Abstract
Objectives
This single‐center, cross‐sectional study aims to elucidate the clinical presentation, diagnostic evaluation, and outcomes in a subset of pediatric patients with atypical and/or challenging presentations of Meckel's diverticulum.
Methods
We conducted a single‐center cross‐sectional study on children diagnosed with Meckel's diverticulum at Children's Health in Dallas, Texas between 2010 and 2022. We identified 11 patients aged 0–17‐years‐old with confirmed Meckel's diverticulum who presented with atypical symptoms and/or a challenging diagnostic course. Patient demographics, symptoms at presentation, diagnostic workup, time to diagnosis, management, and outcomes were collected. Descriptive statistics were utilized.
Results
Eleven patients (n = 8, 73% male) were included in the study with an average age of 10.5 years (range: 1–17 years). The mean time interval from initial presentation of symptoms to diagnosis was 8 months (range: 0–33 months). Barriers to diagnosis of Meckel's diverticulum identified in our study included atypical presentations, negative or nonconfirmatory Meckel scan results, negative surgical findings, and competing differential diagnoses.
Conclusion
Meckel's diverticulum is a challenging diagnosis and should be considered even if initial evaluation is negative as certain patients exhibit atypical presentations that necessitate surgical intervention for diagnosis.
Keywords: atypical presentation, Meckel's scan, surgery
What is Known
Meckel's diverticulum classically presents in pediatric patients with painless rectal bleeding.
Technetium‐99m pertechnetate scan (Meckel's scan) is the most common initial diagnostic modality for Meckel's diverticulum.
Meckel's diverticulum can lead to complications such as obstruction, perforation, and intussusception, and so forth.
What is New
Diagnosis of Meckel's diverticulum can be challenging due to atypical clinical presentations, negative or unusual diagnostic testing, complex medical history, competing differential diagnoses, and negative surgical findings.
Surgical intervention is the cornerstone for diagnosis and treatment of Meckel's diverticulum in challenging cases.
1. INTRODUCTION
Meckel's diverticulum is a common congenital abnormality caused by incomplete obliteration of the omphalomesenteric canal during the fifth through seventh weeks of embryological development resulting in a true diverticulum in the small bowel. 1 Though most cases remain asymptomatic throughout a person's lifetime, the most common symptomatic presentation of Meckel's diverticulum in children is painless rectal bleeding. 2 The presence of heterotopic tissue, most commonly gastric or pancreatic tissue, occurs in up to 57% of symptomatic patients and can lead to substantial gastrointestinal blood loss, small bowel obstruction, perforation, ulceration, and diverticulitis. 1 Prompt diagnosis and intervention may be difficult as symptomatic Meckel's diverticulum can mimic other conditions including milk protein allergy, infectious enteritis, inflammatory bowel disease, acute appendicitis, peptic ulcer disease, and small bowel obstruction. The most common diagnostic modality utilized is the Technetium‐99m pertechnetate scan (Meckel's scan), which concentrates in heterotopic gastric tissue with greater than 90% sensitivity and specificity. 3 Sensitivity and specificity of Meckel's scan have been reported to be higher in patients with rectal bleeding compared with any other presenting symptom. 4 Other diagnostic methods such as video capsule endoscopy (VCE) of the small bowel and computed tomography enterography have also been used to identify diverticula and bleeding in the small bowel. 5 , 6 , 7 Despite the advances in noninvasive diagnostic testing, preoperative diagnosis of Meckel's diverticulum can be challenging, and often surgical exploration is required to diagnose and treat symptomatic Meckel's diverticulum. 5
We aim to describe clinical features, diagnostic testing, and outcomes of pediatric patients with a challenging diagnosis of Meckel's diverticulum that will contribute to improved awareness and knowledge of uncommon presentations of this common anomaly.
2. METHODS
Following approval by the University of Texas Southwestern Medical Center Institutional Review Board (IRB), the electronic medical record at the University of Texas Southwestern/Children's Health was utilized to obtain clinical information. Eleven patients were included in our study. Six patients were identified by another University of Texas Southwestern/Children's Health IRB‐approved retrospective study of small bowel VCE in pediatric patients; this subset of patients underwent VCE before diagnosis of Meckel's diverticulum. Five patients were identified through discussion of challenging patient cases at our division pediatric gastroenterology meeting. Inclusion criteria included surgical histopathology reports confirming a diagnosis of Meckel's diverticulum. An additional criterion for inclusion was a challenging diagnosis of Meckel's diverticulum as defined by an uncommon presentation, multiple or inconclusive diagnostic testing, and/or delay in diagnosis. Exclusion criteria included patients over 21 years old, missing data (no available records or accessible clinical records), incidental diagnosis of Meckel's diverticulum, or other etiologies (i.e., inflammatory bowel disease, polyposis, etc.).
Deidentified patient information was collected and tabulated including age at presentation, sex, clinical presentation, laboratory studies (complete blood count, comprehensive metabolic panel, inflammatory markers, and albumin), imaging reports, endoscopic findings, histopathology reports, surgical interventions, and operative findings (Table 1). Pertinent patient outcomes were also collected. Descriptive statistics were utilized with continuous variables summarized as median and standard deviation, and dichotomous variables were described using frequency and proportion.
Table 1.
Summary of presentation, diagnostic evaluation, and challenges faced to diagnosis.
| 1 | Age, sex | 7‐year‐old male |
| Presenting symptoms | Blood in stool, acute anemia | |
| Time to diagnosis | 6 months | |
| Pertinent lab results | Hgb ≥ 12, albumin > 4.0, fecal calprotectin 40 μg/g, CRP < 0.9, ESR < 20 | |
| Imaging findings | Meckel's scan positive, CT abdomen, and pelvis revealed ileitis, 2 cm abscess in the right lower quadrant, and pneumoperitoneum | |
| Meckel scan pretreatment (if applicable) | Performed at an outside hospital, unable to determine | |
| Endoscopic findings | No EGD or colonoscopy was performed, small bowel VCE‐negative | |
| Surgical findings | Laparoscopy revealed perforation and a small abscess cavity | |
| Histopathology | Meckel's diverticulum with mucosal ulcer and perforation with abscess, unspecified heterotopic gastric tissue present | |
| Challenges faced to diagnosis | Prior surgical findings negative, atypical presentation with perforation of Meckel's diverticulum | |
| 2 | Age, sex | 10‐year‐old female |
| Presenting symptoms | Blood in stool, acute anemia | |
| Time to diagnosis | 0 months | |
| Pertinent lab results | Hgb ≤ 8, albumin < 4.0, fecal calprotectin 168 μg/g, CRP < 0.9, ESR < 20 | |
| Imaging findings | CT abdomen with fluid‐filled structure in central superior pelvis that correlated with positive Meckel's scan; CT angiogram negative | |
| Meckel scan pretreatment (if applicable) | NPO 4 h before exam, IV famotidine 1 h before exam. Patient was also receiving IV omeprazole 1 mg/kg twice daily for gastrointestinal bleeding | |
| Endoscopic findings | One month before presentation, EGD revealed distal esophagus erythema; colonoscopy revealed pinworm infestation in colon. No VCE performed | |
| Surgical findings | Laparoscopy revealed deposit of glandular tissue in proximal jejunum | |
| Histopathology | Meckel's diverticulum with oxyntic‐type gastric mucosa and chronic inflammation | |
| Challenges faced to diagnosis | Competing differential diagnoses due to recent pinworm infection and abnormal CT abdomen at outside hospital | |
| 3 | Age, sex | 17‐year‐old male |
| Presenting symptoms | Blood in stool, acute anemia | |
| Time to diagnosis | 0 months | |
| Pertinent lab results | Hgb ≤ 8, albumin < 4.0, fecal calprotectin 327 μg/g, CRP > 0.9, ESR > 20 | |
| Imaging findings | CT angiogram negative, Meckel's scan positive | |
| Meckel scan pretreatment (if applicable) | NPO 4 h before exam, IV famotidine 1 h before exam. Patient was also receiving IV omeprazole twice daily for 6 days and octreotide 50 μg/h for one day for gastrointestinal bleeding | |
| Endoscopic findings | EGD with cobble stoning in stomach; colonoscopy normal. VCE negative | |
| Surgical findings | Laparoscopy converted to laparotomy revealed Meckel's diverticulum comprising >50% ileal lumen | |
| Histopathology | Meckel's diverticulum and ulcer, unspecified heterotopic gastric mucosa | |
| Challenges faced to diagnosis | Competing differential diagnoses given a history of gastrointestinal bleed due to NSAIDs and Helicobacter pylori infection, concern for infectious colitis | |
| 4 | Age, sex | 15‐year‐old male |
| Presenting symptoms | Chronic anemia | |
| Time to diagnosis | 15 months | |
| Pertinent lab results | Hgb ≤ 8, albumin < 4.0, fecal calprotectin 147 μg/g, CRP < 0.9, ESR > 20 | |
| Imaging findings | Negative Meckel's scan, magnetic resonance enterography abdomen and pelvis negative | |
| Meckel scan pretreatment (if applicable) | NPO 4 h before exam, oral famotidine 20 mg twice daily for 48 h before exam | |
| Endoscopic findings | EGD and colonoscopy normal. Single balloon enteroscopy revealed two lesions suspicious for ulcers. VCE revealed ulcers in jejunum suggestive of Crohn's and signs of bleeding in jejunum and ileum | |
| Surgical findings | Laparoscopy revealed healed chronic ulcer on mesenteric wall of small bowel opposite to the Meckel's diverticulum | |
| Histopathology | Meckel's diverticulum with focal chronic ulceration and antral‐type gastric mucosa | |
| Challenges faced to diagnosis | Negative Meckel's scan, competing differential diagnoses due to concern for bone marrow failure as well as small bowel VCE findings suggesting inflammatory bowel disease | |
| 5 | Age, sex | 1‐year‐old female |
| Presenting symptoms | Blood in stool, abdominal pain, nonbloody, and nonbilious emesis | |
| Time to diagnosis | 33 months | |
| Pertinent lab results | Hgb ≤ 8, albumin < 4.0, fecal calprotectin NA, CRP < 0.9, ESR < 20 | |
| Imaging findings | Two negative Meckel's scans 1 week apart | |
| Meckel scan pretreatment (if applicable) | NPO 4 h before the first exam. No pretreatment was given for the first Meckel scan, though the patient was receiving IV omeprazole 1 mg/kg twice daily for gastrointestinal bleeding. NPO status is unclear for the second exam. Pretreatment for the second exam included oral ranitidine twice daily and oral esomeprazole daily for 7 days before exam | |
| Endoscopic findings | EGD revealed ulcer in the fundus, treated with APC and 2 clips; normal colonoscopy. VCE revealed Meckel's diverticulum with ulceration | |
| Surgical findings | Laparoscopy revealed wide‐based Meckel's with ulceration | |
| Histopathology | Meckel's diverticulum with oxyntic‐type gastric mucosa | |
| Challenges faced to diagnosis | Two negative Meckel's scans, atypical presentation of emesis and abdominal pain, competing differential diagnoses due to history of gastric ulcer | |
| 6 | Age, sex | 14‐year‐old male |
| Presenting symptoms | Chronic anemia | |
| Time to diagnosis | 21 months | |
| Pertinent lab results | Hgb ≤ 8, albumin > 4.0, fecal calprotectin 198 μg/g, CRP < 0.9, ESR NA | |
| Imaging findings | Negative Meckel's scan, CT abdomen and pelvis negative, MRE negative | |
| Meckel scan pretreatment (if applicable) | Performed at an outside hospital, unable to determine | |
| Endoscopic findings | EGD and colonoscopy normal. VCE negative | |
| Surgical findings | Laparoscopy converted to laparotomy revealed Meckel's diverticulum suspended to midline abdominal wall | |
| Histopathology | Meckel's diverticulum with mucosal ulceration and acute inflammation, no heterotopic tissue identified | |
| Challenges faced to diagnosis | Atypical presentation of mild chronic anemia with intermittent bleeding per rectum, guaiac stool negative, and negative Meckel's scan | |
| 7 | Age, sex | 12‐year‐old male |
| Presenting symptoms | Blood in stool, acute anemia | |
| Time to diagnosis | 2 months | |
| Pertinent lab results | Hgb ≤ 8, albumin < 4.0, fecal calprotectin NA, CRP NA, ESR NA | |
| Imaging findings | Negative Meckel's scan, NM‐RBC scan revealed active bleeding in the right upper quadrant of the abdomen, likely in the small bowel | |
| Meckel scan pretreatment (if applicable) | NPO 4 h before exam, IV famotidine 1 h before exam. Patient was also receiving oral lansoprazole twice daily for 3 days before exam for gastrointestinal bleeding | |
| Endoscopic findings | EGD with nodularity and furrowing of esophagus, erythema in antrum; colonoscopy revealed descending colon with edema and mild erythema. VCE negative. | |
| Surgical findings | Laparoscopy revealed Meckel's diverticulum adherent to the adjacent ileum | |
| Histopathology | Meckel's diverticulum with oxyntic‐type gastric mucosa | |
| Challenges faced to diagnosis | Negative Meckel's scan, negative VCE | |
| 8 | Age, sex | 5‐year‐old male |
| Presenting symptoms | Blood in stool, acute anemia, abdominal pain | |
| Time to diagnosis | 1 month | |
| Pertinent lab results | Hgb ≤ 8, albumin < 4.0, Fecal calprotectin NA, CRP < 0.9, ESR > 20 | |
| Imaging findings | Meckel's scan negative | |
| Meckel scan pretreatment (if applicable) | No pretreatment medication received, NPO status unclear before the exam | |
| Endoscopic findings | EGD revealed erythema and white exudates in the duodenum; colonoscopy revealed old red blood. VCE revealed fresh blood originating from area suspicious for Meckel's diverticulum | |
| Surgical findings | Laparoscopy revealed Meckel's diverticulum | |
| Histopathology | Meckel's diverticulum with oxyntic‐type gastric mucosa | |
| Challenges faced to diagnosis | Negative Meckel's scan, atypical abdominal pain, competing differential diagnoses due to inflammation seen on EGD | |
| 9 | Age, sex | 12‐year‐old male |
| Presenting symptoms | Blood in stool, acute anemia, abdominal pain | |
| Time to diagnosis | 0 months | |
| Pertinent lab results | Hgb 8–12, Albumin NA, Fecal calprotectin NA, CRP NA, ESR NA | |
| Imaging findings | Negative Meckel's scan, negative CT abdomen and pelvis | |
| Meckel scan pretreatment (if applicable) | Performed at an outside hospital, unable to determine | |
| Endoscopic findings | EGD and colonoscopy normal. VCE normal | |
| Surgical findings | Laparoscopy converted to laparotomy revealed inflamed Meckel's diverticulum in the mid‐jejunum | |
| Histopathology | Meckel's diverticulum with oxyntic‐type gastric mucosa | |
| Challenges faced to diagnosis | Atypical presentation of abdominal pain, negative Meckel's scan at outside facility, negative VCE | |
| 10 | Age, sex | 11‐year‐old male |
| Presenting symptoms | Bilious emesis, abdominal pain | |
| Time to diagnosis | 0 months | |
| Pertinent lab results | Hgb ≥ 12, albumin < 4.0, fecal calprotectin NA, CRP < 0.9, ESR < 20 | |
| Imaging findings | CT abdomen with IV and oral contrast revealed extensive fecalization and bowel wall thickening concerning for chronic partial small bowel obstruction | |
| Meckel scan pretreatment (if applicable) | NA | |
| Endoscopic findings | NA | |
| Surgical findings | Exploratory celiotomy revealed necrotic diverticulitis creating an internal hernia with small bowel stricture; Meckel's resection and small bowel stricturoplasty | |
| Histopathology | Meckel's diverticulum with transmural necrosis, hemorrhage, and prominent neutrophilic infiltrate | |
| Challenges faced to diagnosis | Atypical presentation of small bowel obstruction | |
| 11 | Age, sex | 12‐year‐old female |
| Presenting symptoms | Constipation, abdominal pain | |
| Time to diagnosis | 9 months | |
| Pertinent lab results | Hgb 8–12, albumin NA, fecal calprotectin NA, CRP NA, ESR NA | |
| Imaging findings | Abdominal x‐ray negative, MRE negative | |
| Meckel scan pretreatment (if applicable) | NA | |
| Endoscopic findings | EGD revealed findings suggestive of eosinophilic esophagitis; colonoscopy revealed fresh blood in terminal ileum and colon suggestive of recent mid‐intestinal bleeding. VCE revealed polypoid lesions suspicious of Peutz‐Jegher syndrome versus malignancy | |
| Surgical findings | Laparoscopy with laparoscopic‐assisted push enterostomy revealed thickened area of mesentery deemed abnormal | |
| Histopathology | Meckel's diverticulum with oxyntic‐type gastric mucosa with adjacent deep ulcer | |
| Challenges faced to diagnosis | Atypical presentation of abdominal pain and constipation, competing differential diagnoses due to VCE findings suggesting polyps |
Abbreviations: APC, argon plasma coagulation; CRP, C‐reactive protein; CT, computed tomography; EGD, esophagogastroduodenoscopy; ESR, erythrocyte sedimentation rate; Hgb, hemoglobin; IV, intravenous; MRE, magnetic resonance enterography; NA, not obtained; NM‐RBC, nuclear medicine‐tagged red blood cell; NPO, nothing by mouth; NSAIDs, nonsteroidal anti‐inflammatory drugs; VCE, video capsule endoscopy.
3. RESULTS
Eleven patients (n = 8, 73% male) were included in the study with an average age of 10.5 years (range: 1–17 years). Initial clinical presentations included bloody stools (n = 7), acute symptomatic anemia (n = 7), abdominal pain (n = 3), chronic anemia (n = 2), emesis (n = 2), and constipation (n = 1). The patients are divided below into three subgroups: positive Meckel's scans, negative Meckel's scans, and no Meckel's scan performed. A comprehensive summary for each patient is provided including pertinent laboratory, radiographic, endoscopic, surgical, and pathologic findings (Table 1).
3.1. Positive Meckel's scans
Patient 1 is a 7‐year‐old male who initially presented to an outside hospital for bloody stools and anemia who underwent a Meckel's scan which was positive. However, laparoscopy at that time was negative. Six months later, he presented with acute abdominal pain due to perforation of his Meckel's diverticulum and a small abscess cavity seen on computed tomography (CT) of his abdomen and pelvis (Figure 2).
Figure 2.
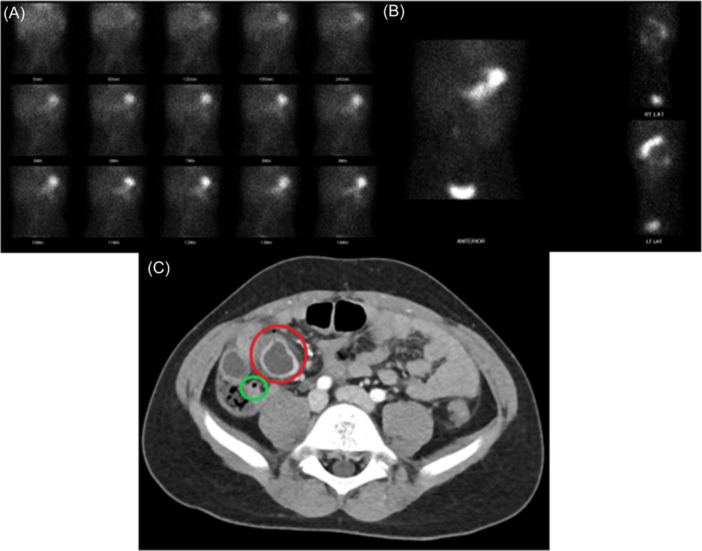
Imaging findings of two patients with Meckel's diverticulum. (A, B) The first 15 min (A) and 1‐h images (B) of a Meckel's scan in a 5‐year‐old boy with abdominal pain, anemia, and bloody stools. No preimaging medication was received. Physiologic radiotracer uptake is seen, and no abnormal radiotracer accumulation is identified. (C) CT abdomen and pelvis with IV contrast in a 7‐year‐old boy with abdominal pain who previously had a negative Meckel's scan and negative laparoscopy. A fluid collection with thick enhancing wall, inflammatory fat stranding, and a punctate focus of extraluminal air along its anterior margin (red circle) suggested perforation. A normal appendix was identified (green circle). CT, computed tomography.
Patient 2 is a 10‐year‐old female who presented with bloody stools and acute anemia. However, she was diagnosed with a pinworm infection 1 month prior at an outside hospital after presenting with abdominal pain, where a CT abdomen also revealed a fluid‐filled structure in the central superior pelvis. At Children's Health, a CT angiogram was negative for vascular malformations, and a Meckel's scan revealed positive uptake in the area correlating with the previously identified fluid‐filled structure on CT abdomen.
Patient 3 is a 17‐year‐old male with a history of an nonsteroidal anti‐inflammatory drug (NSAID)‐induced upper gastrointestinal bleed and Helicobacter pylori infection presenting with a 2‐day history of bloody stools and fatigue. Due to his history, CT angiogram abdomen, and pelvis, esophagogastroduodenoscopy (EGD), colonoscopy, and small bowel VCE were performed first and were unrevealing. His Meckel's scan was then positive, and laparotomy confirmed the diagnosis.
3.2. Negative Meckel's scans
Patient 4 is a 15‐year‐old male with an atypical presentation of chronic anemia requiring multiple hospitalizations for blood transfusions and intravenous (IV) iron. A bone marrow evaluation was prompted due to symptomatic thrombocytopenia with epistaxis and leukopenia, which was unremarkable. Single balloon enteroscopy revealed two lesions suspicious for ulcers. He had two small bowel VCE studies suggesting Crohn's disease due to ulcers, inflammation, and bleeding in the jejunum. Laparoscopy revealed a Meckel's diverticulum, and his pancytopenia was attributed to severe iron‐restricted hematopoiesis, which resolved after his Meckel's diverticulum was removed (Figure 1).
Figure 1.
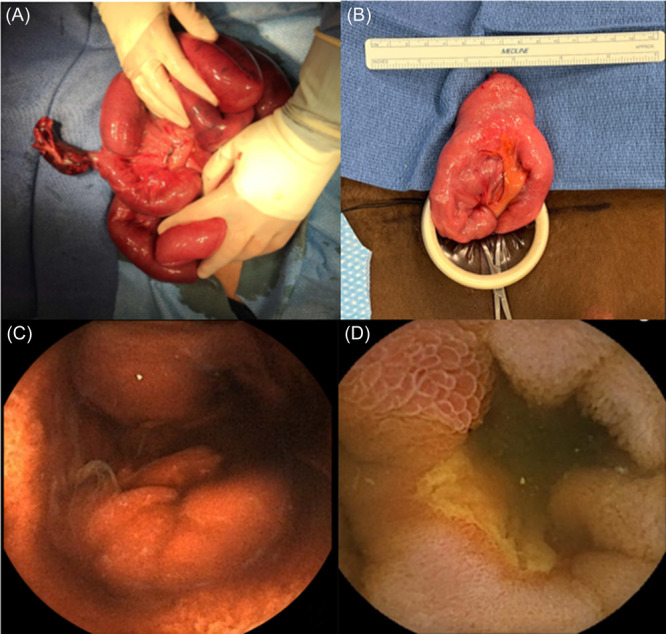
Operative and capsule endoscopy findings in patients with Meckel's diverticulum. (A) Acute Meckel's diverticulitis causing an internal hernia and small bowel obstruction in an 11‐year‐old patient presenting with severe abdominal pain and bilious emesis. (B) Large Meckel's diverticulum in a 15‐year‐old patient presenting with chronic anemia, and small bowel VCE revealed ulcers concerning for Crohn's disease (view D). (C) VCE image of a suspected polypoid lesion in the small bowel of a 12‐year‐old patient presenting with chronic abdominal pain and constipation. Surgical exploration confirmed diagnosis of Meckel's diverticulum. (D) VCE image of ulcers and inflammation, suggesting Crohn's disease, in a 15‐year‐old patient presenting with chronic anemia. VCE, video capsule endoscopy.
Patient 5 is a 1‐year‐old female who initially presented with bloody stools, nonbloody and non‐bilious emesis, and symptomatic anemia requiring a blood transfusion. She had two negative Meckel's scans 1 week apart from one another. EGD revealed a Dieulafoy's ulcer in the fundus that was not actively bleeding, but argon plasma coagulation and clip placement were performed due to a pulsating vessel, and her symptoms eventually resolved. Almost 3 years later, she presented again at age 4 with the same initial symptoms in addition to abdominal pain. Repeat Meckel's scan was not performed due to her history of a gastric ulcer and repeat EGD and colonoscopy were negative. Small bowel VCE revealed a Meckel's diverticulum, and the diagnosis was confirmed by laparoscopy.
Patient 6 is a 14‐year‐old male with an atypical presentation of chronic anemia. Laparoscopy converted to laparotomy revealed a Meckel's diverticulum suspended to the midline abdominal wall. Following surgery, his chronic anemia resolved, and he was able to discontinue long‐term iron infusions.
Patient 7 is a 12‐year‐old male presenting with bloody stools and symptomatic anemia requiring a blood transfusion. His Meckel's scan was negative, and the bleeding resolved spontaneously. Two months later, the bleeding recurred, and a nuclear medicine‐tagged red blood cell (NM‐RBC) scan demonstrated active gastrointestinal bleeding in the right upper quadrant consistent with small bowel bleeding. Laparoscopy revealed an area of thickening adherent to the adjacent ileum, which was confirmed as a Meckel's diverticulum on surgical pathology.
Patient 8 is a 5‐year‐old male presenting with bloody stools and symptomatic anemia, though he also presented atypically with abdominal pain. His Meckel's scan was negative (Figure 2). EGD revealed erythema and white exudates in the duodenum, and colonoscopy revealed old red blood. Small bowel VCE suggested Meckel's diverticulum due to bleeding in the ileum. Laparoscopy confirmed the diagnosis.
Patient 9 is a 12‐year‐old male presenting atypically with abdominal pain in addition to bloody stools and anemia. After negative work‐up including Meckel's scan, CT abdomen and pelvis, EGD, colonoscopy, and small bowel VCE, he underwent laparoscopy which was converted to laparotomy and revealed a Meckel's diverticulum in the mid‐jejunum (as opposed to the typical location in the ileum).
3.3. No Meckel's scan performed
Patient 10 is an 11‐year‐old male with an atypical presentation of acute periumbilical pain and bilious emesis due to necrotic and perforated Meckel's diverticulitis creating an internal hernia with small bowel obstruction (Figure 1).
Patient 11 is a 12‐year‐old female with an atypical presentation of persistent periumbilical pain and constipation. Small bowel VCE revealed polypoid lesions in the proximal and mid‐small bowel that were suspected to be possible Peutz–Jegher polyps versus clots versus malignant mass (Figure 1). Laparoscopy revealed a thickened area of mesentery deemed abnormal (thought to be the suspected polypoid lesions seen on small bowel VCE) and was found to be a Meckel's diverticulum.
4. DISCUSSION
The results of our study highlight the challenges faced when diagnosing Meckel's diverticulum. While most symptomatic pediatric patients present classically with painless rectal bleeding, others may present with a constellation of symptoms, laboratory results, endoscopy findings, and imaging findings. Negative Meckel's scan coupled with unrevealing endoscopy findings along with competing diagnoses may lead to a delay in diagnosis and treatment. In addition, a patient's medical history may obscure the interpretation of certain studies and/or the decision to perform one diagnostic test over another.
Older children and adolescents may present with an atypical presentation of solely abdominal pain due to obstruction, perforation, diverticulitis, inversion, volvulus, or intermittent intussusception. 8 , 9 These patients are more likely to undergo a CT abdomen as their initial imaging study, which has low sensitivity for identifying a Meckel's diverticulum, though it may be useful in identifying complications such as the abscess identified in Patient 1 (Figure 2). 10 Meckel's diverticulitis, an uncommon complication, usually presents like acute appendicitis and might be accompanied by enteroliths, fecaliths, or perforation as seen in acute appendicitis. 11 , 12 Complications of Meckel's diverticulum and mimicking diagnoses are listed in Table 3 (Supporting Information).
In addition, endoscopic and surgical findings may not initially reveal a Meckel's diverticulum. Two patients' small bowel VCE studies depicted ulceration and polypoid formation of the mucosa suggesting alternate diagnoses including Crohn's disease, Peutz–Jeghers syndrome, and malignancy. Limited literature exists regarding VCE findings associated with Meckel's diverticulum, though a double lumen sign (Supporting Information: Figure 3), ulcers in the lumen, polypoid structures (in diverticular mucosa or diverticular eversion), and a stenotic lumen with a circumferential ulcer have been described in patients. 7 Patient 1 initially presented with painless rectal bleeding and a positive Meckel's scan; however, when he underwent laparoscopy at an outside institution, no abnormalities were detected. Months later, repeat laparoscopy revealed a perforated Meckel's diverticulum. Of note, several of our patient's diverticula were found in atypical locations such as the mid‐jejunum rather than the mid‐ to distal ileum. As reiterated in a case series of rare, inverted Meckel's diverticula, careful exploration of the entire length of the bowel for diverticula or lead points is important to reduce the risk of missed lesions and the need for repeat surgeries. 13
Furthermore, even in patients who present with classic symptoms, diagnosis may be difficult if radiographic studies do not identify or localize a lesion. We discussed five patients with negative Meckel scans despite a history of bleeding and anemia who were found to have gastric heterotopic mucosa on surgical pathology. These cases highlight the need to identify reasons why a Meckel's scan may be falsely negative or positive (Supporting Information: Table 4). A false‐negative result may occur if there is little or inactive gastric mucosa, if the Meckel's diverticulum is necrotic or ischemic, if there is rapid clearance of the Technetium‐99m pertechnetate as observed with rapid active bleeding, or if there is poor preparation and positioning for the procedure. 14 Therefore, to optimize the aspects of the study that are within the practitioner's control, the patient should be fasting 3–4 h before the study, receive pretreatment with histamine H2‐receptor antagonists, proton pump inhibitors, pentagastrin, or glucagon, and fully void the bladder (Table 2). 14 , 17 , 18 The Meckel's scan may identify a positive area of radiotracer uptake that moves from one position to another on delayed imaging after positional changes or voiding. 15 Other less commonly recognized causes of a false‐negative Meckel's scan are performing an NM‐RBC scan too soon before the Meckel's scan and recent administration of perchlorate. 14 , 19 Known causes of false‐positive Meckel's scans include entities that cause bowel inflammation, bowel obstruction, urinary tract abnormalities, or bleeding abnormalities in the bowel. 3 , 14 , 16 , 19
Table 2.
Pretreatment, positioning, and imaging techniques for technetium‐99m pertechnetate scan in pediatric patients. 15 , 16 , 20
| Pretreatment options | |
|---|---|
| Cimetidine |
Neonates: 10–20 mg/kg/day by mouth for 2 days Infants and older children: 20 mg/kg/day by mouth for 2 days OR IV 300 mg/100 mL 5% dextrose over 20 min, scan 1 h later (must not be given with pentagastrin) |
| Ranitidine |
2 mg/kg by mouth OR 1 mg/kg IV (maximum 50 mg) over 20 min, scan 1 h later (must not be given with pentagastrin) |
| Famotidine |
*0.5 mg/kg/day by mouth twice daily 48 h before scan OR 0.5 mg/kg/day IV OR *0.25 mg/kg IV (maximum 20 mg) given over 20 min, scan 1 h later (must not be given with pentagastrin) |
| Proton pump inhibitor | Esomeprazole 10–40 mg IV, scan 30–45 min later [25]
OR *1 mg/kg (maximum 20 mg) by mouth once daily for 48 h before scan |
| Pentagastrin | 6 μg/kg subcutaneously before scan |
| Glucagon |
50 μg/kg IV (maximum 1 mg), diluted to 10 mL with sterile water, infused over 2 min immediately before scan (must be given with pentagastrin) (must not be given to patient with diabetes) |
Proper positioning:
| |
Proper Imaging technique:
| |
Abbreviations: IV, intravenous; SPECT, single‐photon emission computerized tomography.
Included in Children's Health Meckel scan protocol.
In some cases, a repeat Meckel's scan might be warranted if clinical suspicion remains high despite equivocal or negative results, and additional delayed views may be necessary. 20 Up to 58% of equivocal studies and 14% of negative studies may be positive on repeat scanning. 20 Technetium‐99m pertechnetate is taken up by the mucin‐producing foveolar cells in gastric mucosa, which are more concentrated in antral‐type mucosa than oxyntic‐type mucosa. 19 While a reasonable assumption might be that a Meckel's diverticulum with antral‐type gastric mucosa is more likely to demonstrate a positive Meckel's scan than one with oxyntic‐type gastric mucosa, this trend is not seen within our limited pool of patients. Furthermore, although the most common heterotopic mucosa found in a Meckel's diverticulum is gastric mucosa, mucosa from other less common sources such as the pancreas is not detected on a Meckel's scan.
Lastly, some pediatric patients with Meckel's diverticulum may not have a definitive diagnosis until surgical exploration. In patients with unexplained causes of obstruction, perforation, or intussusception, it is important to keep an atypical presentation of Meckel's diverticulum on the differential. Maintaining a high suspicion for Meckel's diverticulum may result in expedited surgical involvement and avoid further symptomatic episodes or complications. A limitation of our study includes a small sample size as 11 patients are not representative of all cases of Meckel's diverticulum that are difficult to diagnose or have atypical presentations. Another limitation of our study includes its retrospective nature and our inability to direct the diagnostic workup of each patient. However, a strength of our study is our patient population which is high in both volume and diversity. Furthermore, our center is a tertiary care center where we have access to multiple disciplines including surgery, pathology, and radiology. Our findings may help others at both large and smaller centers to be aware of atypical presentations for Meckel's diverticulum so that appropriate imaging and surgical involvement can be elicited early on for a prompter diagnosis and better patient outcome. Future areas of study include improving the preoperative diagnosis of symptomatic Meckel's diverticulum and further characterizing the VEC features of a Meckel's diverticulum.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
Supporting information
Supporting information.
ACKNOWLEDGMENTS
The authors report no funding for this study.
Kaihlanen K, Phen C, Sengupta A, Diesen D, Fernandes NJ, Rojas I. Meckel's diverticulum: a challenging diagnosis. JPGN Rep. 2024;5:423‐432. 10.1002/jpr3.12140
REFERENCES
- 1. Sagar J, Kumar V, Shah DK. Meckel's diverticulum: a systematic review. J R Soc Med. 2006;99(10):501‐505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kuru S, Kismet K. Meckel's diverticulum: clinical features, diagnosis and management. Rev Esp Enferm Dig. 2018;110(11):726‐732. [DOI] [PubMed] [Google Scholar]
- 3. Sinha CK, Pallewatte A, Easty M, et al. Meckel's scan in children: a review of 183 cases referred to two paediatric surgery specialist centres over 18 years. Pediatr Surg Int. 2013;29(5):511‐517. [DOI] [PubMed] [Google Scholar]
- 4. Devi GK, Goei AHY, Ragavendra K, et al. Meckel's diverticulum ‐ clinical presentation and pitfalls in diagnosis in the pediatric age group in Singapore. J Indian Assoc Pediatr Surg. 2022;27(3):340‐344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hansen CC, Søreide K. Systematic review of epidemiology, presentation, and management of Meckel's diverticulum in the 21st century. Medicine. 2018;97(35):e12154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Elsayes KM, Menias CO, Harvin HJ, Francis IR. Imaging manifestations of Meckel's diverticulum. Am J Roentgenol. 2007;189(1):81‐88. [DOI] [PubMed] [Google Scholar]
- 7. García‐Compeán D, Jiménez‐Rodríguez AR, Del Cueto‐Aguilera ÁN, Herrera‐Quiñones G, González‐González JA, Maldonado‐Garza HJ. Meckel's diverticulum diagnosis by video capsule endoscopy: a case report and review of literature. World J Clin Cases. 2018;6(14):791‐799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Schaedlich DS, Borges PCM, Lacombe A, Moron RA. Intestinal intussusception of Meckel's diverticulum, a case report and literature review of the last five years. Einstein. 2023;21:eRC0173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Keese D, Rolle U, Gfroerer S, Fiegel H. Symptomatic Meckel's diverticulum in pediatric patients‐case reports and systematic review of the literature. Front Pediatr. 2019;7:267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McDonald JS, Horst KK, Thacker PG, Thomas KB, Klinkner DB, Kolbe AB. Meckel diverticulum in the pediatric population: patient presentation and performance of imaging in prospective diagnosis. Clin Imaging. 2022;91:37‐44. [DOI] [PubMed] [Google Scholar]
- 11. Malik A, Shams‐ul‐Bari S, Wani K, Khaja A. Meckel's diverticulum‐revisited. Saudi J Gastroenterol. 2010;16(1):3‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Aamery A, Al‐Shehhi R, Malik K, Al‐Harthy A. Perforation of Meckel's diverticulum with a foreign body mimicking acute appendicitis: a rare complication. J Pak Med Assoc. 2017;67(6):942‐944. [PubMed] [Google Scholar]
- 13. Tang XB, Wang X, Ma Y, Bai YZ. Radiological and clinical characteristics of intussuscepted, inverting, and inverted Meckel's diverticulum: a case series. Eur J Radiol. 2022;157:110611. [DOI] [PubMed] [Google Scholar]
- 14. Aboughalia HA, Cheeney SHE, Elojeimy S, Blacklock LC, Parisi MT. Meckel diverticulum scintigraphy: technique, findings and diagnostic pitfalls. Pediatr Radiol. 2023;53(3):493‐508. [DOI] [PubMed] [Google Scholar]
- 15. Chang WT, LaBuda CS, Brown JM, Nakamura KM. Delayed imaging of Meckel's diverticulum: observation of a quadrantal shift. Clin Nucl Med. 2009;34(1):50‐52. [DOI] [PubMed] [Google Scholar]
- 16. Blackmon KN, Rao AG. Ectopic kidney mimicking a Meckel's diverticulum on Tc‐99m pertechnetate scan. Clin Nucl Med. 2011;36(12):e228‐e230. [DOI] [PubMed] [Google Scholar]
- 17. Shammas A, Vali R, Charron M. Pediatric nuclear medicine in acute care. Semin Nucl Med. 2013;43(2):139‐156. [DOI] [PubMed] [Google Scholar]
- 18. Ververs TF, Lobbezoo AFH, Hobbelink MG, Braat AJ. Patient preparation with esomeprazole is comparable to ranitidine in meckel diverticulum scintigraphy. J Nucl Med Technol. 2023;51(3):211‐214. [DOI] [PubMed] [Google Scholar]
- 19. Spottswood SE, Pfluger T, Bartold SP, et al. SNMMI and EANM practice guideline for meckel diverticulum scintigraphy 2.0. J Nucl Med Technol. 2014;42(3):163‐169. [DOI] [PubMed] [Google Scholar]
- 20. Vali R, Daneman A, McQuattie S, Shammas A. The value of repeat scintigraphy in patients with a high clinical suspicion for Meckel diverticulum after a negative or equivocal first Meckel scan. Pediatr Radiol. 2015;45(10):1506‐1514. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.


