Abstract
Complete surgical excision for extensive left atrial tumors are technically demanding procedures because of limited surgical corridor. We report a case of a giant left atrial ancient schwannoma in a 67-year-old woman, who underwent extensive bi-atrial and interatrial septal resection and reconstruction without auto-transplantation via a modified superior trans-septal approach.
Key Words: atrial fibrillation, atrial septal defect, imaging
Graphical Abstract
Take-Home Messages
-
•
Because the surgical corridor to the left atrium through left atriotomy alone is limited, a variety of techniques to improve surgical exposure were used including total cardiac autotransplantation, partial autotransplantation, and the modified superior transseptal approach. The choice of technique relies on surgical expertise and needs to be individualized.
-
•
The extent of atrial and septal resection to achieve oncological clearance may be extensive. Novel reconstructive techniques may be required to restore atrioventricular continuum.
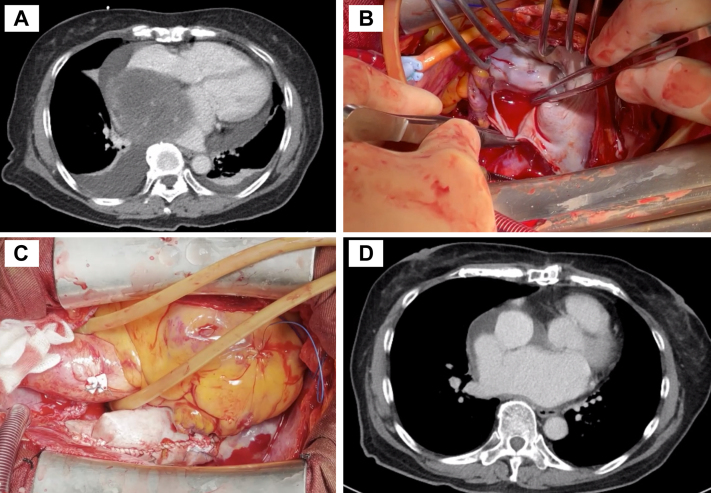
A 67-year-old woman with good past health presented to the emergency department with dyspnea on exertion and palpitations for 2 weeks. Electrocardiogram showed fast atrial fibrillation. Transthoracic echocardiography showed a 9-cm hyperechogenic left atrial tumor. Contrast computed tomography (CT) image of the thorax showed that the tumor was broad-based with no demonstrable tissue planes with the left atrial (LA) roof, interatrial septum (IAS), and the right pulmonary vein (PV) antrum close to the right superior pulmonary vein (RSPV) (Video 1). A positron emission tomography CT scan was non-revealing for extracardiac malignancies.
Complete tumor excision was performed via a median sternotomy. The patient was put on cardiopulmonary bypass via ascending aortic, superior vena cava (SVC), and left femoral venous cannulation. After cross-clamping and cardioplegia administration, cavae were snared and SVC was transected at the SVC–right atrial (RA) junction below the sinoatrial node. A modified superior transseptal approach was used to widen the surgical corridor for exposure. It was not possible to peel the tumor from the adherent LA surfaces without compromising oncological clearance. Therefore, extensive bi-atrial and interatrial septal resection was performed.
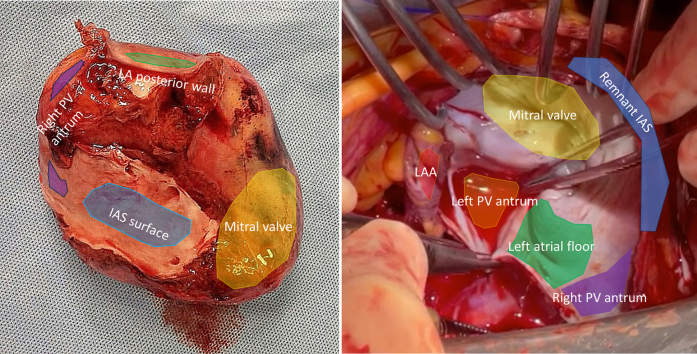
The resection included the tumor en bloc with the entire LA roof, most of the posterior LA wall, the entire IAS, and part of the right pulmonary vein antrum close to the RSPV (Figure 1). The resection bed consisted of the remnant left atrial appendage (LAA), the left PV antrum, and a 3-cm strip of LA floor connecting the left antrum to the remnant right antrum. The intrapericardial RSPV remnant was disconnected from the right antrum and measured 1.5 cm in length.
Figure 1.
Photo of the Specimen and Resection Bed
(Left panel) Excised specimen. The tumor was grossly adherent to the adjacent left atrial (LA) surfaces including the LA roof, posterior LA wall, and right pulmonary vein (PV) antrum. Blue indicates the interatrial septum (IAS) surface. Green indicates the posterior LA wall surface; Purple indicates the right PV antrum surface. Yellow indicates the mitral valve surface. (Right panel) Resection bed. The resection bed consisted of the remnant left atrial appendage (LAA), the left PV antrum, and a 3-cm strip of LA floor connecting the left antrum to the remnant right antrum. Blue indicates remnant IAS. Red indicates the LAA. Green indicates the posterior LA wall surface and LA floor. Purple indicates the remnant right PV antrum. Orange indicates the left PV antrum. Yellow indicates the mitral valve.
Reconstruction began with a piece of bovine pericardium first sutured near the LAA orifice and carried along the remnant native LA tissue in a circumferential manner along the LA floor and left PV antrum (Video 2). A 2-cm hole was made in the patch at the location of RSPV reimplantation. The backwall of the RSPV was reconstructed with interrupted 5/0 Prolene sutures, and the anastomosis was completed in a running continuous fashion. The suture line was continued along the remnant IAS, terminating at the right PV antrum.
A cylindrical pericardial conduit was fashioned to restore continuity between the cavae and the tricuspid valve (Video 3). The inferior end was sutured along the IAS and right atrial (RA) free wall. The superior end was sutured to the SVC-RA junction. After declamping, the heart entered a junctional rhythm of 45 to 50 beats/min. Two temporary epicardial ventricular pacing wires were placed. At approximately 1 week after the operation, she recovered an atrial ectopic rhythm of 70 beats/min. Conduction block was not observed on telemetry in the subsequent week. Therefore, a permanent pacemaker was not required.
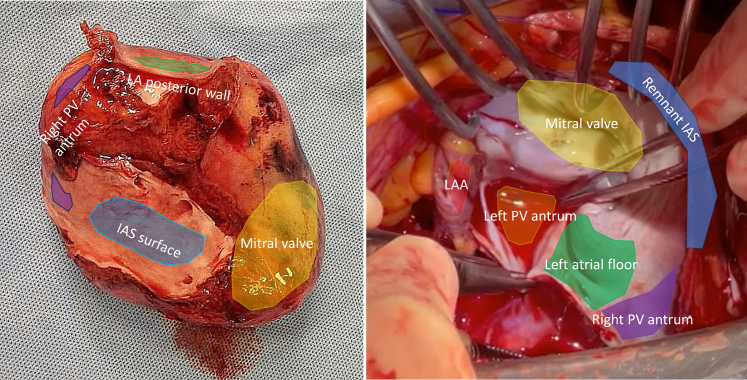
Histopathologic examination showed circumscribed proliferation of spindle cells with immunostaining positive for S100 and SOX10, compatible with Schwann cell origin (Figure 2). Resection margins were clear. The pathologic diagnosis was ancient schwannoma, with the term “ancient” referring to the presence of advanced degenerative changes and diffuse hypocellular areas in the tumor core. These changes are believed to occur because it takes a long time for schwannomas to develop.1 A contrast CT scan of the thorax at 6 months showed no locoregional recurrence (Video 4; see Figure 3 for still images from each video). The patient is alive and well after 18 months of clinical follow-up. Informed consent was obtained for publication of recorded materials.
Figure 2.
Histomicrograph of the Ancient Schwannoma
(A) Microscopic examination reveals nuclear palisading, Verocay bodies, myxoid changes, and dilated vessels (hematoxylin and eosin stain, original magnification ×4). (B) Positivity for S100 (immunohistochemistry, original magnification ×20). (C) Positivity for SOX10 (immunohistochemistry, original magnification ×20). Photo courtesy of Dr Pensi Lam, Department of Anatomical and Cellular Pathology, Prince of Wales Hospital.
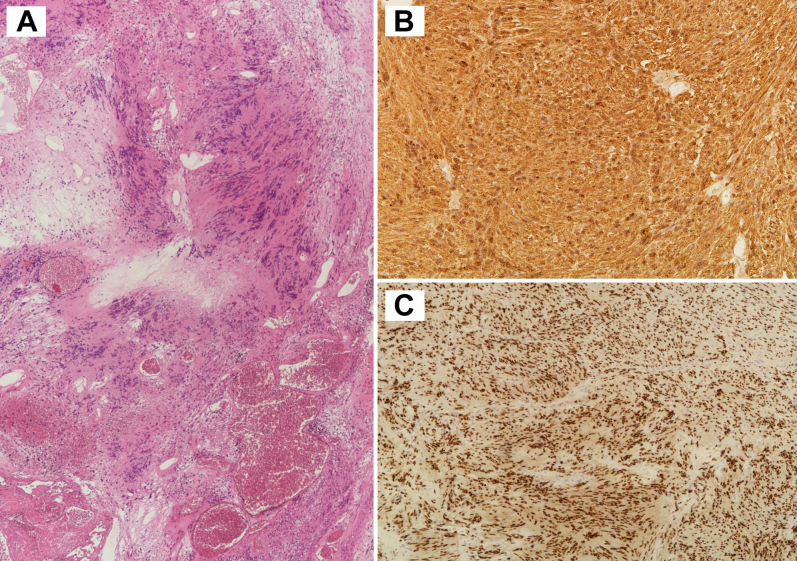
Figure 3.
The Most Important Stills From Each Video
(A) Preoperative computed tomography scan (from Video 1). (B) Left atrial resection bed (from Video 2). (C) Reconstructed right atrium (from Video 3). (D) Postoperative computed tomography scan (from Video 4).
The procedure of choice for extensive LA tumors is cardiac autotransplantation, with the largest modern case series from Houston Methodist Hospital.2 The procedure involves complete cardiac explantation, ex vivo tumor resection, and reconstruction with subsequent autotransplantation. The modified superior transseptal approach eliminates the aorta, pulmonary trunk, and inferior vena cava (IVC) anastomoses. Although this significantly reduces cross-clamp time and maintains cardiac alignment, this comes at the cost of worse exposure for the left PV antrum and LAA. The choice between superior transseptal, partial, and complete autotransplantation relies on surgical expertise and must be individualized.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
Preoperative Computed Tomography Scan of the Thorax
The tumor was broad-based with no demonstrable tissue planes with the LA roof, IAS, and the right PV antrum near the RSPV.
Reconstruction of the Left Atrium
Resection bed anatomy was inspected. Technique of right superior pulmonary vein reimplantation shown.
Cavo-Tricuspid Conduit Creation
A cylindrical cavo-tricuspid conduit was fashioned, sewing the superior end to the right atrium–superior vena cava junction, and the inferior end to the right atrial free wall and remnant interatrial septum.
Postoperative Computed Tomography of the Thorax
No evidence of locoregional recurrence at 6 months postoperatively.
References
- 1.WHO Classification of Tumours Editorial Board . 5th ed. International Agency for Research on Cancer; Lyon: 2021. World Health Organization Classification of Tumours of the Central Nervous System. [Google Scholar]
- 2.Al Abri Q., El Nihum L.I., Ali A., et al. Outcomes of full and partial cardiac autotransplantation for complex left-sided heart tumors. Ann Thorac Surg Short Rep. 2023;1(1):164–167. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Preoperative Computed Tomography Scan of the Thorax
The tumor was broad-based with no demonstrable tissue planes with the LA roof, IAS, and the right PV antrum near the RSPV.
Reconstruction of the Left Atrium
Resection bed anatomy was inspected. Technique of right superior pulmonary vein reimplantation shown.
Cavo-Tricuspid Conduit Creation
A cylindrical cavo-tricuspid conduit was fashioned, sewing the superior end to the right atrium–superior vena cava junction, and the inferior end to the right atrial free wall and remnant interatrial septum.
Postoperative Computed Tomography of the Thorax
No evidence of locoregional recurrence at 6 months postoperatively.