengthening health systems by engaging the private health sector: promising hiv/aids partnerships. SHOPS Plus. 2011. [11-Dec-2023]. https://shopsplusproject.org/resource-center/strengthening-health-systems-engaging-private-health-sector-promising-hivaids Available. Accessed.
- 125.Wafula F, Onoka C, Musiega A, et al. Healthcare clinic and pharmacy chains in Kenya and Nigeria: A qualitative exploration of the opportunities and risks they present for healthcare regulatory systems. Int J Health Plann Manage. 2022;37:3329–43. doi: 10.1002/hpm.3560. [DOI] [PubMed] [Google Scholar]
- 126.Miller R, Wafula F, Onoka CA, et al. When technology precedes regulation: the challenges and opportunities of e-pharmacy in low-income and middle-income countries. BMJ Glob Health. 2021;6:e005405. doi: 10.1136/bmjgh-2021-005405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Hutchinson E, Hansen KS, Sanyu J, et al. Is it possible for drug shops to abide by the formal rules? The structural determinants of community medicine sales in Uganda. BMJ Glob Health . 2023;8:e011097. doi: 10.1136/bmjgh-2022-011097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Onwujekwe O, Agwu P, Orjiakor C, et al. Corruption in Anglophone West Africa health systems: a systematic review of its different variants and the factors that sustain them. Health Policy Plan. 2019;34:529–43. doi: 10.1093/heapol/czz070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Gaitonde R, Oxman AD, Okebukola PO, et al. Interventions to reduce corruption in the health sector. Cochrane Database Syst Rev. 2016;2016 doi: 10.1002/14651858.CD008856.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.