Abstract
Objective
To assess and compare changes in the dimension and position of the mandibular condyle after tooth-borne (Hyrax) and tooth-bone-borne (Hybrid Hyrax) expansion.
Methods
Twenty-five patients who underwent expansion with either tooth-borne appliances (8 girls, 5 boys; mean age 14.3 ± 2.3 years) or tooth-bone-borne appliances (6 girls, 6 boys; mean age 13.8 ± 2.2 years) were examined. Condylar and glenoid fossa morphology before (T0) and 3 months after (T1) expansion were evaluated using cone-beam computed tomography. Condylar measurements (anterior, posterior, and superior joint spaces; condylar height, length, and width), along with sagittal and vertical skeletal and maxillary transversal measurements, were analyzed using Dolphin Imaging software. Wilcoxon and Paired t tests were used for T0 and T1 evaluations, and the Mann–Whitney U test for intergroup comparisons.
Results
At both T0 and T1, no statistically significant differences were observed between the groups in terms of condylar dimensions or the position of the condyle within the glenoid fossa. Maxillary transversal measurements increased after expansion in both groups (P < 0.01), with a significantly greater increase in first premolar width in the Hyrax group (P < 0.05). The vertical position of the posterior teeth showed no noteworthy changes (P > 0.05), except for the right second premolar. Temporomandibular joint measurements did not significantly change in either group after treatment (P > 0.05).
Conclusions
Neither tooth-borne nor tooth-bone-borne expansion caused significant changes in the condylar dimensions and position at the end of treatment.
Keywords: Temporomandibular joint, Expansion, Appliances, Computed tomography
INTRODUCTION
Rapid maxillary expansion (RME) is frequently used to address transverse maxillary deficiency and correct crowding and posterior crossbites.1,2 The most common RME appliance, a tooth-anchored expander, is bonded to the maxillary premolars and molars, with or without an acrylic plate. However, conventional RME appliances, such as banded Hyrax and acrylic cap splints, may lead to undesirable outcomes like root resorption, dentoalveolar tipping, and detrimental periodontal effects, such as alveolar bone dehiscence.2-4 To mitigate these side effects, overcome dental anchorage limitations, and enhance the skeletal effects of RME, clinicians have adopted bone-anchored expanders, which are attached to the palatal bone using mini-implants, including bone-borne and tooth-bone-borne expanders.2,3
RME induces notable skeletal, dental, and alveolar changes.1,2,5,6 In addition to skeletal and dentoalveolar effects, researchers have investigated its potential impact on temporomandibular structures, though findings are inconsistent. Some studies indicate no significant changes in condylar position following maxillary expansion,7-9 while others report displacement of the condyles.7,10,11 RME has been associated with changes in condylar position measurements in patients with unilateral posterior crossbite.10-14
Several explanations for condylar positional and morphological changes following maxillary expansion exist. Some studies suggest that in mixed dentition patients with functional posterior crossbite, condyles may become symmetrical after expansion due to the mandible’s regained freedom of movement from tooth movements during expansion.15 Others have observed significant condylar remodeling 18 weeks post-expansion.16 Another explanation, proposed by Ghoussoub et al.,17 suggests that RME may affect structures on the temporal bone, far from the activation region, thus, the relationship with the mandibular condyle may be affected.
According to another hypothesis, along with maxillary suture changes, the association between maxillary expansion and mandibular changes, such as increased width and rotation, may influence the spatial position of the condyle.10 However, the RME’s direct impact on condylar position and its precise mechanism has not yet been fully proven. One prominent hypothesis is that dental tipping during expansion causes premature contact in the mandibular posterior region, potentially exerting additional stress on the condyle, leading to mandibular backward rotation and impacting the glenoid fossa.7 Different types of expansion appliances may produce varying degrees of dental and alveolar tipping depending on the anchorage unit, either dental or skeletal.18 Given that these “appliance-induced” inclinations or vertical dental differences in the posterior teeth may cause premature contact, this study was designed.
To the best of our knowledge, no studies have examined the effects of tooth-borne (Hyrax) and tooth-bone-borne (Hybrid Hyrax) expansion appliances on the condyle. Based on this information, this study aimed to evaluate and compare the changes in the dimension and position of the mandibular condyle following tooth-borne and tooth-bone-borne expansion. The null hypothesis of this study is that tooth-borne and tooth-bone-borne expansion do not cause significant changes in the dimension or position of the mandibular condyle.
MATERIALS AND METHODS
This clinical retrospective study was conducted on participants who (1) had maxillary constriction and unilateral or bilateral posterior crossbite without functional shift, (2) had not undergone previous orthodontic treatment, (3) did not have any systemic or genetic diseases, and (4) had completed permanent dentition. Approval for this study was granted by the institutional review board of Yeditepe University, Istanbul, Turkey (approval date and number: 10.03.2023 and E.83321821-805.02.03-169), and both participants and their parents provided written informed consent.
Out of 51 patients with maxillary constriction referred to the orthodontic clinic at Yeditepe University over a two-year period, 26 patients who met the inclusion criteria and consented to participate were consecutively enrolled in the study. Following the order of referral, with a randomization ratio of 1:1, an orthodontist (DGC), who was unaware of the treatment assignments for subsequent patients, randomly assigned them to two groups. One patient, who lost the palatal miniscrews two days after the expander was inserted due to eating hard foods, was excluded from the study.
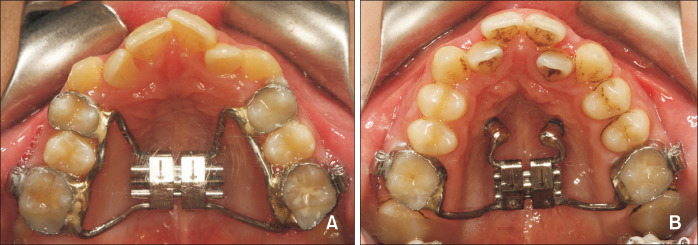
The records of 25 patients who underwent expansion with Hyrax (Figure 1A) or Hybrid Hyrax appliances (Figure 1B) were evaluated. The Hyrax group comprised 13 patients (eight girls and five boys; average age 14.3 ± 2.3 years), while the Hybrid Hyrax group included 12 patients (six girls and six boys; average age 13.8 ± 2.2 years). A comparison of age at T0, activation time, and sex distribution between groups is given in Table 1. Measurements of condyle and glenoid fossa dimensions were conducted using cone-beam computed tomography (CBCT) scans taken before (T0) and 3 months after (T1) the expansion procedure. CBCT scans were acquired with an Iluma device (IMTEC [3M], Ardmore, Ok, USA) with the following parameters: 3.8 mA, 120 kV, an exposure time of 40 seconds, a voxel size of 0.2 mm, an axial slice thickness of 0.3 mm, and a scanning area measuring 20 × 25 cm.
Figure 1.
A, Tooth-borne Hyrax expansion appliance. B, Tooth-bone-borne Hybrid Hyrax expansion appliance.
Table 1.
Comparison of age at T0, activation time, and sex distribution between groups
| Hyrax | Hybrid Hyrax | P value | |
|---|---|---|---|
| Age (yr) at T0 | 14.3 ± 2.3 | 13.8 ± 2.2 | 0.6* |
| Activation time (day) | 19.2 ± 4.5 | 20.2 ± 3.0 | 0.5* |
| Female/Male | 8 (61.5)/5 (38.5) | 6 (50.0)/6 (50.0) | 0.6† |
Values are presented as mean ± standard deviation or number (%).
*P values for 2 independent-sample t test, †P value for the fisher exact test.
For tooth-bone-borne appliances, two miniscrews (Diameter: 1.8 mm/Length: 9 mm) (Total Anchor; Trimed, Ankara, Türkiye) were placed in 1 mm predrilled areas with a piezosurgery device, close to the midpalatal suture in the 2nd and 3rd rugae at the level of the first premolars, under local anesthesia. Silicone impressions were taken with transfer caps. One week after miniscrew placement, the appliances were applied to the maxillary first molars using bands and to the miniscrews using the caps (TTA S-cap; Trimed) secured in place with glass ionomer cement (Multi-cure glass ionomer band cement; 3M Unitek, Monrovia, CA, USA). In all patients, the expansion screw was rotated a quarter-turn twice daily. In both groups, after expansion, a split was clinically observed in the midpalatal suture. The expansion procedure was applied as described in Gunyuz Toklu et al.’s study.18 The activation period was approximately 19.2 ± 4.5 days for the Hyrax group and 20.2 ± 3.0 days for the Hybrid Hyrax group. During retention, the appliance remained in the mouth for 3 months. The appliance was then removed, and CBCT was taken at the end of the 3-month retention period (T1). The patients’ reconstructed data with 1 mm slice thickness were recorded as a Digital Imaging and Communication in Medicine file. They were transferred and measured using Dolphin Imaging software V.11.9 (Dolphin Imaging and Management Solutions, Chatsworth, CA, USA).
CBCT images obtained at T0 and T1 were oriented based on the Frankfort horizontal (FH) plane, which was kept parallel to the floor, while on the coronal plane, the midsagittal plane was kept perpendicular to the FH plane, ensuring a standardized head position. The FH plane was constructed by passing through the right and left orbitale and the right external acoustic meatus. The midsagittal plane was constructed using the anterior nasal spine, nasion, and basion. All 2D images were then resliced in accordance with the FH plane.
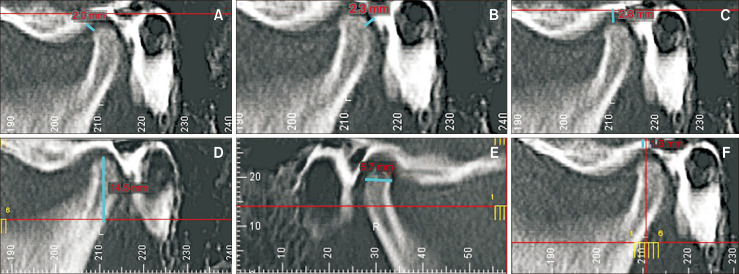
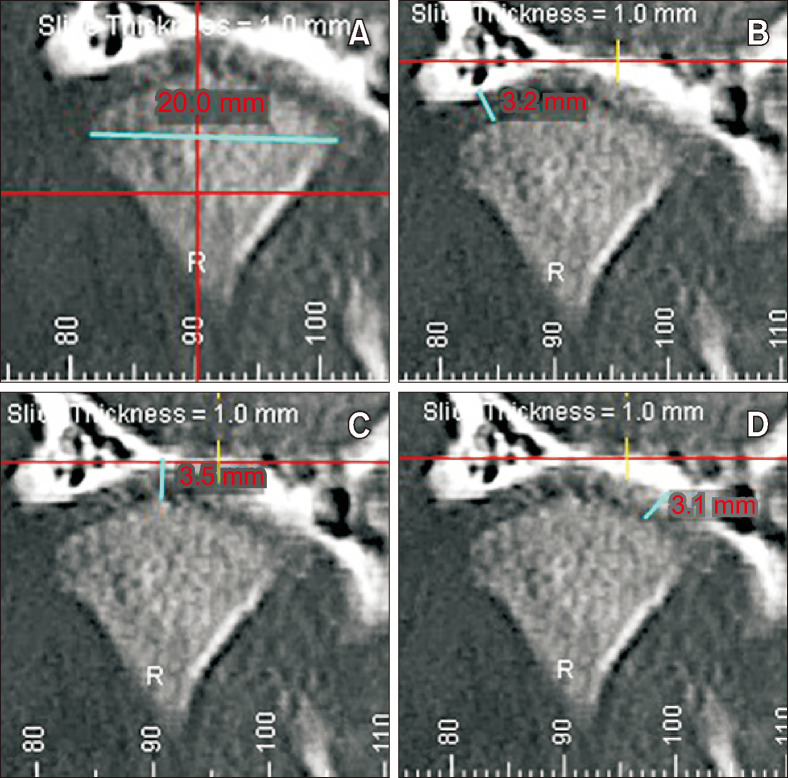
The reference points and linear measurements shown in Table 2 were used during the evaluation of the condyle and glenoid fossa. In the sagittal view, anterior joint space (AJS), posterior joint space (PJS), superior joint space (SJS), condylar height, condylar length, and glenoid fossa roof thickness (Figure 2); and, in the coronal view, condylar width, distal joint space, middle joint space, and medial joint space, were evaluated (Figure 3).
Table 2.
Description of the reference points and linear measurements in the sagittal and coronal views used for evaluating temporomandibular joint changes
| Parameter | Description | |
|---|---|---|
| Reference points | Superior mandibular condyle (Sco) | The most superior point of the condyle |
| Anterior-most condylar point (Aco) | Anterior condyle point 4 mm from the Sco | |
| Posterior-most mandibular condyle point (Pco) | Posterior condyle point 4 mm from the Sco | |
| Inferior sigmoid notch (Inf Sig) | The most inferior point of the sigmoid notch | |
| Inner cortical outline (IC) | The top most point of inner cortical outline | |
| Outer cortical outline (OC) | The lower most point of outer cortical outline | |
| Linear measurements in sagittal view | Anterior joint space (AJS) | The shortest distance between the anterior surface of the mandibular condyle and the glenoid fossa |
| Posterior joint space (PJS) | The shortest distance between the posterior surface of the mandibular condyle and the glenoid fossa | |
| Superior joint space (SJS) | The shortest distance between the superior surface of the mandibular condyle and the glenoid fossa | |
| Condylar height (Ch) | Perpendicular distance between Sco and Inf Sig | |
| Condylar length (Cl) | The distance between Aco and Pco | |
| Glenoid fossa roof thickness (TGF) | Distance between IC and OC | |
| Linear measurements in coronal view | Condylar width (Cw) | The distance between the mesial and distal maximum curvature points of the condyle |
| Distal joint space (DJS) | The shortest distance between the lateral surface of the mandibular condyle and the glenoid fossa | |
| Middle joint space (MidJS) | The shortest distance between the middle surface of the mandibular condyle and the glenoid fossa | |
| Medial joint space (MJS) | The shortest distance between the medial surface of the mandibular condyle and the glenoid fossa |
Figure 2.
Linear measurements taken in the sagittal view. A, Anterior joint space; B, Posterior joint space; C, Superior joint space; D, Condylar height; E, Condylar length; F, Glenoid fossa roof thickness.
Figure 3.
Linear measurements taken in the coronal view. A, Condylar width; B, Distal joint space; C, Middle joint space; D, Medial joint space.
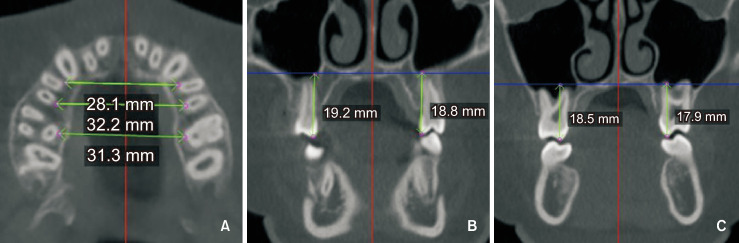
For transversal evaluation, the distance between the first molars, first premolars, and second premolars at the molar’s trifurcation level in the axial section (Figure 4A); for vertical dental evaluation, the distance between the palatal cusp tips of molars and premolars to the palatal plane was measured (Figure 4B and 4C). SNA, SNB, ANB angles, and SNGoGn were measured on lateral cephalometric radiographs obtained from CBCT. After 2 weeks, 10 randomly selected CBCTs were remeasured by the same examiner (SA) for intra-examiner reliability assessment.
Figure 4.
Dental measurements evaluated in the axial and coronal planes; A, Transverse measurements of premolars and molars. B, C, Vertical measurements of premolars and molars.
Statistical analyses
Power analysis was conducted using G*Power version 3.1.10 (Franz Faul, Christian-Albrechts-Universität, Kiel, Germany) software. The sample size was calculated based on the ability to detect 4.64 mm of expansion in the first premolars. The expected standard deviation of expansion was taken from the thesis study of Muştu19 who studied upper airway changes following RME with tooth-tissue-borne and tooth-borne expanders in a similar study sample. The calculation, performed for a t test, indicated that for a study with a power of 0.85 and an alpha of 0.05, a total of 24 patients (12 in each group) were required.
Statistical analyses were performed using SPSS version 25 (IBM Corp., Armonk, NY, USA). The normality of the data was evaluated by the Shapiro–Wilk test. According to the normality test results, numerical variables were assessed using the Wilcoxon test and Paired t test for intragroup evaluations at T0 and T1. Intergroup comparisons of treatment-induced changes were assessed using the Mann–Whitney U test. The reliability of intra-examiner measurements was evaluated with the intraclass correlation coefficient.
RESULTS
Intra-examiner correlation was assessed at a 95% confidence interval, with the variables ranging from 0.80 to 0.95, indicating high reliability in both measurements. Non-parametric variables were assessed using the Wilcoxon test, and parametric variables were assessed using the Paired t test.
Changes in skeletal and dental measurements are presented in Table 3. Expansion with Hyrax or Hybrid Hyrax appliances did not cause changes in sagittal and vertical measurements (P > 0.05). In both groups, interdental distances increased after expansion (P < 0.01), although no statistically significant differences were observed between the groups regarding increases in intermolar and inter-second premolar distances (P > 0.05). However, the increase in inter-first premolar distance was significantly greater in the Hyrax group (P < 0.05). Regarding vertical dental measurement changes, the only significant change was observed in the right second premolars (P < 0.05), whereas no statistically significant difference was found between the two groups (P > 0.05).
Table 3.
Comparison of transverse and vertical dental measurements, and sagittal and vertical skeletal measurements within and between groups
| Hyrax (mean ± SD) |
Hybrid Hyrax (mean ± SD) |
P value | |
|---|---|---|---|
| Transversal dental measurements (T1-T0) | |||
| Intermolar width | 6.71 ± 2.13** | 6.24 ± 3.06** | 0.786 |
| First premolar width | 7.51 ± 2.61** | 4.40 ± 2.80** | 0.017† |
| Second premolar width | 6.05 ± 2.91** | 4.28 ± 2.80** | 0.211 |
| Vertical dental measurements (T1-T0) | |||
| Right | |||
| Molar vertical difference | 0.46 ± 1.90 | −0.06 ± 1.55 | 0.514 |
| First premolar vertical difference | 0.38 ± 1.69 | 0.69 ± 1.59 | 0.531 |
| Second premolar vertical difference | 1.38 ± 2.18* | 0.98 ± 2.19 | 0.849 |
| Left | |||
| Molar vertical difference | −0.02 ± 1.68 | 0.26 ± 1.87 | 0.341 |
| First premolar vertical difference | 2.25 ± 8.54 | 0.53 ± 2.61 | 0.462 |
| Second premolar vertical difference | 0.53 ± 1.78 | 1.10 ± 1.71 | 0.369 |
| Sagittal and vertical skeletal measurements (T1-T0) | |||
| SNA | −0.53 ± 1.28 | −0.34 ± 1.79 | 0.567 |
| SNB | 0.10 ± 1.53 | −0.55 ± 1.66 | 0.114 |
| ANB | −0.43 ± 1.22 | −1.16 ± 1.54 | 0.341 |
| SNGoGn | −0.36 ± 2.20 | −1.39 ± 1.74 | 0.231 |
SD, standard deviation.
*P < 0.05, **P < 0.01 according to Wilcoxon Test results for evaluation T1-T0 difference.
†P < 0.05 according to Mann–Whitney U test results for evaluation differences between 2 groups.
Measurements related to the condylar position and dimensions are presented in Table 4. In both groups, condylar dimensions and the condyle’s position in the glenoid fossa did not change significantly from T0 to T1 (P > 0.05).
Table 4.
Comparison of condylar changes within and between groups
| Hyrax (n = 13) | Hybrid Hyrax (n = 12) | Hyrax | Hybrid Hyrax | P value | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T0 (mean ± SD) |
T1 (mean ± SD) |
P value | T0 (mean ± SD) |
T1 (mean ± SD) |
P value | T1-T0 (mean ± SD) |
T1-T0 (mean ± SD) |
|||||
| Right | ||||||||||||
| Anterior joint space | 2.22 ± 1.11 | 2.24 ± 0.71 | 0.937 | 2.27 ± 1.27 | 2.22 ± 0.73 | 0.860 | 0.02 ± 1.02 | −0.05 ± 0.95 | 0.856 | |||
| Posterior joint space | 2.06 ± 0.54 | 2.07 ± 0.49 | 0.928 | 2.25 ± 0.76 | 2.07 ± 0.53 | 0.183 | 0.02 ± 0.60 | −0.18 ± 0.44 | 0.363 | |||
| Superior joint space | 2.20 ± 0.75 | 2.39 ± 0.61 | 0.280 | 2.60 ± 0.68 | 2.39 ± 0.68 | 0.463 | 0.18 ± 0.58 | −0.20 ± 0.94 | 0.222 | |||
| Condylar height | 15.96 ± 2.86 | 15.96 ± 2.89 | > 0.999 | 16.23 ± 2.41 | 16.05 ± 2.72 | 0.572 | 0 ± 1.68 | −0.17 ± 1.04 | 0.760 | |||
| Condylar length | 6.39 ± 0.78 | 6.09 ± 0.66 | 0.073 | 6.25 ± 1.19 | 6.35 ± 1.08 | 0.542 | −0.30 ± 0.55 | 0.10 ± 0.55 | 0.083 | |||
| Glenoid fossa roof thickness | 1.84 ± 0.46 | 1.83 ± 0.42 | 0.936 | 1.80 ± 0.55 | 1.90 ± 0.29 | 0.556 | −0.01 ± 0.33 | 0.09 ± 0.52 | 0.575 | |||
| Condylar width | 18.36 ± 2.40 | 18.43 ± 2.84 | 0.843 | 17.34 ± 2.11 | 17.21 ± 2.38 | 0.543 | 0.07 ± 1.23 | −0.12 ± 0.69 | 0.635 | |||
| Distal joint space | 2.43 ± 0.69 | 2.35 ± 0.73 | 0.614 | 2.56 ± 1.01 | 2.05 ± 0.74 | 0.091 | −0.08 ± 0.58 | −0.51 ± 0.96 | 0.186 | |||
| Middle joint space | 2.24 ± 0.71 | 2.37 ± 0.63 | 0.582 | 2.33 ± 0.73 | 2.25 ± 0.79 | 0.636 | 0.13 ± 0.83 | −0.07 ± 0.53 | 0.474 | |||
| Medial joint space | 2.27 ± 0.62 | 2.15 ± 0.47 | 0.347 | 2.58 ± 0.82 | 2.58 ± 0.67 | > 0.999 | −0.12 ± 0.45 | 0.01 ± 0.80 | 0.638 | |||
| Left | ||||||||||||
| Anterior joint space | 2.21 ± 1.57 | 2.18 ± 1.67 | 0.912 | 1.96 ± 0.53 | 1.91 ± 0.37 | 0.723 | −0.03 ± 0.98 | −0.05 ± 0.47 | 0.952 | |||
| Posterior joint space | 2.35 ± 0.77 | 2.22 ± 0.81 | 0.504 | 1.92 ± 0.46 | 2.11 ± 0.28 | 0.318 | −0.13 ± 0.68 | 0.19 ± 0.63 | 0.236 | |||
| Superior joint space | 2.70 ± 9.91 | 2.79 ± 0.99 | 0.545 | 2.19 ± 0.65 | 2.41 ± 0.78 | 0.179 | 0.09 ± 0.53 | 0.22 ± 0.54 | 0.544 | |||
| Condylar height | 16.12 ± 2.40 | 15.71 ± 2.55 | 0.239 | 16.03 ± 3.46 | 15.88 ± 3.64 | 0.640 | −0.40 ± 1.18 | −0.15 ± 1.08 | 0.577 | |||
| Condylar length | 6.28 ± 0.66 | 6.52 ± 0.93 | 0.218 | 6.25 ± 0.85 | 6.18 ± 0.90 | 0.561 | 0.23 ± 0.66 | −0.07 ± 0.43 | 0.178 | |||
| Glenoid fossa roof thickness | 1.70 ± 0.48 | 1.66 ± 0.38 | 0.828 | 1.76 ± 0.44 | 1.67 ± 0.36 | 0.317 | −0.04 ± 0.62 | −0.09 ± 0.52 | 0.792 | |||
| Condylar width | 18.25 ± 2.24 | 18.14 ± 2.45 | 0.594 | 17.47 ± 1.97 | 17.45 ± 2.04 | 0.826 | −0.11 ± 0.71 | −0.02 ± 0.38 | 0.724 | |||
| Distal joint space | 2.71 ± 0.81 | 2.43 ± 1.18 | 0.432 | 2.78 ± 0.45 | 2.34 ± 0.98 | 0.544 | −0.28 ± 1.26 | −0.44 ± 0.78 | 0.100 | |||
| Middle joint space | 2.68 ± 0.97 | 2.68 ± 1.04 | 0 | 2.14 ± 0.77 | 2.21 ± 0.71 | 0.782 | 0 ± 1.03 | 0.07 ± 0.53 | 0.474 | |||
| Medial joint space | 1.97 ± 0.57 | 2.26 ± 0.69 | 0.137 | 2.65 ± 1.37 | 2.60 ± 1.03 | 0.854 | 0.28 ± 0.64 | −0.05 ± 0.92 | 0.300 | |||
SD, standard deviation.
DISCUSSION
The present study was designed to compare the alterations in mandibular condyle and glenoid fossa morphology among patients undergoing expansion with Hyrax and Hybrid Hyrax appliances. Although the effects of tooth-borne maxillary expansion appliances on the condyle have been evaluated before,20 the effects of tooth-bone-borne expansion appliances on the condyle have not yet been examined in the literature.
CBCT was used to evaluate the temporomandibular area after RME to overcome the limitations of conventional 2D evaluation methods, including difficulties in landmark identification and the superimposition of anatomic structures.18 Conventional 2D records have not yet demonstrated superior diagnostic capability compared to CBCT, and they have caused interpretation mistakes.14,21 CBCT allows a more comprehensive examination of the temporomandibular joint, and a detailed CBCT analysis can contribute to a precise assessment of positional and morphological changes in the temporomandibular joint following various orthodontic treatments.22,23
As a result of the 3-dimensional evaluations, condylar morphology and position in both groups did not indicate any significant change after the expansion. Similar to our findings, McLeod et al.7 found no statistically significant change in the position of the condyle within the glenoid fossa following RME therapy with Hyrax appliances. They reported that RME treatments resulted in subtle effects or changes in condylar position. Additionally, in a case report by Huqh et al.,14 no changes were found in condylar height, width, length, and volume. However, they did find a decrease in the SJS and PJS and an increase in the AJS due to changes in condyle position, which may be attributed to the use of Class III elastics during both the active expansion and retention periods.
Contrary to our findings, some studies indicate differences in condylar position following RME in patients with unilateral crossbite and functional shift.10,12,13,24,25 These contradictory findings may be due to the different nature of the studied cases. In our study, patients had bilateral or unilateral crossbite with no functional shift, and since the condylar positions were normal at the beginning, condylar spaces and positions may not have changed after RME. Changes in the condyle could be adaptive alterations to occlusal changes, facilitating correction of mandibular position. Studies have shown that condyles rotate to correct deviation after maxillary expansion in participants with unilateral crossbite and functional shift. There was no major difference in joint spaces and relative condylar position on the crossbite side after RME.9,10,12,13,24,25 Furthermore, it was reported that the condyle on the crossbite side was located more normally than the non-crossbite condyle;25,26 the difference was due to the non-crossbite condyle, and this incorrect position was corrected with RME.9,10,25 If the condylar position is normal before maxillary expansion, no change in condylar position is likely.
In these studies where condylar changes were observed following expansion in patients with functional shift,10,12,13,24 the average age of the patients was younger than in our study. Participants in the late adolescent stage were selected to control relapse following expansion. According to the regression analysis, Wang et al.12 reported less change in condyle position after RME in those with more advanced skeletal maturation. The age difference may also explain the lack of condyle position changes before and after expansion in our study.
Short- and long-term evaluation of expansion effects may also explain the inconsistent findings across studies.11,20,24 In the short term, premature contacts become evident after expansion,11,27,28 which may lead to positional changes of the condyle in the glenoid fossa. In their CBCT evaluation 3 weeks after expansion, Melgaço et al.20 observed an immediate change in condyle position, showing that the condyle moved downward and forward. Leonardi et al.24 evaluated CBCT images taken at the end of an average 18-day activation period and reported statistically notable alterations in condylar position, even in small amounts. A symmetrical condyle-fossa relationship was observed on both sides after expansion. Therefore, in studies examining the short-term effects of RME on the condyle,20,24 differences related to changes in intercuspation following RME may have been observed. On the other hand, during the retention phase after expansion, settling of the occlusion may be expected,11,15,27,28 leading the condyles to return to their original positions. Thus, in relatively long-term studies, these short-term effects of RME on the condyles could not be demonstrated.7 However, studies evaluating both short- and long-term effects of RME should be conducted to support this explanation.
Buccal tipping of the posterior teeth during expansion is a common side effect, which may lead to condylar rotation and mandibular clockwise rotation, causing increased vertical dimensions and open bite. In our study, condylar rotation was assessed by comparing pre- and post-expansion vertical cephalometric measurements and glenoid fossa dimensions. Since there were no significant changes in vertical cephalometric measurements or superior, anterior, and PJSs, we concluded that there was no significant condylar and mandibular rotation 3 months after RME. In the literature, no studies have directly evaluated condylar rotation after RME. However, similar to our findings, Lagravère et al.29 and Rossi et al.30 reported no vertical dimensional changes after a 3–6 month retention period. On the other hand, there is no consensus on the effects of RME regarding vertical dimensional changes.28,31,32 Several authors stated that vertical dimension changes after RME were less than 2 mm or 2 degrees and might not be clinically significant.27,33 In the short term, the only variable that exhibited a notable increase was total anterior facial height, reflecting a temporary effect due to occlusal interferences.27,28,30,31
When tooth- and tooth-bone-borne appliances were compared, no transversal differences were found in the first molar region between the groups, similar to the findings of Garib et al.6 This finding may be explained by the fact that the first molar teeth served as the anchorage teeth in both appliances. However, in the premolar region, less expansion was achieved in the Hybrid Hyrax group. This difference might be due to contact between the Hyrax expander arms and the premolars, whereas the Hybrid Hyrax appliance is supported by two miniscrews inserted bilaterally to the midpalatal suture in the anterior region and is not attached to the premolars. In accordance with the transversal changes, no vertical dental changes were observed in the posterior teeth of the Hybrid Hyrax group. Thus, it was hypothesized that this would cause less premature contact with the mandibular teeth, and accordingly, a difference would be seen in condylar measurements. However, our hypothesis was rejected because no significant differences in condylar measurements were observed between the groups. In the literature, comparison of different expansion appliances in terms of condylar response is rare, but Melgaço et al.,20 who compared the short-term effects of Hyrax and Haas appliances on condylar position, found no difference between the two appliances, although both caused some changes in condylar position. They attributed this to similar intercuspal changes with both appliances and reported that the change in condyle position could be caused by the appliance effect rather than the appliance type.
One limitation of this study is the relatively short 3-month follow-up period. Three months may be considered relatively short for completing condylar changes. This period is also necessary to determine whether changes in condyle position and joint spaces are temporary or likely to recur. Given these limitations, the findings should be interpreted as preliminary. Further prospective longitudinal studies with larger sample sizes are warranted to verify our findings and evaluate the response of different RME appliances on the condyle and glenoid fossa.
CONCLUSIONS
The null hypothesis of the study was accepted: both tooth- and tooth-bone-borne appliances did not cause any changes in condylar positions and dimensions after RME.
Footnotes
AUTHOR CONTRIBUTIONS
Conceptualization: All authors. Data curation: SA. Formal analysis: DGC. Investigation: SA. Methodology: MNE, DGC. Software: SA. Validation: MNE, SA. Visualization: SA. Writing–original draft: MNE. Writing–review & editing: MNE, DGC.
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
None to declare.
REFERENCES
- 1.Haas AJ. Palatal expansion: just the beginning of dentofacial orthopedics. Am J Orthod. 1970;57:219–55. doi: 10.1016/0002-9416(70)90241-1. https://doi.org/10.1016/0002-9416(70)90241-1. [DOI] [PubMed] [Google Scholar]
- 2.Mehta S, Chen PJ, Vich ML, Upadhyay M, Tadinada A, Yadav S. Bone-anchored versus tooth-anchored expansion appliances: long-term effects on the condyle-fossa relationship. J World Fed Orthod. 2021;10:144–54. doi: 10.1016/j.ejwf.2021.07.001. https://doi.org/10.1016/j.ejwf.2021.07.001. [DOI] [PubMed] [Google Scholar]
- 3.Lin L, Ahn HW, Kim SJ, Moon SC, Kim SH, Nelson G. Tooth-borne vs bone-borne rapid maxillary expanders in late adolescence. Angle Orthod. 2015;85:253–62. doi: 10.2319/030514-156.1. https://doi.org/10.2319/030514-156.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baysal A, Uysal T, Veli I, Ozer T, Karadede I, Hekimoglu S. Evaluation of alveolar bone loss following rapid maxillary expansion using cone-beam computed tomography. Korean J Orthod. 2013;43:83–95. doi: 10.4041/kjod.2013.43.2.83. https://doi.org/10.4041/kjod.2013.43.2.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim YH, Yang SM, Kim S, Lee JY, Kim KE, Gianelly AA, et al. Midpalatal miniscrews for orthodontic anchorage: factors affecting clinical success. Am J Orthod Dentofacial Orthop. 2010;137:66–72. doi: 10.1016/j.ajodo.2007.11.036. https://doi.org/10.1016/j.ajodo.2007.11.036. [DOI] [PubMed] [Google Scholar]
- 6.Garib D, Miranda F, Palomo JM, Pugliese F, da Cunha Bastos JC, Dos Santos AM, et al. Orthopedic outcomes of hybrid and conventional Hyrax expanders. Angle Orthod. 2021;91:178–86. doi: 10.2319/060820-527.1. https://doi.org/10.2319/060820-527.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McLeod L, Hernández IA, Heo G, Lagravère MO. Condylar positional changes in rapid maxillary expansion assessed with cone-beam computer tomography. Int Orthod. 2016;14:342–56. doi: 10.1016/j.ortho.2016.07.006. https://doi.org/10.1016/j.ortho.2016.07.006. [DOI] [PubMed] [Google Scholar]
- 8.Lam PH, Sadowsky C, Omerza F. Mandibular asymmetry and condylar position in children with unilateral posterior crossbite. Am J Orthod Dentofacial Orthop. 1999;115:569–75. doi: 10.1016/S0889-5406(99)70282-9. https://doi.org/10.1016/s0889-5406(99)70282-9. [DOI] [PubMed] [Google Scholar]
- 9.Nerder PH, Bakke M, Solow B. The functional shift of the mandible in unilateral posterior crossbite and the adaptation of the temporomandibular joints: a pilot study. Eur J Orthod. 1999;21:155–66. doi: 10.1093/ejo/21.2.155. https://doi.org/10.1093/ejo/21.2.155. [DOI] [PubMed] [Google Scholar]
- 10.Hesse KL, Artun J, Joondeph DR, Kennedy DB. Changes in condylar postition and occlusion associated with maxillary expansion for correction of functional unilateral posterior crossbite. Am J Orthod Dentofacial Orthop. 1997;111:410–8. doi: 10.1016/S0889-5406(97)80023-6. https://doi.org/10.1016/s0889-5406(97)80023-6. [DOI] [PubMed] [Google Scholar]
- 11.Torres D, Lopes J, Magno MB, Cople Maia L, Normando D, Leão PB. Effects of rapid maxillary expansion on temporomandibular joints. Angle Orthod. 2020;90:442–56. doi: 10.2319/080619-517.1. https://doi.org/10.2319/080619-517.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang Z, Spoon ME, Khan J, Barmak AB, Rossouw PE, Michelogiannakis D. Cone beam computed tomographic evaluation of the changes in condylar position in growing patients with unilateral posterior crossbite undergoing rapid maxillary expansion followed by fixed orthodontic therapy. Eur Arch Paediatr Dent. 2021;22:959–67. doi: 10.1007/s40368-021-00628-z. https://doi.org/10.1007/s40368-021-00628-z. [DOI] [PubMed] [Google Scholar]
- 13.Pinto AS, Buschang PH, Throckmorton GS, Chen P. Morphological and positional asymmetries of young children with functional unilateral posterior crossbite. Am J Orthod Dentofacial Orthop. 2001;120:513–20. doi: 10.1067/mod.2001.118627a. https://doi.org/10.1067/mod.2001.118627a. [DOI] [PubMed] [Google Scholar]
- 14.Huqh MZU, Hassan R, Rahman RA, Yusof A, Narmada IB, Ahmad W. The short-term effect of active skeletonized sutural distractor appliance on temporomandibular joint morphology of class III malocclusion subjects. Eur J Dent. 2021;15:523–32. doi: 10.1055/s-0040-1722483. https://doi.org/10.1055/s-0040-1722483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kecik D, Kocadereli I, Saatci I. Evaluation of the treatment changes of functional posterior crossbite in the mixed dentition. Am J Orthod Dentofacial Orthop. 2007;131:202–15. doi: 10.1016/j.ajodo.2005.03.030. https://doi.org/10.1016/j.ajodo.2005.03.030. [DOI] [PubMed] [Google Scholar]
- 16.Arat FE, Arat ZM, Tompson B, Tanju S, Erden I. Muscular and condylar response to rapid maxillary expansion. Part 2: magnetic resonance imaging study of the temporomandibular joint. Am J Orthod Dentofacial Orthop. 2008;133:823–9. doi: 10.1016/j.ajodo.2006.07.029. https://doi.org/10.1016/j.ajodo.2006.07.029. [DOI] [PubMed] [Google Scholar]
- 17.Ghoussoub MS, Rifai K, Garcia R, Sleilaty G. Effect of rapid maxillary expansion on glenoid fossa and condyle-fossa relationship in growing patients (MEGP): study protocol for a controlled clinical trial. J Int Soc Prev Community Dent. 2018;8:130–6. doi: 10.4103/jispcd.JISPCD_458_17. https://doi.org/10.4103/jispcd.JISPCD_458_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gunyuz Toklu M, Germec-Cakan D, Tozlu M. Periodontal, dentoalveolar, and skeletal effects of tooth-borne and tooth-bone-borne expansion appliances. Am J Orthod Dentofacial Orthop. 2015;148:97–109. doi: 10.1016/j.ajodo.2015.02.022. https://doi.org/10.1016/j.ajodo.2015.02.022. [DOI] [PubMed] [Google Scholar]
- 19.Muştu ÜC. Yeditepe University; Istanbul: 2015. Three-dimensional evaluation of upper airway following tooth and tooth-bone borne rapid maxillary expansion [PhD dissertation] https://platform.almanhal.com/Details/Thesis/2000089013. [Google Scholar]
- 20.Melgaço CA, Columbano Neto J, Jurach EM, Nojima Mda C, Nojima LI. Immediate changes in condylar position after rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2014;145:771–9. doi: 10.1016/j.ajodo.2014.01.024. https://doi.org/10.1016/j.ajodo.2014.01.024. [DOI] [PubMed] [Google Scholar]
- 21.Arieta-Miranda JM, Silva-Valencia M, Flores-Mir C, Paredes-Sampen NA, Arriola-Guillen LE. Spatial analysis of condyle position according to sagittal skeletal relationship, assessed by cone beam computed tomography. Prog Orthod. 2013;14:36. doi: 10.1186/2196-1042-14-36. https://doi.org/10.1186/2196-1042-14-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lascala CA, Panella J, Marques MM. Analysis of the accuracy of linear measurements obtained by cone beam computed tomography (CBCT-NewTom) Dentomaxillofac Radiol. 2004;33:291–4. doi: 10.1259/dmfr/25500850. https://doi.org/10.1259/dmfr/25500850. [DOI] [PubMed] [Google Scholar]
- 23.Nithin, Ahmed J, Sujir N, Shenoy N, Binnal A, Ongole R. Morphological assessment of TMJ spaces, mandibular condyle, and glenoid fossa using cone beam computed tomography (CBCT): a retrospective analysis. Indian J Radiol Imaging. 2021;31:78–85. doi: 10.1055/s-0041-1729488. https://doi.org/10.1055/s-0041-1729488. 63d7e8ca7a214b09acb2780b633f8e8f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leonardi R, Caltabiano M, Cavallini C, Sicurezza E, Barbato E, Spampinato C, et al. Condyle fossa relationship associated with functional posterior crossbite, before and after rapid maxillary expansion. Angle Orthod. 2012;82:1040–6. doi: 10.2319/112211-725.1. https://doi.org/10.2319/112211-725.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Myers DR, Barenie JT, Bell RA, Williamson EH. Condylar position in children with functional posterior crossbites: before and after crossbite correction. Pediatr Dent. 1980;2:190–4. [PubMed] [Google Scholar]
- 26.Thurston MH. University of California; Los Angeles: 1986. Dental and facial characteristics associated with an unilateral posterior crossbite in the permanent dentition [PhD dissertation] https://search.worldcat.org/ko/title/13880631. [Google Scholar]
- 27.Lione R, Franchi L, Cozza P. Does rapid maxillary expansion induce adverse effects in growing subjects? Angle Orthod. 2013;83:172–82. doi: 10.2319/041012-300.1. https://doi.org/10.2319/041012-300.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chung CH, Font B. Skeletal and dental changes in the sagittal, vertical, and transverse dimensions after rapid palatal expansion. Am J Orthod Dentofacial Orthop. 2004;126:569–75. doi: 10.1016/j.ajodo.2003.10.035. https://doi.org/10.1016/j.ajodo.2003.10.035. [DOI] [PubMed] [Google Scholar]
- 29.Lagravère MO, Carey J, Heo G, Toogood RW, Major PW. Transverse, vertical, and anteroposterior changes from bone-anchored maxillary expansion vs traditional rapid maxillary expansion: a randomized clinical trial. Am J Orthod Dentofacial Orthop. 2010;137:304.e1–12. discussion 304–5. doi: 10.1016/j.ajodo.2009.09.016. https://doi.org/10.1016/j.ajodo.2009.09.016. [DOI] [PubMed] [Google Scholar]
- 30.Rossi M, Rossi A, Abrão J. Skeletal alterations associated with the use of bonded rapid maxillary expansion appliance. Braz Dent J. 2011;22:334–9. doi: 10.1590/S0103-64402011000400013. https://doi.org/10.1590/s0103-64402011000400013. [DOI] [PubMed] [Google Scholar]
- 31.Reed N, Ghosh J, Nanda RS. Comparison of treatment outcomes with banded and bonded RPE appliances. Am J Orthod Dentofacial Orthop. 1999;116:31–40. doi: 10.1016/S0889-5406(99)70300-8. https://doi.org/10.1016/s0889-5406(99)70300-8. [DOI] [PubMed] [Google Scholar]
- 32.Sandikçioğlu M, Hazar S. Skeletal and dental changes after maxillary expansion in the mixed dentition. Am J Orthod Dentofacial Orthop. 1997;111:321–7. doi: 10.1016/S0889-5406(97)70191-4. https://doi.org/10.1016/s0889-5406(97)70191-4. [DOI] [PubMed] [Google Scholar]
- 33.Cozza P, Baccetti T, Franchi L, De Toffol L, McNamara JA., Jr Mandibular changes produced by functional appliances in Class II malocclusion: a systematic review. Am J Orthod Dentofacial Orthop. 2006;129:599.e1–12. discussion e1–6. doi: 10.1016/j.ajodo.2005.11.010. https://doi.org/10.1016/j.ajodo.2005.11.010. [DOI] [PubMed] [Google Scholar]