Abstract
Background:
Peripheral nerve injuries (PNI) range from mild neurapraxia to severe transection, leading to significant morbidity. Despite their impact, the societal implications of PNI in the United States are not well understood. This study aims to systematically review the literature on PNI epidemiology in the United States. We hypothesize that this review will reveal significant gaps in the understanding of PNI incidence, demographics, and economic impact.
Methods:
Following Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines, we queried the literature for studies on PNI that reported at least one of the following: incidence rates, demographics, affected nerve distribution, injury mechanisms, surgical intervention rates, and associated direct costs. Exclusion criteria included non-English publications, abstracts, conference proceedings, reviews, or editorials, studies published before 2000, non-US studies, or studies focusing solely on digital nerves or plexus injuries.
Results:
Fifteen studies met the inclusion criteria. Data indicate a higher incidence of upper extremity nerve injuries compared with lower extremity injuries. The literature lacks comprehensive reporting on surgical intervention rates, with no recent data since 2013. There is a notable absence of nationwide epidemiological data on PNI mechanisms and recent cost data, with most information over a decade old and primarily focused on inpatient costs, neglecting outpatient visits, physical therapy, and medication expenses.
Conclusion:
The epidemiological data on PNI are limited and outdated, highlighting the need for further research. Future studies should focus on recent trends in PNI incidence, injury mechanisms, and financial burden, including comprehensive reporting on surgical interventions, to inform strategies aimed at improving patient outcomes and health care resource allocation.
Keywords: peripheral nerve injury, incidence, direct cost, epidemiology
Introduction
Peripheral nerve injuries (PNI) present across a spectrum of severity and can result in considerable morbidity. 1 Less severe PNI may resolve in the initial 3 to 6 months after injury; however, some patients may show no improvement in that time frame and may be candidates for operative intervention.2 -5 The optimal treatment strategy is determined by the injury severity, patient-specific factors, and the reasonable anticipated outcomes.3,6 -8 The literature on PNI mechanisms is focused mostly on countries outside of the United States, with an unknown generalizability. 9 The demographic makeup of individuals affected by PNI within the United States remains inadequately characterized, as limited studies have examined the distribution across different age groups, genders, and racial or ethnic backgrounds.10 -12 This deficiency of demographic data impedes our ability to mitigate the burden of PNI in vulnerable populations. In addition, the economic ramifications of PNI in the United States are not well understood, limiting the ability to perform comprehensive cost-effectiveness analyses and to inform resource allocation.
Despite the potentially devastating effects of PNI, their epidemiology and burden on the health care system in the United States remain poorly studied. As such, the purpose of this study is to systematically review the literature on PNI epidemiology in the United States focusing specifically on incidence, rate of surgical intervention, mechanisms, and patient characteristics such as age, race, and gender. We hypothesize that a comprehensive analysis of the available literature will reveal significant limitations in the understanding of the epidemiology, management, and financial burden of PNI in the United States.
Methods
Information Sources
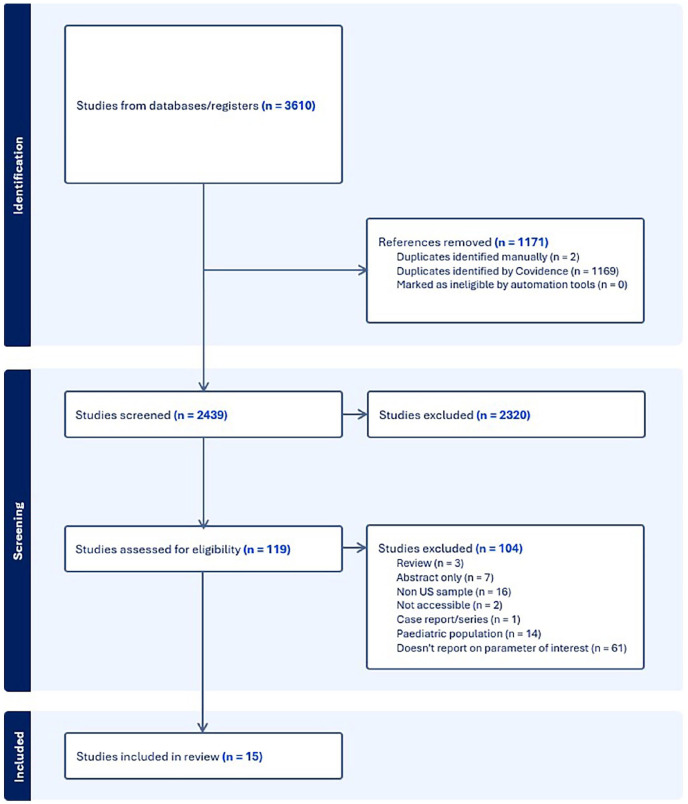
With the expertise and assistance of a medical librarian, we searched the literature for records that included PNI in the United States and included at least one of our variables of interest. Embase, Ovid MEDLINE, Clinicaltrials.gov, Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, and Scopus databases were queried from database inception to 2024. The initial search strategy was date limited to 2000 to 2024, to capture recent epidemiological studies, and resulted in a total of 3610 articles identified. A total of 1171 duplicate records were deleted resulting in a total of 2439 unique citations included in the project library. Fully reproducible search strategies for each database can be found in the Supplemental Material.
Eligibility Criteria
Studies eligible for inclusion examined PNI and reported on at least one of the following variables of interest: incidence rates, demographics (age, gender, race), affected nerve distribution, injury mechanisms, surgical intervention rates for PNI, and associated direct costs. Studies were excluded if they: (1) were non-English, abstracts, conference proceedings, letters, perspective pieces, reviews, or editorials; (2) were published before 2000; (3) were not conducted in the United States; or (4) reported entirely on digital nerves or brachial plexus injuries without examining other peripheral nerves. These injuries were excluded to minimize heterogeneity in the data collected, as both digital nerve injuries and brachial plexus injuries have greater variability in both their management and financial burden relative to mixed and motor peripheral nerves.
Selection Process
Two authors independently screened and reviewed the full texts of the returned studies, applying the above inclusion and exclusion criteria. Any disagreements between the 2 authors were resolved by a third author; no disagreements were encountered. A kappa coefficient was calculated to assess interrater reliability agreement on inclusion. Two authors then worked independently, to group, review, and extract data from each study.
Data Extraction and Synthesis
For each study, data on incidence, incidence surgically treated, demographics including age, gender, race, specific nerve distribution, mechanism, and direct cost of PNI were extracted and reported with descriptive statistics where applicable.
Results
Study Selection
From the database searches, a total of 2439 unique citations were returned. Of these, the authors selected 119 abstracts for full text review. On independently reviewing the full texts of the 119 studies, the 2 reviewers attained a Cohen kappa demonstrating “moderate” initial agreement (k = 0.57). After deliberation between the authors, 100% agreement was obtained on inclusion/exclusion, and 15 studies were included for analysis (Figure 1). The 15 studies can be found delineated in the Supplemental Table (Table S1).
Figure 1.
PRISMA flow diagram for study inclusion.
Demographics
In a study using administrative data from 2001 to 2013, lower extremity (LE) PNI (LE PNI) affected individuals with a mean age of 41.6 years. 10 Among these individuals, 61% were men and 39% were women. 10 The racial distribution of LE PNI during this period was as follows: 66.6% non-Hispanic white, 11.3% Hispanic white, 16.7% black, 0.9% Native American, 1.6% Asian/Pacific Islander, and 3% other. 10 During the same time period, another administrative dataset study showed that upper extremity (UE) PNI (UE PNI) also exhibited a male predominance, with 74.3% men and 25.7% women. 11 The racial distribution of UE PNI was as follows: 49% non-Hispanic white, 12.5% black, 0.8% Native American, 1.5% Asian/Pacific Islander, and 29% other. 11 Tapp et al reported a mean age of 38.4 years among individuals with diagnoses of UE PNI in the emergency department, with a majority being men (68.2%). 13 Another study analyzed PNI data from a single institution reporting a mean age of 35.9 years, with 57% being men and 43% women. 14 A study examining PNI resulting from athletic activities from 2009 to 2018 reported a mean age of 39.5, with 59.6% male and 41.4% female participants. 15 The racial distribution included 49.5% non-Hispanic white, 11.2% black, 4.8% Hispanic, and 34.7% other. 15
Bellaire et al 12 used the State Ambulatory Surgery and Services Databases (SASD) between 2006 and 2011 and reported a mean age of 37.6 years among individuals undergoing PNI surgical interventions, with 79.4% men and 20.6% women. The racial demographics of their cohort were: 66.4% non-Hispanic white, 20.2% Hispanic, 0.3% African American, 6.3% Asian/Pacific Islander, and 6.8% categorized as Other. 12 Adidharma et al, 16 using data from the Merative MarketScan Commercial and Medicare Databases between 2015 and 2020, reported demographics on 4331 patients who underwent nerve gap reconstruction or primary nerve repair, with 52.2% being women and 47.8% men (Table 1).
Table 1.
Peripheral Nerve Injury Study Demographics.
| Author | Year published | Study type | Database used | Year(s) database used | Age (mean ± SD) | Male, % | Female, % | White non-Hispanic, % | Hispanic, % | Black, % | Native American, No. (%) | Asian/Pacific Islander, No. (%) | Other, % |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Foster et al | 2019 | Administrative | NIS (UE PNI) | 2001-2013 | 41.6 (±0.1) | 61 | 39 | 66.6 | NA | 16.7 | 0.9 | 1.6 | 3 |
| Karsey et al | 2019 | Administrative | NIS (LE PNI) | 2001-2013 | 38.01 (±0.05) | 74.3 | 25.7 | 49 | NA | 12.5 | 0.8 | 1.5 | 29 |
| Li et al | 2020 | Administrative | NEISS (sports/recreational etiology only) | 2009-2018 | 39.5 (±17.4) | 59.6 | 41.4 | 49.5 | 4.8 | 11.2 | NA | NA | 34.7 |
| Tapp et al | 2019 | Administrative | Nationwide emergency department sample database | 2014 | 38.4 (±0.5) | 68.2 | 31.8 | NA | NA | NA | NA | NA | NA |
| Bellaire et al | 2021 | Administrative | SASD a | 2006-2011 | 37.6 (±16.5) | 79.4 | 20.6 | 66.4 | 20.2 | NA | NA | 6.3 | 6.8 |
| Adidharma et al | 2024 | Administrative | MarketScan Commercial and Medicare Databases a | 2015-2020 | NA | 47.8 | 52.2 | NA | NA | NA | NA | NA | NA |
| Azad et al | 2023 | Retrospective cohort study | Single institution | NA | 35.9 | 57 | 43 | NA | NA | NA | NA | NA | NA |
Note. NIS = Nationwide Inpatient Sample; NEISS = National Electronic Injury Surveillance System; SASD = State Ambulatory Surgery and Services Databases; UE PNI = upper extremity peripheral nerve injury; LE PNI = lower extremity peripheral nerve injury; SD = standard deviation; NA = not applicable.
Reporting only on patients treated surgically.
Three studies reported on basic demographics of individuals with PNI after gunshot wounds (GSW), all reporting mean ages between 23 and 34, with 88% to 96% being men and 4% to 12% women.17 -19
Incidence
A pair of studies examined the incidence of PNI using the Nationwide Inpatient Sample (NIS) database.10,11 They examined data from 2001 to 2013 with 101 000 000 available individuals included and reported a mean annual incidence of 13.6:1 000 000 for LE PNI and 43.8:1 000 000 for UE PNI.10,11 A study evaluating PNI caused by sports, exercise, or recreational activities from 2009 to 2018, using the National Electronic Injury Surveillance System, found that there were 120 675 PNI during that time period that were involving athletic activities. 15 The overall incidence of PNI within 90 days of trauma was reported as 1.64% based on data drawn from the MEDSTAT database covering the year 1998. 20 A study using IBM MarketScan Commercial Database years from 2010 to 2015 provided cumulative incidence rates of 2.3% and 1.3% at 2 years and 90 days post-trauma. 21 Tapp et al 13 used the Nationwide Emergency Department Sample database year 2014 data to report an incidence rate of 0.33% of UE PNI among patients presenting to emergency departments with UE injuries.
Surgical Intervention
For UE PNI, a study using the NIS database from 2001 to 2013 reported that 33.6% of UE PNI were linked with the Current Procedural Terminology (CPT) code for suturing of peripheral nerve and 6.7% were linked with the CPT code for other neuroplasty. 11 For LE PNI, a study using the NIS database from 2001 to 2013 reported that 5.8% of PNI were linked with the CPT code for suturing of peripheral nerve. 10 Donnally et al 22 reported 19 cases of UE machete PNI treated operatively out of 48 total machete injuries, indicating a peripheral nerve surgical intervention incidence of 39.6% in UE machete injuries.
Nerve Distribution
For UE PNI from 2001 to 2013, as reported in a study using the NIS database, the distribution by nerve affected was as follows: 15.1% radial nerve, 17.8% ulnar nerve, 13% median nerve, 13% axillary nerve, 18% digital nerves, and 25.6% other. 11 In LE PNI, during the same period again using the NIS database, the distribution by nerve affected was 33.4% peroneal nerve, 6% tibial nerve, 16.6% sciatic nerve, 10.7% femoral nerve, and 32% other nerves. 10 Padovano et al, 21 using the IBM MarketScan Commercial Database spanning 2010 to 2015, delineated nerve involvement post-extremity trauma, with a UE PNI incidence at 86.5% and LE at 13.5%. They reported the incidence of each specific nerve: 6.7% radial, 13.6% ulnar, 37.5% median, 1% axillary, 22.6% digital, 2.4% peroneal, 0.6% femoral, 1.30% sciatic, and 14.3% other. 21 In emergency department trauma patients with UE PNI, the affected nerve distribution reported was: 30.3% ulnar nerve, 23.2% digital nerves, 22.8% radial nerve, 15.8% median nerve, 5.2% other nerves, 1.5% axillary nerve, 0.5% musculocutaneous nerve, and 0.7% multiple nerve injuries. 13 Over a 14-year interval from 1993 to 2006, the average annual discharges for PNI were 2963 for the median nerve, 3981 for the ulnar nerve, and 2954 for the radial nerve. 23
In a single institution retrospective study focusing on UE PNI resulting from machete injuries, it was found that the digital nerves were involved in approximately 58% of individuals, whereas the ulnar nerve was affected in 5%, the median nerve in 10%, and the radial nerve in 27%. 22 For individuals with GSW, Fagan et al, 18 using a retrospective cohort from a single institution, reported the injured nerves as follows: 25% median, 15% ulnar, 15% radial, 35% sciatic, 5% peroneal, and 5% tibial. This compares with Pannell et al 17 who reported involvement of the radial nerve in 34.9%, ulnar nerve in 30.2%, and median nerve in 20.9% among individuals with UE GSW (Table 2).
Table 2.
Affected Nerve Distribution.
| Author | Year published | Study type | Database used | Years database used | Radial nerve, % | Ulnar nerve, % | Median nerve, % | Axillary nerve, % | Digital nerves, % | Peroneal nerve, % | Tibial nerve, % | Femoral nerve, % | Sciatic nerve, % | Other, % |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Foster et al | 2019 | Administrative | NIS | 2001-2013 | 15.1 | 17.8 | 13 | 13 | 18 | NA | NA | NA | NA | 25.6 |
| Karsey et al | 2019 | Administrative | NIS | 2001-2013 | NA | NA | NA | NA | NA | 33.4 | 6 | 10.7 | 16.6 | 32 |
| Padovano et al | 2022 | Administrative | IBM MarketScan Commercial | 2010-2015 | 6.7 | 13.6 | 37.5 | 1 | 22.6 | 2.4 | NA | 0.6 | 1.3 | 14.3 |
| Donnally et al | 2017 | Retrospective Review of Machete Injuries | Single Institution | 2008-2016 | 22.8 | 30.3 | 15.8 | 1.5 | 23.2 | NA | NA | NA | NA | 5.2 |
| Fagan et al | 2024 | Retrospective Cohort of GSW | Single Institution | 2018-2023 | 15 | 15 | 25 | NA | NA | 5 | 5 | 35 | NA | NA |
| Pannell et al | 2017 | Retrospective Cohort of GSW | Single Institution | 2007-2015 | 34.9 | 30.2 | 20.9 | NA | NA | NA | NA | NA | NA | 14 |
Note. NIS = Nationwide Inpatient Sample; IBM = International Business Machines Corporation; GSW = gunshot wound; NA = not applicable.
Injury Mechanisms
Although available studies focus on specific mechanisms such as trauma, sports, or GSW, no available studies in the United States report on holistic nationwide epidemiological data regarding the burden of various mechanisms of PNI on its overall incidence. Known mechanisms of PNI include iatrogenic, trauma (blunt, GSW, penetrating), motor vehicle collisions (MVC), falls, workplace accidents, and sports or recreation. However, the available literature does not specify the individual contribution of the major drivers of PNI in the United States.
Direct Costs
Between 1993 and 2006, Lad et al, 23 using the NIS database, reported a significant rise in hospital charges for median, ulnar, and radial nerve injuries, with costs increasing as follows: median from $9257 to $27 962, ulnar from $10 563 to $25 311, and radial from $9884 to $18 666. Costs continue to trend upward with 2 studies, using the NIS database, reporting on inpatient direct cost for PNI from 2001 to 2013, with $64 031 ± $421 for LE PNI and $47 004 ± $185 for UE PNI.10,11 One study reported a mean direct cost of $5779 for emergency department visits for UE nerve injuries in 2014 using the Nationwide Emergency Department Sample database. 13 Bellaire et al, 12 using the SASD database accessed from 2006 to 2011, reported mean direct costs associated with surgical interventions for PNI, including direct repair ($14 976), nerve grafts ($19 968), synthetic conduits ($19 043), and vein conduits ($25 324).
Discussion
The incidence of PNI as reported in data from over a decade ago was found to be 13.6 people per 1 000 000 for LE PNI and 43.8 people per 1 000 000 for UE PNI.10,11 The frequency of PNI diagnosed after traumatic injuries is reported to be 0.33% at initial ED visit, 1.3% to 1.6% within the first 90 days post-trauma, and 2.3% within 2 years post-trauma.13,20,21 However, due to the nature of PNI, it is challenging to precisely estimate its true incidence, especially for those treated nonoperatively, as many cases are not diagnosed at the initial presentation. For those treated surgically, updated data are necessary to better reflect the current epidemiologic burden of PNI. For context, other conditions such as spinal cord injury and distal radius fractures have better-characterized incidence rates. Spinal cord injury, for instance, has an estimated incidence of around 54 cases per 1 000 000 people annually, whereas distal radius fractures are among the most common fractures, particularly in children or older adults, with an incidence of 2280 people per 1 000 000 in an adult population.24 -26 Although PNI appears to be less common, it is crucial to have a better understanding of its epidemiologic burden to advocate for appropriate clinical and research resources.
The available studies show that the majority of PNI occurs in men and the racial/ethnic distribution does not vary substantially from the national population. This may be explained by men working in higher risk occupations or engaging in riskier activities. The mean age of all patients with PNI was consistently in the late fourth to early fifth decade; however, this appears to be dependent on the mechanism. Three studies found the mean age of PNI following GSW to be between 23 and 34 years, which follows the data on overall GSW which tends to skew toward younger adults.17 -19 Unfortunately, there is a lack of detailed data reported on the individual contributions of each mechanism of PNI. Some studies focus on a specific mechanism such as MVC, GSW, or sports injuries; however, the contribution of each mechanism to the overall PNI incidence has been unstudied in the United States. Future research aimed at assessing the frequency of various injury mechanisms holds significant importance. Such endeavors can provide valuable insights into how each mechanism impacts injury severity. Understanding the associated effects of these mechanisms on subsequent PNI can play a crucial role in injury triage and the development of risk reduction strategies.
In our systematic review, more than one-third of UE PNIs were treated surgically, but less than 10% of LE PNIs underwent surgery.10,11 These data, however, may not accurately represent current trends for a number of reasons. First, the examined International Classification of Diseases codes may not capture the range of surgical options and often fail to differentiate between treatments. In addition, we did not find any large-scale studies on the incidence of surgical treatment of PNI with data from the last 10 years, so any recent trends are not recognized. One interesting finding regarding surgical decision-making was Adidharma et al, 16 who found that the gender distribution among patients undergoing surgery for PNI was near 1:1, despite the incidence of PNI being consistently reported as majority male.
Overall cost of PNI has greatly increased in recent decades. In the mid-1990s, mean hospital charges for UE PNI were around $10 000, but recent studies found mean hospital charges to be 2 to 3 times greater.10,11,23 Other studies found inpatient direct costs could be greater than $50 000, whereas direct cost of surgery alone ranged from $15 000 to $20 000, and direct cost of ED visits was around $5000.12,13 These costs are perhaps a reflection of rising health care costs in general but may also be a result of increased treatment options and a trend toward early treatment of PNI. These costs are also likely not representative of the present day or do they consider the full cost associated with a PNI; the most recent data regarding cost are from over a decade ago and many of these costs only reflect direct inpatient and surgical cost. These data fail to capture cost of outpatient visits and rehabilitation or inability to work. As these are also major costs and stressors for patients with PNI, future studies should more accurately describe all aspects of costs related to PNI.
Conclusion
Based on the published literature, the incidence of PSNI in the United States is somewhat variable but occurs in a small proportion of traumatic accidents and typically in the upper extremities and in men. Data on the rate and types of surgical intervention of PNI demonstrate that a minority of PNI are treated surgically; however, current data are limited and outdated. The financial burden of PNI has risen over the past few decades, though capturing the true impact is limited by the narrow scope of available studies. The currently available epidemiologic and economic data regarding PNI are outdated, demonstrating a clear need for more thorough investigation of current incidence, surgical options and trends, and true burden of PNI.
Supplemental Material
Supplemental material, sj-docx-1-han-10.1177_15589447241299050 for Insights Into the Epidemiology of Peripheral Nerve Injuries in the United States: Systematic Review by Zachary D. Randall, Brendan J. Navarro, David M. Brogan and Christopher J. Dy in HAND
Footnotes
Ethical Approval: This study did not involve human or animal subjects, and no ethical approval was required.
Statement of Human and Animal Rights: This study conformed to all human and animal rights laws.
Statement of Informed Consent: No informed consent was required for this study, as it did not involve any identifiable human subjects or personal data.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: ZDR and BJN do not have any potential conflicts of interest with respect to this manuscript. CJD and DMB report the following potential conflict of interest: Research funding from the National Institutes of Health, the Department of Defense and American Foundation for Surgery of the Hand; research funding and speaker fees from Checkpoint Surgical and both are on the Medical Advisory Board of OrthoCell.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Zachary D. Randall  https://orcid.org/0000-0002-3820-5787
https://orcid.org/0000-0002-3820-5787
David M. Brogan  https://orcid.org/0000-0001-6259-4885
https://orcid.org/0000-0001-6259-4885
Christopher J. Dy  https://orcid.org/0000-0003-1422-2483
https://orcid.org/0000-0003-1422-2483
Supplemental material is available in the online version of the article.
References
- 1. Lopes B, Sousa P, Alvites R, et al. Peripheral nerve injury treatments and advances: one health perspective. Int J Mol Sci. 2022;23(2):918. doi: 10.3390/ijms23020918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bhandari PS. Management of peripheral nerve injury. J Clin Orthop Trauma. 2019;10(5):862-866. doi: 10.1016/j.jcot.2019.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dahlin LB, Wiberg M. Nerve injuries of the upper extremity and hand. EFORT Open Rev. 2017;2(5):158-170. doi: 10.1302/2058-5241.2.160071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ljungquist KL, Martineau P, Allan C. Radial nerve injuries. J Hand Surg Am. 2015;40(1):166-172. doi: 10.1016/j.jhsa.2014.05.010 [DOI] [PubMed] [Google Scholar]
- 5. Gordon T, English AW. Strategies to promote peripheral nerve regeneration: electrical stimulation and/or exercise. Eur J Neurosci. 2016;43(3):336-350. doi: 10.1111/ejn.13005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Grinsell D, Keating CP. Peripheral nerve reconstruction after injury: a review of clinical and experimental therapies. Biomed Res Int. 2014;2014:698256-698213. doi: 10.1155/2014/698256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chimutengwende-Gordon M, Khan W. Recent advances and developments in neural repair and regeneration for hand surgery. Open Orthop J. 2012;6:103-107. doi: 10.2174/1874325001206010103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lee SK, Wolfe SW. Peripheral nerve injury and repair. J Am Acad Orthop Surg. 2000;8(4):243-252. doi: 10.5435/00124635-200007000-00005 [DOI] [PubMed] [Google Scholar]
- 9. Aman M, Zimmermann KS, Thielen M, et al. An epidemiological and etiological analysis of 5026 peripheral nerve lesions from a European Level I Trauma Center. J Pers Med. 2022;12(10):1673. doi: 10.3390/jpm12101673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Foster CH, Karsy M, Jensen MR, et al. Trends and cost-analysis of lower extremity nerve injury using the national inpatient sample. Neurosurgery. 2019;85(2):250-256. doi: 10.1093/neuros/nyy265 [DOI] [PubMed] [Google Scholar]
- 11. Karsy M, Watkins R, Jensen MR, et al. Trends and cost analysis of upper extremity nerve injury using the national (nationwide) inpatient sample. World Neurosurg. 2019;123:e488-e500. doi: 10.1016/j.wneu.2018.11.192 [DOI] [PubMed] [Google Scholar]
- 12. Bellaire CP, Inglesby DC, Marayati NF, et al. Trends in peripheral nerve epidemiology and reconstruction: a state database study of direct repairs, grafts, and conduits. Ann Plast Surg. 2021;87(2):179-186. doi: 10.1097/SAP.0000000000002823 [DOI] [PubMed] [Google Scholar]
- 13. Tapp M, Wenzinger E, Tarabishy S, et al. The epidemiology of upper extremity nerve injuries and associated cost in the US emergency departments. Ann Plast Surg. 2019;83(6):676-680. doi: 10.1097/SAP.0000000000002083 [DOI] [PubMed] [Google Scholar]
- 14. Azad A, Birnbaum A, Roller R, et al. The effect of surgical timing on upper extremity nerve repair. Hand. Published online September 14, 2023. doi: 10.1177/15589447231198125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Li NY, Onor GI, Lemme NJ, et al. Epidemiology of peripheral nerve injuries in sports, exercise, and recreation in the United States, 2009 – 2018. Phys Sportsmed. 2021;49(3):355-362. doi: 10.1080/00913847.2020.1850151 [DOI] [PubMed] [Google Scholar]
- 16. Adidharma W, Wang Y, Kotsis SV, et al. Utilization trends of nerve autograft alternatives for the reconstruction of peripheral nerve defects. Plast Reconstr Surg. 2024;153(4):863-872. doi: 10.1097/PRS.0000000000011153 [DOI] [PubMed] [Google Scholar]
- 17. Pannell WC, Heckmann N, Alluri RK, et al. Predictors of nerve injury after gunshot wounds to the upper extremity. Hand. 2017;12(5):501-506. doi: 10.1177/1558944716675294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fagan P, Geiger CD, Chenji G, et al. Neuromuscular ultrasound findings in gunshot wounds. Muscle Nerve. 2024;69(4):416-421. doi: 10.1002/mus.28048 [DOI] [PubMed] [Google Scholar]
- 19. Bercik MJ, Kingsbery J, Ilyas AM. Peripheral nerve injuries following gunshot fracture of the humerus. Orthopedics. 2012;35(3):e349-e352. doi: 10.3928/01477447-20120222-18 [DOI] [PubMed] [Google Scholar]
- 20. Taylor CA, Braza D, Rice JB, et al. The incidence of periph-eral nerve injury in extremity trauma. Am J Phys Med Rehabil. 2008;87(5):381-385. doi: 10.1097/PHM.0b013e31815e6370 [DOI] [PubMed] [Google Scholar]
- 21. Padovano WM, Dengler J, Patterson MM, et al. Incidence of nerve injury after extremity trauma in the United States. Hand. 2022;17(4):615-623. doi: 10.1177/1558944720963895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Donnally CJ, 3rd, Hannay W, Rapp DA, et al. Machete injuries to the upper extremity. Arch Orthop Trauma Surg. 2017;137(12):1615-1621. doi: 10.1007/s00402-017-2783-y [DOI] [PubMed] [Google Scholar]
- 23. Lad SP, Nathan JK, Schubert RD, et al. Trends in median, ulnar, radial, and brachioplexus nerve injuries in the United States. Neurosurgery. 2010;66(5):953-960. doi: 10.1227/01.neu.0000368545.83463.91 [DOI] [PubMed] [Google Scholar]
- 24. National Spinal Cord Injury Statistical Center, Traumatic Spinal Cord Injury Facts and Figures at a Glance. University of Alabama at Birmingham; 2024. [Google Scholar]
- 25. Jain NB, Ayers GD, Peterson EN, et al. Traumatic spinal cord injury in the United States, 1993-2012. JAMA. 2015;313(22):2236-2243. doi: 10.1001/jama.2015.6250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Viberg B, Tofte S, Rønnegaard AB, et al. Changes in the incidence and treatment of distal radius fractures in adults—a 22-year nationwide register study of 276,145 fractures. Injury. 2023;54(7):110802. doi: 10.1016/j.injury.2023.05.033 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-han-10.1177_15589447241299050 for Insights Into the Epidemiology of Peripheral Nerve Injuries in the United States: Systematic Review by Zachary D. Randall, Brendan J. Navarro, David M. Brogan and Christopher J. Dy in HAND