Abstract
Prostatic cysts are common in the adult male population with intervention of these cysts typically reserved for symptomatic patients. However, current literature is limited on the diagnosis and management of prostatic cysts in the pediatric population. We report the case of a 13-year-old boy with autosomal recessive polycystic kidney disease (ARPKD) who presented with an incidentally discovered prostatic cyst. This is the first known case report to highlight the clinical presentation, diagnosis, and management of an asymptomatic prostatic cyst in ARPKD.
Keywords: Prostatic cyst, Renal cysts, Autosomal recessive polycystic kidney disease, Pediatric
Highlights
-
•
Although previously never reported, prostatic cysts may occur in pediatric patients with ARPKD.
-
•
The majority of prostatic cysts are asymptomatic and incidentally discovered on imaging studies.
-
•
There is currently insufficient data to recommend routine screening for or specific management of prostatic cysts in ARPKD.
1. Introduction
Cysts of prostate tissue are commonly seen in urological practice with a prevalence of 0.5%–7.9% among adult male patients.1 Most cases are asymptomatic and diagnosed incidentally on imaging. Specific subgroups of prostatic cysts are associated with clinically significant findings including lower urinary tract symptoms (LUTS); malignancy; infertility; or infectious processes, such as urinary tract infections (UTIs) and prostatitis.2,3 Typically, intervention is reserved for these symptomatic patients. In the pediatric population, however, less is known regarding the diagnosis and management of prostatic cysts as literature regarding this topic has mainly been limited to case reports.4,5
A case report published in 2021 described a 15-year-old male patient with autosomal dominant polycystic kidney disease (ADPKD) who was incidentally diagnosed with a prostatic cyst.6 ADPKD is a multisystem disease characterized by cysts of the kidneys, liver, pancreas and spleen. Prostatic cysts in ADPKD are less common and mostly present asymptomatically, with a minority of patients reporting irritative or obstructive urinary symptoms.7,8 Autosomal recessive polycystic kidney disease (ARPKD) similarly has cystic disease of the kidney; however, cysts in ARPKD are mostly microcystic and occur within the collecting tubule.9 To our knowledge, we present the first report of a prostatic cyst in a patient with ARPKD.
2. Case presentation
A 13-year-old male with past medical history significant for ARPKD, chronic kidney disease (CKD) stage 3a, and congenital hepatic fibrosis status post orthotopic liver transplant was admitted to the hospital for fever in the setting of Granulicatella adiacens bacteremia. Regarding this patient's urological history, he had known prenatal oligohydramnios and enlarged kidney size on prenatal ultrasound. At 34 weeks, he was delivered via C-section due to breech presentation and was hospitalized in the neonatal intensive care unit for one month, briefly requiring intubation and vasopressors. During this time, he was found to have echogenic, enlarged bilateral kidneys with multiple small cysts. He was diagnosed with ARPKD in his first year of life, further confirmed by genetic testing for PKHD1. Since his diagnosis, he has received a yearly ultrasound of his abdomen.
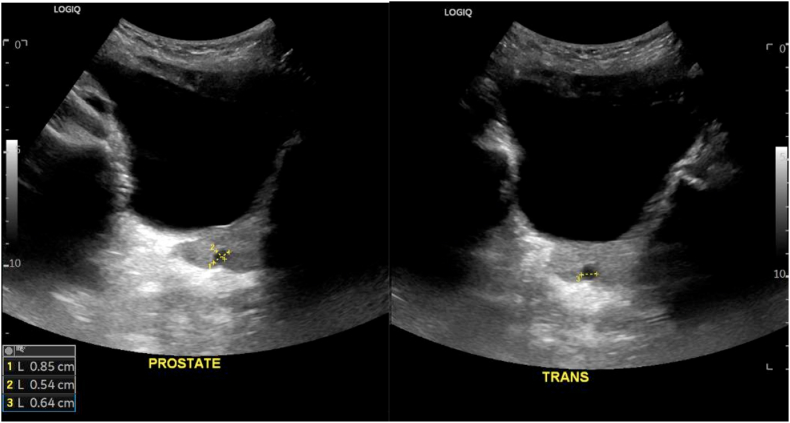
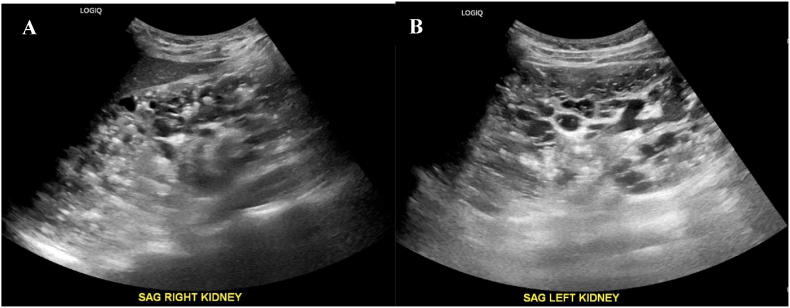
During his recent hospital admission, a repeat renal-bladder ultrasound (RBUS) was obtained due to concern for genitourinary infection given his history of ARPKD. This demonstrated a 0.9 x 0.5 × 0.6 cm simple cyst within the prostate gland (Fig. 1), which had not been present on previous studies. The RBUS was additionally notable for an enlarged right kidney measuring at least 17.5 cm, an enlarged left kidney measuring at least 15 cm, and loss of normal corticomedullary differentiation with diffuse cystic changes throughout the kidneys bilaterally (Fig. 2), consistent with ARPKD. Postvoid residual was measured to be 38 cc. From a clinical perspective, the patient was asymptomatic at this time, without irritative or obstructive voiding symptoms.
Fig. 1.
Ultrasonography of the prostate showing a simple cyst measuring 0.9 x 0.5 × 0.6 cm.
Fig. 2.
Ultrasonography of bilateral kidneys showing enlarged (A) right and (B) left kidneys with diffuse, innumerable cysts.
A RBUS obtained 6 weeks post-hospital discharge demonstrated the same findings. The total prostate-specific antigen (PSA) at this time was 0.9 ng/mL. Active surveillance was the recommended management plan, which includes a yearly RBUS with special attention to the prostate and PSA monitoring.
3. Discussion
Prostatic cyst is a common diagnosis in the adult male population, with a prevalence of 0.5%–7.9%. There have been several classifications proposed for prostatic cysts in accordance with clinical presentation or diagnostic imaging. A retrospective analysis of a transrectal ultrasound database of 6000 patients seen between 2001 and 2007 at an Italian institution proposed clinical management for prostatic cysts based on ultrasound findings and pathological features. The study recommended observation for isolated medial cysts, ejaculatory duct cysts, and simple or multiple cysts of the parenchyma. The authors note that treatment should be reserved for men who are infertile or exhibit symptoms of infection.1
Prostatic cysts in the pediatric population have been rarely reported in literature. The majority of reports in this population have been regarding prostatic utricle cysts (PUC), a specific type of prostatic cysts that are midline cysts thought to originate from Mullerian ducts, Wolffian ducts, and urogenital sinus remnants. They occur due to abnormalities during embryogenesis and are commonly associated with genitourinary abnormalities, with hypospadias or disorders of sexual development present in up to 90% of cases.10 The incidence of PUC at time of autopsy is 1% in men, with most cases found in individuals under 20 years old. The prevalence of symptomatic PUC is significant at 30%–40%, with the most common presenting complaint being genitourinary tract infections, such as recurrent UTIs and epididymo-orchitis.4 Notably, our patient has no history of hypospadias or disorders of sexual development, which indicates that his prostatic cyst is likely not a PUC.
In our patient, it is plausible that his prostatic cyst was either an independent finding or occurred in association with his ARPKD. Upon reviewing previously published reports of autopsies in patients with ARPKD, we found no mentions of cysts in organs outside the kidneys. Authors focused primarily on the histopathological findings in the kidneys, as well as associated hepatic fibrosis and pulmonary hypoplasia in neonates.11, 12, 13 There has been one prior case report published on the diagnosis of an incidental prostatic cyst on routine RBUS imaging in an ADPKD pediatric patient. He was asymptomatic and management strategy included active surveillance with yearly RBUS with additional focus on his prostate.6 In ADPKD, extrarenal cysts of the liver, seminal vesicles, arachnoid membrane, and pancreas are common. In contrast, ARPKD presents with microcystic lesions confined to the collecting tubules of kidneys.14
Due to lack of literature on prostatic cysts in both the pediatric population and ARPKD patient population, there are no existing guidelines for the management of prostatic cysts in ARPKD. In this case, we proceeded with nonsurgical outpatient management. This approach was chosen considering the asymptomatic nature of the prostatic cyst and potential complications of surgical intervention, including infertility, urinary incontinence, and urethral stricture. We recommended RBUS and PSA monitoring at yearly intervals, acknowledging that the relationship between prostatic cysts and PSA has not been fully elucidated.15 If the patient were to present with symptoms such as recurrent UTIs, voiding disorders, abdominal pain, or hematuria in the future, further imaging studies and possible surgical intervention may be considered.
4. Conclusion
This is the first known case report documenting a prostatic cyst in a pediatric patient with ARPKD. We highlight a possible association between prostatic cysts and ARPKD, although little is documented in the literature regarding the screening, surveillance, and management of these prostatic cysts. Given the majority of prostatic cysts are incidentally discovered on imaging studies,16 the prevalence of these cysts may be underreported in both ARPKD and pediatric patients. Considering the rarity and relatively asymptomatic nature of this condition, we currently cannot recommend routine screening of prostatic cysts in all ARPKD patients. Future case reports documenting prostatic cysts in ARPKD patients would be helpful to further elucidate the prevalence, pathogenesis, and prognosis of this condition.
CRediT authorship contribution statement
Ketty Bai: Writing – original draft, Investigation, Data curation, Conceptualization. Niccola B. Lynch: Writing – review & editing. Christina P. Carpenter: Writing – review & editing, Supervision.
Consent statement
We obtained written consent for publication of this case report.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interests
None.
References
- 1.Galosi A.B., Montironi R., Fabiani A., Lacetera V., Galle G., Muzzonigro G. Cystic lesions of the prostate gland: an ultrasound classification with pathological correlation. J Urol. 2009;181(2):647–657. doi: 10.1016/j.juro.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 2.Issa M.M., Kalish J., Petros J.A. Clinical features and management of anterior intraurethral prostatic cyst. Urology. 1999;54(5):923. doi: 10.1016/s0090-4295(99)00315-5. [DOI] [PubMed] [Google Scholar]
- 3.Qiu Y., Liu Y., Ren W., Ren J. Prostatic cyst in general practice: a case report and literature review. Medicine (Baltim) 2018;97(9) doi: 10.1097/MD.0000000000009985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dai L.N., He R., Wu S.F., Zhao H.T., Sun J. Surgical treatment for prostatic utricle cyst in children: a single-center report of 15 patients. Int J Urol. 2021;28(6):689–694. doi: 10.1111/iju.14543. [DOI] [PubMed] [Google Scholar]
- 5.Schuhrke T.D., Kaplan G.W. Prostatic utricle cysts (mullerian duct cysts) J Urol. 1978;119(6):765–767. doi: 10.1016/s0022-5347(17)57627-2. [DOI] [PubMed] [Google Scholar]
- 6.Colaco M., Cannon G.M., Moritz M.L. Prostatic cyst in a pediatric patient with autosomal dominant polycystic kidney disease. BMJ Case Rep. 2021;14(2) doi: 10.1136/bcr-2020-236237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hooda A.K., Sanga S., Raychaudhury N., Narula A.S. Prostatic cyst : association with autosomal dominant polycystic kidney disease. Med J Armed Forces India. 2006;62(3):273–274. doi: 10.1016/S0377-1237(06)80019-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sood V., Pattanashetti N., Bilal Azam M., Ramachandran R. Prostatic cyst in autosomal dominant polycystic kidney disease: unusual association. BMJ Case Rep. 2019;12(4) doi: 10.1136/bcr-2018-228617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hartung E.A., Guay-Woodford L.M. Autosomal recessive polycystic kidney disease: a hepatorenal fibrocystic disorder with pleiotropic effects. Pediatrics. 2014;134(3):e833–e845. doi: 10.1542/peds.2013-3646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aminsharifi A., Afsar F., Pakbaz S. Laparoscopic management of mullerian duct cysts in infants. J Pediatr Surg. 2011;46(9):1859–1864. doi: 10.1016/j.jpedsurg.2011.04.008. [DOI] [PubMed] [Google Scholar]
- 11.Taneda S., Honda K., Aoki A., et al. An autopsy case of clinically un-diagnosed autosomal recessive polycystic kidney disease in 77-year-old male. Pathol Int. 2012;62(12):811–816. doi: 10.1111/pin.12011. [DOI] [PubMed] [Google Scholar]
- 12.Sherwani R.K., Kumar A., Rahman K., Rabbani T. Autosomal recessive polycystic kidney disease: the importance of autopsy of suspected cases and genetic counselling. BMJ Case Rep. 2010;2010 doi: 10.1136/bcr.03.2010.2843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou X.H., Hui Z.Y., Li Y. Clinical and pathological features of a neonate with autosomal recessive polycystic kidney disease caused by a nonsense PKHD1 mutation. World J Pediatr. 2013;9(1):76–79. doi: 10.1007/s12519-013-0407-3. [DOI] [PubMed] [Google Scholar]
- 14.Bergmann C., von Bothmer J., Ortiz Bruchle N., et al. Mutations in multiple PKD genes may explain early and severe polycystic kidney disease. J Am Soc Nephrol. 2011;22(11):2047–2056. doi: 10.1681/ASN.2010101080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen H.K., Pemberton R. A large, benign prostatic cyst presented with an extremely high serum prostate-specific antigen level. BMJ Case Rep. 2016;2016 doi: 10.1136/bcr-2015-213381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nghiem H.T., Kellman G.M., Sandberg S.A., Craig B.M. Cystic lesions of the prostate. Radiographics. 1990;10(4):635–650. doi: 10.1148/radiographics.10.4.1696019. [DOI] [PubMed] [Google Scholar]